Ankle Lateral Ligament Injury Assessment: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
[https://physio-pedia.com/Ankle_Sprain#cite_note-Roos-1 Lateral ankle ligament injruy] is a common MSK condition representing 85% of ankle injuries <ref>Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wickstrom EA. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. American journal of sports medicine. 2016.''The American Journal of Sports Medicine'' Vol 45, Issue 1, pp. 201 - 209</ref>and has a high recurrencce rate<ref | [https://physio-pedia.com/Ankle_Sprain#cite_note-Roos-1 Lateral ankle ligament injruy] is a common MSK condition representing 85% of ankle injuries <ref name=":0">Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wickstrom EA. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. American journal of sports medicine. 2016.''The American Journal of Sports Medicine'' Vol 45, Issue 1, pp. 201 - 209</ref>and has a high recurrencce rate<ref name=":0" />. Persisting post-injury symptoms such as swelling, impaired strength, instability (occasional giving way), and impaired balance responses for more than 12 months following the initial injury is defined as <nowiki>''</nowiki> [https://physio-pedia.com/Chronic_Ankle_Instability_Risk_Identification#cite_note-2 Chronic Ankle Instability-CAI]<nowiki>''</nowiki><ref>Fernández-de-las-Peñas C, editor. Manual therapy for musculoskeletal pain syndromes: An evidence-and clinical-informed approach. Elsevier Health Sciences; 2015 Jun 17</ref>. Up to 70% of patients report developing chronic ankle instability<ref>Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med 2005;39:e14; discussion e14. | ||
</ref>. | |||
</ref>. | |||
Limited dorsiflexion<ref>Pope R, Herbert R, Kirwan J. Effects of ankle dorsiflexion range and pre-exercise calf muscle stretching on injury risk in Army recruits. Australian Journal of Physiotherapy. 1998 Jan 1;44(3):165-72.</ref>, reduced proprioception, reduced isometric abductor hip strength<ref>Powers CM, Ghoddosi N, Straub RK, Khayambashi K. Hip strength as a predictor of ankle sprains in male soccer players: a prospective study. Journal of athletic training. 2017 Nov;52(11):1048-55.</ref>, postural control deficiencies on SLS <ref>Kobayashi T, Yoshida M, Yoshida M, et al. Intrinsic Predictive Factors of Noncontact Lateral Ankle Sprain in Collegiate Athletes: A Case-Control Study. Orthop J SportsMed 2013;1:232596711351816.</ref> were associated with higher risk of ankle sprain and instability. | |||
The highest incidence of LAS was found for aeroball, basketball, indoor volleyball, field sports and climbing<ref>Waterman BR, Belmont PJ, Cameron KL, et al. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med 2010;38:797–803.</ref>. | |||
A systematic review by Hiller et al<ref>Hiller CE, Nightingale EJ, Lin CW, Coughlan GF, Caulfield B, Delahunt E. Characteristics of people with recurrent ankle sprains: a systematic review with meta-analysis. Br J Sports Med. 2011 Jun 1;45(8):660-72.</ref> reported greater larger talar curve, reduced concentric inversion strength, greater sway when standing on stable surfaces with eyes closed, a more inverted ankle position and decreased foot clearance during gait, and prolonged time to stabilisation after a jump. | |||
== Assessment == | == Assessment == | ||
| Line 45: | Line 40: | ||
=== Objective Assessment: === | === Objective Assessment: === | ||
Assessment of ligamentous laxity: anterior drawer, talar tilt and ankle syndesmosis. | Assessment of ligamentous laxity: anterior drawer, talar tilt and ankle syndesmosis. | ||
{| | {| border="1" cellpadding="1" cellspacing="1" | ||
|- | |- | ||
| {{#ev:youtube|YyAgAKykgKs|300}} | | {{#ev:youtube|YyAgAKykgKs|300}} | ||
Revision as of 21:01, 13 November 2019
Original Editor - Mariam Hashem
Top Contributors - Mariam Hashem, Kim Jackson, Tarina van der Stockt, Jess Bell and Olajumoke Ogunleye
Introduction[edit | edit source]
Lateral ankle ligament injruy is a common MSK condition representing 85% of ankle injuries [1]and has a high recurrencce rate[1]. Persisting post-injury symptoms such as swelling, impaired strength, instability (occasional giving way), and impaired balance responses for more than 12 months following the initial injury is defined as '' Chronic Ankle Instability-CAI''[2]. Up to 70% of patients report developing chronic ankle instability[3].
Limited dorsiflexion[4], reduced proprioception, reduced isometric abductor hip strength[5], postural control deficiencies on SLS [6] were associated with higher risk of ankle sprain and instability.
The highest incidence of LAS was found for aeroball, basketball, indoor volleyball, field sports and climbing[7].
A systematic review by Hiller et al[8] reported greater larger talar curve, reduced concentric inversion strength, greater sway when standing on stable surfaces with eyes closed, a more inverted ankle position and decreased foot clearance during gait, and prolonged time to stabilisation after a jump.
Assessment[edit | edit source]
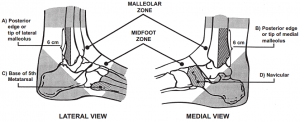
The Ottawa Ankle Rules to determine the need for radiographs in acute ankle injuries. If these rules were positive, the patient/athlete needs an x-ray to rule out fractures.
These rules are as follows:
1-Tenderness on plapation of :
A-posterior edge/dip of lateral malleoulus
B-Posterior edge/dip of medial malleoulus
C-Base of 5th metatarsal
D-Navicular
2-Inability to fully weight bear for normal 4 steps at time of injury or on examination
Subjective Assessment[edit | edit source]
- Mechanism of Injury and WB status. If an athelete was injured during a game, a decision has to be made on return to play based on the MOI and WB status.
- Contributing Factors
- When acute symptoms subside, the Cumberland Ankle Instability Tool can be used to predict the developmene tof CAI. A cut off 11.5 > unlikely to progress . less: high likely to progress
Objective Assessment:[edit | edit source]
Assessment of ligamentous laxity: anterior drawer, talar tilt and ankle syndesmosis.
- Swelling
- Isometric eversion/abduciton
Chronic ankle instability checklist:[edit | edit source]
Identifies a failed outcome of rehabilitation following an ATFL injury and increased risk of developing CAI.
ROM markers:
WB ankle DF < 34 degrees
Strength markers:
isometric hip abduction strength <34% of body weight
Balance-stability markers:
Single-leg balance test <10 seconds and on toes < 5 seconds without wobbliness.
SEBT: measures.
Performance markers:
unable to complete dingle leg drop landing
References[edit | edit source]
- ↑ 1.0 1.1 Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wickstrom EA. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. American journal of sports medicine. 2016.The American Journal of Sports Medicine Vol 45, Issue 1, pp. 201 - 209
- ↑ Fernández-de-las-Peñas C, editor. Manual therapy for musculoskeletal pain syndromes: An evidence-and clinical-informed approach. Elsevier Health Sciences; 2015 Jun 17
- ↑ Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med 2005;39:e14; discussion e14.
- ↑ Pope R, Herbert R, Kirwan J. Effects of ankle dorsiflexion range and pre-exercise calf muscle stretching on injury risk in Army recruits. Australian Journal of Physiotherapy. 1998 Jan 1;44(3):165-72.
- ↑ Powers CM, Ghoddosi N, Straub RK, Khayambashi K. Hip strength as a predictor of ankle sprains in male soccer players: a prospective study. Journal of athletic training. 2017 Nov;52(11):1048-55.
- ↑ Kobayashi T, Yoshida M, Yoshida M, et al. Intrinsic Predictive Factors of Noncontact Lateral Ankle Sprain in Collegiate Athletes: A Case-Control Study. Orthop J SportsMed 2013;1:232596711351816.
- ↑ Waterman BR, Belmont PJ, Cameron KL, et al. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med 2010;38:797–803.
- ↑ Hiller CE, Nightingale EJ, Lin CW, Coughlan GF, Caulfield B, Delahunt E. Characteristics of people with recurrent ankle sprains: a systematic review with meta-analysis. Br J Sports Med. 2011 Jun 1;45(8):660-72.