Cognitive Behavioural Therapy: Difference between revisions
(Updated how it is used section) |
(REVIEW , content AND UP-TO-DATE REFERENCE) |
||
| Line 10: | Line 10: | ||
Cognitive Behavioural Therapy (CBT) is a method that can help manage problems by changing the way patients would think and behave. It is not designed to remove any problems but help manage them in a positive manner <ref name="Beck 1995">Beck, J., 1995. Cognitive Therapy: Basics and Beyond. Guildford Press: New York</ref> <ref name="NHS Choices 2012">NHS Choices, 2012. Cognitive behavioural therapy. [online] Available at:http://www.nhs.uk/conditions/cognitive-behavioural-therapy/Pages/Introduction.aspx[Accessed 8th Jan 2014]</ref>. | Cognitive Behavioural Therapy (CBT) is a method that can help manage problems by changing the way patients would think and behave. It is not designed to remove any problems but help manage them in a positive manner <ref name="Beck 1995">Beck, J., 1995. Cognitive Therapy: Basics and Beyond. Guildford Press: New York</ref> <ref name="NHS Choices 2012">NHS Choices, 2012. Cognitive behavioural therapy. [online] Available at:http://www.nhs.uk/conditions/cognitive-behavioural-therapy/Pages/Introduction.aspx[Accessed 8th Jan 2014]</ref>. | ||
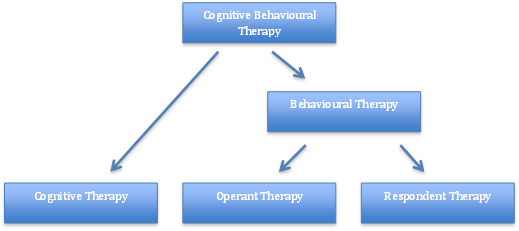
Behaviour therapy (BT) was developed in the 1950’s independently in three countries: South Africa, USA and England <ref name="Ost 2008">Öst, L.G., 2008. Efficacy of the third wave of behavioral therapies: a systematic review and meta-analysis. Behaviour research and therapy, 46(3): 296–321</ref>. It was further developed to Cognitive Therapy (CT) in the 1970’s by Dr Aaron Beck with its main application on people with [[depression]], anxiety and eating disorders <ref name="Beck 1995" /> | Behaviour therapy (BT) was developed in the 1950’s independently in three countries: South Africa, USA and England <ref name="Ost 2008">Öst, L.G., 2008. Efficacy of the third wave of behavioral therapies: a systematic review and meta-analysis. Behaviour research and therapy, 46(3): 296–321</ref>. It was further developed to Cognitive Therapy (CT) in the 1970’s by Dr Aaron Beck with its main application on people with [[depression]], anxiety and eating disorders <ref name="Beck 1995" /><ref name="Hayes 2004">Hayes, S.C., 2004. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy, 35: 639–665</ref>. However, the main evidence today focuses on CBT, after the merging of BT and CT in the late 80’s <ref name="Roth 2005">Roth, A., Fonagy, P. “What works for whom? A critical review of psychotherapy research”. 2nd ed. Guilford Press: New York 2005</ref>.<br> | ||
<br> | <br> | ||
| Line 33: | Line 33: | ||
===CBT and Chronic Pain=== | ===CBT and Chronic Pain=== | ||
CBT has been increasingly studied and considered as an intervention as part of a multimodal approach for those with chronic pain. CBT has been studied to address activity pacing, sleep hygiene, pain perception, disability, mood, and catastrophization<ref name=":0" />. Recent clinical trials and integrative reviews found 6-10 weeks of CBT had positive effects on pain intensity but further research is need to identify optimal dosage<ref name=":0" /> | CBT has been increasingly studied and considered as an intervention as part of a multimodal approach for those with chronic pain. CBT has been studied to address activity pacing, sleep hygiene, pain perception, disability, mood, fatigue <ref name=":1">Chong HY, McNamee P, Bachmair EM, Martin K, Aucott L, Dhaun N, Dures E, Emsley R, Gray SR, Kidd E, Kumar V. Cost-effectiveness of cognitive behavioural and personalised exercise interventions for reducing fatigue in inflammatory rheumatic diseases. Rheumatology. 2023 Feb 27.</ref> and catastrophization<ref name=":0" />. Recent clinical trials and integrative reviews found 6-10 weeks of CBT had positive effects on pain intensity but further research is need to identify optimal dosage<ref name=":0" /><ref name=":1" /><br> | ||
<br> | |||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 15:47, 18 July 2023
Original Editor - Rachael Lowe
Top Contributors - Scott Buxton, Kim Jackson, Anthonia Abraham, Vidya Acharya, Patti Cavaleri, Shaimaa Eldib, Rachael Lowe, Mariam Hashem, WikiSysop and Claire Knott
What is Cognitive Behavioural Therapy?[edit | edit source]
Cognitive Behavioural Therapy (CBT) is a method that can help manage problems by changing the way patients would think and behave. It is not designed to remove any problems but help manage them in a positive manner [1] [2].
Behaviour therapy (BT) was developed in the 1950’s independently in three countries: South Africa, USA and England [3]. It was further developed to Cognitive Therapy (CT) in the 1970’s by Dr Aaron Beck with its main application on people with depression, anxiety and eating disorders [1][4]. However, the main evidence today focuses on CBT, after the merging of BT and CT in the late 80’s [5].
Fig.2 - Breakdown of CBT theory
The Cognitive Behavioural Therapy Model[edit | edit source]
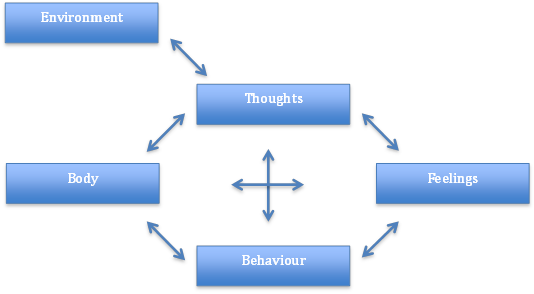
Fig.3 - Factors involved within the Cognitive Behavioural Therapy Model
Aaron Beck and Christine Padesky first recognised this CBT model in the 1970s [6].
How it is Used[edit | edit source]
Negative thoughts (e.g., "My back pain is uncontrollable" --> Negative feelings (e.g., depression, anger) and maladaptive health behaviours (e.g., skipping treatment sessions) --> Reinforcing negative cycle.
If one negative thought can be changed or better understood, then it can break down this negative cycle. This can be addressed through education and methods to manage symptoms [6]. This is address through various approaches including cognitive restructuring, behavior activation, exposure, and problem-solving strategies[7].
CBT can be delivered through individualized sessions or group sessions. A recent integrative review found that online formats of CBT may be comparable with traditional formats[8].
CBT and Chronic Pain[edit | edit source]
CBT has been increasingly studied and considered as an intervention as part of a multimodal approach for those with chronic pain. CBT has been studied to address activity pacing, sleep hygiene, pain perception, disability, mood, fatigue [9] and catastrophization[8]. Recent clinical trials and integrative reviews found 6-10 weeks of CBT had positive effects on pain intensity but further research is need to identify optimal dosage[8][9]
References[edit | edit source]
- ↑ 1.0 1.1 Beck, J., 1995. Cognitive Therapy: Basics and Beyond. Guildford Press: New York
- ↑ NHS Choices, 2012. Cognitive behavioural therapy. [online] Available at:http://www.nhs.uk/conditions/cognitive-behavioural-therapy/Pages/Introduction.aspx[Accessed 8th Jan 2014]
- ↑ Öst, L.G., 2008. Efficacy of the third wave of behavioral therapies: a systematic review and meta-analysis. Behaviour research and therapy, 46(3): 296–321
- ↑ Hayes, S.C., 2004. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy, 35: 639–665
- ↑ Roth, A., Fonagy, P. “What works for whom? A critical review of psychotherapy research”. 2nd ed. Guilford Press: New York 2005
- ↑ 6.0 6.1 Beck, A.T., 1976. Cognitive Therapy and the Emotional Disorders. New York: International Universities Press
- ↑ Wenzel A. Basic Strategies of Cognitive Behavioral Therapy. Psychiatr Clin North Am. 2017 Dec;40(4):597-609. doi: 10.1016/j.psc.2017.07.001. Epub 2017 Aug 18.
- ↑ 8.0 8.1 8.2 Knoerl, R., Lavoie Smith, E. M. and Weisberg, J. (2016) ‘Chronic Pain and Cognitive Behavioral Therapy: An Integrative Review’, Western Journal of Nursing Research, 38(5), pp. 596–628. doi: 10.1177/0193945915615869.
- ↑ 9.0 9.1 Chong HY, McNamee P, Bachmair EM, Martin K, Aucott L, Dhaun N, Dures E, Emsley R, Gray SR, Kidd E, Kumar V. Cost-effectiveness of cognitive behavioural and personalised exercise interventions for reducing fatigue in inflammatory rheumatic diseases. Rheumatology. 2023 Feb 27.