Anaphylaxis
Original Editor - Wajeeha Hassan
Top Contributors - Wajeeha Hassan, Kim Jackson and Lucinda hampton
Introduction[edit | edit source]
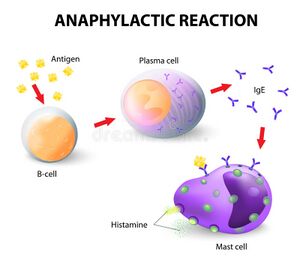
It is a life threatening syndrome that results from sudden release of basophil derived mediators and mast cells into blood circulation. It is a serious allergic reaction which is rapid in onset can lead to even death.
However, no universally accepted clinical definition has been found. According to some clinicians it is defined as a syndrome of one or more than one systemic signs and symptoms but does not identify the specific features alone or in combination.
French physiologist Charles Robert Richet in 1913 was awarded with Nobel prize in Medicine and Physiology for his collaborative research with Paul Portier on anaphylaxis. [1]
Causes[edit | edit source]
Common triggers which can induce an anaphylaxis includes
- Certain foods such as shell fish, peanuts, food additives or spices, tree nuts, beef, pork and almonds etc.
- Medication including Aspirin, Other NSAIDs, β -Lactams, Insulin, Protamine, Codeine, Meperidine, Dextromethorphan, Erythromycin, Methylprednisolone and Salmon calcitonin.
- Exercise induced
- Latex
- insect stings
- Idiopathic[2]
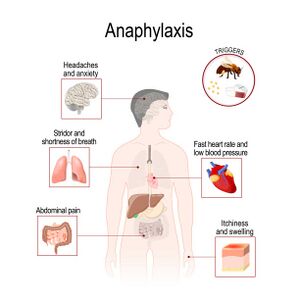
Effected Organs[edit | edit source]
Organs which are most commonly effected in anaphylaxis include
- Skin
- Respiratory tract
- Gastrointestinal tract
- Cardiovascular system
- Central nervous system[3]
Classification[edit | edit source]
It has been classified into 3 categories on basis of severity of symptoms.
- Severe Reactions: It includes clinical features such as confusion, incontinence, collapse and unconsciousness and are associated with hypotension and hypoxia.
- Moderate Reactions: Diaphoresis, presyncope, dyspnea, vomiting, stridor, wheeze, chest tightness, nausea and abdominal pain has weak but significant association and is used to define moderate reactions.
- Mild Reactions: It includes reactions which are limited to skin such as urticaria, erythema, and angioedema. [4]
Treatment[edit | edit source]
Epinephrine is most effective drug in initial treatment of anaphylaxis. This is because epinephrine works as alpha-1 adrenergic agonist and causes vasoconstriction which in turns helps in relieving laryngeal edema , hypotension and shock. [5] If timely injection of epinephrine is not given, it can lead an increased risk of hypoxic ischemic encephalopathy, biphasic anaphylaxis and fatality.[6] World Health Organization has designated the epinephrine as an essential medication for treatment of anaphylaxis and ampules of epinephrine are also available worldwide as compare to epinephrine auto-injectors.[7]
References[edit | edit source]
- ↑ Kemp SF, Lockey RF. Anaphylaxis: a review of causes and mechanisms. Journal of allergy and clinical immunology. 2002 Sep 1;110(3):341-8 https://www.sciencedirect.com/science/article/abs/pii/S0091674902001197
- ↑ Webb LM, Lieberman P. Anaphylaxis: a review of 601 cases. Annals of Allergy, Asthma & Immunology. 2006 Jul 1;97(1):39-43. https://www.sciencedirect.com/science/article/abs/pii/S1081120610613671
- ↑ Simons FE. Anaphylaxis pathogenesis and treatment. Allergy. 2011 Jul;66:31-4.https://onlinelibrary.wiley.com/doi/10.1111/j.1398-9995.2011.02629.x
- ↑ Brown SG. Clinical features and severity grading of anaphylaxis. Journal of Allergy and Clinical Immunology. 2004 Aug 1;114(2):371-6. https://www.sciencedirect.com/science/article/abs/pii/S0091674904013983
- ↑ Simons KJ, Simons FE. Epinephrine and its use in anaphylaxis: current issues. Current opinion in allergy and clinical immunology. 2010 Aug 1;10(4):354-61.https://pubmed.ncbi.nlm.nih.gov/20543673/
- ↑ Simons FE. 9. Anaphylaxis. Journal of Allergy and Clinical Immunology. 2008 Feb 1;121(2):S402-7. https://pubmed.ncbi.nlm.nih.gov/20176258/
- ↑ Simons FE, World Allergy Organization. World Allergy Organization survey on global availability of essentials for the assessment and management of anaphylaxis by allergy-immunology specialists in health care settings. Annals of Allergy, Asthma & Immunology. 2010 May 1;104(5):405-12.https://pubmed.ncbi.nlm.nih.gov/20486330/