Hemiplegic Shoulder Subluxation
Original Editor - Fasuba Ayobami
Top Contributors - Vaibhav Panchal, Manisha Shrestha, Fasuba Ayobami, Yesmine Gouddi, Kim Jackson, Lucinda hampton, Mohamed Abdelraof Mohamed, Candace Goh, Shreya Pavaskar, Robin Tacchetti, Dinu Dixon, Naomi O'Reilly, Mariam Hashem, Amanda Ager and Lauren Lopez
Introduction[edit | edit source]
Shoulder subluxation is one of the major complications experienced among stroke survivors.Glenohumeral subluxation (GHS) is a inferior displacement of humeral head from the glenoid fossa. [2] The glenohumeral joint is the most vulnerable joint in the shoulder complex to sublux due to its anatomical structure being stabilized only by surrounding muscles, the joint capsules and ligamentous structures.Also as an extremely mobile joint, it sacrifices stability for mobility.[3][4]
The association between GHS and other poststroke complications such as pain and poor motor recovery is uncertain.[5] But in long term due to GHS may lead to the adhesive capsulitits, reduce proprioception causing shoulder pain that increase over time. This may delay the recovery of upper extremity function and a key factor in post-stroke disability is the involvement of the upper limb.[6][7]
On this page, emphasis is centred on Physical therapy management. Kindly refer to Shoulder Subluxation for more details.
Epidemiology[edit | edit source]
The incidence of shoulder subluxation in patients following a stroke varies from 7–81% (depending on the measurement methods used and the time frames over which it is assessed) and 73% occur in the acute stage In a 10-month follow-up study, shoulder subluxation was shown to be further aggravated in 67% of patients over time. [6]
Pathomechanics and Risk factors[edit | edit source]
Studies had shown that the supraspinatus, and to a lesser extent the posterior deltoid muscles, played a key role in maintaining glenohumeral alignment and in preventing downward subluxation of the humerus.[8]
In 1959, Basmajian and Bazant offered a theory to explain the development of GHS . During the flaccid stage, the trunk tends to lean or shorten toward the hemiplegic side, which causes the scapula to descend from its normal horizontal level. The trapezium and the serratus anterior also become flaccid, causing the scapula to rotate downwardly. Without normal tone, the rotator cuff can no longer maintain the integrity of the GHJ. These conditions contribute to a subluxing GHJ. During the spastic stage, the pectoralis major and minor, rhomboideus, elevator scapulae, and latissimus dorsi can become hypertonic, further rotating the scapula downward, causing GHS. In contrary, other studies had not shown a relationship between scapular orientation and GHS. Severe loss of motor function and apparent absence of supraspinatus muscle contraction are potential risk factors for GHS, [8]
Other factors contributing to subluxation include improper positioning, lack of support in the upright position, and pulling on the hemiplegic arm when the patient is transferred.[8]
Assessment[edit | edit source]
Several method for the assessment of Shoulder subluxation.
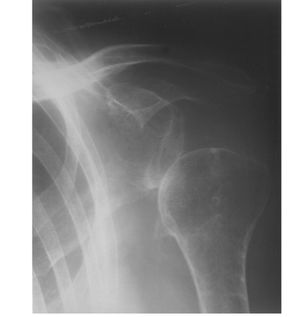
Radiographic measurements ( X- ray and ultrasound ) considered a standard measurement, have been used in several studies to assess the effectiveness of therapy or development of GHS over time. But due to the several problems, such as costs, exposure to radiation, specialized eqiupments or delayed feedback for therapeutic choices, make measurements difficult to put into practice in many clinical settings.[8][5]
So other method commonly used is Fingerbreadth palpation method.
Fingerbreadth Palpation Method[edit | edit source]
Patients were seated in a chair or wheelchair with both feet flat on the ground or on a footrest. The physical therapist first assessed the unaffected side to palpate the gap between the acromion and the head of the humerus, and this assessment was repeated on the affected shoulder. Shoulders were positioned in neutral rotation, with the arm hanging by the side (thumb pointing forward) close to the body with no abduction ([null Fig. 1]). Some patients who demonstrated high tone were unable to hang their affected arm freely by the side. For these patients, the shoulder was maintained in internal rotation with slight elbow flexion and the forearm resting on their lap. Glenohumeral subluxation was defined as a palpable gap between the inferior aspect of the acromion and the superior aspect of the humeral head that is ½ fingerbreadth or more. A 0–5 grading scheme was used:
0=no subluxation,
1=½ fingerbreadth gap,
2=1 fingerbreadth gap,
3=1½ fingerbreadth gap,
4=2 fingerbreadth gap, and
5=2½ fingerbreadth gap.[5]
Evidence Based Physical Therapy Management[edit | edit source]
Acute Management[edit | edit source]
- Education: Caregivers/Health Professionals/Relatives need to be informed on the importance of proper handling of the arm. Stroke patients who have their arm unsupported and/or handled inappropriately by caregivers (pulling on the arm) are at a higher risk for traction neuropathy and injury. Hence, it is essential that caregivers of stroke survivors are adequately trained in handling the hemiplegic arm especially when shoulder subluxation is present.[2][7][9]
- Positioning: Lap trays, Pillows and foam support help to keep the arm and shoulder supported in the correct position. Good positioning will help reduce strain on your ligaments and prevent frozen shoulder from occurring.[2][7][10]
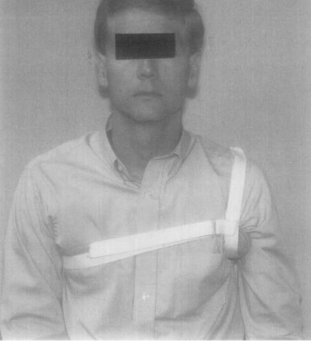
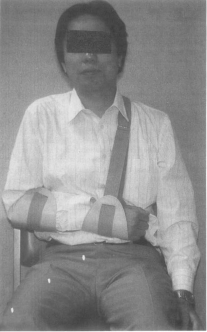
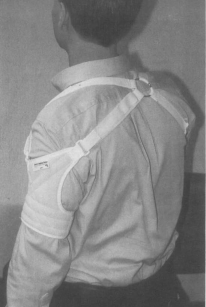
- Orthotic devices: The use of shoulder supports is common early after stroke to decrease glenohumeral subluxation and support the shoulder joint. Examples of shoulder supports are the Henderson shoulder ring, Bobath roll, Harris hemi-sling, Rolyan humeral cuff sling, Cavalier shoulder support, arm trough or lapboard and shoulder strapping.[2] A study conducted by Nadler et al found reducing vertical subluxation with a shoulder orthoses may reduce hemiplegic shoulder pain. Orthosis with proximal and distal attachments are more effective.[11] In addition, care must be take in its usage to avoid contractures.
- Taping:A study conducted by Chatterjee et al found California Tri-pull Taping method to reduces pain, improves active shoulder flexion, and improves distal UE functional ability. This appears to be a promising early adjunctive treatment for clients who have suffered a stroke and demonstrate pain in a subluxed shoulder. This taping method allows the patients to participate in all active UE exercises as well as all ADL's. However, there was no follow-up to determine if the effects demonstrated were maintained.[17]
- Neuro-muscular Electrical Stimulation:
Electrical stimulation can prevent shoulder subluxation and decrease shoulder pain in acute phase, but this effect was not maintained after the withdrawal of treatment in later follow ups.[3]
| Indication | Patient Position | Electrode Placement | Parameter Recommendations |
|---|---|---|---|
| Prevention or treatment of
shoulder sublux resulting from UE flaccidity poststroke |
Patient sitting with arm support | One channel over muscle belly of supraspinatus
and posterior deltoid. Avoid upper trapezius fibres and excessive shoulder shrug. Applying a second channel to stimulate the long head of biceps can be beneficial in correcting humeral head alignment. |
NMES waveform: symmetric or asymmetric biphasic PC
Frequency: 30–35 Hz Pulse duration: 250–350 ms Current amplitude: sufficient to produce a smooth,sustained muscle contraction and reduction of shoulder sublux Work–rest cycle: ON:OFF 10–15 s ON time with progressively shorter rest time (30 s ON time, 2 s OFF time). Rampup time (1–4 s) is set to ensure patient comfort; longer ramp-down time may be required to prevent pain or tissue stretching when the arm sags due to gravity. Treatment schedule: progress to 2–4 h/d on the basis of muscle fatigue Session frequency: 7 d/wk for 4–6 wk or until voluntary control has been restored |
- Exercises: In the early phase of rehabilitation passive range of motion exercises has been shown to be effective in preventing shoulder subluxation among stroke patients. Range-of-motion exercises for the shoulder joint include flexion-extension, abduction-adduction and external-internal rotation. It is important to know that if the exercises are improperly carried out, it can cause injury to the shoulder and increase the stroke patient’s risk for shoulder subluxation.[2] Also, weight bearing exercises on the affected upper extremity proved to be beneficial. From a seated position on your bed or bench, prop yourself up on your affected arm by placing your affected arm about a foot away from your body. Then lean into it. If the patient feels comfort, this position should last for 10 seconds or so. And if otherwise, it should be stopped immediately.[10]
Chronic Management[edit | edit source]
Proper positioning/good handling techniques should continue in this phase of management. Stroke survivors need to be reminded periodically on the rationale behind it. Although Shoulder supports are used commonly during the rehabilitation of stroke survivors, there is no absolute evidence that supports prevent or reduce long-term shoulder subluxation when spontaneous recovery of motor function occurs, or that a support will prevent supposed complications of shoulder subluxation. Without proper training in the use of a support, stroke survivors may face potential complications such as pain or contracture.[12] NMES can reduce existing sublux even 6 mo post-stroke; however, the likelihood of improvement markedly reduces with time post-stroke[19] Strength training can be used to build the muscles surrounding the affected UE. It involves progressive active exercises against resistance. Strength training on upper limb, function and ADL performance following stroke; there was a significant effect associated with training. [20] Patients with subluxed shoulder can be treated with Task-specific practice. The best way to relearn a given task is to retrain for that task.Task-specific, low-intensity regimens designed to improve use and function of affected limb have reported significant improvements.[20]
Resources[edit | edit source]
References[edit | edit source]
- ↑ Linn SL, Granat MH, Lees KR. Prevention of shoulder subluxation after stroke with electrical stimulation. Stroke. 1999 May;30(5):963-8.
- ↑ 2.0 2.1 2.2 2.3 2.4 Seneviratne, Cydnee; Then, Karen L.; Reimer, Marlene. Post-stroke shoulder subluxation: A concern for neuroscience nurses. AXON/ L'AXONE . Sep2005, Vol. 27 Issue 1, p26-31.
- ↑ 3.0 3.1 Linn SL, Granat MH, Lees KR. Prevention of shoulder subluxation after stroke with electrical stimulation. Stroke. 1999 May;30(5):963-8.
- ↑ Dohle CI, Rykman A, Chang J, Volpe BT. Pilot study of a robotic protocol to treat shoulder subluxation in patients with chronic stroke. Journal of neuroengineering and rehabilitation. 2013 Dec;10(1):88.
- ↑ 5.0 5.1 5.2 Kumar P, Mardon M, Bradley M, Gray S, Swinkels A. Assessment of glenohumeral subluxation in poststroke hemiplegia: Comparison between ultrasound and fingerbreadth palpation methods. Physical therapy. 2014 Nov 1;94(11):1622-31.
- ↑ 6.0 6.1 Jung KM, Choi JD. The Effects of Active Shoulder Exercise with a Sling Suspension System on Shoulder Subluxation, Proprioception, and Upper Extremity Function in Patients with Acute Stroke. Medical science monitor: international medical journal of experimental and clinical research. 2019;25:4849.
- ↑ 7.0 7.1 7.2 https://www.stroke-rehab.com/shoulder-subluxation.html (Accessed 6th May, 2018)
- ↑ 8.0 8.1 8.2 8.3 Paci M, Nannetti L, Rinaldi LA. Glenohumeral subluxation in hemiplegia: An overview. Journal of Rehabilitation Research & Development. 2005 Jul 1;42(4).
- ↑ Pamela W. Duncan, Richard Zorowitz, Barbara Bates, John Y. Choi, Jonathan J. Glasberg, Glenn D. Graham, Richard C. Katz, Kerri Lamberty, Dean Reker. Management of Adult Stroke Rehabilitation CareA Clinical Practice Guideline. Stroke. 2005;36:e100-e143, originally published August 24, 2005
- ↑ 10.0 10.1 https://www.flintrehab.com/2016/shoulder-rehab-exercises-to-alleviate-pain-and-improve-mobility/ (Accessed on 6th May, 2018)
- ↑ Nadler M, Pauls M. Shoulder orthoses for the prevention and reduction of hemiplegic shoulder pain and subluxation: systematic review.Cline Rehabil. 2017 Apr;31(4):444-453. doi: 10.1177/0269215516648753. Epub 2016 Jul 10.
- ↑ 12.0 12.1 Zorowitz RD, Idank D, Ikai T, Hughes MB, Johnston MV. Shoulder subluxation after stroke: a comparison of four supports. Arch Phys Med Rehabil 1995;76:763-71.
- ↑ Zorowitz RD, Idank D, Ikai T, Hughes MB, Johnston MV. Shoulder subluxation after stroke: a comparison of four supports. Arch Phys Med Rehabil 1995;76:763-71.
- ↑ Zorowitz RD, Idank D, Ikai T, Hughes MB, Johnston MV. Shoulder subluxation after stroke: a comparison of four supports. Arch Phys Med Rehabil 1995;76:763-71.
- ↑ Zorowitz RD, Idank D, Ikai T, Hughes MB, Johnston MV. Shoulder subluxation after stroke: a comparison of four supports. Arch Phys Med Rehabil 1995;76:763-71.
- ↑ https://www.givmohrsling.com/images/instPictNum%201-h350.jpg (Accessed 6th May 2018)
- ↑ Subhasish Chatterjee, Kate A Hayner, Narkeesh Arumugam, Manu Goyal, Divya Midha, Ashima Arora, Sorabh Sharma, Senthil P Kumar. The California Tri-pull Taping Method in the Treatment of Shoulder Subluxation After Stroke: A Randomized Clinical Trial.N Am J Med Sci. 2016 Apr;8(4):175-82. doi: 10.4103/1947-2714.179933
- ↑ Subhasish Chatterjee, Kate A Hayner,1 Narkeesh Arumugam,2 Manu Goyal, Divya Midha, Ashima Arora, Sorabh Sharma, and Senthil P Kumar. The California Tri-pull Taping Method in the Treatment of Shoulder Subluxation After Stroke: A Randomized Clinical Trial. N Am J Med Sci. 2016 Apr;8(4):175-82. doi: 10.4103/1947-2714.179933
- ↑ 19.0 19.1 Ethne L. Nussbaum, Pamela Houghton, Joseph Anthony,Sandy Rennie, Barbara L. Shay, Alison M. Hoens.Neuromuscular Electrical Stimulation for Treatment of Muscle Impairment: Critical Review and Recommendations for Clinical Practice. Physiotherapy Canada Special Issue 2017; 69;1–76; doi:10.3138/ptc.2015-88
- ↑ 20.0 20.1 Robert Teasell, Norhayati Hussein. Chapter 4. Motor Rehabilitation. Stroke Rehabilitation Clinician Handbook 2016. www.ebrsr.com