Cognitive Behavioural Therapy
Original Editor - Rachael Lowe
Top Contributors - Scott Buxton, Anthonia Abraham, Kim Jackson, Vidya Acharya, Patti Cavaleri, Shaimaa Eldib, Claire Knott, Rachael Lowe, Mariam Hashem and WikiSysop
What is Cognitive Behavioural Therapy?[edit | edit source]
Cognitive Behavioural Therapy (CBT) is a method that can help manage problems by changing the way patients would think and behave. It is not designed to remove any problems but help manage them in a positive manner [1] [2].
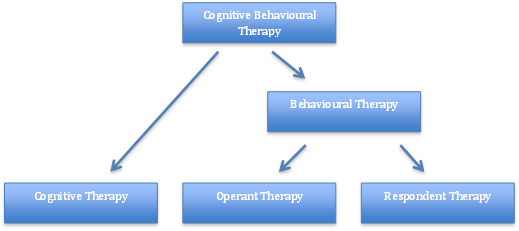
Behaviour therapy (BT) was developed in the 1950’s independently in three countries: South Africa, USA and England [3]. It was further developed to Cognitive Therapy (CT) in the 1970’s by Dr Aaron Beck with its main application on people with depression, anxiety and eating disorders [1][4]. However, the main evidence today focuses on CBT, after the merging of BT and CT in the late 80’s [5].
Fig.2 - Breakdown of CBT theory
The Cognitive Behavioural Therapy Model[edit | edit source]
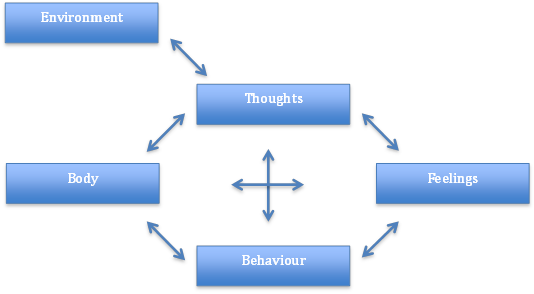
Fig.3 - Factors involved within the Cognitive Behavioural Therapy Model
Aaron Beck and Christine Padesky first recognised this CBT model in the 1970s [6].
How it is Used[edit | edit source]
Negative thoughts (e.g., "My back pain is uncontrollable" --> Negative feelings (e.g., depression, anger) and maladaptive health behaviours (e.g., skipping treatment sessions) --> Reinforcing negative cycle.
If one negative thought can be changed or better understood, then it can break down this negative cycle. This can be addressed through education and methods to manage symptoms [6]. This is address through various approaches including cognitive restructuring, behavior activation, exposure, and problem-solving strategies[7].
CBT can be delivered through individualized sessions or group sessions. A recent integrative review found that online formats of CBT may be comparable with traditional formats[8].
CBT and Chronic Pain[edit | edit source]
CBT has been increasingly studied and considered as an intervention as part of a multimodal approach for those with chronic pain. CBT has been studied to address activity pacing, sleep hygiene, pain perception, disability, mood, fatigue [9] and catastrophization[8]. Recent clinical trials and integrative reviews found 6-10 weeks of CBT had positive effects on pain intensity but further research is need to identify optimal dosage[8][9]
Cognitive behavioral therapy (CBT) can help people with chronic pain to improve their physical function by:
- Setting realistic goals: CBT can help people to set realistic goals for their activity level, such as walking for 30 minutes a day or doing some light stretching exercises. This can help people to gradually increase their activity level and to overcome fear of movement.
- Developing coping strategies: CBT can help people to develop strategies for managing pain during activity, such as using relaxation techniques or distraction techniques. This can help people to stay active and to avoid becoming more disabled by their pain.
The role of the physiotherapist in CBT[edit | edit source]
Physiotherapists can play a key role in the delivery of CBT for pain management. They can:
- Provide education about pain: Physiotherapists can educate people about the nature of pain and how it can affect their physical function. This can help people to understand their pain and to develop realistic expectations for their recovery.
- Teach relaxation techniques: Physiotherapists can teach people relaxation techniques, such as deep breathing or progressive muscle relaxation. These techniques can help people to manage pain and to reduce stress, which can also improve physical function.
- Help people to develop coping strategies: Physiotherapists can help people to develop coping strategies for managing pain during activity. This can include teaching people how to use relaxation techniques, distraction techniques, or other strategies that have been found to be helpful.
Effectiveness of CBT for pain management[edit | edit source]
There is a growing body of evidence to support the effectiveness of CBT for pain management. A systematic review of 60 randomized controlled trials found that CBT was effective in reducing pain intensity, improving function, and reducing disability in people with chronic pain.[10]
Limitations of CBT for pain management[edit | edit source]
CBT is not a miracle cure for pain, and it is not effective for everyone. However, it is a safe and effective treatment option for many people with chronic pain. Some of the limitations of CBT include:
- It can be time-consuming and expensive.
- It requires a motivated and committed patient.
- It may not be effective for all types of pain.[11]
Overall, CBT is a safe and effective treatment option for many people with chronic pain. It can help to reduce pain intensity, improve function, and reduce disability[12]. Physiotherapists can play a key role in the delivery of CBT for pain management by providing education, teaching relaxation techniques, and helping people to develop coping strategies.
References[edit | edit source]
- ↑ 1.0 1.1 Beck, J., 1995. Cognitive Therapy: Basics and Beyond. Guildford Press: New York
- ↑ NHS Choices, 2012. Cognitive behavioural therapy. [online] Available at:http://www.nhs.uk/conditions/cognitive-behavioural-therapy/Pages/Introduction.aspx[Accessed 8th Jan 2014]
- ↑ Öst, L.G., 2008. Efficacy of the third wave of behavioral therapies: a systematic review and meta-analysis. Behaviour research and therapy, 46(3): 296–321
- ↑ Hayes, S.C., 2004. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy, 35: 639–665
- ↑ Roth, A., Fonagy, P. “What works for whom? A critical review of psychotherapy research”. 2nd ed. Guilford Press: New York 2005
- ↑ 6.0 6.1 Beck, A.T., 1976. Cognitive Therapy and the Emotional Disorders. New York: International Universities Press
- ↑ Wenzel A. Basic Strategies of Cognitive Behavioral Therapy. Psychiatr Clin North Am. 2017 Dec;40(4):597-609. doi: 10.1016/j.psc.2017.07.001. Epub 2017 Aug 18.
- ↑ 8.0 8.1 8.2 Knoerl, R., Lavoie Smith, E. M. and Weisberg, J. (2016) ‘Chronic Pain and Cognitive Behavioral Therapy: An Integrative Review’, Western Journal of Nursing Research, 38(5), pp. 596–628. doi: 10.1177/0193945915615869.
- ↑ 9.0 9.1 Chong HY, McNamee P, Bachmair EM, Martin K, Aucott L, Dhaun N, Dures E, Emsley R, Gray SR, Kidd E, Kumar V. Cost-effectiveness of cognitive behavioural and personalised exercise interventions for reducing fatigue in inflammatory rheumatic diseases. Rheumatology. 2023 Feb 27.
- ↑ Morley, S., Williams, A., & Eccleston, C. (1999). Systematic review and meta-analysis of randomised controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults. Pain, 80(3), 159-169.
- ↑ Eccleston, C., Crombez, G., & Williams, A. (2006). Psychological therapies for chronic pain. The Cochrane Database of Systematic Reviews, 3, CD003968.
- ↑ Morley, S. (2010). Cognitive behaviour therapy for chronic pain: A guide for practitioners. London: Routledge