Cervical Spondylosis: Difference between revisions
Rachael Lowe (talk | contribs) mNo edit summary |
Rachael Lowe (talk | contribs) mNo edit summary |
||
| Line 6: | Line 6: | ||
== Definition/Description == | == Definition/Description == | ||
The term spondylosis is used to define a generalised natural ageing process that involves a sequence of degenerative changes in spinal structure.<ref name=":8">Ferrara LA. [[The biomechanics of cervical spondylosis.]] Advances in orthopedics. 2012 Feb 1;2012.</ref><ref name=":9">Moon MS, Yoon MG, Park BK, Park MS. A[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5081320/ ge-Related Incidence of Cervical Spondylosis in Residents of Jeju Island]. Asian spine journal. 2016 Oct 1;10(5):857-68.</ref> In the cervical spine this chronic degenerative process affects the intervertebral discs and facet joints, and may progress to disk herniation, osteophyte formation, vertebral body degeneration, compression of the spinal cord, or cervical spondylotic myelopathy<ref>Xiong W, Li F, Guan H. [[Tetraplegia after thyroidectomy in a patient with cervical spondylosis: a case report and literature review.]] Medicine (Baltimore) 2015;94(6):e524.</ref>. It has been defined as vertebral osteophytosis secondary to degenerative disc disease due to the osteophytic formations that occur with progressive spinal segment degeneration<ref name=":8" />. Therm term is often used synonymously with [[Cervical Osteoarthritis]]. | |||
= | Although ageing is the primary cause<ref name=":8" />, the location and rate of degeneration as well as degree of symptoms and functional disturbance varies and is unique to the individual. | ||
== Clinically Relevant Anatomy == | |||
The cervical spine is made up of seven segments and is highly mobile. <ref>Boek R. Putz, R. Pabst. Sobotta, Atlas of Human Anatomy Volume 1: Head, Neck, Upper Limb.2006.Elsevier.</ref> It performs 3 important functions; it forms the structural support for the head, protects the cervical spine cord and the exiting nerve roots enclosed within it. <ref>Ippei Takagi, Cervical Spondylosis: An Update on Pathophysiology, Clinical Manifestation, and Management Strategies. DM, October 2011</ref> There is an important distinction between the high and mid cervical regions and the lower cervical region. The first two vertebrae, the atlas and axis, are anatomically and functionally different segments. The atlas is a uniquely shaped ring without a vertebral body, it articulates with the skull at the atlanto-occipital joint and allows for approximately 50% of the flexion and extension movements of the neck. It pivots on the odontoid process of the axis, which arises from the superior surface of the latter’s body. The atlanto-axial joint is responsible for approximately 50% of the rotational movement in the neck. There is no intervertebral disc between C0-C1 and C1-C2. The lower five cervical vertebrae are roughly cylindrical in shape with bony projections <ref name=":0">McCormack B M, Weinstein P R, Cervical Spondylosis. An update. Western Journal of Medicine, Jul-Aug 1996</ref>. The intervertebral discs act as shock absorbers, stabilisers and allow the spine to be flexible. <br> | The cervical spine is made up of seven segments and is highly mobile. <ref>Boek R. Putz, R. Pabst. Sobotta, Atlas of Human Anatomy Volume 1: Head, Neck, Upper Limb.2006.Elsevier.</ref> It performs 3 important functions; it forms the structural support for the head, protects the cervical spine cord and the exiting nerve roots enclosed within it. <ref>Ippei Takagi, Cervical Spondylosis: An Update on Pathophysiology, Clinical Manifestation, and Management Strategies. DM, October 2011</ref> There is an important distinction between the high and mid cervical regions and the lower cervical region. The first two vertebrae, the atlas and axis, are anatomically and functionally different segments. The atlas is a uniquely shaped ring without a vertebral body, it articulates with the skull at the atlanto-occipital joint and allows for approximately 50% of the flexion and extension movements of the neck. It pivots on the odontoid process of the axis, which arises from the superior surface of the latter’s body. The atlanto-axial joint is responsible for approximately 50% of the rotational movement in the neck. There is no intervertebral disc between C0-C1 and C1-C2. The lower five cervical vertebrae are roughly cylindrical in shape with bony projections <ref name=":0">McCormack B M, Weinstein P R, Cervical Spondylosis. An update. Western Journal of Medicine, Jul-Aug 1996</ref>. The intervertebral discs act as shock absorbers, stabilisers and allow the spine to be flexible. <br> | ||
| Line 18: | Line 19: | ||
*Posterior: All the structures that are posteriorly positioned compared to the longitudinal posterior ligament. | *Posterior: All the structures that are posteriorly positioned compared to the longitudinal posterior ligament. | ||
== Epidemiology == | == Epidemiology == | ||
The prevalence of cervical spondylosis is similar for both sexes, although the degree of severity is greater for males.<ref>D.H. Irvine, J.B. Foster, Prevalence of cervical spondylosis in a general practice, The Lancet, May 22 1965</ref> <ref>Sandeep S Rana, MD, Diagnosis and Management of Cervical Spondylosis. Medscape, 2015</ref> Approximately 95% of people by the age of 65 will have a degree of cervical spondylosis, the most prevalent spine dysfunction in elderly people. It has been estimated that 75% of persons over the age of 50 have a narrowing of the spinal canal or intervertebral foramina, and 50% of these cases are symptomatic.By age 65 that incidence increases to 75%.<ref>HUBERT L. ROSOMOFF, FERDINAND ROSSMANN, Treatment of Cervical Spondylosis by Anterior Cervical Diskectomy and Fusion, Archives of neurology, 1966</ref> Spondylotic changes in the cervical spine occur at singular disc space levels in 15-40% of patients and at multiple levels in 60-85%. The discs between the 3rd and 7th cervical vertebrae are most commonly affected. | The prevalence of cervical spondylosis is similar for both sexes, although the degree of severity is greater for males.<ref>D.H. Irvine, J.B. Foster, Prevalence of cervical spondylosis in a general practice, The Lancet, May 22 1965</ref> <ref>Sandeep S Rana, MD, Diagnosis and Management of Cervical Spondylosis. Medscape, 2015</ref> Approximately 95% of people by the age of 65 will have a degree of cervical spondylosis, the most prevalent spine dysfunction in elderly people. It has been estimated that 75% of persons over the age of 50 have a narrowing of the spinal canal or intervertebral foramina, and 50% of these cases are symptomatic. By age 65 that incidence increases to 75%.<ref>HUBERT L. ROSOMOFF, FERDINAND ROSSMANN, Treatment of Cervical Spondylosis by Anterior Cervical Diskectomy and Fusion, Archives of neurology, 1966</ref> Spondylotic changes in the cervical spine occur at singular disc space levels in 15-40% of patients and at multiple levels in 60-85%. The discs between the 3rd and 7th cervical vertebrae are most commonly affected. | ||
Although ageing is the major risk factor that contributes to the onset of cervical spondylosis<ref name=":8" />, repeated occupational trauma may contribute to the development of cervical spondylosis. An increased incidence has been noted in patients who carried heavy loads on their heads or shoulders, dancers, gymnasts, and in patients with spasmodic torticollis, although this cause is not widely accepted. In about 10% of patients, cervical spondylosis is due to congenital bony anomalies, blocked vertebrae, malformed laminae that place undue stress on adjacent intervertebral discs.<ref name="update" /> | Although ageing is the major risk factor that contributes to the onset of cervical spondylosis<ref name=":8" />, repeated occupational trauma may contribute to the development of cervical spondylosis<ref name=":9" />. An increased incidence has been noted in patients who carried heavy loads on their heads or shoulders, dancers, gymnasts, and in patients with spasmodic torticollis, although this cause is not widely accepted. In about 10% of patients, cervical spondylosis is due to congenital bony anomalies, blocked vertebrae, malformed laminae that place undue stress on adjacent intervertebral discs.<ref name="update" /> | ||
== Etiology == | == Etiology == | ||
Ferrara<ref name=":8" /> describes the process | Ferrara<ref name=":8" /> describes the process of cervical spondylosis as follows: | ||
"Early spondylosis is associated with degenerative changes within the intervertebral disc where desiccation of the disc occurs, thus causing overall disc height loss and a reduction in the ability of the disc to maintain or bear additional axial loads along the cervical spine..... Once the disc starts to degenerate and a loss in disc height occurs, the soft tissue (ligamentous and disc) becomes lax, resulting in ventral and/or dorsal margin disc bulge and buckling of the ligaments surrounding the spinal segment, accompanied by a reduction in the structural and mechanical integrity of the supportive soft tissues across a cervical segment. As the ventral column becomes compromised, there is greater transfer of the axial loads to the uncovertebral joints and also along the dorsal column, resulting in greater loads borne by the facet joints. As axial loads are redistributed to a greater extent along the dorsal column of the cervical spine, the facet joints are excessively loaded resulting in hypertrophic facets with possible long-term ossification of the posterior longitudinal ligament. When the load balance of the cervical spine is altered and disrupted, as is the situation with cervical degeneration, the remaining functional and supportive structures along the cervical spinal column will absorb the added stress that is transferred to the surrounding structures and adjacent levels along the spine. Eventually these structures will also be excessively loaded, resulting in a cascade of events of further degeneration and tissue adaptation. Overloading the soft tissues and bone eventually causes osteophytes to form in response to excessive loading in order to compensate for greater stresses to the surrounding bone and soft tissue" | "Early spondylosis is associated with degenerative changes within the intervertebral disc where desiccation of the disc occurs, thus causing overall disc height loss and a reduction in the ability of the disc to maintain or bear additional axial loads along the cervical spine..... Once the disc starts to degenerate and a loss in disc height occurs, the soft tissue (ligamentous and disc) becomes lax, resulting in ventral and/or dorsal margin disc bulge and buckling of the ligaments surrounding the spinal segment, accompanied by a reduction in the structural and mechanical integrity of the supportive soft tissues across a cervical segment. As the ventral column becomes compromised, there is greater transfer of the axial loads to the uncovertebral joints and also along the dorsal column, resulting in greater loads borne by the facet joints. As axial loads are redistributed to a greater extent along the dorsal column of the cervical spine, the facet joints are excessively loaded resulting in hypertrophic facets with possible long-term ossification of the posterior longitudinal ligament. When the load balance of the cervical spine is altered and disrupted, as is the situation with cervical degeneration, the remaining functional and supportive structures along the cervical spinal column will absorb the added stress that is transferred to the surrounding structures and adjacent levels along the spine. Eventually these structures will also be excessively loaded, resulting in a cascade of events of further degeneration and tissue adaptation. Overloading the soft tissues and bone eventually causes osteophytes to form in response to excessive loading in order to compensate for greater stresses to the surrounding bone and soft tissue" | ||
Possible characteristics | Possible degenerative characteristics include: | ||
*[[Degenerative Disc Disease]] | *[[Degenerative Disc Disease]] | ||
*Formation of osteophytes | *Formation of osteophytes | ||
*Facet and uncovertebral joint | *Facet and uncovertebral joint degeneration | ||
*Ossification of the posterior longitudinal ligament | *Ossification of the posterior longitudinal ligament | ||
*Hypertrophy of the ligamentum flavum causing posterior compression of the cord especially as it buckles in extension | *Hypertrophy of the ligamentum flavum causing posterior compression of the cord especially as it buckles in extension | ||
*[[Spinal Stenosis|Spinal stenosis]] | *[[Spinal Stenosis|Spinal stenosis]] | ||
*Degenerative subluxation of cervical vertebra | *Degenerative subluxation of cervical vertebra | ||
*Dislocated fragment of annular cartilage compressing the spinal cord or nerve root <ref>Torrens M, Cervical Spondylosis Part 1: Pathogenesis, Diagnosis and Management Options</ref> < | *Dislocated fragment of annular cartilage compressing the spinal cord or nerve root <ref>Torrens M, Cervical Spondylosis Part 1: Pathogenesis, Diagnosis and Management Options</ref> | ||
*Neural and vascular compression<ref name=":8" /> | |||
In some cases this degeneration also leads to a posterior protrusion of the annulus fibres of the intervertebral disc, causing compression of the nerve roots, pain, motor disturbances such as muscle weakness, and sensory disturbances. As the spondylosis progresses there may even be interference with the blood supply to the spinal cord where the vertebral canal is at its most narrow. | In some cases this degeneration also leads to a posterior protrusion of the annulus fibres of the intervertebral disc, causing compression of the nerve roots, pain, motor disturbances such as muscle weakness, and sensory disturbances. As the spondylosis progresses there may even be interference with the blood supply to the spinal cord where the vertebral canal is at its most narrow. | ||
== Clinical Presentation == | == Clinical Presentation == | ||
Cervical spondylosis can presents in three symptomatic forms as: | Cervical spondylosis can presents in three symptomatic forms as: | ||
# | # Non specific neck pain | ||
# [[Cervical Radiculopathy|Cervical radiculopathy]] | # [[Cervical Radiculopathy|Cervical radiculopathy]] | ||
# [[Cervical Myelopathy|Cervical myelopathy]]<ref>Emery SE. Cervical spondylotic myelopathy: diagnosis and treatment. J Am Acad Orthop Surg. Nov-Dec 2001;9(6):376-88. (Level: A1)</ref><ref name="Rahim">Rahim KA, Stambough JL. Radiographic evaluation of the degenerative cervical spine. Orthop Clin North Am. Jul 1992;23(3):395-403.</ref><ref>Heller JG. The syndromes of degenerative cervical disease. Orthop Clin North Am. Jul 1992;23(3):381-94. (Level: A1)</ref> | # [[Cervical Myelopathy|Cervical myelopathy]]<ref>Emery SE. Cervical spondylotic myelopathy: diagnosis and treatment. J Am Acad Orthop Surg. Nov-Dec 2001;9(6):376-88. (Level: A1)</ref><ref name="Rahim">Rahim KA, Stambough JL. Radiographic evaluation of the degenerative cervical spine. Orthop Clin North Am. Jul 1992;23(3):395-403.</ref><ref>Heller JG. The syndromes of degenerative cervical disease. Orthop Clin North Am. Jul 1992;23(3):381-94. (Level: A1)</ref> | ||
Symptoms can depend on the stage of the pathological process and the site of neural compression | Symptoms can depend on the stage of the pathological process and the site of neural compression. Diagnostic imaging may show spondylosis, but the patient may be asymptomatic<ref>Takagi I, Cervical Spondylosis: An Update on Pathophysiology, Clinical Manifestation, and Management Strategies. DM, October 2011</ref> and vice versa. Many people over 30 show similar abnormalities on plain radiographs of the cervical spine, so the boundary between normal ageing and disease is difficult to define<ref>Binder AI. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1819511/ Cervical spondylosis and neck pain]. BMJ: British Medical Journal. 2007 Mar 10;334(7592):527.</ref>. | ||
Pain is the most commonly reported symptom. McCormack et al <ref name="update">McCormack BM, Weinstein PR. Cervical spondylosis. An update. West J Med. Jul-Aug 1996;165(1-2):43-51. </ref> reported that intermittent neck and shoulder pain is the most common syndrome seen in clinical practice. With [[Cervical Radiculopathy|cervical radiculopathy]] the pain most often occurs in the cervical region, the upper limb, shoulder, and/or interscapular region <ref>Ellenberg MR, Honet JC, Treanor WJ. Cervical radiculopathy. Arch Phys Med Rehabil. Mar 1994;75(3):342-52</ref>. In some cases the pain may be atypical and manifest as chest or breast pain, although it is most frequently present in the upper limbs and the neck. Chronic suboccipital headache could also be a clinical syndrome in patients with cervical spondylosis <ref>Heller JG. The syndromes of degenerative cervical disease. Orthop Clin North Am. Jul 1992;23(3):381-94. (Level: A1)</ref> , which may radiate to the base of the neck and the vertex of the skull. | |||
Paraesthesia or muscle weakness, or a combination of these are often reported and indicate radiculopathy. | |||
Central cord syndrome may also be seen in relation to cervical spondylosis and in some cases dysphagia or airway dysfunction have been reported. <ref>Kaye JJ, Dunn AW. Cervical spondylotic dysphagia. South Med J. May 1977;70(5):613-4. (Level: A1)</ref><ref>Kanbay M, Selcuk H, Yilmaz U. Dysphagia caused by cervical osteophytes: a rare case. J Am Geriatr Soc. Jul 2006;54(7):1147-8. (Level: C)</ref> | |||
== Differential Diagnosis<ref>Binder AI. Cervical spondylosis and neck pain: clinical review. BMJ 2007:334:527-31 </ref> == | == Differential Diagnosis<ref>Binder AI. Cervical spondylosis and neck pain: clinical review. BMJ 2007:334:527-31 </ref> == | ||
| Line 215: | Line 223: | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Cervical Spondylosis is a degenerative disorder | Cervical Spondylosis is a normal degenerative disorder of the cervical spine. Whether spondylosis should be considered a degenerative change or an age related change is simply a matter of semantics. But the development of osteophytes can be viewed as a reactive and adaptive change that seeks to compensate for biomechanical aberrations. | ||
It can be described as the result of degeneration of the intervertebral discs or the corpus vertebrae in the cervical region. It is the most common cause of non-traumatic myelopathy, resulting in paraparesis and quadriparesis. The incidence of neck pain in adults is approximately 20-50% per year, much of which is caused by spondylosis. Approximately 95% of people by age 65 have cervical spondylosis to some degree, it’s the most common spine dysfunction in elderly people. The symptoms can depend on the stage of the pathologic process and the site of neural compression. On imaging studies you can see that there is a spondylosis, but the patient can’t have any symptoms at all. Most of the time cervical spondylosis is diagnosed on clinical signs and symptoms alone. C. Xu et al found that MRI can reliably determine the presence or degree of facet tropism, but not facet arthrosis. Therefor, it is advisable to augment CT with MRI for an accurate diagnosis. Surgical intervention is only in rare cases required, it should be chosen with great care. The treatment should be tailored to individual patients but includes supervised isometric exercises, proprioceptive reeducation, manual therapy and posture education. | |||
== References == | == References == | ||
Revision as of 14:46, 2 September 2017
Original Editors - Gertjan Peeters
Top Contributors - Bruno Luca, Rachael Lowe, Jolien Wauters, Scott Cornish, Gertjan Peeters, Deborah Huart, Garima Gedamkar, Kim Jackson, Admin, Lucinda hampton, Tony Lowe, Simisola Ajeyalemi, Aline Tréfois, Rucha Gadgil, Jess Bell and Olajumoke Ogunleye
Definition/Description[edit | edit source]
The term spondylosis is used to define a generalised natural ageing process that involves a sequence of degenerative changes in spinal structure.[1][2] In the cervical spine this chronic degenerative process affects the intervertebral discs and facet joints, and may progress to disk herniation, osteophyte formation, vertebral body degeneration, compression of the spinal cord, or cervical spondylotic myelopathy[3]. It has been defined as vertebral osteophytosis secondary to degenerative disc disease due to the osteophytic formations that occur with progressive spinal segment degeneration[1]. Therm term is often used synonymously with Cervical Osteoarthritis.
Although ageing is the primary cause[1], the location and rate of degeneration as well as degree of symptoms and functional disturbance varies and is unique to the individual.
Clinically Relevant Anatomy[edit | edit source]
The cervical spine is made up of seven segments and is highly mobile. [4] It performs 3 important functions; it forms the structural support for the head, protects the cervical spine cord and the exiting nerve roots enclosed within it. [5] There is an important distinction between the high and mid cervical regions and the lower cervical region. The first two vertebrae, the atlas and axis, are anatomically and functionally different segments. The atlas is a uniquely shaped ring without a vertebral body, it articulates with the skull at the atlanto-occipital joint and allows for approximately 50% of the flexion and extension movements of the neck. It pivots on the odontoid process of the axis, which arises from the superior surface of the latter’s body. The atlanto-axial joint is responsible for approximately 50% of the rotational movement in the neck. There is no intervertebral disc between C0-C1 and C1-C2. The lower five cervical vertebrae are roughly cylindrical in shape with bony projections [6]. The intervertebral discs act as shock absorbers, stabilisers and allow the spine to be flexible.
The sides of the vertebrae are linked by small facet joints. Strong ligaments attach to adjacent vertebrae to give extra support and strength. The cervical spine can be split into three columns; anterior, middle and posterior: [6]
- Anterior: consists of the longitudinal anterior ligament , the annulus of the disc and the anterior part of the corpus vertebrae
- Middle: consists of the longitudinal posteriorligament , the posterior part of the annulus and the corpus vertebrae.
- Posterior: All the structures that are posteriorly positioned compared to the longitudinal posterior ligament.
Epidemiology[edit | edit source]
The prevalence of cervical spondylosis is similar for both sexes, although the degree of severity is greater for males.[7] [8] Approximately 95% of people by the age of 65 will have a degree of cervical spondylosis, the most prevalent spine dysfunction in elderly people. It has been estimated that 75% of persons over the age of 50 have a narrowing of the spinal canal or intervertebral foramina, and 50% of these cases are symptomatic. By age 65 that incidence increases to 75%.[9] Spondylotic changes in the cervical spine occur at singular disc space levels in 15-40% of patients and at multiple levels in 60-85%. The discs between the 3rd and 7th cervical vertebrae are most commonly affected.
Although ageing is the major risk factor that contributes to the onset of cervical spondylosis[1], repeated occupational trauma may contribute to the development of cervical spondylosis[2]. An increased incidence has been noted in patients who carried heavy loads on their heads or shoulders, dancers, gymnasts, and in patients with spasmodic torticollis, although this cause is not widely accepted. In about 10% of patients, cervical spondylosis is due to congenital bony anomalies, blocked vertebrae, malformed laminae that place undue stress on adjacent intervertebral discs.[10]
Etiology[edit | edit source]
Ferrara[1] describes the process of cervical spondylosis as follows:
"Early spondylosis is associated with degenerative changes within the intervertebral disc where desiccation of the disc occurs, thus causing overall disc height loss and a reduction in the ability of the disc to maintain or bear additional axial loads along the cervical spine..... Once the disc starts to degenerate and a loss in disc height occurs, the soft tissue (ligamentous and disc) becomes lax, resulting in ventral and/or dorsal margin disc bulge and buckling of the ligaments surrounding the spinal segment, accompanied by a reduction in the structural and mechanical integrity of the supportive soft tissues across a cervical segment. As the ventral column becomes compromised, there is greater transfer of the axial loads to the uncovertebral joints and also along the dorsal column, resulting in greater loads borne by the facet joints. As axial loads are redistributed to a greater extent along the dorsal column of the cervical spine, the facet joints are excessively loaded resulting in hypertrophic facets with possible long-term ossification of the posterior longitudinal ligament. When the load balance of the cervical spine is altered and disrupted, as is the situation with cervical degeneration, the remaining functional and supportive structures along the cervical spinal column will absorb the added stress that is transferred to the surrounding structures and adjacent levels along the spine. Eventually these structures will also be excessively loaded, resulting in a cascade of events of further degeneration and tissue adaptation. Overloading the soft tissues and bone eventually causes osteophytes to form in response to excessive loading in order to compensate for greater stresses to the surrounding bone and soft tissue"
Possible degenerative characteristics include:
- Degenerative Disc Disease
- Formation of osteophytes
- Facet and uncovertebral joint degeneration
- Ossification of the posterior longitudinal ligament
- Hypertrophy of the ligamentum flavum causing posterior compression of the cord especially as it buckles in extension
- Spinal stenosis
- Degenerative subluxation of cervical vertebra
- Dislocated fragment of annular cartilage compressing the spinal cord or nerve root [11]
- Neural and vascular compression[1]
In some cases this degeneration also leads to a posterior protrusion of the annulus fibres of the intervertebral disc, causing compression of the nerve roots, pain, motor disturbances such as muscle weakness, and sensory disturbances. As the spondylosis progresses there may even be interference with the blood supply to the spinal cord where the vertebral canal is at its most narrow.
Clinical Presentation[edit | edit source]
Cervical spondylosis can presents in three symptomatic forms as:
- Non specific neck pain
- Cervical radiculopathy
- Cervical myelopathy[12][13][14]
Symptoms can depend on the stage of the pathological process and the site of neural compression. Diagnostic imaging may show spondylosis, but the patient may be asymptomatic[15] and vice versa. Many people over 30 show similar abnormalities on plain radiographs of the cervical spine, so the boundary between normal ageing and disease is difficult to define[16].
Pain is the most commonly reported symptom. McCormack et al [10] reported that intermittent neck and shoulder pain is the most common syndrome seen in clinical practice. With cervical radiculopathy the pain most often occurs in the cervical region, the upper limb, shoulder, and/or interscapular region [17]. In some cases the pain may be atypical and manifest as chest or breast pain, although it is most frequently present in the upper limbs and the neck. Chronic suboccipital headache could also be a clinical syndrome in patients with cervical spondylosis [18] , which may radiate to the base of the neck and the vertex of the skull.
Paraesthesia or muscle weakness, or a combination of these are often reported and indicate radiculopathy.
Central cord syndrome may also be seen in relation to cervical spondylosis and in some cases dysphagia or airway dysfunction have been reported. [19][20]
Differential Diagnosis[21][edit | edit source]
- Other non-specific neck pain lesions - acute neck strain, postural neck ache or Whiplash, Fibromyalgia and psychogenic neck pain;
- Mechanical lesions - disc prolapse or diffuse idiopathic skeletal hyperostosis;
- Inflammatory disease - Rheumatoid arthritis, Ankylosing spondylitis or Polymyalgia rheumatica, Metabolic diseases - Paget's disease, osteoporosis, gout or pseudo-gout, Infections - osteomyelitis or tuberculosis, Malignancy - primary tumours, secundary deposits or myeloma;
- Adhesive Capsulitis in Physical Medicine and Rehabilitation;
- Brown-Sequard Syndrome;
- Carpal Tunnel Syndrome;
- Central Cord Syndrome;
- Cervical Disc Disease;
- Cervical Myofascial Pain;
- Cervical Sprain and Strain;
- Chronic Pain Syndrome;
- Diabetic Neuropathy;
- Multiple Sclerosis;
- Neoplastic Brachial Plexopathy;
- Osteoporosis and Spinal Cord Injury;
- Physical Medicine and Rehabilitation for Myofascial Pain;
- Radiation-Induced Brachial Plexopathy;
- Rheumatoid Arthritis;
- Traumatic Brachial Plexopathy. [22]
Diagnostic Procedures[edit | edit source]
Cervical spondylosis is often diagnosed on clinical signs and symptoms alone.
Signs:
- Poorly localised tenderness
- Limited range of motion, forward flexion, backward extension, lateral flexion, and rotation to both sides
- Minor neurological changes, such as inverted supinator jerks (unless complicated by myelopathy or radiculopathy.
Symptoms:
- Cervical pain aggravated by movement
- Referred pain
- Retro-orbital or temporal pain
- Cervical stiffness
- Vague numbness, tingling or weakness in upper limbs
- Dizzyness or vertigo
- Poor balance
- Rarely, syncope, triggers migraine. [22]
Diagnostic imaging such as X-ray, CT, MRI, and EMG can also be used to confirm a diagnosis. [23] C. Xu et al found that MRI can reliably determine the presence or degree of facet tropism, but not facet arthrosis. It is, therefore, advisable to augment CT with MRI for an accurate diagnosis. [24]
Outcomes Measures[edit | edit source]
Visual analogue scale (VAS)
Short Form 36 (SF-36)
Neck Disability Index (NDI). [25]
Spondylotic changes may result in direct compression and ischemic dysfunction of the spinal cord. [26] Several clinical measures of disease severity have been developed such as the Japanese Orthopaedic Association (JOA) and the Nurick Classification scoring systems. These popular scales have been developed to quantify the extent and progression of this disease.[27]
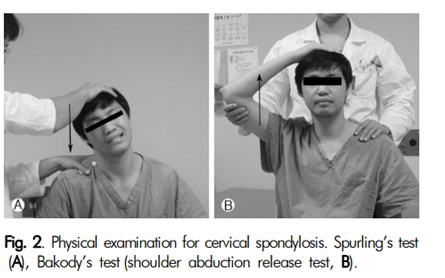
Test's such as Spurling’s test (A) and Bakody’s test (shoulder abduction release test B) can be used to differentiate between shoulder disorders and cervical spondylosis. [28]
Examination[edit | edit source]
Muscle atrophy is assessed on the affected side in the upper limb, shoulders and scapular regions and compared with the unaffected side. Muscle strength is tested in 4 muscles representing the myotomes C5-C8. Anterior, middle, and posterior parts of the deltoid muscle are tested by resisting flexion, abduction, and extension of the humerus. Strength of biceps brachii is assessed by resisted elbow flexion when the forearm is supinated. Triceps brachii muscle strength is tested by resisted elbow extension from 90 degrees of elbow flexion. The dorsal interosseus muscles are tested by resisting the separation of the 2nd through 5th fingers. Sensitivity to light touch and to pain are also tested for the relevant cervical dermatomes. [29]
Medical Management[30] [31][edit | edit source]
Cervical spondylosis is more often seen as a chronic condition, but in most cases it is not progressive and only in rare cases is surgery required. Initial management should be nonoperative. [32]
There are various medications used to treat cervical spondylosis:
- Non-Steroidal Anti-Inflammatory Drugs (NSAID’s) [32] although is an absence of clinical trials for the use of NSAIDs in the treatment of cervical spondylosis, but in theory they will reduce inflammation around the nerve, decreasing its sensitivity to compression.
- Opioid analgesics. The use of opoid analgesics has been limited/reduced because of the ineffectiveness in neuropathic pain, yet despite this, there is evidence that oxytocyne can be effective in the treatment of cervical spondylosis.
- Muscle relaxants. The use of muscle relaxants is effective for any associated spasm of the trapezius muscle, but the treatment duration is relative short, lasting for a maximum of two weeks.
- Corticosteroids [32] There is limited evidence to support the use of systemic corticosteroids in the treatment of cervical spondyolosis.
Poor prognostic indicators and absolute indications for surgery are:
- Progression of signs and symptoms;
- Presence of myelopathy for six months or longer;
- Compression ratio approaching 0,4 or transverse area of the spinal cord of 40mm squared or less. [33]
The goals of surgical treatment of cervical spondylosis are:
- Improvement or preservation of neurological function;
- Prevention or correction of spinal deformity;
- Maintenance of spinal stability. [33]
Decompression may be achieved using an anterior, a posterior, or a combined approach. Recommended decompression is anterior when there is anterior compression at one or two levels and no significant developmental narrowing of the canal. [33]
Anterior decompression, the different surgical options:[34]
- Anterior cervical foraminotomy
- Anterior cervical discectomy without fusion
- Anterior cervical discectomy with fusion
- Cervical arthroplasty
For compression at more than two levels, developmental narrowing of the canal, posterior compression, and ossification of the posterior longitudinal ligament, posterior decompression is recommended: Posterior laminoforaminotomy/foraminotomy and/or discectomy [34]
Physical Therapy Management[edit | edit source]
- There is little evidence for using exercise alone or mobilisation and/or manipulations alone.
- Mobilisation and/or manipulations in combination with exercises are effective for pain reduction and improvement in daily functioning in sub-acute or chronic mechanical neck pain with or without headache.
- There is moderate evidence that various exercise regimens, like proprioceptive, strengthening, endurance, or coordination exercises are more effective than usual care (analgesics, non-steroïdal anti-inflammatory drugs, or muscle relaxants) [35][36][37]
Typically, treatment requires 15–20 sessions over a 3-month period. The treatment should individualised, but generally includes isometric exercises, proprioceptive re-education, manual therapy and postural education. [38] [39]
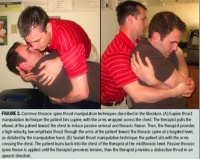
Manual therapy is defined as high-velocity; low-amplitude thrust manipulation or non-thrust manipulation.
Manual therapy of the thoracic spine will be used for reduction of pain, improving function, to increase the range of motion and to address the thoracic hypomobility [40]
Thrust manipulation of the thoracic spine could include techniques in a prone, supine, or sitting position based on therapist preference. Also cervical traction can be used as physical therapy to enlarge the neural foramen and reduce the neck stress [34]
Non-thrust manipulation included posterior-anterior (PA) glides in the prone position. The cervical spine techniques could include retractions, rotations, lateral glides in the ULTT1 position, and PA glides. The techniques are chosen based on patient response and centralisation or reduction of symptoms.[39]
Postural education includes the alignment of the spine during sitting and standing activities.[39]
Thermal therapy provides symptomatic relief only and ultrasound appears to be ineffective. Other methods such as infrared radiation, interferential therapy and massage can also be used in the treatment of cervical spondylosis. [41]
Soft tissue mobilisation was performed on the muscles of the upper quarter with the involved upper extremity positioned in abduction and external rotation to pre-load the neural structures of the upper limb.[41]
Home Exercices
Exercises include cervical retraction, cervical extension, deep cervical flexor strengthening, scapular strengthening, stretching of the chest muscles via isometric contraction of flexor of extensor muscles to encourage the mobility of the neural structures of the upper extremity.[40] [41]
|
cervical Retraction Exercise
|
The patient retracts their head as far as comfortably possible with head and eyes remaining on the same level. |
|
cervical extension exercises
|
The patient retracts the cervical spine, lifts the chin up, and extends the cervical spine to end range. Then 2-3 small right to left oscillations of the head are performed. The head is returned to the midline position, the chin tucked under and then return to the retracted position. |
|
Deep neck flexor exercises
|
The patient nods the head and flattens the spine without pushing the head back into the table, with minimal activation of the sternocleidomastoid muscle during the deep neck flexor contraction. |
|
Scapular strengthening exercises
|
Squeeze the shoulder blades together with or without resistance (seated or standing), without shrugging the shoulders (activating the upper trapezius muscle) during the exercise |
Clinical Bottom Line[edit | edit source]
Cervical Spondylosis is a normal degenerative disorder of the cervical spine. Whether spondylosis should be considered a degenerative change or an age related change is simply a matter of semantics. But the development of osteophytes can be viewed as a reactive and adaptive change that seeks to compensate for biomechanical aberrations.
It can be described as the result of degeneration of the intervertebral discs or the corpus vertebrae in the cervical region. It is the most common cause of non-traumatic myelopathy, resulting in paraparesis and quadriparesis. The incidence of neck pain in adults is approximately 20-50% per year, much of which is caused by spondylosis. Approximately 95% of people by age 65 have cervical spondylosis to some degree, it’s the most common spine dysfunction in elderly people. The symptoms can depend on the stage of the pathologic process and the site of neural compression. On imaging studies you can see that there is a spondylosis, but the patient can’t have any symptoms at all. Most of the time cervical spondylosis is diagnosed on clinical signs and symptoms alone. C. Xu et al found that MRI can reliably determine the presence or degree of facet tropism, but not facet arthrosis. Therefor, it is advisable to augment CT with MRI for an accurate diagnosis. Surgical intervention is only in rare cases required, it should be chosen with great care. The treatment should be tailored to individual patients but includes supervised isometric exercises, proprioceptive reeducation, manual therapy and posture education.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Ferrara LA. The biomechanics of cervical spondylosis. Advances in orthopedics. 2012 Feb 1;2012.
- ↑ 2.0 2.1 Moon MS, Yoon MG, Park BK, Park MS. Age-Related Incidence of Cervical Spondylosis in Residents of Jeju Island. Asian spine journal. 2016 Oct 1;10(5):857-68.
- ↑ Xiong W, Li F, Guan H. Tetraplegia after thyroidectomy in a patient with cervical spondylosis: a case report and literature review. Medicine (Baltimore) 2015;94(6):e524.
- ↑ Boek R. Putz, R. Pabst. Sobotta, Atlas of Human Anatomy Volume 1: Head, Neck, Upper Limb.2006.Elsevier.
- ↑ Ippei Takagi, Cervical Spondylosis: An Update on Pathophysiology, Clinical Manifestation, and Management Strategies. DM, October 2011
- ↑ 6.0 6.1 McCormack B M, Weinstein P R, Cervical Spondylosis. An update. Western Journal of Medicine, Jul-Aug 1996
- ↑ D.H. Irvine, J.B. Foster, Prevalence of cervical spondylosis in a general practice, The Lancet, May 22 1965
- ↑ Sandeep S Rana, MD, Diagnosis and Management of Cervical Spondylosis. Medscape, 2015
- ↑ HUBERT L. ROSOMOFF, FERDINAND ROSSMANN, Treatment of Cervical Spondylosis by Anterior Cervical Diskectomy and Fusion, Archives of neurology, 1966
- ↑ 10.0 10.1 McCormack BM, Weinstein PR. Cervical spondylosis. An update. West J Med. Jul-Aug 1996;165(1-2):43-51.
- ↑ Torrens M, Cervical Spondylosis Part 1: Pathogenesis, Diagnosis and Management Options
- ↑ Emery SE. Cervical spondylotic myelopathy: diagnosis and treatment. J Am Acad Orthop Surg. Nov-Dec 2001;9(6):376-88. (Level: A1)
- ↑ Rahim KA, Stambough JL. Radiographic evaluation of the degenerative cervical spine. Orthop Clin North Am. Jul 1992;23(3):395-403.
- ↑ Heller JG. The syndromes of degenerative cervical disease. Orthop Clin North Am. Jul 1992;23(3):381-94. (Level: A1)
- ↑ Takagi I, Cervical Spondylosis: An Update on Pathophysiology, Clinical Manifestation, and Management Strategies. DM, October 2011
- ↑ Binder AI. Cervical spondylosis and neck pain. BMJ: British Medical Journal. 2007 Mar 10;334(7592):527.
- ↑ Ellenberg MR, Honet JC, Treanor WJ. Cervical radiculopathy. Arch Phys Med Rehabil. Mar 1994;75(3):342-52
- ↑ Heller JG. The syndromes of degenerative cervical disease. Orthop Clin North Am. Jul 1992;23(3):381-94. (Level: A1)
- ↑ Kaye JJ, Dunn AW. Cervical spondylotic dysphagia. South Med J. May 1977;70(5):613-4. (Level: A1)
- ↑ Kanbay M, Selcuk H, Yilmaz U. Dysphagia caused by cervical osteophytes: a rare case. J Am Geriatr Soc. Jul 2006;54(7):1147-8. (Level: C)
- ↑ Binder AI. Cervical spondylosis and neck pain: clinical review. BMJ 2007:334:527-31
- ↑ 22.0 22.1 Binder AI. Cervical spondylosis and neck pain: clinical review. BMJ 2007:334:527-31
- ↑ Zhijun Hu et al., A 12-Words-for-Life-Nurturing Exercise Program as an Alternative Therapy for Cervical Spondylosis: A Randomized Controlled Trial, 20 March 2014
- ↑ C. Xu et al., Comparison of computed tomography and magnetic resonance imaging in the evaluation of facet tropism and facet arthrosis in degenerative cervical spondylolisthesis, 2014
- ↑ J. Lafuente, A.T.H. Casey, A. Petzold, S. Brew, The Bryan cervical disc prosthesis as an alternative to arthrodesis in the treatment of cervical spondylosis, The Bone and Joint Journal, 2005.
- ↑ M. Pumberger, D. Froemel, Clinical predictors of surgical outcome in cervical spondylotic myelopathy, The Bone and Joint Journal, 2013
- ↑ D.R. Lebl, A. Hughes, P.F. O’Leary, Cervical Spondylotic Myelopathy: Pathophysiology, Clinical Presentation, and Treatment, the Musculoskeletal Journal of Hospital for Special Surgery, Jul 2011.
- ↑ Hyun-Jin Jo et al., Unrecognized Shoulder Disorders in Treatment of Cervical Spondylosis Presenting Neck and Shoulder Pain, The Korean Spinal Neurosurgery Society, 9(3):223-226, 2012
- ↑ EIRA Viikari-Juntura, Interexaminer Reliability of Observations in Physical Examinations of the Neck, Journal of the American Physical Therapy Association
- ↑ Benatar M., Neuromuscular Disease - Evidence and Analysis in Clinical Neurology, Humana Press Inc., Totowa, NJ, 2006, p. 61-78.
- ↑ Macnab I. Cervical spondylosis. Clin Orthop Relat Res. 1975;(109):69-77
- ↑ 32.0 32.1 32.2 Kieran Michael Hirpara, Joseph S. Butler, Roisin T. Dolan, John M. O'Byrne, and Ashley R. Poynton , Nonoperative Modalities to Treat Symptomatic Cervical Spondylosis, Advances in Orthopedics, 2011
- ↑ 33.0 33.1 33.2 Melvin D. Law, Jr., M.D.a, Mark Bemhardt, M.D.b, and Augustus A. White, III, M.D., Cervical Spondylotic Myelopathy: A Review of Surgical Indications and Decision Making, Yale journal of biology and medicine,1993
- ↑ 34.0 34.1 34.2 Kyoung-Tae Kim and Young-Baeg Kim, Cervical Radiculopathy due to Cervical Degenerative Diseases : Anatomy, Diagnosis and Treatment, The Korean Neurosurgical Society, 2010
- ↑ Rahim KA, Stambough JL. Radiographic evaluation of the degenerative cervical spine. Orthop Clin North Am. Jul 1992;23(3):395-403.
- ↑ Heller JG. The syndromes of degenerative cervical disease. Orthop Clin North Am. Jul 1992;23(3):381-94.
- ↑ Binder AI. Cervical spondylosis and neck pain: clinical review. BMJ 2007:334:527-31
- ↑ Kieran Michael Hirpara, Joseph S. Butler, Roisin T. Dolan, John M. O'Byrne, and Ashley R. Poynton , Nonoperative Modalities to Treat Symptomatic Cervical Spondylosis, Advances in Orthopedics, 2011
- ↑ 39.0 39.1 39.2 . Ian A. Young, Lori A. Michener, Joshua A. Cleland, Arnold J. Aguilera, Alison R. Snyde, Manual Therapy, Exercise, andTraction for Patients With Cervical Radiculopathy: A Randomized Clinical Trial, 2009
- ↑ 40.0 40.1 Michale Costello, Treatment of a Patient with Cervical Radiculopathy Using Thoracic Spine Thrust Manipulation, Soft Tissue Mobilization, and Exercise, the Journal of Manual and manipulative therapy
- ↑ 41.0 41.1 41.2 Ibrahim M. Moustafa and Aliaa A. Diab, Multimodal Treatment Program Comparing 2 Different Traction Approaches for Patients With Discogenic Cervical Radiculopathy: A Randomized Controlled Trial, Journal of Chiropractic Medicine (2014) 13, 157–167