Assessment and Treatment of the Thoracic Spine: Difference between revisions
No edit summary |
No edit summary |
||
| Line 51: | Line 51: | ||
** Is the postural change a primary problem or related to something else in the chain (e.g. lumbopelvic dysfunction) | ** Is the postural change a primary problem or related to something else in the chain (e.g. lumbopelvic dysfunction) | ||
* [[Assessment of Breathing Pattern Disorders|Breathing mechanics]] | * [[Assessment of Breathing Pattern Disorders|Breathing mechanics]] | ||
* ROM tests from neutral | * [[File:Dermatomes Grant.png|thumb|Figure 2. Dermatomes. ]]ROM tests from neutral | ||
** Look for intersegmental restrictions | ** Look for intersegmental restrictions | ||
** Assess from behind | ** Assess from behind | ||
* Inter-ring and articular palpation during motion | * Inter-ring and articular palpation during motion | ||
* | * Motor control and strength tests | ||
** Sitting | ** Sitting | ||
** Puppy lie | ** Puppy lie | ||
| Line 71: | Line 71: | ||
</div> | </div> | ||
=== Active Thoracic Movement Tests === | |||
During the active movement tests:<ref name=":0" /> | |||
* Assess the patient in sitting in order to isolate the thoracic spine (by blocking the lumbar spine) | |||
* Assess for asymmetry of movement and any segmental cause of restriction | |||
** Remember that motor control is also important in the thoracic region, not just stiffness | |||
==== Thoracic Flexion and Extension ==== | |||
* Flexion: feel for anterior tilt of the ribs | |||
* Extension: feel for posterior rib tilt | |||
* NB extension is the most limited movement in the thoracic spine | |||
Thoracic Rotation | |||
Rotation is one of the most useful tests for the thoracic spine. During rotation movements, it is possible to identify: | |||
* Stiffness | |||
* Sequencing issues | |||
== References == | == References == | ||
Revision as of 01:33, 4 September 2021
Top Contributors - Jess Bell, Kim Jackson, Kirenga Bamurange Liliane, Tarina van der Stockt, Lucinda hampton, Olajumoke Ogunleye, Aminat Abolade and Merinda Rodseth
Subjective Assessment[edit | edit source]
Detailed information on the assessment of the thoracic spine is available here, but specific questions to consider in the subjective assessment include:[1]
- How did the problem begin? How long has it been a problem?
- How has the pain progressed over time?
- Is there a history of overload or trauma?
- Does the patient have pain with breathing? And during which part of the breath does this occur?
- What effect does coughing and / or sneezing have?
- Can the patient lie on the affected side at night?
- How is the pain behaving and what is the level of irritability?
- Consider in particular more stiffness
- If there is stiffness for a prolonged period in the morning, and a history of enthesopathies, the patient may have a spondyloarthropathy[1][2]
- What are the specific functional impairments? (e.g. during sport, activities of daily living)
- What is the patient’s medical history?
- Essential to know due to spinal masqueraders in the thoracic spine
- Are there any psychosocial factors contributing to the pain?
- The sympathetic nervous system is prominent in the thoracic region[1]
- Are there any red flags?[3]
Pain can be caused by inflammation, or it may originate in the cartilage, ligaments, bone (fracture) or the nerve root:[1]
- Nerve root or facet pain may be described as lancinating / nauseating and it may radiate and follow angulation of rib
- Costochondritis tends to be described as a deep, boring, aching pain in the chest wall that may radiate (often posteriorly or to the neck)
- Rib fracture or intercostal strain is typically described as a sudden, sharp / piercing pain, which is then aggravated by laughing, sneezing, coughing, deep breaths or any type of straining manoeuvre
- When patients have immobility, they tend to report stiffness, restricted movement, or a sense of feeling ‘stuck’
Objective Assessment[edit | edit source]
The objective examination is guided by findings in the subjective interview. Remember:[1]
- It is essential to understand which structures are loaded during each test
- Keep tests to a minimum
- “Less is more” to avoid flaring up the patient
- Consider combinations of tests
- The best ‘special test’ is the one the patient demonstrates to you
- Consider the diaphragm
During the assessment, the therapist should develop a sound hypothesis. “If you can’t find it, you can’t assess it and you can’t treat it”.[1]
Objective Testing[edit | edit source]
The following tests should be included in an objective examination of the thoracic spine:[1]
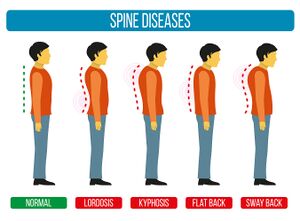
- Static and dynamic postural assessment:
- Watch how the patient moves / drifts / hinges
- Consider different types of postural dysfunctions[4](see Figure 1)
- Is the postural change a primary problem or related to something else in the chain (e.g. lumbopelvic dysfunction)
- Breathing mechanics
- ROM tests from neutral
- Look for intersegmental restrictions
- Assess from behind
- Inter-ring and articular palpation during motion
- Motor control and strength tests
- Sitting
- Puppy lie
- 4 point
- Neurodynamic tests
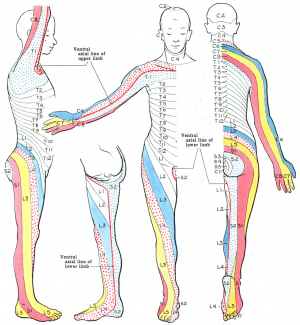
- Neurological
- Thoracic dermatome testing (see Figure 2)
- Palpation, including the clavicle and first rib
Active Thoracic Movement Tests[edit | edit source]
During the active movement tests:[1]
- Assess the patient in sitting in order to isolate the thoracic spine (by blocking the lumbar spine)
- Assess for asymmetry of movement and any segmental cause of restriction
- Remember that motor control is also important in the thoracic region, not just stiffness
Thoracic Flexion and Extension[edit | edit source]
- Flexion: feel for anterior tilt of the ribs
- Extension: feel for posterior rib tilt
- NB extension is the most limited movement in the thoracic spine
Thoracic Rotation
Rotation is one of the most useful tests for the thoracic spine. During rotation movements, it is possible to identify:
- Stiffness
- Sequencing issues
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Bell-Jenje T. Assessment and Treatment of the Thoracic Spine Course. Physioplus, 2021.
- ↑ Martey C. Co-morbidities within Spondyloarthritis Course. Physioplus, 2020.
- ↑ Finucane LM, Downie A, Mercer C, Greenhalgh SM, Boissonnault WG, Pool-Goudzwaard AL et al. International framework for red flags for potential serious spinal pathologies. J Orthop Sports Phys Ther. 2020;50(7):350-72.
- ↑ Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018;13:6.
- ↑ Jones MR, Prabhakar A, Viswanath O, Urits I, Green JB, Kendrick JB et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment. Pain Ther. 2019;8(1):5-18.
- ↑ Li N, Dierks G, Vervaeke HE, Jumonville A, Kaye AD, Myrcik D et al. Thoracic outlet syndrome: a narrative review. J Clin Med. 2021;10(5):962.
- ↑ John Gibbons. Upper Limb Tension Test (ULTT) for the Median Nerve (C5-T1 Brachial plexus). Available from: https://www.youtube.com/watch?v=fhsrNKWVh0s [last accessed 4/9/2021]
- ↑ ohn Gibbons. Upper Limb Tension Test - Radial Nerve (C5-T1 Brachial Plexus). Available from: https://www.youtube.com/watch?v=VngRTMhAlGE [last accessed 4/9/2021]