Effects of Ageing on Hand Function: Difference between revisions
Kim Jackson (talk | contribs) m (Text replacement - "[[Metabolic/Endocrine Disorders" to "[[Metabolic and Endocrine Disorders") |
Mohit Chand (talk | contribs) (w2d1 content review and edit) |
||
| Line 6: | Line 6: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
[[File: | [[File:Old client.jpg|thumb|330x330px|Age-Induced Hand Impairment]] | ||
[[Wrist and Hand|Hand]] function decreases with age in both men and women, especially after the age of 65 years. Deterioration in hand function in the elderly population is, to a large degree, secondary to age-related degenerative changes in the musculoskeletal, vascular, and nervous systems. Deterioration of hand function in elderly adults is a combination of local structural changes ([[Joint Classification|joints]], [[muscle]], [[Tendon Anatomy|tendon]], [[Bone|bone,]] nerve and receptors, blood supply, skin, and fingernails) and more distant changes in neural control. These age-related changes are often accompanied by underlying pathological conditions ([[osteoporosis]], [[osteoarthritis]], [[Rheumatoid Arthritis|rheumatic arthritis]], and [[Parkinson's|Parkinson's disease]]) that are common in the elderly population<ref name=":0">Carmeli E, Patish H, Coleman R. [https://academic.oup.com/biomedgerontology/article/58/2/M146/593573 The aging hand]. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2003 Feb 1;58(2):M146-52. Available from:https://academic.oup.com/biomedgerontology/article/58/2/M146/593573 (accessed 16 March 2020)</ref>. | [[Wrist and Hand|Hand]] function decreases with age in both men and women, especially after the age of 65 years. Deterioration in hand function in the elderly population is, to a large degree, secondary to age-related degenerative changes in the musculoskeletal, vascular, and nervous systems. Deterioration of hand function in elderly adults is a combination of local structural changes ([[Joint Classification|joints]], [[muscle]], [[Tendon Anatomy|tendon]], [[Bone|bone,]] nerve and receptors, blood supply, skin, and fingernails) and more distant changes in neural control. These age-related changes are often accompanied by underlying pathological conditions ([[osteoporosis]], [[osteoarthritis]], [[Rheumatoid Arthritis|rheumatic arthritis]], and [[Parkinson's|Parkinson's disease]]) that are common in the elderly population<ref name=":0">Carmeli E, Patish H, Coleman R. [https://academic.oup.com/biomedgerontology/article/58/2/M146/593573 The aging hand]. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2003 Feb 1;58(2):M146-52. Available from:https://academic.oup.com/biomedgerontology/article/58/2/M146/593573 (accessed 16 March 2020)</ref>. | ||
Age and grip strength are significant predictors of hand dexterity Aiming and tapping hand dexterity (involving rapid, coordinated, goal-directed actions) is moderated by the factor of grip strength more than age | === Hand Dexterity === | ||
Hand dexterity is a term used to explain a range of different hand abilities and performances. These include reaction time; hand preference; wrist flexion speed; finger tapping speed; aiming; hand stability and arm stability. Age and grip strength are significant predictors of hand dexterity. | |||
Aiming and tapping hand dexterity (involving rapid, coordinated, goal-directed actions) is moderated by the factor of grip strength more than age i.e. [https://www.keckmedicine.org/blog/5-hand-exercises-to-help-you-maintain-your-dexterity-flexibility/ hand exercises] may improve particular types of hand dexterity. <ref>Martin JA, Ramsay J, Hughes C, Peters DM, Edwards MG. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4331509/ Age and grip strength predict hand dexterity in adults.] PloS one. 2015;10(2):e0117598</ref> | |||
=== Musculoskeletal Hand Problems in Older Adults === | |||
* Musculoskeletal hand problems are common in the population aged over 50 yrs. | * Musculoskeletal hand problems are common in the population aged over 50 yrs. | ||
* Hand function seems to remain stable until age 65 years, after which it gradually reduces. | * Hand function seems to remain stable until age 65 years, after which it gradually reduces. | ||
* After age 75 years, age differences in performance | * [https://pubmed.ncbi.nlm.nih.gov/2818041/ Prehension] pattern selection did not seem to differ with age. | ||
* Statistically significant differences in age were found for prehension pattern frequency, hand strength, and performance time''.'' | |||
* After age 75 years, age differences in performance are apparent.<ref><section> | |||
American Journal of Occupational Therapy, September 1992, Vol. 46, 785-792.[https://ajot.aota.org/article.aspx?articleid=1875308 Effects of Aging on Adult Hand Function] https://doi.org/10.5014/ajot.46.9.785 (last accessed 16.3.2020) | American Journal of Occupational Therapy, September 1992, Vol. 46, 785-792.[https://ajot.aota.org/article.aspx?articleid=1875308 Effects of Aging on Adult Hand Function] https://doi.org/10.5014/ajot.46.9.785 (last accessed 16.3.2020) | ||
</section>Shiffman LM. Effects of aging on adult hand function. Am J Occup Ther. 1992;46(9):785–792. doi:10.5014/ajot.46.9.785 | </section>Shiffman LM. Effects of aging on adult hand function. Am J Occup Ther. 1992;46(9):785–792. doi:10.5014/ajot.46.9.785 | ||
</ref> | </ref> | ||
* Most are | * Most are painful and have a significant impact on everyday life. | ||
* Women | * Women that are very old are especially vulnerable to the effect of hand problems on their daily activities.<ref>Dziedzic K, Thomas E, Hill S, Wilkie R, Peat G, Croft PR. [https://academic.oup.com/rheumatology/article/46/6/963/2899444 The impact of musculoskeletal hand problems in older adults: findings from the North Staffordshire Osteoarthritis Projec]t (NorStOP). Available from:https://academic.oup.com/rheumatology/article/46/6/963/2899444 (accessed 16 March 2020)</ref> | ||
=== Factors Affecting Function in Aging Hands === | === Factors Affecting Function in Aging Hands === | ||
Extrinsic Factors | [[File:Rheumatoid Arthritis hand.jpeg|thumb|406x406px|Rheumatic Hand]] | ||
==== Extrinsic Factors ==== | |||
* Environmental factors (ultraviolet radiation, chemical irritants) | * Environmental factors (ultraviolet radiation, chemical irritants) | ||
* [[Physical Activity|Physical activities]] (work-related, recreational sports, and hobbies) | * [[Physical Activity|Physical activities]] (work-related, recreational sports, and hobbies) | ||
* [[Nutrition]] | * [[Nutrition]] | ||
* Traumatic injuries | * Traumatic injuries | ||
Intrinsic Factors | ==== Intrinsic Factors ==== | ||
* Genetic factors | * Genetic factors | ||
* [[Metabolic and Endocrine Disorders|Endocrine factors]] | * [[Metabolic and Endocrine Disorders|Endocrine factors]] | ||
* [[Metabolic and Endocrine Disorders|Metabolic disorders]] | * [[Metabolic and Endocrine Disorders|Metabolic disorders]] | ||
* Diseases ([[osteoarthritis]], [[Rheumatoid Arthritis|rheumatoid arthritis]], [[osteoporosis]]) | * Diseases ([[osteoarthritis]], [[Rheumatoid Arthritis|rheumatoid arthritis]], [[osteoporosis]]) | ||
Pathological | |||
* | ==== Pathological Changes ==== | ||
* | * Soft tissues (muscles, tendons, blood vessels, nerves) | ||
* Hard tissues ([[bone]], hyaline [[cartilage]], fingernails)<ref name=":0" /> | |||
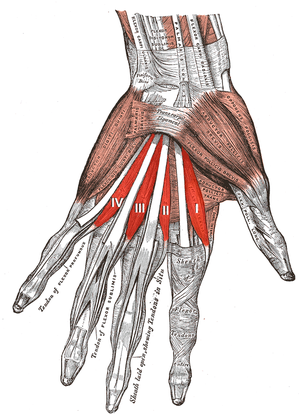
=== Muscles === | === Muscles === | ||
[[File:Lumbricales muscles of the left hand.png|thumb|Muscles of Left Hand]] | |||
One of the most common changes in aging skeletal muscle in the body is the major reduction in muscle mass ranging from 25% to 45%, | One of the most common changes in aging skeletal muscle in the body is the major reduction in muscle mass ranging from 25% to 45%, i.e. “[[Muscle Function: Effects of Aging|Sarcopenia]] of old age”<ref>Eli Carmeli, Hagar Patish, Raymond Coleman, The Aging Hand, The Journals of Gerontology: Series A. 2003; 58(2):M146-M152. <nowiki>https://doi.org/10.1093/gerona/58.2.M146</nowiki></ref>. The diminished muscle strength of the aging hand is attributed to decreasing muscle mass. There are 11 intrinsic muscles and 15 extrinsic [https://teachmeanatomy.info/upper-limb/muscles/hand/ hand muscles] with direct functional roles in the hand. | ||
* There is a significant reduction in both action potentials and in the number of viable motor units associated with the hand muscles in the elderly. | * There is a significant reduction in both action potentials and in the number of viable motor units associated with the hand muscles in the elderly. | ||
* Extrinsic and intrinsic hand muscles produce the force required for gripping objects (grip force). | * Extrinsic and intrinsic hand muscles produce the force required for gripping objects (grip force). | ||
| Line 53: | Line 63: | ||
* Changes due to [[Ageing Effects on Motor Control|aging]] cause reduced microcirculation of the synovial sheaths of the tendons and tendons unit, causing difficulties in the ability to adapt to environmental stress, decreased range of joint motion, and decreased flexion. This may also cause flexion contractures of the overlying joints. | * Changes due to [[Ageing Effects on Motor Control|aging]] cause reduced microcirculation of the synovial sheaths of the tendons and tendons unit, causing difficulties in the ability to adapt to environmental stress, decreased range of joint motion, and decreased flexion. This may also cause flexion contractures of the overlying joints. | ||
* The tensile strength of tendons is a measure of elongation of the tendon during tensile testing, the ultimate tensile strength values for aged tendons decrease by 30–50%. | * The tensile strength of tendons is a measure of elongation of the tendon during tensile testing, the ultimate tensile strength values for aged tendons decrease by 30–50%. | ||
* Biochemical changes in the aging tendons result in a stiffer, more irregular dense connective tissue. This involves a reduction in water content accompanied by a loss of proteoglycans and also degradation of the | * Biochemical changes in the aging tendons result in a stiffer, more irregular dense connective tissue. This involves a reduction in water content accompanied by a loss of proteoglycans and also degradation of the Type I Collagen fiber.<ref name=":0" /> | ||
== | === Bones and Joints of Hand === | ||
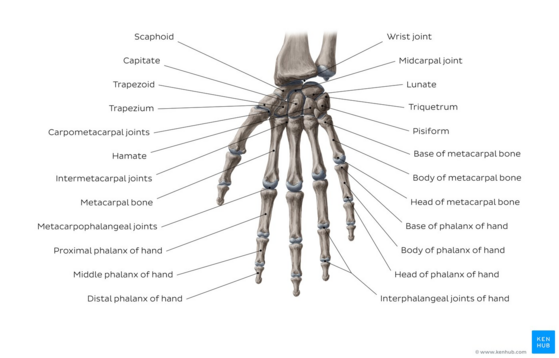
With [[Older People - An Introduction|aging]], the hand | [[File:Overview of the bones of the wrist and hand - Kenhub.png|center|frameless|559x559px]] | ||
* Aging hands and fingers are especially prone to | The 29 bones of hands and wrists come together to form many small joints. With [[Older People - An Introduction|aging]], the hand bones and joints (especially the synovial joints) are accompanied by morphological and pathological changes common to aging skeletal tissues. | ||
* Aging hands and fingers are especially prone to Osteoarthritis and Rheumatoid arthritis. | |||
* Osteoarthritis of the hand and finger joints is a disease process that destroys interphalangeal cartilage, synovial membranes, and the joint capsule. Consequences of osteoarthritis of the fingers include pain, swelling, joint deformities, bone spur formation, restricted range of motion of wrist and fingers, and difficulty in performing manual activities that require grip and pinch. | |||
* After the age of 50, the bone density of the hand decreases by approximately 0.72% per year.<ref name=":0" /> | * After the age of 50, the bone density of the hand decreases by approximately 0.72% per year.<ref name=":0" /> | ||
== Fingernails == | === Fingernails === | ||
Functionally, nails are important tools for fine grip and manipulation of small objects in various ways. | Functionally, nails are important tools for fine grip and manipulation of small objects in various ways. | ||
Age-associated nail changes are also common in elderly people. | |||
The rate of fingernail growth diminishes with aging. | The rate of fingernail growth diminishes with aging. | ||
These may involve: | |||
* Discoloration with changes in color from white | * Discoloration with changes in color from white/pink to yellowish/gray. | ||
* Changes in contour (longitudinal ridges, or less concave shape) | * Changes in contour (longitudinal ridges, or less concave shape) | ||
* Changes in the thickness and roughness of the nail surface. | * Changes in the thickness and roughness of the nail surface. | ||
* Structural changes include brittle nails; onychauxis (hypertrophic nail); subungual exostosis (a variant of osteochondroma). | * Structural changes include brittle nails; onychauxis (hypertrophic nail); subungual exostosis (a variant of osteochondroma). | ||
* The most common disorders of aging fingernails are common fungal infections. | * The most common disorders of aging fingernails are common fungal infections. | ||
* With the loss of manual dexterity with aging, elderly adults may not be able to cut their own nails and commonly require manicure assistance. | * With the loss of manual dexterity with aging, elderly adults may not be able to cut their own nails and commonly require manicure assistance. | ||
* Several of the changes in aging fingernails may be symptoms of underlying disease or metabolic disorders and can provide diagnostic indications for the physician. The translucent nature of the nail plate enables the coloration of the underlying nail bed, predominantly provided by the dermal vascularization, to be seen; this can provide an indication of problems such as anemia. | * Several of the changes in aging fingernails may be symptoms of underlying disease or metabolic disorders and can provide diagnostic indications for the physician. The translucent nature of the nail plate enables the coloration of the underlying nail bed, predominantly provided by the dermal vascularization, to be seen; this can provide an indication of problems such as anemia. | ||
== Nerve Changes and Hand Motor Control == | === Nerve Changes and Hand Motor Control === | ||
Loss of functioning of motor neuron and ventral root axons has been demonstrated in the elderly population, approximately 25% of the motor axons in hand muscles are lost in old age. | [[File:Grip strengthening exercises.JPG|right|frameless]]Loss of functioning of motor neuron and ventral root axons has been demonstrated in the elderly population, approximately 25% of the motor axons in hand muscles are lost in old age. | ||
* There is a reduction in the number of myelinated nerve fibers from the seventh and eighth cervical nerve roots, together with diminished nerve fiber diameters. | * There is a reduction in the number of myelinated nerve fibers from the seventh and eighth cervical nerve roots, together with diminished nerve fiber diameters. | ||
* Muscle twitches become smaller and slower. | * Muscle twitches become smaller and slower. | ||
* There | * There is loss of motor units after the age of 60, although they are less obvious in the ''Hypothenar'' group. The motor units in the ''Thenar'' and ''Dorsal interossei'' muscles decrease significantly with age. | ||
* Muscles in elderly adults have fewer (but on average larger and slower) motor units, which has an important effect on both motor control and function. There is a critical decline in age-related motor performance, which has been attributed to loss of motor | * Muscles in elderly adults have fewer (but on average larger and slower) motor units, which has an important effect on both motor control and function. There is a critical decline in age-related motor performance, which has been attributed to loss of motor neurons. | ||
* There is evidence indicating that age-related changes occur in both | * There is evidence indicating that age-related changes occur in both neurophysiology and in responses to neurotransmitters. | ||
* The integrity of the CNS is reflected in the cognitive and psychomotor ability of the individual. For a successful | * The integrity of the CNS is reflected in the cognitive and psychomotor ability of the individual. For a successful prehension task, CNS control processes of negative and positive feedback mechanisms are needed. This motor task requires the integrity of a circuit of interconnected hand-related areas, including a ventral subdivision of the premotor and sensorimotor cortical areas, the cerebellum, and the basal ganglia. With physiologic changes this may be affected, affecting prehension tasks.<ref name=":0" /> | ||
== Sensory Changes in the Aging Hand == | === Sensory Changes in the Aging Hand === | ||
Our senses and sensory integrity decline with aging. An understanding of the somatosensory system of the hand is important for therapists. | Our senses and sensory integrity decline with aging. An understanding of the somatosensory system of the hand is important for therapists. | ||
* Accurate functional sensory input is essential for well-controlled precision manipulation of small objects needed for many different activities of daily living. This requires refined coordination of forces exerted on the object by the tips of the finger and thumb. | * Accurate functional sensory input is essential for well-controlled precision manipulation of small objects needed for many different activities of daily living. This requires refined coordination of forces exerted on the object by the tips of the finger and thumb. | ||
* Peripheral decrement in tactile sensibility contributes to slowness in processing afferent information associated with hand movement. | * Peripheral decrement in tactile sensibility contributes to slowness in processing afferent information associated with hand movement. | ||
* The effects of old age on fingertip force responses have indicated degraded central information processing and deterioration of cutaneous mechanoreceptors. | * The effects of old age on fingertip force responses have indicated degraded central information processing and deterioration of cutaneous mechanoreceptors. | ||
== Skin Changes | === Skin Changes due to age === | ||
[[File:Aging hand.jpg|thumb|Skin Changes due to age]] | |||
* [[Older People Introduction|Elderly people]] are more susceptible to feeling cold in their hands than younger people, and this is probably due to the poorer blood flow in the elderly hands. | * [[Older People Introduction|Elderly people]] are more susceptible to feeling cold in their hands than younger people, and this is probably due to the poorer blood flow in the elderly hands. | ||
* Reduced sensitivity to local heat sources or slower reflexes may explain the increased incidence of burns to the hands of the elderly population (hot water scalding). | * Reduced sensitivity to local heat sources or slower reflexes may explain the increased incidence of burns to the hands of the elderly population (hot water scalding). | ||
* The thin skin of the dorsal aspect of the hand undergoes morphological changes with aging and becomes much thinner. | * The thin skin of the dorsal aspect of the hand undergoes morphological changes with aging and becomes much thinner. | ||
* The numbers and activities of sweat and sebaceous glands are also reduced in elderly people, who find it more difficult to accommodate to environmental heat stress. One of the consequences of the thinner dorsal hand skin in elderly adults is that it is more fragile, drier, and heals more slowly after injury. | * The numbers and activities of sweat and sebaceous glands are also reduced in elderly people, who find it more difficult to accommodate to environmental heat stress. One of the consequences of the thinner dorsal hand skin in elderly adults is that it is more fragile, drier, and heals more slowly after injury. | ||
* Obvious signs of dorsal skin aging of the hand are wrinkling and loss of elasticity, resulting from changes in the amount and biomechanical properties of the elastic fibers in the | * Obvious signs of dorsal skin aging of the hand are wrinkling and loss of elasticity, resulting from changes in the amount and biomechanical properties of the elastic fibers in the | ||
* The reduction in tactile sensation of fingers in elderly adults is due to the loss of the various sensory mechanoreceptors (Pacinian corpuscles, Meissner corpuscles, etc.). | * The reduction in tactile sensation of fingers in elderly adults is due to the loss of the various sensory mechanoreceptors (Pacinian corpuscles, Meissner corpuscles, etc.). | ||
=== Functional Movements of the Hand and Fingers === | |||
[[File:Finger flexion.jpg|right|frameless]] | [[File:Finger flexion.jpg|right|frameless]] | ||
* Tests show that in elderly people the largest declines in upper extremity functioning (greater than 50%) are in hand-force steadiness, speed of hand-arm movements, and vibration sense. | * Tests show that in elderly people the largest declines in upper extremity functioning (greater than 50%) are in hand-force steadiness, speed of hand-arm movements, and vibration sense. | ||
* Hand function remains fairly stable until the age of 65 years, after which it diminishes slowly. After the age of 75 years, age differences in performance become more apparent as seen in prehensile pattern frequency, hand strength, performance time, and range of motion. The percentage decrease in strength with age is similar for men and women regardless of their lifestyle. | * Hand function remains fairly stable until the age of 65 years, after which it diminishes slowly. After the age of 75 years, age differences in performance become more apparent as seen in prehensile pattern frequency, hand strength, performance time, and range of motion. The percentage decrease in strength with age is similar for men and women regardless of their lifestyle. | ||
* By the age of 90, an individual may be expected to have wrist range-of-motion (ROM) values that are approximately 60% of those of average 30-year-old individuals, affecting functional hand activities. | * By the age of 90, an individual may be expected to have wrist range-of-motion (ROM) values that are approximately 60% of those of average 30-year-old individuals, affecting functional hand activities. | ||
* Difficulties to adduct the thumb cause elderly people to substitute thumb adduction by using thumb flexors to compensate for their weakness (Froment's sign is positive). | * Difficulties to adduct the thumb cause elderly people to substitute thumb adduction by using thumb flexors to compensate for their weakness (Froment's sign is positive). | ||
* Aging has marked degenerative effects on hand function, age-related declines in hand and finger strength and the ability to control submaximal pinch posture, manual speed, and hand sensation occur. Moreover, a gender difference was also found, with elderly women experiencing more serious declines in fine manual dexterity and strength than men of a similar age. | * Aging has marked degenerative effects on hand function, age-related declines in hand and finger strength and the ability to control submaximal pinch posture, manual speed, and hand sensation occur. Moreover, a gender difference was also found, with elderly women experiencing more serious declines in fine manual dexterity and strength than men of a similar age. | ||
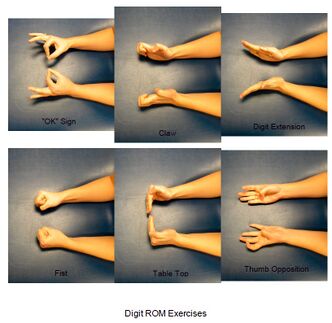
== Therapeutic Exercises and Ergonomic Devices for the Aging Hand == | == Therapeutic Exercises and Ergonomic Devices for the Aging Hand == | ||
[[File:Digit ROM Exercise Handout.jpg|right|frameless|332x332px]] | |||
Functional aging changes in hands can possibly be retarded by introducing suitable simple regular [[Hand Exercises|hand exercise]] programs for hand strengthening and hand flexibility. It is important that the exercises selected are appropriate and do not lead to damage or overexertion | Functional aging changes in hands can possibly be retarded by introducing suitable simple regular [[Hand Exercises|hand exercise]] programs for hand strengthening and hand flexibility. It is important that the exercises selected are appropriate and do not lead to damage or overexertion. | ||
* Exercise can be very simple | * Exercise can be very simple e.g. squeezable rubber balls, or elastic bands on fingers and exercises to strengthen grip and maintain joint flexibility of fingers and the wrist. See home-exercise plan below. | ||
Ergonomic devices are important: modifying tools and instruments of daily living for the elderly population, especially those with impaired functioning. | Ergonomic devices are important: modifying tools and instruments of daily living for the elderly population, especially those with impaired functioning. e.g. basic items such as cutlery, pens, scissors, nail clippers, hairbrushes, and combs. Large phone pads. <ref name=":0" /> | ||
== Simple Home Exercise Plan == | === Simple Home Exercise Plan === | ||
A simple | ==== 1. Finger Bends ==== | ||
A simple home exercise plan that keeps the joints in fingers moving. For best results, perform these bends on each individual finger of both hands. | |||
* Begin by holding up your right hand straight. | * Begin by holding up your right hand straight. | ||
* Bend your thumb downward in the direction of your palm. | * Bend your thumb downward in the direction of your palm. | ||
| Line 125: | Line 140: | ||
* Repeat on each finger on the right hand. | * Repeat on each finger on the right hand. | ||
* Repeat the entire sequence on the opposite hand. | * Repeat the entire sequence on the opposite hand. | ||
How to | ==== 2. Make a Fist ==== | ||
How to make a Fist? | |||
* Start by holding your right hand up and straight (as if you were going to shake someone’s hand). Keep your wrist and forearm close to a tabletop or another flat surface. | * Start by holding your right hand up and straight (as if you were going to shake someone’s hand). Keep your wrist and forearm close to a tabletop or another flat surface. | ||
* Close your fingers together to create a gentle fist. Try not to squeeze your fingers into your palms. | * Close your fingers together to create a gentle fist. Try not to squeeze your fingers into your palms. | ||
* Slowly and gently return your fingers to the starting position. | * Slowly and gently return your fingers to the starting position. | ||
* Repeat multiple times on each hand. | * Repeat multiple times on each hand. | ||
How to | ==== 3. Thumb Bends ==== | ||
How to perform a Thumb Bend? | |||
* Start by holding your right hand up and straight – just as you did with the previous exercise. | * Start by holding your right hand up and straight – just as you did with the previous exercise. | ||
* Bend your thumb down and inward toward your palm. | * Bend your thumb down and inward toward your palm. | ||
| Line 142: | Line 157: | ||
* Repeat 10 times. | * Repeat 10 times. | ||
* Repeat on the left hand. | * Repeat on the left hand. | ||
How to | ==== 4. Make a “C” ==== | ||
How to make a “C” With Your Hands? | |||
* Begin with your right hand up and your fingers straight. | * Begin with your right hand up and your fingers straight. | ||
* Curve your fingers downward and your thumb out and to the side to create a “C” shape. | * Curve your fingers downward and your thumb out and to the side to create a “C” shape. | ||
| Line 150: | Line 165: | ||
* Repeat multiple times on your right hand. | * Repeat multiple times on your right hand. | ||
* Repeat on the left hand. | * Repeat on the left hand. | ||
How to | ==== 5. Finger Lifts ==== | ||
How to perform Finger Lifts? | |||
* Start with your hand palm-side down on the table. | * Start with your hand palm-side down on the table. | ||
* Lift your thumb slowly off the table. | * Lift your thumb slowly off the table. | ||
| Line 159: | Line 174: | ||
* Repeat on each finger. | * Repeat on each finger. | ||
* Repeat the entire sequence on the opposite hand. | * Repeat the entire sequence on the opposite hand. | ||
How to | ==== 6. Wrist Stretches ==== | ||
How to perform Wrist Stretches? | |||
* Begin with your right arm stretched out in front of you, hands flat. | * Begin with your right arm stretched out in front of you, hands flat. | ||
* Gently press down on your right hand. The tips of your fingers should be facing the floor. | * Gently press down on your right hand. The tips of your fingers should be facing the floor. | ||
| Line 167: | Line 182: | ||
* Repeat 10 times. | * Repeat 10 times. | ||
* Repeat on the left hand. | * Repeat on the left hand. | ||
7. Give the Okay | |||
==== 7. Give the Okay ==== | |||
* Begin with your hand up and straight (as if you were going to shake someone’s hand). | * Begin with your hand up and straight (as if you were going to shake someone’s hand). | ||
* Create an “O” shape by touching your thumb to your index fingertip. | * Create an “O” shape by touching your thumb to your index fingertip. | ||
Revision as of 16:58, 13 November 2023
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Lucinda hampton, Mohit Chand, Uchechukwu Chukwuemeka, Kim Jackson and Shaimaa Eldib
Introduction[edit | edit source]
Hand function decreases with age in both men and women, especially after the age of 65 years. Deterioration in hand function in the elderly population is, to a large degree, secondary to age-related degenerative changes in the musculoskeletal, vascular, and nervous systems. Deterioration of hand function in elderly adults is a combination of local structural changes (joints, muscle, tendon, bone, nerve and receptors, blood supply, skin, and fingernails) and more distant changes in neural control. These age-related changes are often accompanied by underlying pathological conditions (osteoporosis, osteoarthritis, rheumatic arthritis, and Parkinson's disease) that are common in the elderly population[1].
Hand Dexterity[edit | edit source]
Hand dexterity is a term used to explain a range of different hand abilities and performances. These include reaction time; hand preference; wrist flexion speed; finger tapping speed; aiming; hand stability and arm stability. Age and grip strength are significant predictors of hand dexterity.
Aiming and tapping hand dexterity (involving rapid, coordinated, goal-directed actions) is moderated by the factor of grip strength more than age i.e. hand exercises may improve particular types of hand dexterity. [2]
Musculoskeletal Hand Problems in Older Adults[edit | edit source]
- Musculoskeletal hand problems are common in the population aged over 50 yrs.
- Hand function seems to remain stable until age 65 years, after which it gradually reduces.
- Prehension pattern selection did not seem to differ with age.
- Statistically significant differences in age were found for prehension pattern frequency, hand strength, and performance time.
- After age 75 years, age differences in performance are apparent.[3]
- Most are painful and have a significant impact on everyday life.
- Women that are very old are especially vulnerable to the effect of hand problems on their daily activities.[4]
Factors Affecting Function in Aging Hands[edit | edit source]
Extrinsic Factors[edit | edit source]
- Environmental factors (ultraviolet radiation, chemical irritants)
- Physical activities (work-related, recreational sports, and hobbies)
- Nutrition
- Traumatic injuries
Intrinsic Factors[edit | edit source]
- Genetic factors
- Endocrine factors
- Metabolic disorders
- Diseases (osteoarthritis, rheumatoid arthritis, osteoporosis)
Pathological Changes[edit | edit source]
- Soft tissues (muscles, tendons, blood vessels, nerves)
- Hard tissues (bone, hyaline cartilage, fingernails)[1]
Muscles[edit | edit source]
One of the most common changes in aging skeletal muscle in the body is the major reduction in muscle mass ranging from 25% to 45%, i.e. “Sarcopenia of old age”[5]. The diminished muscle strength of the aging hand is attributed to decreasing muscle mass. There are 11 intrinsic muscles and 15 extrinsic hand muscles with direct functional roles in the hand.
- There is a significant reduction in both action potentials and in the number of viable motor units associated with the hand muscles in the elderly.
- Extrinsic and intrinsic hand muscles produce the force required for gripping objects (grip force).
- After 60 years of age, there is a rapid decline in hand-grip strength, by as much as 20–25%, accompanied by a substantial loss of muscle fibers and decreased muscle-fiber length, particularly in the Thenar muscle group.
- The thumb intrinsic musculature constitutes approximately 40% of the total intrinsic musculature of the hand.[6]
- Three of the main thumb muscles play important roles in stabilizing the thumb during strong pinch grips of objects and these commonly show age-related dysfunction.
- The contractile capacity of the Thenar muscle in elderly people has been assessed finding higher muscle fatigue resistance in elderly adults, attributed to differences in both the PNS and CNS.[1]
Tendons[edit | edit source]
Tendons are composed of dense connective tissue, primarily formed by densely packed, orderly arranged, collagen fibers.
- Tendons have a very poor blood supply and are virtually avascular in the regions of tendon insertion[7].
- The primary function of tendons is to attach muscles to bone and to transmit muscle force to the skeletal system with limited stretch or elongation.
- Changes due to aging cause reduced microcirculation of the synovial sheaths of the tendons and tendons unit, causing difficulties in the ability to adapt to environmental stress, decreased range of joint motion, and decreased flexion. This may also cause flexion contractures of the overlying joints.
- The tensile strength of tendons is a measure of elongation of the tendon during tensile testing, the ultimate tensile strength values for aged tendons decrease by 30–50%.
- Biochemical changes in the aging tendons result in a stiffer, more irregular dense connective tissue. This involves a reduction in water content accompanied by a loss of proteoglycans and also degradation of the Type I Collagen fiber.[1]
Bones and Joints of Hand[edit | edit source]
The 29 bones of hands and wrists come together to form many small joints. With aging, the hand bones and joints (especially the synovial joints) are accompanied by morphological and pathological changes common to aging skeletal tissues.
- Aging hands and fingers are especially prone to Osteoarthritis and Rheumatoid arthritis.
- Osteoarthritis of the hand and finger joints is a disease process that destroys interphalangeal cartilage, synovial membranes, and the joint capsule. Consequences of osteoarthritis of the fingers include pain, swelling, joint deformities, bone spur formation, restricted range of motion of wrist and fingers, and difficulty in performing manual activities that require grip and pinch.
- After the age of 50, the bone density of the hand decreases by approximately 0.72% per year.[1]
Fingernails[edit | edit source]
Functionally, nails are important tools for fine grip and manipulation of small objects in various ways.
Age-associated nail changes are also common in elderly people.
The rate of fingernail growth diminishes with aging.
These may involve:
- Discoloration with changes in color from white/pink to yellowish/gray.
- Changes in contour (longitudinal ridges, or less concave shape)
- Changes in the thickness and roughness of the nail surface.
- Structural changes include brittle nails; onychauxis (hypertrophic nail); subungual exostosis (a variant of osteochondroma).
- The most common disorders of aging fingernails are common fungal infections.
- With the loss of manual dexterity with aging, elderly adults may not be able to cut their own nails and commonly require manicure assistance.
- Several of the changes in aging fingernails may be symptoms of underlying disease or metabolic disorders and can provide diagnostic indications for the physician. The translucent nature of the nail plate enables the coloration of the underlying nail bed, predominantly provided by the dermal vascularization, to be seen; this can provide an indication of problems such as anemia.
Nerve Changes and Hand Motor Control[edit | edit source]
Loss of functioning of motor neuron and ventral root axons has been demonstrated in the elderly population, approximately 25% of the motor axons in hand muscles are lost in old age.
- There is a reduction in the number of myelinated nerve fibers from the seventh and eighth cervical nerve roots, together with diminished nerve fiber diameters.
- Muscle twitches become smaller and slower.
- There is loss of motor units after the age of 60, although they are less obvious in the Hypothenar group. The motor units in the Thenar and Dorsal interossei muscles decrease significantly with age.
- Muscles in elderly adults have fewer (but on average larger and slower) motor units, which has an important effect on both motor control and function. There is a critical decline in age-related motor performance, which has been attributed to loss of motor neurons.
- There is evidence indicating that age-related changes occur in both neurophysiology and in responses to neurotransmitters.
- The integrity of the CNS is reflected in the cognitive and psychomotor ability of the individual. For a successful prehension task, CNS control processes of negative and positive feedback mechanisms are needed. This motor task requires the integrity of a circuit of interconnected hand-related areas, including a ventral subdivision of the premotor and sensorimotor cortical areas, the cerebellum, and the basal ganglia. With physiologic changes this may be affected, affecting prehension tasks.[1]
Sensory Changes in the Aging Hand[edit | edit source]
Our senses and sensory integrity decline with aging. An understanding of the somatosensory system of the hand is important for therapists.
- Accurate functional sensory input is essential for well-controlled precision manipulation of small objects needed for many different activities of daily living. This requires refined coordination of forces exerted on the object by the tips of the finger and thumb.
- Peripheral decrement in tactile sensibility contributes to slowness in processing afferent information associated with hand movement.
- The effects of old age on fingertip force responses have indicated degraded central information processing and deterioration of cutaneous mechanoreceptors.
Skin Changes due to age[edit | edit source]
- Elderly people are more susceptible to feeling cold in their hands than younger people, and this is probably due to the poorer blood flow in the elderly hands.
- Reduced sensitivity to local heat sources or slower reflexes may explain the increased incidence of burns to the hands of the elderly population (hot water scalding).
- The thin skin of the dorsal aspect of the hand undergoes morphological changes with aging and becomes much thinner.
- The numbers and activities of sweat and sebaceous glands are also reduced in elderly people, who find it more difficult to accommodate to environmental heat stress. One of the consequences of the thinner dorsal hand skin in elderly adults is that it is more fragile, drier, and heals more slowly after injury.
- Obvious signs of dorsal skin aging of the hand are wrinkling and loss of elasticity, resulting from changes in the amount and biomechanical properties of the elastic fibers in the
- The reduction in tactile sensation of fingers in elderly adults is due to the loss of the various sensory mechanoreceptors (Pacinian corpuscles, Meissner corpuscles, etc.).
Functional Movements of the Hand and Fingers[edit | edit source]
- Tests show that in elderly people the largest declines in upper extremity functioning (greater than 50%) are in hand-force steadiness, speed of hand-arm movements, and vibration sense.
- Hand function remains fairly stable until the age of 65 years, after which it diminishes slowly. After the age of 75 years, age differences in performance become more apparent as seen in prehensile pattern frequency, hand strength, performance time, and range of motion. The percentage decrease in strength with age is similar for men and women regardless of their lifestyle.
- By the age of 90, an individual may be expected to have wrist range-of-motion (ROM) values that are approximately 60% of those of average 30-year-old individuals, affecting functional hand activities.
- Difficulties to adduct the thumb cause elderly people to substitute thumb adduction by using thumb flexors to compensate for their weakness (Froment's sign is positive).
- Aging has marked degenerative effects on hand function, age-related declines in hand and finger strength and the ability to control submaximal pinch posture, manual speed, and hand sensation occur. Moreover, a gender difference was also found, with elderly women experiencing more serious declines in fine manual dexterity and strength than men of a similar age.
Therapeutic Exercises and Ergonomic Devices for the Aging Hand[edit | edit source]
Functional aging changes in hands can possibly be retarded by introducing suitable simple regular hand exercise programs for hand strengthening and hand flexibility. It is important that the exercises selected are appropriate and do not lead to damage or overexertion.
- Exercise can be very simple e.g. squeezable rubber balls, or elastic bands on fingers and exercises to strengthen grip and maintain joint flexibility of fingers and the wrist. See home-exercise plan below.
Ergonomic devices are important: modifying tools and instruments of daily living for the elderly population, especially those with impaired functioning. e.g. basic items such as cutlery, pens, scissors, nail clippers, hairbrushes, and combs. Large phone pads. [1]
Simple Home Exercise Plan[edit | edit source]
1. Finger Bends[edit | edit source]
A simple home exercise plan that keeps the joints in fingers moving. For best results, perform these bends on each individual finger of both hands.
- Begin by holding up your right hand straight.
- Bend your thumb downward in the direction of your palm.
- Hold the bend for two to five seconds.
- Straighten your thumb.
- Repeat on each finger on the right hand.
- Repeat the entire sequence on the opposite hand.
2. Make a Fist[edit | edit source]
How to make a Fist?
- Start by holding your right hand up and straight (as if you were going to shake someone’s hand). Keep your wrist and forearm close to a tabletop or another flat surface.
- Close your fingers together to create a gentle fist. Try not to squeeze your fingers into your palms.
- Slowly and gently return your fingers to the starting position.
- Repeat multiple times on each hand.
3. Thumb Bends[edit | edit source]
How to perform a Thumb Bend?
- Start by holding your right hand up and straight – just as you did with the previous exercise.
- Bend your thumb down and inward toward your palm.
- The goal is to reach for the bottom of your pinky finger, but don’t worry if you cannot reach that far just yet.
- Hold the bend for a few seconds.
- Return to the starting position.
- Repeat 10 times.
- Repeat on the left hand.
4. Make a “C”[edit | edit source]
How to make a “C” With Your Hands?
- Begin with your right hand up and your fingers straight.
- Curve your fingers downward and your thumb out and to the side to create a “C” shape.
- Return to the starting position.
- Repeat multiple times on your right hand.
- Repeat on the left hand.
5. Finger Lifts[edit | edit source]
How to perform Finger Lifts?
- Start with your hand palm-side down on the table.
- Lift your thumb slowly off the table.
- Hold for two seconds.
- Gently lower your thumb back down.
- Repeat on each finger.
- Repeat the entire sequence on the opposite hand.
6. Wrist Stretches[edit | edit source]
How to perform Wrist Stretches?
- Begin with your right arm stretched out in front of you, hands flat.
- Gently press down on your right hand. The tips of your fingers should be facing the floor.
- Hold the stretch for a few seconds.
- Repeat 10 times.
- Repeat on the left hand.
7. Give the Okay[edit | edit source]
- Begin with your hand up and straight (as if you were going to shake someone’s hand).
- Create an “O” shape by touching your thumb to your index fingertip.
- Next, touch your thumb to your middle fingertip.
- Repeat the same movement on the remaining fingers.
- Repeat the sequence multiple times.
- Repeat the entire exercise on the opposite hand.[8]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Carmeli E, Patish H, Coleman R. The aging hand. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2003 Feb 1;58(2):M146-52. Available from:https://academic.oup.com/biomedgerontology/article/58/2/M146/593573 (accessed 16 March 2020)
- ↑ Martin JA, Ramsay J, Hughes C, Peters DM, Edwards MG. Age and grip strength predict hand dexterity in adults. PloS one. 2015;10(2):e0117598
- ↑ <section> American Journal of Occupational Therapy, September 1992, Vol. 46, 785-792.Effects of Aging on Adult Hand Function https://doi.org/10.5014/ajot.46.9.785 (last accessed 16.3.2020) </section>Shiffman LM. Effects of aging on adult hand function. Am J Occup Ther. 1992;46(9):785–792. doi:10.5014/ajot.46.9.785
- ↑ Dziedzic K, Thomas E, Hill S, Wilkie R, Peat G, Croft PR. The impact of musculoskeletal hand problems in older adults: findings from the North Staffordshire Osteoarthritis Project (NorStOP). Available from:https://academic.oup.com/rheumatology/article/46/6/963/2899444 (accessed 16 March 2020)
- ↑ Eli Carmeli, Hagar Patish, Raymond Coleman, The Aging Hand, The Journals of Gerontology: Series A. 2003; 58(2):M146-M152. https://doi.org/10.1093/gerona/58.2.M146
- ↑ Chen CY, McGee CW, Rich TL, Prudente CN, Gillick BT. Reference values of intrinsic muscle strength of the hand of adolescents and young adults. Journal of Hand Therapy. 2018; 31(3): 348–356.
- ↑ Tempfer H, Traweger A. Tendon Vasculature in Health and Disease. Front Physiol. 2015; 6: 330. doi: 10.3389/fphys.2015.00330
- ↑ Uplifting mobility Hand exercises Available from:https://www.upliftingmobility.com/exercises-combat-arthritis/ (accessed 16 March 2020)