Introduction to Cerebral Visual Impairment and Cerebral Palsy
Original Editor - Ewa Jaraczewska based on the course by Angela Kiger
Top Contributors - Ewa Jaraczewska, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Cerebral visual impairment (CVI) occurs in children with cerebral palsy (CP) or developmental delay. [1] Children with CVI have been frequently diagnosed with cerebral palsy. Despite the importance of early diagnosis, there is no standardised assessment tool to diagnose CVI and one referral criteria guideline. [1] The challenge in early diagnosis comprises a wide range of visual dysfunctions present in CVIs. They include central and peripheral vision dysfunction, dysfunctions in movement perception, gaze control, visual guidance of movement, visual attention, attentional orientation in space, visual analysis and recognition, visual memory and spatial cognition, which can affect a child's learning and social interactions. [2]This article presents an overview of CVI and its relationship with cerebral palsy.
Definitions[edit | edit source]
Cerebral Visual Impairment[edit | edit source]
Cerebral Visual Impairment (CVI) is “a verifiable visual dysfunction, which cannot be attributed to disorders of the anterior visual pathways or any potentially co-occurring ocular impairment.” [3]
Cerebral Palsy[edit | edit source]
Cerebral Palsy (CP) "describes a group of permanent disorders of the development of movement and posture causing activity limitation, which is attributed to non-progressive disturbances that occurred in the developing fetal or infant brain."[4]
Brain Involvement in Vision[edit | edit source]
"It is estimated that over 50% of the brain is involved in vision processing." [5] --Angela Kiger
The following example explains the process of the brain controlling the eyesight:
Example: the child plays the game of ball catching:[5][6][2]
- The child sees the ball
- The frontal lobe of the brain decides about taking the action of ball catching and decides about its strategy.
- The occipital lobe process the information received through the eyes. It passes the processed image data to the posterior parietal lobes via the superior longitudinal fasciculi.
- The middle part of the temporal lobe supports this process, together with the posterior thalamus and superior colliculi, facilitating visual search and visual guidance of movement.
- The ball is identified and chosen for the target.
- The parietal lobe gauges the distance between the child's hands and the ball. If this is not the child's first involvement in this game, the temporal lobe takes part in the process as it controls memory. It subconsciously reminds the child that their hands are used to catch the ball, that he needs to reach out, and that his body needs to adjust.
- The temporal lobes via a bundle of nerve fibres on each side, process the local and detailed visual feedback.
- The child involves his cerebellum to adjust his actions' timing and balance.
Epidemiology[edit | edit source]
- CVI affect at least 3.4% of children. However, the number may be higher as many affected children go unidentified. [7]
- More than 50% of children with learning difficulties who attend special schools have CVI. [7]
- CVI is present in 2 per 1000 live births and 19 per 1000 live births for infants born at 20-27 weeks gestation, with subcortical damages being more common in preterms. [8][9]
- Most common cause of permanent vision loss in children 1-3 years old.[5]
- Almost 50% of the children diagnosed with a visual impairment have CVI. [5]
- 56% of individuals with CVI have additional disabilities. [5]
Aetiology[edit | edit source]
The aetiology of CVI in children can be either prenatal, perinatal or postnatal:[10]
Prenatal:
- hydrocephalus
- congenital central nervous system malformation
Perinatal:
- hypoxic ischemic injury
- genetic/chromosomal disorders
- metabolic disorders
- infection during pregnancy
- neonatal hypoglycemia
- medication during pregnancy
Postnatal:
- meningitis
- encephalitis
- brain tumours
- cerebrovascular accidents
- seizures
- periventricular leukomalacia
- cardiac arrest
- cranio-cerebral trauma
Brain Damage and CVI[edit | edit source]
The brain damage in patients with CVI can be categorised as subcortical, cortical or both.
Brain lesions resulting in CVI can affect the following parts of the brain:
- the posterior visual pathways (the visual cortex of the occipital lobe)
- the optic chiasm ("part of the brain where the optic nerves cross" [11])
- lateral geniculate bodies (a structure in the thalamus)
- optic radiations ("key white matter structures that cross the temporal lobe"[12])
- primary visual cortices (part of the occipital lobe that processes visual information)
- the middle temporal lobes
- the visual association areas
The following video explains the role of the visual association areas:
Characteristics of CVI[edit | edit source]
The symptoms of CVI and the severity of visual impairment vary in children. They can affect the following:[10]
- sensory visual function: it enables an individual "to be aware of colour, light level, contrast, motion and other visual stimuli".[14]
- oculomotor function: "the ability to use the eyes systematically to efficiently scan and locate an object in the field of vision." [15]
- visual-motor function: "integration between visual perception and motor skills."[16]
- cognitive visual function: ability to analyse and process visual information. [17]
Other characteristics of CVI are as follow:
- can occur in isolation or association with eye or optic nerve damage
- when thalamus is involved than the lack of vision tends to be profound
Symptoms of CVI[edit | edit source]
The child with CVI diagnosis presents with the following:[5]
- Often have a normal or near normal eye exam
- Has a history or presence of a neurological disorder
- Demonstrates behavioural responses to visual stimuli unique to CVI
- Has difficulty to sustain gaze
- Head tilted slightly forward and tilted to the side as a common presentation
Behavioural Changes[edit | edit source]
Children diagnosed with CVI can demonstrate specific behavioural signs:[18]
- short visual attention span
- markedly fluctuating visual performances
- the need for time, environmental stability, and repetition of items to obtain the best response
Diagnosis and Assessment[edit | edit source]
Admission Referral[edit | edit source]
Children are referred to a specialist or specialists for assessment of visual impairment because: [1]
- the parents are concerned about child's visual functioning
- they have an increased risk on CVI
- they have intellectual disability or syndrome who can be screened on visual functioning.
Multidisciplinary Team[edit | edit source]
The multidisciplinary team for CVI diagnostics is necessary for accurate and timely diagnosis. The team should include the following specialties at the minimum:
- pediatric ophthalmologist
- pediatric neurologist
- orthoptist or optometrist
- neuropsychologist.
Follow-up Referral[edit | edit source]
The assessment results should be discussed with all members of the multidisciplinary team. Based on the outcome, the child can be referred to:[1]
- Vision Teacher and Developmental Therapist Vision Specialization in CVI
- Rehabilitation center or a specialized center
- School for visually impaired children if there is evidence of CVI
Assessment Tools[edit | edit source]
There is no standardised assessment tool for diagnosis of CVI. The following assessment tools are recommended:[19]
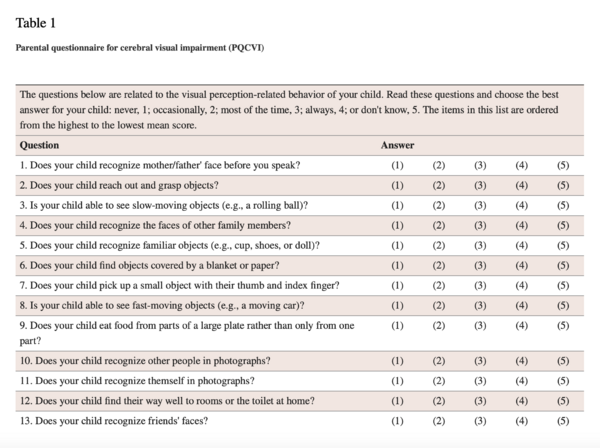
- Questionnaires
- Parental questionnaire for cerebral visual impairment (PQCVI)
- The CVI Questionnaire: 46 item screening questionnaire. [20]
- The Five Questions completed by a parent. 5-point Likert Scale describes if the child ‘always’, ‘often’, ‘sometimes’, ‘rarely’ or ‘never’ struggles with the described tasks.[20]
- Functional vision assessment (CVI Range)
- "Behavioural assessment of functional vision, which defines the ability to interpret and react to visual information"[21]
- Assessment based on observation, parent interview and direct assessment
- The evaluator grades the child on 10 characteristics of CVI:[21]
- Colour preference.
- Need for movement.
- Visual latency.
- Visual field preferences.
- Difficulties with visual complexity.
- Need for light.
- Difficulty with distance viewing.
- Atypical visual reflexes.
- Difficulty with visual novelty.
- Absence of visually guided reach.
- Scores range from 0 to 10, when 0 represents no functional vision, and 10 means typical or near typical functional vision
- Neuropsychological assessment in children with possible CVI
- no consensus in diagnostic protocol
- Neuropsychological tests of visual perception [22]
- Eye tracking
- Genetic Assessment
- Neuroradiological Evaluation and Magnetic Resonance Imaging (MRI)
- recording of the damage of those parts of the brain involved in visual processing
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Boonstra FN, Bosch DGM, Geldof CJA, Stellingwerf C, Porro G. The Multidisciplinary Guidelines for Diagnosis and Referral in Cerebral Visual Impairment. Front Hum Neurosci. 2022 Jun 30;16:727565.
- ↑ 2.0 2.1 Chokron S, Kovarski K, Dutton GN. Cortical Visual Impairments and Learning Disabilities. Front Hum Neurosci. 2021 Oct 13;15:713316.
- ↑ Sakki HEA, Dale NJ, Sargent J, Perez-Roche T, Bowman R. Is there consensus in defining childhood cerebral visual impairment? A systematic review of terminology and definitions. Br J Ophthalmol. 2018 Apr;102(4):424-432.
- ↑ Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, Dan B, Jacobsson B. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007 Feb;109:8-14. Erratum in: Dev Med Child Neurol. 2007 Jun;49(6):480.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Kiger A. Cerebral Visual Impairment and Cerebral Palsy. Plus Course 2023.
- ↑ Debrowski A. How does the brain control eyesight? (2020) Available from https://www.allaboutvision.com/resources/part-of-the-brain-controls-vision/ [last access 26.11.2023]
- ↑ 7.0 7.1 Williams C, Pease A, Warnes P, Harrison S, Pilon F, Hyvarinen L, West S, Self J, Ferris J; CVI Prevalence Study Group. Cerebral visual impairment-related vision problems in primary school children: a cross-sectional survey. Dev Med Child Neurol. 2021 Jun;63(6):683-689.
- ↑ Robertson CM, Watt MJ, Dinu IA. Outcomes for the extremely premature infant: what is new? And where are we going? Pediatr Neurol. 2009 Mar;40(3):189-96.
- ↑ Hoyt CS, Fredrick DR. Cortically visually impaired children: a need for more study. Br J Ophthalmol. 1998 Nov;82(11):1225-6.
- ↑ 10.0 10.1 Kozeis N. Brain visual impairment in childhood: mini review. Hippokratia. 2010 Oct;14(4):249-51.
- ↑ Ireland AC, Carter IB. Neuroanatomy, Optic Chiasm. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542287 [last access 26.11.2023]
- ↑ Rodrigues EM, Isolan GR, Becker LG, Dini LI, Vaz MAS, Frigeri TM. Anatomy of the optic radiations from the white matter fibre dissection perspective: A literature review applied to practical anatomical dissection. Surg Neurol Int. 2022 Jul 22;13:309.
- ↑ Neuro-Ophthalmology with Dr. Andrew G. Lee. Visual association cortex. Available from: https://www.youtube.com/watch?v=pD_kAQ6Et5Y[last accessed 26/11/2023]
- ↑ How the Visual Sensory System Works - HandsOn OT. Available from https://handsonotrehab.com/visual-sensory-system/ [last access 26.11.2023]
- ↑ What Are Oculomotor Skills? (2022). Available from https://llatherapy.org/what-are-oculomotor-skills/ [last access 26.11.2023]
- ↑ Stevens A, Bernier R. Visual-Motor Function. In: Volkmar, F.R. (eds) Encyclopedia of Autism Spectrum Disorders. Springer, New York, NY.
- ↑ Fazzi E, Bova S, Giovenzana A, Signorini S, Uggetti C, Bianchi P. Cognitive visual dysfunctions in preterm children with periventricular leukomalacia. Dev Med Child Neurol. 2009 Dec;51(12):974-81.
- ↑ Boonstra FN, Bosch DGM, Geldof CJA, Stellingwerf C, Porro G. The Multidisciplinary Guidelines for Diagnosis and Referral in Cerebral Visual Impairment. Front Hum Neurosci. 2022 Jun 30;16:727565.
- ↑ Chang M, Borchert M. Methods of visual assessment in children with cortical visual impairment. Current Opinion in Neurology, 2021; 34(1):p 89-96.
- ↑ 20.0 20.1 Gorrie F, Goodall K, Rush R, Ravenscroft J. Towards population screening for Cerebral Visual Impairment: Validity of the Five Questions and the CVI Questionnaire. PLoS One. 2019 Mar 26;14(3):e0214290.
- ↑ 21.0 21.1 Chang M, Roman-Lantzy C, O’Neil SH, Reid MW, Borchet MS. Validity and reliability of CVI Range assessment for Clinical Research (CVI Range-CR): a longitudinal cohort study. BMJ Open Ophthalmology 2022;7:e001144.
- ↑ Lanca M, Jerskey BA, O'Connor MG. Neuropsychologic assessment of visual disorders. Neurol Clin. 2003 May;21(2):387-416.
- ↑ Spencer RJ, Wendell CR, Giggey PP, Seliger SL, Katzel LI, Waldstein SR. Judgment of Line Orientation: an examination of eight short forms. J Clin Exp Neuropsychol. 2013;35(2):160-6.
- ↑ Zhang X, Lv L, Min G, Wang Q,Zhao Y, Li Y. Overview of the Complex Figure Test and Its Clinical Application in Neuropsychiatric Disorders, Including Copying and Recall. Front. Neurol.,2021;12.