Benign Paroxysmal Positional Vertigo: A Case Study
Abstract[edit | edit source]
This is a fictional story depicting a patient diagnosed with idiopathic benign paroxysmal positional vertigo (BPPV). The purpose of this fictional case study is to investigate the physiotherapy-related approaches for assessing, diagnosing and treating this condition. The patient decided to seek out physiotherapy treatment to reduce his symptoms. He currently is unable to perform activities he usually enjoys such as driving or walking his dog. He is also stressed out about his work performance.
The Epley’s maneuver treatment technique was used to target the semicircular canals in order to minimize patient symptoms. Patient education of risk factors for recurrence as well as vestibular exercises were employed to reduce the risk of recurrence. A variety of outcome measures (Dynamic Gait Index, Dizziness Handicap Inventory, Vertigo Handicap Questionnaire, Activities-specific Balance Confidence Scale) were used to monitor progression of treatment/symptoms. The patient surpassed the minimally detectable changes for each of the outcome measures.
After completing the physiotherapist's treatment plan, the patient stated that he only had mild dizziness during specific tasks. With adequate education on how to manage symptoms, the patient has been discharged.
Introduction[edit | edit source]
This case study involves a 55-year-old male with Benign Paroxysmal Positional Vertigo (BPPV).
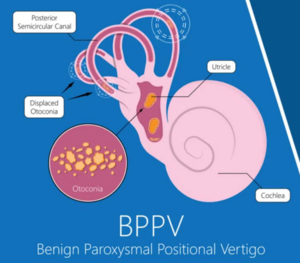
BPPV is a common disorder of the inner ear associated with the sensation of vertigo or dizziness. BPPV is the most common type of related vertigo condition and has an incidence of 107 cases out of 100,000 people per year[1]. It also has a 2.4% lifetime prevalence rate which increases with age [2]. The cause of this condition is usually insidious, but can also be brought on by a traumatic blow to the head. In this case study, the patient had a history of chronic headaches which is what may have caused his BPPV. Within the utricle of the inner ear, there are calcium-carbonate crystals (otoconia). These crystals may displace from their original location into the semicircular canals of the inner ear. Once the crystals are dislodged, the body’s ability to sense positional changes of the head, along with rotation and linear acceleration will be affected. Thus, creating symptoms of spinning or dizziness. This condition will cause a loss of balance, creating difficulties when attempting activities of daily living (ADLs).
Physiotherapists may assist patients with this condition through education, manual therapy, and exercise prescription. By minimizing symptoms, the patient will have much more independence and an increased quality of life.
When investigating other studies, we came across Burrows & Price case study of a 33-year-old male soccer player who had suffered from BPPV. They discuss the occupational risk of playing soccer with this condition due to the repetitive heading contact of the ball. As previously mentioned, the cause of this condition is most often insidious. Even if a patient has BPPV due to a non-traumatic cause, therapists must educate their patients on the risk of exacerbating their condition, even if their symptoms are resolved.[3]
The purpose of this fictional case study is to examine the role of physiotherapists in assessing, diagnosing, and treating posterior canal BPPV. Patient-centered goals will be identified to manage a typical problem list for this condition.
[edit | edit source]
Client Characteristics[edit | edit source]
The patient is a 55 year old male who lives a relatively sedentary lifestyle and works as an accountant. He has high blood pressure which has been controlled by 40mg of Diovan daily. The patient also has high cholesterol in which he takes 5mg of Crestor daily to help control. The patient enjoys gardening, driving with his wife and walking his dog. He complains of nausea, dizziness and the feeling of the room spinning. He is planning on retiring and is nervous about not being able to do what he wants and enjoy his retirement because of his symptoms. He first noticed symptoms 2 weeks ago while turning his head quickly while driving. Following the onset, medications did not help symptoms and therefore he has since been getting treatment for BPPV. Sleeping has become increasingly difficult as any time he lays down he begins to feel dizzy.
Examination Findings[edit | edit source]
Subjective[edit | edit source]
History of Present Illness
His symptoms first started on April 22nd, 2022, while he was shoulder checking to switch lanes while driving. He went to see his Family Physician on April 24th, 2022 who referred him to physiotherapy. Currently, his chief complaints are dizziness, a feeling of his surroundings "spinning", and occasional nausea.
Past Medical History
This patient was diagnosed with hypertension and hypercholesterolemia in December 2015. He has also been experiencing headaches for the past three months (about one headache per week, lasting longer than 30 minutes)
Medications
Currently, this patient takes 40mg of Diovan daily to control his high blood pressure and 5mg of Crestor daily to control his high cholesterol. He also takes 1 Gravol liquid gel capsule (50mg) every 4 hours when he begins feeling symptomatic.
Functional History
The patient has mentioned that he is unable to perform activities that he usually enjoys such as gardening, driving, and walking his dog. Although he can perform basic activities of daily living independently such as getting dressed, eating, walking short distances, using the washroom, and bathing, he has more difficulty with instrumental activities of daily living such as shopping, housework, and cooking. Aggravating activities include rolling out of bed and bending over. Pain is alleviated when lying on his back with his head elevated using multiple pillows.
Social History
This patient works full-time as an accountant. He lives in a bungalow in a small neighbourhood with his wife and golden retriever. All of the rooms that he needs are on the main floor (i.e. bedroom, kitchen, bathroom), with the top floor mainly used for storage and guest bedrooms. His two adult children (aged 30 and 27) live within a 15 minute drive and visit often. In his free time, he enjoys gardening, walking his dog, and going on drives into the city with his wife. He has never been a smoker and does not use any recreational drugs, but will have the occasional beer or glass of wine on the weekend with his wife and kids. He reports feeling stressed about getting tasks done at work due to having to take frequent breaks.
Family History
When asked, the patient could not recall any family members having BPPV. However, he did report that his father also has hypertension and suffered a heart attack at the age of 65. His mother is also currently exhibiting signs of early dementia, although this has not been officially diagnosed yet. No other family history can be recalled by the patient.
Objective[edit | edit source]
Positive Findings
- Vestibulocochlear nerve exam - right side
- Dix-Hallpike test - right side
Negative Findings
- All other cranial nerve examinations
- Dix-Hallpike test - left side
- Supine roll test (for Horizontal semicircular canal) - bilateral
- Head Pitch Test
- Finger to nose test
Outcome Measures[edit | edit source]
The outcome measures chosen to assess this patient were the Dynamic Gait Index, Dizziness Handicap Inventory, Vertigo Handicap Questionnaire and Activities-specific Balance Confidence Scale. He obtained baseline scores of 18/24 on the Dynamic Gait Index, 37/100 on the Dizziness Handicap Inventory, 76% on the Vertigo Handicap Questionnaire and 44% on the Activities-specific Balance Confidence Scale.
Clinical Hypothesis[edit | edit source]
Physiotherapy Diagnosis[edit | edit source]
A 55 year old male patient presents with vertigo, nystagmus, dizziness and balance issues caused by different head positions onset 2 weeks ago. The present symptoms put the patient at a higher risk of falls and a decreased quality of life. Based on past level of functioning and timeline of onset the patient is expected to make a full recovery. Subjective and objective measures are consistent with right-sided posterior canal BPPV (canalithiasis) with unknown insidious cause.
Problem List[edit | edit source]
- Vertigo, nystagmus, dizziness and imbalance caused by sudden specific head position changes
- Unable to work caused by symptoms
- Unable to garden
- Unable to walk/play with dog
- Decreased productivity at work due to fear of onset of vertigo
- Unable to drive since onset of symptoms
Intervention[edit | edit source]
Goals:
Short-term Goals:
- The patient wants to go 48 hours without any provocation of symptoms by the second week of treatment (14 days post-treatment).
- The patient wants to improve his dynamic gait index score to 20 by the 10th-day post-treatment.
Long-term Goals:
- Patient wants to be able to drive to work without feeling dizzy checking his blindspots (30 min drive) in 6 weeks.
- Patient wants to be able to play fetch with his dog for 20 minutes without an onset of symptoms from picking up the ball in 8 weeks.
Following the assessment and informed consent for treatment, the Epley’s maneuver was performed 3 times on the right affected side to target the posterior semicircular canal which immediately reduced the patient’s BPPV symptoms. (Source 5). The patient reported no symptoms within the 24 hours following this technique.
The Semont maneuver is another effective approach for treating posterior canal BPPV, however it was not performed because Epley’s has better short-term effectiveness for treating this condition (although the two maneuver’s are equally as effective when it comes to long-term effectiveness for treating it) (Source 6 and 4).
The patient was also educated on recurrence rates and risk factors before leaving the clinic. This included to keep their head vertical and to sleep in the semi-recumbent for the next 24 hours. In addition they were also instructed to avoid provoking head positions such as sleeping on their right side, not flexing, extending, rotating or side bending their head excessively in the next week (source 15). If they were experiencing symptoms they were also instructed not to drive.
Upon the next treatment visit, vestibular rehabilitation was performed. The patient was taught Cawthrone-Cooksey exercises with a focus of training the eyes to move independently of the head. This consisted of performing exercises by gradually building up from one exercise to the next. Having the patient rate the severity of symptoms during the exercise on a scale of 0-5 (where 0 = no symptoms and 5 = severe symptoms) to pace the progression of exercises. Exercises may include gaze training, balancing in day-to-day situations, improving coordination (catching and throwing a ball, walking on incline, stooping) (14).
The patient was also taught Brandt-Daroff exercises at the 1 week physiotherapy intervention mark to promote loosening of canals and to prevent the patient’s chance for BPPV recurrence (source 18). They were instructed to perform 1-4 reps of 3 sets a day for 2 weeks. In addition, the patient was educated that if BPPV symptoms were to recur, this technique does show some effectiveness for self symptomatic relief (source 19).
Outcome[edit | edit source]
After six weeks of treatment, this patient experiences a great degree of improvement. First, his Dynamic Gait Index post-treatment score is now 22, compared to his baseline score of 18. This is considered a significant change as minimal detectable change is expected to be approximately 4 points. This also means that this patient is no longer considered to be a fall risk as their score is now higher than 19/24.
Additionally, his Dizziness Handicap Inventory post-treatment score improved to 14, compared to his baseline score of 37 which surpasses the estimated minimal clinically important difference of 4 points and the minimal detectable change of 17 points. This means that he is no longer considered to have a handicap associated with their dizziness.
Furthermore, his Activities-specific Balance Confidence Scale post-treatment score is now 86%, compared to his baseline score of 44%. This surpasses the estimated minimal detectable change of 15 points. This also means that he is now considered to have a high level of functioning.
His Vertigo Handicap Questionnaire score has decreased from 76% down to 24%, indicating an improvement (less of a handicap), with key improvements with regards to the items on anxiety and fear surrounding his vertigo. Additionally, he no longer indicates that his vertigo is causing him issues at work, and he is able to carry on with what he is doing when his vertigo becomes present. (Sources 24/25)
In addition to outcome measures, the patient now only reports mild dizziness during specific tasks, but does not feel like the room is spinning around them and no longer feels nauseous. He is also now able to do all the tasks he was able to do prior to the onset of symptoms such as gardening and driving. He is very motivated and continues to work on his balance training at home.
Due to our patient's current functional status as well as their high motivation levels, we believe they are ready for discharge. In order to prepare them for discharge, we will have a meeting with out patient along with any family members they want to include in this process (ex. spouse) to make a plan together. We will have the patient continue their at-home balance management program and we will also provide him with resources to educate him on his condition as well as positions and movements that might alleviate or aggravate symptoms. We will explain to him that although his scores have improved tremendously since beginning treatment, there is always room for improvement. We will make a follow-up appointment for three months from the discharge date with a goal of near-perfect scores on the Dynamic Gait Index, Dizziness Handicap Inventory, and Activities-specific Balance Confidence Scale.
At this time, we do not believe that referral to other health care providers is necessary as our patient is highly functional with minimal symptoms. However, we will ensure to let the patient know that if symptoms become worse or they experience any other symptoms, they should seek help from their Family Physician, a neurologist or an otolaryngologist as soon as possible.
Multidisciplinary Team[edit | edit source]
While the physiotherapist will be the main health care professional responsible in this case, otolaryngologists may also be used if imaging or surgery is required. The patient’s family doctor should also monitor their medication or if any new or ongoing symptoms are representing. (source: #11-15 from poster)
Discussion[edit | edit source]
The patient's reason for physiotherapy visit and chief complaints included dizziness, feeling of the room spinning, and nausea. After a full examination, the patient showed signs of a posterior canal BPPV caused by chronic headaches. After 6 weeks of treatment, their outcome measures dramatically improved and they were able classified as having a high level of functioning.
Techniques outlined in the management program included the Epley maneuver, Cawthrone-Cooksey exercises and Brandt-Daroff exercises are appropriate treatment techniques for this case of vertigo. Similar interventions outlined may also be implemented to treat dizzy spells caused by medication side effects or other vestibular conditions. Additionally, balance training is beneficial for the general population and can help reduce the risk of falls and improve stability. </ref>.
Study Questions[edit | edit source]
Q1: Which score would indicate that a patient is a falls risk based on the dynamic gait index?
- 15
- 19
- 20
- All of the above
- A and B only
Q2: Which of the following statements is true regarding posterior canal BPPV?
- Dix-Hallpike Test will be positive on the affected side
- Supine roll test will be positive on the affected side
- Dix-Hallpike test will be positive on the unaffected side
- Posterior canal BPPV is less common than anterior canal BPPV
Q3: Which of the following would is not a symptom of posterior canal BPPV?
- Complete vision loss
- Dizziness
- Nystagmus
- Balance loss
Answers[edit | edit source]
Q1: 5 - A & B only
Q2: 1 -Dix-Hallpike Test will be positive on the affected side
Q3: 1 - Complete vision loss
References[edit | edit source]
- ↑ Froehling DA, Silverstein MD, Mohr DN, Beatty CW, Offord KP, Ballard DJ. Benign positional vertigo: incidence and prognosis in a population-based study in Olmsted County, Minnesota. Mayo Clin Proc [internet]. 1991 Jun [cited 2022 May 5]; 66(6):596-601. doi: 10.1016/s0025-6196(12)60518-7.
- ↑ von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, Neuhauser H. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry [internet]. 2007 Jul [cited 2022 May 5]; 78(7):710-5. doi: 10.1136/jnnp.2006.100420.
- ↑ Burrows, L, Price, R. Benign paroxysmal positional vertigo (BPPV) diagnosis and treatment in an elite professional football (soccer) player. BMJ Case Reports [internet]. 2017 Jul [cited 2022 May 4] 1-4. Available frome doi:10.1136/bcr-2017-220000.