Achilles Tendinopathy Toolkit: Section A - Clinical Evaluation
Introduction[edit | edit source]
The purpose of this document is to summarize the clinical evaluation of somebody who has been diagnosed with Achilles Tendinopathy.
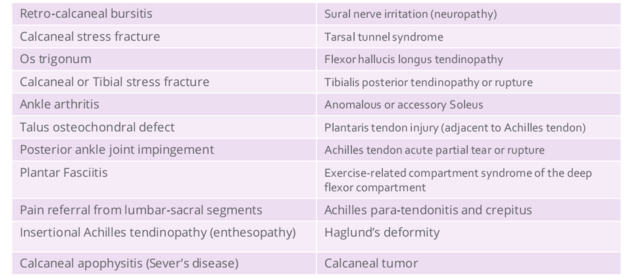
The first steps involved in assessing a person presenting with Achilles tendinopathy is to carry out a subjective and objective examination, including a detailed history, to confirm the diagnosis. The toolkit leads you through the process of identifying potential risk factors association with Mid-Portion Achilles Tendinopathy, important questions and observations that form part of the subjective and objective assessment, as well as discussing Functional Tests and Differential Diagnosis.
Risk Factors[edit | edit source]
There are potential risk factors associated with mid-portion achilles tendinopathy. These can be further classified as non-modifiable and modifiable risk factors:
- Non-Modifiable Risk Factors
- mid-age 30-60 years [ref 3,5]
- male>female [ref 6]
- Metabolic Disorders:
- Renal disease [ref 3] - Urate deposits (tophi) in the Achilles tendon related to hyperuricemia (gout) [ref 7]
- Diabetes [ref 3]
- Family history:
- Familial Hypercholesterolemia (HeFH) [ref 3] - New onset of Achilles tendon pain is often the first sign of hypercholesterolemia and should be investigated for serum cholesterol levels. [ref 7]. Tendon Xanthomas are fatty deposits from high cholesterol levels and commonly found at the Achilles tendon.
- Genetic variants [ref 2,3] -Certain genetic polymorphisms predispose tendon to altered collagen structure.
- Systemic Inflammatory Disorder:
- Seronegative Spondyloarthropathy (SpA) - 98% of SpAhave at least one enthesis disorder, commonly at the Achilles tendon.[ref 9]. Consider use of SpAscreening tools such as SCREEND’EM [ref 9]
- Modifiable Risk Factors
- Lifestyle:
- Medications:
- Fluoroquinolones [ref 2] - Specifically, Ofloxacin was identified compared to similar anti-biotics from the same drug group. [ref 1]
- Systemic corticosteroid (long term Prednisone) [ref 10]
- Hormone Replacement Therapy (HRT) [ref 5]
- Previous lower extremity tendinopathy [ref 1]
- Footwear [ref 2,4,5]
- Biomechanics:
- Limited dorsiflexion [ref 2,4,5]
- Decreased plantar flexor strength [ref 2,4,5]
- Limited hip mobility [ref 2]
- Altered gait pattern [ref 2]
- Foot posture and mechanics [ref 5] - Static exam: hindfoot INV/EV (subtalar mobility)[ref 5]
- Dynamic exam: excess foot pronation [ref 2]
- Training Errors:
- Training load - abrupt change in load, intensity, or volume [ref 4]
- Training environment - higher risk with cold weather and winter training season [ref 1]
Assessment[edit | edit source]
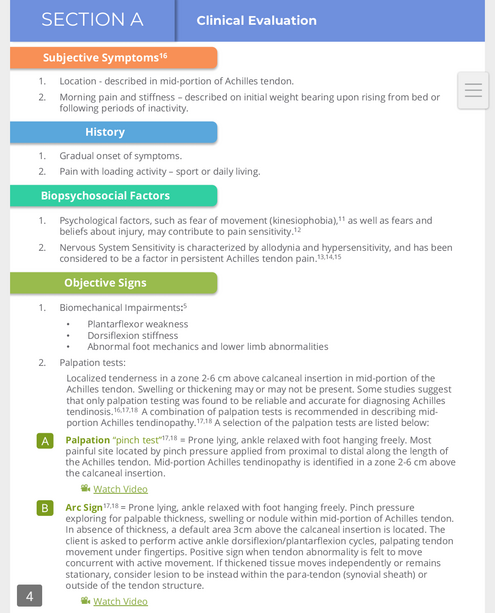
Things to look out for when assessing for achilles tendinopathy include; the subjective symptoms from patients, onset of injury, objective signs and psychological factors.
- Click to go back to the Main Achilles Tendinopathy Toolkit page
- Click to continue to Section B - Outcome Measures
- Click to continue to Section C - Summary of Evidence and Recommendations for Interventions
- Click to continue to Section D - Exercise Programs
- Click to continue to Section E - Low Level Laser Therapy Dosage Calculation
- Click to continue to Section F - Medical and Surgical Interventions