Assessment and Treatment of the Thoracic Spine: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
<div class="noeditbox">This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}})</div> | <div class="noeditbox">This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}})</div> | ||
Detailed information on the assessment of the thoracic spine is available here, | == Subjective Assessment == | ||
Detailed information on the assessment of the thoracic spine is available [[Thoracic Examination|here]], but specific questions to consider in the subjective assessment include:<ref name=":0">Bell-Jenje T. Assessment and Treatment of the Thoracic Spine Course. Physioplus, 2021.</ref> | |||
* How did the problem begin? How long has it been a problem? | |||
* How has the pain progressed over time? | |||
* Is there a history of overload or trauma? | |||
* Does the patient have pain with breathing? And during which part of the breath does this occur? | |||
* What effect does coughing and / or sneezing have? | |||
* Can the patient lie on the affected side at night? | |||
* How is the pain behaving and what is the level of irritability? | |||
** Consider in particular more stiffness | |||
** If there is stiffness for a prolonged period in the morning, and a history of enthesopathies, the patient may have a [[Co-morbidities and Extra-articular Manifestations of Spondyloarthropathy|spondyloarthropathy]]<ref name=":0" /><ref>Martey C. Co-morbidities within Spondyloarthritis Course. Physioplus, 2020.</ref> | |||
* What are the specific functional impairments? (e.g. during sport, activities of daily living) | |||
* What is the patient’s medical history? | |||
** Essential to know due to [[Clinical Reasoning and Pathologies of the Thoracic Spine|spinal masqueraders]] in the thoracic spine | |||
* Are there any psychosocial factors contributing to the pain? | |||
** The sympathetic nervous system is prominent in the thoracic region<ref name=":0" /> | |||
* Are there any [[An Introduction to Red Flags in Serious Pathology|red flags]]?<ref>Finucane LM, Downie A, Mercer C, Greenhalgh SM, Boissonnault WG, Pool-Goudzwaard AL et al. [https://www.jospt.org/doi/10.2519/jospt.2020.9971?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed International framework for red flags for potential serious spinal pathologies]. J Orthop Sports Phys Ther. 2020;50(7):350-72.</ref> | |||
Pain can be caused by inflammation, or it may originate in the cartilage, ligaments, bone (fracture) or the nerve root:<ref name=":0" /> | |||
* Nerve root or facet pain may be described as lancinating / nauseating and it may radiate and follow angulation of rib | |||
* Costochondritis tends to be described as a deep, boring, aching pain in the chest wall that may radiate (often posteriorly or to the neck) | |||
* Rib fracture or intercostal strain is typically described as a sudden, sharp / piercing pain, which is then aggravated by laughing, sneezing, coughing, deep breaths or any type of straining manoeuvre | |||
* When patients have immobility, they tend to report stiffness, restricted movement, or a sense of feeling ‘stuck’ | |||
== Objective Assessment == | |||
The objective examination is guided by findings in the subjective interview. Remember:<ref name=":0" /> | |||
* It is essential to understand which structures are loaded during each test | |||
* Keep tests to a minimum | |||
** “Less is more” to avoid flaring up the patient | |||
** Consider combinations of tests | |||
* The best ‘special test’ is the one the patient demonstrates to you | |||
* Consider the diaphragm | |||
During the assessment, the therapist should develop a sound hypothesis. “If you can’t find it, you can’t assess it and you can’t treat it”.<ref name=":0" /> | |||
=== Objective Testing === | |||
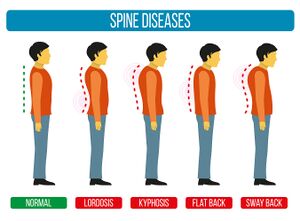
[[File:Adapted Bigstock Image - Spine Diseases - ID 129611492.jpg|thumb|Figure 1. Common postural dysfunctions. ]] | |||
The following tests should be included in an objective examination of the thoracic spine:<ref name=":0" /> | |||
* Static and dynamic postural assessment: | |||
** Watch how the patient moves / drifts / hinges | |||
** Consider different [[Postural Changes Affecting Voice Production|types of postural dysfunctions]]<ref>Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5836359/ Non-structural misalignments of body posture in the sagittal plane]. Scoliosis Spinal Disord. 2018;13:6. </ref>(see Figure 1) | |||
** Is the postural change a primary problem or related to something else in the chain (e.g. lumbopelvic dysfunction) | |||
* [[Assessment of Breathing Pattern Disorders|Breathing mechanics]] | |||
* ROM tests from neutral | |||
** Look for intersegmental restrictions | |||
** Assess from behind | |||
* Inter-ring and articular palpation during motion | |||
* Motor control and strength tests | |||
** Sitting | |||
** Puppy lie | |||
** 4 point | |||
* Neurodynamic tests | |||
** Upper limb tension test for thoracic outlet syndrome (see videos below)<ref>Jones MR, Prabhakar A, Viswanath O, Urits I, Green JB, Kendrick JB et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6514035/ Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment]. Pain Ther. 2019;8(1):5-18.</ref><ref>Li N, Dierks G, Vervaeke HE, Jumonville A, Kaye AD, Myrcik D et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7957681/ Thoracic outlet syndrome: a narrative review]. J Clin Med. 2021;10(5):962.</ref> | |||
** NB this test may not always be positive in TOS patients, but it needs to be assessed in detail<ref name=":0" /> | |||
* Neurological | |||
** Thoracic [[Dermatomes|dermatome testing]] | |||
* Palpation, including the clavicle and first rib | |||
== References == | |||
[[Category:Physioplus Content]] | |||
[[Category:Course Pages]] | |||
[[Category:Thoracic Spine]] | |||
Revision as of 01:19, 4 September 2021
Top Contributors - Jess Bell, Kim Jackson, Kirenga Bamurange Liliane, Tarina van der Stockt, Lucinda hampton, Olajumoke Ogunleye, Aminat Abolade and Merinda Rodseth
Subjective Assessment[edit | edit source]
Detailed information on the assessment of the thoracic spine is available here, but specific questions to consider in the subjective assessment include:[1]
- How did the problem begin? How long has it been a problem?
- How has the pain progressed over time?
- Is there a history of overload or trauma?
- Does the patient have pain with breathing? And during which part of the breath does this occur?
- What effect does coughing and / or sneezing have?
- Can the patient lie on the affected side at night?
- How is the pain behaving and what is the level of irritability?
- Consider in particular more stiffness
- If there is stiffness for a prolonged period in the morning, and a history of enthesopathies, the patient may have a spondyloarthropathy[1][2]
- What are the specific functional impairments? (e.g. during sport, activities of daily living)
- What is the patient’s medical history?
- Essential to know due to spinal masqueraders in the thoracic spine
- Are there any psychosocial factors contributing to the pain?
- The sympathetic nervous system is prominent in the thoracic region[1]
- Are there any red flags?[3]
Pain can be caused by inflammation, or it may originate in the cartilage, ligaments, bone (fracture) or the nerve root:[1]
- Nerve root or facet pain may be described as lancinating / nauseating and it may radiate and follow angulation of rib
- Costochondritis tends to be described as a deep, boring, aching pain in the chest wall that may radiate (often posteriorly or to the neck)
- Rib fracture or intercostal strain is typically described as a sudden, sharp / piercing pain, which is then aggravated by laughing, sneezing, coughing, deep breaths or any type of straining manoeuvre
- When patients have immobility, they tend to report stiffness, restricted movement, or a sense of feeling ‘stuck’
Objective Assessment[edit | edit source]
The objective examination is guided by findings in the subjective interview. Remember:[1]
- It is essential to understand which structures are loaded during each test
- Keep tests to a minimum
- “Less is more” to avoid flaring up the patient
- Consider combinations of tests
- The best ‘special test’ is the one the patient demonstrates to you
- Consider the diaphragm
During the assessment, the therapist should develop a sound hypothesis. “If you can’t find it, you can’t assess it and you can’t treat it”.[1]
Objective Testing[edit | edit source]
The following tests should be included in an objective examination of the thoracic spine:[1]
- Static and dynamic postural assessment:
- Watch how the patient moves / drifts / hinges
- Consider different types of postural dysfunctions[4](see Figure 1)
- Is the postural change a primary problem or related to something else in the chain (e.g. lumbopelvic dysfunction)
- Breathing mechanics
- ROM tests from neutral
- Look for intersegmental restrictions
- Assess from behind
- Inter-ring and articular palpation during motion
- Motor control and strength tests
- Sitting
- Puppy lie
- 4 point
- Neurodynamic tests
- Neurological
- Thoracic dermatome testing
- Palpation, including the clavicle and first rib
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Bell-Jenje T. Assessment and Treatment of the Thoracic Spine Course. Physioplus, 2021.
- ↑ Martey C. Co-morbidities within Spondyloarthritis Course. Physioplus, 2020.
- ↑ Finucane LM, Downie A, Mercer C, Greenhalgh SM, Boissonnault WG, Pool-Goudzwaard AL et al. International framework for red flags for potential serious spinal pathologies. J Orthop Sports Phys Ther. 2020;50(7):350-72.
- ↑ Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018;13:6.
- ↑ Jones MR, Prabhakar A, Viswanath O, Urits I, Green JB, Kendrick JB et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment. Pain Ther. 2019;8(1):5-18.
- ↑ Li N, Dierks G, Vervaeke HE, Jumonville A, Kaye AD, Myrcik D et al. Thoracic outlet syndrome: a narrative review. J Clin Med. 2021;10(5):962.