Aquatic Therapy in the Management of Chronic Low Back Pain: Difference between revisions
No edit summary |
No edit summary |
||
| Line 31: | Line 31: | ||
* Difficulty standing up straight, bending and walking | * Difficulty standing up straight, bending and walking | ||
=== Anatomical | === Anatomical relevance === | ||
The lumbar spine consists of 5 lumbar vertebrae (L1-L5). The vertebrae form a slightly inward curve known as lordosis. The lumbar vertebrae are connected in the back by facet joint, which allow flexion, extension, rotation and lateral rotation. The lumbar spine's two lowest segments, L5-S1 and L4-L5, bear the greatest weight and move the most, rendering them vulnerable to injury. In between the vertebral bodies, are the intervertebral discs that provide flexibility to the spine, maintaining the height between the vertebrae and distribute compressive loads by acting as shock absorber. As a result of aging, the discs become less flexible and more prone to tearing even with minor twist, thus more likely to herniate or degenerate which can cause pain in the low back. The lumbar region also contains large muscles that support the back and allow for movement in the trunk of the body when working together with the abdominal, the gluteal and the leg muscles . These muscles can spasm or become strained, which is a common cause of lower back pain. There are studies suggests that para-spinal and multifidus muscle groups are significantly smaller in patients with CLBP than in healthy patients and on the symptomatic side of patients with persistent unilateral low back pain compared with the asymptomatic side. These finding can further explain in 2 aspects (Microscopic and Macroscopic). | The lumbar spine consists of 5 lumbar vertebrae (L1-L5). The vertebrae form a slightly inward curve known as lordosis. The lumbar vertebrae are connected in the back by facet joint, which allow flexion, extension, rotation and lateral rotation. The lumbar spine's two lowest segments, L5-S1 and L4-L5, bear the greatest weight and move the most, rendering them vulnerable to injury. In between the vertebral bodies, are the intervertebral discs that provide flexibility to the spine, maintaining the height between the vertebrae and distribute compressive loads by acting as shock absorber. As a result of aging, the discs become less flexible and more prone to tearing even with minor twist, thus more likely to herniate or degenerate which can cause pain in the low back. The lumbar region also contains large muscles that support the back and allow for movement in the trunk of the body when working together with the abdominal, the gluteal and the leg muscles . These muscles can spasm or become strained, which is a common cause of lower back pain. There are studies suggests that para-spinal and multifidus muscle groups are significantly smaller in patients with CLBP than in healthy patients and on the symptomatic side of patients with persistent unilateral low back pain compared with the asymptomatic side. These finding can further explain in 2 aspects (Microscopic and Macroscopic). | ||
| Line 172: | Line 172: | ||
* Aquatic Dumbbells | * Aquatic Dumbbells | ||
* Wrist and Ankle Weights | * Wrist and Ankle Weights | ||
* Submersible Steps | * [[File:Kickboards in aquatic therapy.jpg|thumb|Equipment used in aquatic therapy - kickboards ]]Submersible Steps | ||
===== Floatation Aids ===== | ===== Floatation Aids ===== | ||
| Line 247: | Line 247: | ||
Numerous psychosocial factors are associated with chronic low back pain, therefore a biopsychosocial perspective is important to provide optimal care (Hartvigsen ''et al.'', 2018a). The biopsychosocial model of back pain is based on a holistic view which recognises the reciprocal influences of the biological, psychological, and social variables that influence low back pain. This is vital to understand due to the variable human experiences of back pain (Lall and Restrepo, 2017). | Numerous psychosocial factors are associated with chronic low back pain, therefore a biopsychosocial perspective is important to provide optimal care (Hartvigsen ''et al.'', 2018a). The biopsychosocial model of back pain is based on a holistic view which recognises the reciprocal influences of the biological, psychological, and social variables that influence low back pain. This is vital to understand due to the variable human experiences of back pain (Lall and Restrepo, 2017). | ||
[[File:BPS Model of pain.png|center|thumb|BPS Model of Chronic Low Back Pain]] | [[File:BPS Model of pain.png|center|thumb|BPS Model of Chronic Low Back Pain]] | ||
Dueñas ''et al.'' (2016) explains that chronic pain causes significant consequences for not only patients but their professional and social environment and therefore both social and psychological domains are important to understand. | Dueñas ''et al.'' (2016) explains that chronic pain causes significant consequences for not only patients but their professional and social environment and therefore both social and psychological domains are important to understand. | ||
| Line 298: | Line 297: | ||
*** Lowest effective dose for the shortest amount of time | *** Lowest effective dose for the shortest amount of time | ||
** Weak opioids if NSAIDs are contraindicated | ** Weak opioids if NSAIDs are contraindicated | ||
| Line 352: | Line 352: | ||
* Increases self-efficacy and confidence | * Increases self-efficacy and confidence | ||
[[File:Group hydrotherapy .png|thumb|Group Hydrotherapy Session]] | [[File:Group hydrotherapy .png|thumb|Group Hydrotherapy Session]] | ||
Revision as of 18:08, 17 May 2022
Chronic Low Back Pain[edit | edit source]
Chronic low back pain (CLBP) refers to pain that persisted for longer than 3 months, even after an initial injury or underlying cause of acute low back pain has been treated. It can be further classify into two main types according to whether there is a specific pathology behind the LBP.
Non-specific LBP is defined as ‘Pain, tension, soreness and/or stiffness in the low back region between the lower margin of the 12th ribs and the gluteal folds that is not attributed to any recognisable pathology.’ NSLBP affects approximately 90% of all patients with LBP which is a diagnosis based on the exclusion of particular pathology. These pathologies can be classified as follow:
- Disc herniation
- Spondylolisthesis
- Lumbar muscles or spinal ligament strain/ sprain
- Scoliosis
- Osteoporosis
- Ankylosing spondylitis
- Cauda equina syndrome
- Scheuerman's Kyphosis
Lower back pain classification by duration:[edit | edit source]
- Acute low back pain- 6 weeks or less
- Sub-acute low back pain- 7-12 weeks
- Chronic low back pain- More than 12 weeks
Epidemiology[edit | edit source]
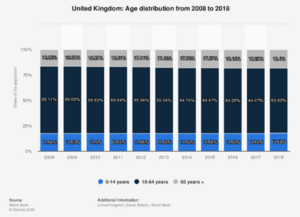
LBP affect around 7.5% of the global population (577.0 million people). Both the number of people living with LBP and the prevalence of LBP in all age groups has been increased from 1990 to 2019 Although the prevalence of LBP increase with increasing age, the greatest number of people with LBP globally are currently in the 50 to 54 year age group. In United Kingdom, Low back pain affects around 1/3 of the adult each year and is the leading cause of disability in the UK.
Clinical Presentation/ Symptoms[edit | edit source]
- Dull and achy pain that contained to the low back region
- Pain that worsen after prolonged sitting or standing
- Muscle spasms and tightness in the pelvis, low back and hips
- Burning and "electrical shock" like pain that radiate from the low back to the backs of the thighs and/ or the lower extremities.
- Difficulty standing up straight, bending and walking
Anatomical relevance[edit | edit source]
The lumbar spine consists of 5 lumbar vertebrae (L1-L5). The vertebrae form a slightly inward curve known as lordosis. The lumbar vertebrae are connected in the back by facet joint, which allow flexion, extension, rotation and lateral rotation. The lumbar spine's two lowest segments, L5-S1 and L4-L5, bear the greatest weight and move the most, rendering them vulnerable to injury. In between the vertebral bodies, are the intervertebral discs that provide flexibility to the spine, maintaining the height between the vertebrae and distribute compressive loads by acting as shock absorber. As a result of aging, the discs become less flexible and more prone to tearing even with minor twist, thus more likely to herniate or degenerate which can cause pain in the low back. The lumbar region also contains large muscles that support the back and allow for movement in the trunk of the body when working together with the abdominal, the gluteal and the leg muscles . These muscles can spasm or become strained, which is a common cause of lower back pain. There are studies suggests that para-spinal and multifidus muscle groups are significantly smaller in patients with CLBP than in healthy patients and on the symptomatic side of patients with persistent unilateral low back pain compared with the asymptomatic side. These finding can further explain in 2 aspects (Microscopic and Macroscopic).
(1) Microscopic change
It has been reported that patient with severe chronic LBP have a higher portion of type IIB muscle fibre (fast twitch glycolytic) at the expense of type I muscle fibre (Slow twitch oxidative). In healthy population, the paraspinal muscles have been found to have more type I muscle fibre in comparison with other skeletal muscle. The alteration in fibre type in severe chronic LBP, could lead to lowered fatigue resistance of the paraspinal muscles which will result in higher vulnerability of the lumbar spine and cause pain.
(2) Macroscopic change
Chronic low back pain can affect muscle structure by compromising muscle function. Comprised muscle function due to pain can alter muscle structure, including reduce muscle cross section and increase fat infiltration. Pain-related nerve inhibition reduces lumbar muscle activity in order to prevent tissue damage and lead to muscle inhibition and atrophy.
Prognostic indicators[edit | edit source]
The importance of prognostic factors[edit | edit source]
- By determining which variables are prognostic outcomes, clinicians gain insight on the biology and natural of the disease
- Appropriate treatment strategies may be optimised based on the prognostic factor
- Prognostic factors are often used in the design, conduct and analysis of clinical trials
- Patient and their families are informed about the risk of recurrence or future development of the disease.
Prognostic indicators for poor outcomes in chronic low back pain[edit | edit source]
- Age
- Gender
- Working status (active/ not working)
- Referred leg pain (yes/ no)
- NSLBP pain medication (yes/no)
- Current episode duration (acute/ sub-acute/ chronic)
- Maladaptive psychosocial factors
- Current pain intensity
- Disability
- HRQoL
Main prognostic indicators for the disability of LBP[edit | edit source]
In a 5- and 12-month follow up Cohort study that aims to identify clinically important prognostic factors of low back pain, it reported that a younger age, less disability at baseline, shorter duration of back complaints at baseline, and higher baseline scores on the SF-36 Physical component Summary and Mental Component Summery were predictors of absolute recovery (Quebec Back Pain Disability Scale score ≤20 points) at both 5- and 12-month follow-ups.
Aquatic Therapy[edit | edit source]
What is Aquatic Therapy?[edit | edit source]
Aquatic therapy can be defined as “A physiotherapy programme utilising the properties of water, designed by a suitably qualified physiotherapist” . This treatment method involves various exercises in water which should be carried out by appropriately trained therapists in a heated, purpose-built hydrotherapy pool.
The use of aquatic therapy is popular amongst patients with musculoskeletal and neurological disorders (Castro-Sánchez et al., 2011). Patients report benefits of increased strength, flexibility, mobility, as well as decreased pain levels (Larmer, Kersten and Dangan Bsc, 2014). These benefits are resultant of the unique properties of water, and therefore cannot always be replicated through land-based exercise.
Unique Properties of Water[edit | edit source]
Water Density[edit | edit source]
The water density counterbalances the effect of gravity which allows the human body to float. This buoyancy effect allows for reduced impact on joints. This is valuable during rehabilitation as it allows patients who are experiencing pain to exercise with reduced loading through the joints. Additionally, this buoyancy effect controls the downwards movement of the body and therefore decreases the need for eccentric control.
Exercises such as walking, jogging or running which may be painful to patients, can therefore be performed in water with less impact on the joint and therefore less pain.
What this means for spinal patients?
- Reduces axial loading and joint stress on the spine
Natural Resistance of Water[edit | edit source]
Water has a natural resistance as a result of its density and viscosity. This allows for effective strengthening during rehabilitation treatment sessions. The intensity of the resistance can be manipulated as well to fit the individual needs of the patient. Altering depth of submergence, speed of exercises performed, and the surface area of the body can affect the resistance profile of the water. For example, when stationary there is less resistance from the water on the body. However, during high speed movements, the resistance from the water will increase. Therefore, high speed resistance training can be performed in water allowing for strength to be built with low impact on the joints. As a result, aquatic therapy can be used as an alternative to land-based strength exercises.
Water as a Compressor[edit | edit source]
When a patient is submerged in water, they are subjected to hydrostatic pressure. This pressure has resultant effects on the body. For example, increased blood flow and circulation. This allows for greater oxygen delivery to the muscles and relaxation. Hydrostatic pressure can also compress the chest wall which alters pulmonary function and respiratory dynamics. As a result, work of breathing is increased by around 60% compared to that on land. This can actually strengthen respiratory muscles and improve the aerobic fitness of individuals.
Temperature[edit | edit source]
Hydrotherapy pools are usually heated to between 32-28 degrees Celsius. When submerged, this warm pool temperature can increase blood flow and range of motion. It can also produce greater muscle elasticity which can be beneficial for patients experiencing tightness of the muscles, stiffness or spasticity.
Indications, Contraindications and Precautions to Aquatic Therapy[edit | edit source]
Indications[edit | edit source]
- Management of muscle tone problems
- Decreased range of movement
- Decreased muscle strength
- Reduced balance
- Joint instability
- Pain
- Gait re-education
- Decreased sensation
- Neurological patients
- Patients who are willing to self-manage through a water-based exercise programme which they can continue with in pools available in leisure centres
- Patients who would benefit from aquatic physiotherapy in the short term to then progress to land-based exercise when ready
This would include conditions such as:
- Fibromyalgia
- Hemiplegia
- Cerebral palsy
- Ankylosing spondylitis
- Juvenile idiopathic arthritis
- Parkinson’s Disease
- Obesity
- Chronic low back pain
- Multiple sclerosis
- Traumatic brain injuries
- Stroke
- Rheumatoid arthritis
Contraindications[edit | edit source]
Absolute Contraindications[edit | edit source]
Patients with the following are not suitable to receive aquatic physiotherapy:
- Acute systemic illness/pyrexia
- Acute vomiting or diarrhoea
- Medical instability following an acute episode e.g. CVA, DVT
- Chlorine or bromine allergy
- Resting angina
- Shortness of breath at rest
- Uncontrolled cardiac failure
- Open infected wounds
Relative Contraindications[edit | edit source]
- Known aneurysm
- Poorly controlled epilepsy
- Open wounds
- Thyroid deficiency
- Neutropenia
- Weight in excess of evacuation equipment limit
- Oxygen dependency
- Unstable diabetes – blood sugar may drop
Precautions[edit | edit source]
- Incontinence of urine/faeces
- Epilepsy
- Hypotension
- Renal failure
- Poor skin integrity
- Risk of aspiration
- Prone to blackouts
- Sickle cell anaemia
- Tracheostomy
- Fear of water
- Pregnancy is water temperature exceeds 35°C
- Low calorie intake
Equipment used in Aquatic Therapy[edit | edit source]
Resistance Aids[edit | edit source]
- Flippers/fins
- Aquatic Dumbbells
- Wrist and Ankle Weights
- Submersible Steps
Floatation Aids[edit | edit source]
- Pool Noodles
- Aqua round body support
- Floatation Belts
- Arm Bands
- Kick boards
- Aqua Plinth
- Sensafloat
Cardiovascular Equipment[edit | edit source]
- Underwater Treadmill
- Underwater Stationary bike
Benefits of Aquatic physiotherapy[edit | edit source]
- Improved flexibility
- Improved balance
- Improved coordination
- Increased muscle strength and endurance
- Enhanced aerobic capacity
- Gait re-education and improving weight bearing capacity
- Relaxation
- Increased mobility
- Improved health-related quality of life
- Decreased pain levels
Assessment and Diagnosis[edit | edit source]
On initial assessment, it is important to examine the patient to diagnostically triage patients as recommended in the international back pain guidelines. Screening patients with new onset of back pain for red flag diagnosis such as neurologic compromise, inflammatory disease, infection, trauma/ fractures, and cancer which may require emergency attention
Next it is important to identify any less serious or non-specific causes of back pain. NICE guidelines recommends considering using risk stratification such as the STarT Back risk assessment at first point contact for new episodes of low back pain with or without sciatica for shared decision-making. If the low back pain is non-specific, it will usually be mechanical in nature and is exacerbated by movement and relived by rest and is affected by psychological and social factors.
Subjective History[edit | edit source]
Undertaking a subjective history allows to build a rapport with your patient, gain a further insight into their low back pain such as onset, duration, location, character, severity and aggravating and relieving factors in addition to identifying serious pathologies.
Physical Assessment[edit | edit source]
A physical assessment will follow the subjective history to clinically reason and confirm hypothesis. A physical assessment for the lower back will include the following:
- Observation – posture, abnormal deformity, and curvature
- Palpation – along spinous process and transverse process, musculature, sacroiliac joint
- Gait – through stance and swing phase
- Range of Motion – Passive and Active of lumbar, thoracic spine, and hip
- Muscle strength – Lumbar spine and Hip
- Neurological testing – Reflexes, Motor and sensory testing, straight leg raise, femoral nerve test
- Testing SIJ and Hip – thigh thrust test, pelvic compression, FABER’s
- Motor control testing – Waiter’s Bow, Pelvic tilts
- Imagining is not routinely offered in non-specialist setting for people with low back pain – NICE
Patient-reported outcome measures[edit | edit source]
Using patient-reported outcomes provides a patient's perceptive of their disease and treatment which we may not be able to gain through the subjective and objective assessment. It allows patients to track their progress, measure quality of care and management and provides motivation and adherence to treatment.
In a Delphi survey which included international multidisciplinary group of researchers, clinicians and patients updated the set outcome domains for low back pain. These domains are mentioned below with the associated outcome measures with the best psychometric properties.
Choosing the domain and outcome measure during clinical assessment will depend on various different factors such as the patient's level of function, disability and goals. It is recommended to use one of these measures due to reasons mentioned above considering the practitioners personal preference, practical aspects e.g. costs and availability.
- Physical function – Oswestry Disability Index or Roland Morris Disability Questionnaire
- Pain intensity – Numerical Rating Scale or Visual Analogue Scale
- Health-related quality of life – Short Form Health Survey 12 or EuroQol-5D-3L
- Work – Work Ability or Work productivity questionnaire
- Psychological functioning – Hospital Anxiety and Disability Scale
- Pain interference – Pain Interference subscale of the Brief Pain Inventory
Psychosocial Effects of Chronic Low Back Pain[edit | edit source]
Introduction[edit | edit source]
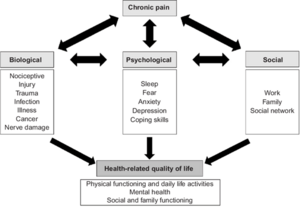
Known predictors of chronicity and disability in patients with low back pain include depression, distress, and somatisation (Pincus et al., 2013). Psychological factors that are associated with all chronic pain include depression and anxiety, fear avoidance, low self-efficacy, and post-traumatic stress disorder (Pincus et al., 2013; Arnold et al., 2006; Chaitow, 2016). Finally, social factors include abstaining from work, detaching and isolating from others and compensatory mechanisms (Pincus et al., 2013)
The Biopsychosocial Model of Chronic Pain[edit | edit source]
Numerous psychosocial factors are associated with chronic low back pain, therefore a biopsychosocial perspective is important to provide optimal care (Hartvigsen et al., 2018a). The biopsychosocial model of back pain is based on a holistic view which recognises the reciprocal influences of the biological, psychological, and social variables that influence low back pain. This is vital to understand due to the variable human experiences of back pain (Lall and Restrepo, 2017).
Dueñas et al. (2016) explains that chronic pain causes significant consequences for not only patients but their professional and social environment and therefore both social and psychological domains are important to understand.
Psychosocial Factors Influences Ones's Life[edit | edit source]
Psychosocial factors cause a continuous detrimental cycle whereby they not only affect the back pain but also one’s life. For example, depressive symptoms may worsen back pain and therefore increase the disability associated with back pain (Hartvigsen et al., 2018b).
Back pain patients are more likely to experience:
- Major depressive disorders
- Anxiety disorders
The coexistence of these conditions and associated back pain may lead to decreased quality of life and a greater chronicity. Despite this, mechanisms of the associations that underly chronic back pain are still not fully understood (IASP, 2021).
Avoidance Behaviour[edit | edit source]
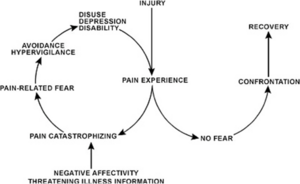
Avoidance behaviour may lead to the maintenance of chronic pain for longer. By avoiding movements, it may lead to cycles of greater disability and increasing pain. Described in the Fear Avoidance and Beliefs Model (FAMB) (Crombez et al., 2012).
Low Back Pain and Depression[edit | edit source]
A study by Robertson et al. (2017) with 1013 first year Canadian university students looked at the association between low back pain and depression and somatisation in adults. Participants completed the modified Zung Depression Index, the modified somatic perception questionnaire and a survey about low back pain and intensity. Results revealed that over 50% of subjects reported low back pain across grades, and both depression and somatisation was positively associated with low back pain, consistent with other studies and reinforcing the understanding of the detrimental association.
Conclusion[edit | edit source]
Due to the large psychosocial element that surrounds chronic low back pain, it is important that we use psychosocial outcome measures when assessing a patient.
PSYCHOLOGICAL FUNCTIONING = HADS – Because there is a big biopsychosocial
The effectiveness of Aquatic Therapy for Chronic Low Back Pain[edit | edit source]
The standardised approach for the management of chronic low back pain is multi-modal. The NICE guidelines recommend:
- Self management
- Advice and information from health care professionals to allow patients to self manage their pain
- Activity modification
- Information about the nature of their back pain
- Advice and information from health care professionals to allow patients to self manage their pain
- Exercise
- Type of exercise should take into account the patients' specific needs, preferences and capabilities
- Group exercise programmes are recommended
- Manual Therapy
- Spinal Manipulation, mobilisation and soft tissue techniques in addition to exercise
- Psychological therapy
- CBT approach for managing low back pain in addition to exercise
- Consider a combined physical and psychological programme
- Promote and facilitate return to work and normal activities
- Pharmacological approach
- Oral NSAIDs
- Lowest effective dose for the shortest amount of time
- Weak opioids if NSAIDs are contraindicated
- Oral NSAIDs
Within these NICE guidelines the importance is placed upon exercise and making sure the type of exercise takes into account the specific needs and preferences of the individual patient. Often, patients are prescribed land-based exercises focusing on strengthening, stretching and motor control.
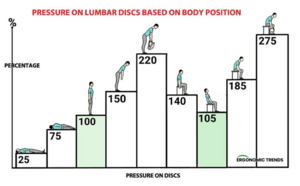
However, when walking or moving on land, our spine gets compressively loaded due to gravity and body positions which can increase intradiscal pressure (10)(6). This is important to note because increased of loading of the facet joints, and other spinal structures has been suggested as a potential cause low back pain (14).
This is why it is important to consider alternative treatment options to land-based exercise which decrease this spinal loading. For example, aquatic therapy can be indicated as a management option for CLBP because the unique properties of water allow for exercise in a medium which reduces pressure on joints.
The main benefits of aquatic therapy for chronic low back pain are:
- Decreased Pain
- Increased Function
- Decreased Disability
Aquatic therapy for improving pain[edit | edit source]
As previously stated, aquatic therapy can have benefits for Chronic low back pain by decreasing patients self-reported pain levels. In research this is often measured using visual analogue scales (VAS).
A randomised control trial by Baena-Beato et al. (2013b) researched the effect aquatic therapy had on patients with chronic low back pain who were sedentary. The 49 participants were split into aquatic therapy and waiting list groups who received advice and education (control). Results found that after 2 months of the aquatic therapy programme, participants experienced significantly improved lower back pain (VAS) at rest, in flexion and in extension compared to the control group. Body composition was also measured, with weight and BMI decreasing for the aquatic therapy group compared to the control. However, this was a small sample size and only evaluated sedentary patients which could impact the generalisation of these results to the wider population.
Aquatic therapy decreasing pain for patients with chronic low back pain has been supported by a systematic review and meta-analysisby Shi et al. (2018). This review included 8 trials with a total of 331 participants, looking at the effectiveness of aquatic therapy for chronic low back patients. Sessions ranged from 2-5x a week and from 30-80-minute sessions over a period of 4-15 weeks. Comparison groups either received land-based therapy, standard general practice or no exercise. Results showed that patients who took part in aquatic therapy experienced a statistically significant reduction in self-reported pain (VAS) compared to the control groups. However, these changes were not always reported as clinically significant.
Aquatic therapy for improving disability and function[edit | edit source]
Chronic low back pain is one the leading cause of disability worldwide (Hartvigsen et al., 2018). As a result, physical function is compromised, and patients often struggle to complete their activities of daily life and work-related activities.
Aquatic therapy aims to improve these two symptoms of chronic low back pain.
A randomised control trial by Dundar et al. (2009) assessed 65 patients with CLBP. They were randomly assigned aquatic exercise or land-based exercise. After 4 weeks, both groups improved in all outcome measures compared to baseline. However, the aquatic exercise group showed a significantly better improvement in the Oswestry Low back pain disability questionnaire and the physical function section of the SF36.
This was further supported by a systematic review (Waller, Lambeck and Daly, 2009). A total of 7 trials were included in the review, and results showed that compared to no intervention, aquatic therapy resulted in a significant improvement in function (Oswestry Disability index). However, the improvements were no better than other interventions.
Aquatic Therapy vs Other Therapies[edit | edit source]
Land-based therapy is recommended for patients with low back pain as an intervention to increase range of motion, flexibility, and strength. As mentioned above, aquatic therapy has a wide range of benefits on patients with low back pain.
Here are two studies comparing aquatic and land-based therapy for patients with low-back pain:
A study by Hend et al. (2021) conducted a randomised control trial comparing aquatic therapy (n=30) to land-based therapy (n=30) on pain level, functional ability, and lumbar range of motion in chronic low back patients. In a population of 60 participants, on multivariate analysis, a statistically significant multivariate effects were found for the main effects of groups for time and interaction between groups and time. Additionally, on univariate analysis, a statistically significant difference (p<0.05) between the groups were observed, favouring the aquatic group for VAS, ODI, flexion, extension, and side flexion outcome after 4 weeks. Land-based exercises did show statistical improvements in pain intensity, ODI and lumbar flexion however no difference was observed in extension and right and left side flexion with aquatic therapy group showing significant results in all outcome measures. However, this study had no control group and did not evaluate the long-term effects of using water-based therapy therefore could have been impacted by bias reducing its validity and reliability.
Another randomised control trail by Peng et al. (2022) compared aquatic therapy to physical activity modalities (TENS). In a population of 113 participants, they were split into aquatic group (56) and physical therapy modalities group (57). After treatment for 12 weeks, which comprised to 60-minute sessions twice per week for a total of 24 sessions, a statistically significant clinically meaningful improvement was observed in disability scores (Roland Morris) in the aquatic group compared to physical modalities after 3, 6 and 12 months (p<0.001). In addition, there was significant improvement in pain rating at 3,6 and 12 months in the aquatic group compared to physical modalities (p<0.001). However this study had no control group, increasing risk of bias and were unable to determine if benefits were from an active warm-up thus reducing validity.
On the other hand, a study by Nemcic et al. (2013) demonstrated no significant difference between an aquatic therapy group and land-based group after a 3 week programme in lumbar mobility and physical disability demonstrating either modality is modality is beneficial in managing low back pain. .
Psychosocial Effects of Aquatic Therapy on Chronic Low Back Pain[edit | edit source]
Introduction[edit | edit source]
There are numerous psychosocial benefits from engaging in aquatic physiotherapy and recent research explains that all aquatic exercise is vital in promoting and managing mental health. Firstly, partaking in physical exercise can have many positive effects on quality of life due to the facilitation and promotion of social interaction (Moore et al., 1999; Salmon, 2001; Silva et al., 2019). On the other hand, psychosocial stressors and a sedentary lifestyle has been shown to reduce cellular functioning. Thus, promoting physical exercise is vital when treating and preventing depression (Hearing et al., 2016) and other mental health disorders.
Psychosocial benefits[edit | edit source]
- Stress relief
- Relaxation of muscles
- Water is associated with fun and relaxation
- Promotes body awareness
- Increases self-efficacy and confidence
The warm water and physical properties of water (buoyancy and hydrostatic pressure) can provide stress relief allowing the muscles to relax, leading to tension relief and a reduction in muscle spasms (Sawant and Shinde, 2019), promoting a less anxious state. Women partaking in aquatic physiotherapy report feeling comfortable and relaxed in the warm water (Maude and Foureur, 2007).
Additionally, aquatic therapy can provide a sense of control and understanding of your own body due to the hydrostatic pressure promoting sensory receptors, allowing patients to take back control of their own movements, increasing self-efficacy and confidence (Frye, Ogonowska-Slodownik and Geigle, 2017).
Aquatic Physiotherapy and Depression[edit | edit source]
Silva et al. (2019) completed a study with 92 elderly people to determine the effects of aquatic exercise on mental health. The participants were allocated into two groups (depression group and non-depression group) in which they completed an aquatic exercise programme for 12 weeks. They discovered that, in depressed elderly individuals, aquatic physiotherapy reduces depression and anxiety, improves activities of daily living, and reduces oxidative stress.
Swim England Supports Aquatic Physiotherapy[edit | edit source]
Swim England’s 2019 Value of Swimming report and the 2021 Decade of Decline report were created to encourage and improve the awareness of swimming and aquatic therapy. Their aim is to prevent the closures of hydrotherapy pools They report this is because of the posititve impact aquatic physiotherapy can have on ones physical and mental well-being.
Conclusion[edit | edit source]
Prescription of Aquatic Therapy for Chronic Low Back Pain[edit | edit source]
As previous studies have shown, aquatic physiotherapy can be proven useful for reducing symptoms of chronic lower back pain. However, the question remains as to how frequent this intervention needs to take place for it to be effective in the short and long term.
Frequency Per Week[edit | edit source]
There are a couple studies which look at the effect of different frequencies for this intervention. For example, Baena-Baeato et al., (2013) compared the effect of completing aquatic therapy either 2x or 3x a week for chronic lower back pain patients over an 8-week period. This study included 54 participants who had chronic lower back pain for more than 12 weeks. They were split into a control group (education/advice only), aquatic therapy 2x a week and then aquatic therapy 3x a week. Outcome measures of pain, disability, quality of life, body composition and health related fitness were used to determine the effects of the different frequencies. Results showed that both groups experienced significant improvements in back pain and disability compared to the control group. However, the 3x a week group showed significantly greater benefits with pain into flexion and disability levels compared to the 2x a week group. Both groups experienced significantly improved quality of life and health related parameters. There were no significant changes between the treatment groups and control in regard to body composition.
Another study by Cuesta-Vargas et al., (2015) investigated the optimal frequency of aquatic therapy for individuals with chronic musculoskeletal pain. This randomised control trial included 114 people with chronic musculoskeletal pain and had them participate in aquatic therapy either 2x or 3x a week for a year. Patients included experienced 1 of 3 musculoskeletal disorders: chronic lower back pain, chronic neck pain or osteoarthritis. Outcome measures included quality of life, disability index and WOMAC for OA patients. Measurements were taken at baseline, 8 weeks, 6 months and a year after the programme started. Results showed that there were no statistical differences between the two groups except the neck disability index at 8 weeks. There were improvements for all groups and all variables from baseline to a year.
Length of Session and Content of Session[edit | edit source]
Both studies included aquatic therapy sessions which were on average 60 minutes long. This is consistent with other studies which look generally at the effectiveness of aquatic therapy on chronic lower back pain. For example, in a systematic review by Christakou and Boulnta (2020), 13 studies were reviewed, and the majority used interventions of aquatic therapy ranging from 45-60 minutes. Aquatic therapy sessions included warmups, muscle strength exercises, aerobic exercises and cool downs working on flexibility. This systematic review concluded that aquatic therapy improved pain, disability and quality of life.
What the Evidence Suggests[edit | edit source]
As a result of these studies, it can be concluded that the optimal aquatic therapy prescription for chronic lower back patients should be 2x a week for 60-minute sessions. These sessions should include a mixture of aerobic and resistance exercises as well as a warmup and cool down. This knowledge has implications for rehabilitation, as it shows that 2x a week is often comparable to 3x a week of aquatic therapy for outcomes of chronic lower back pain. This can save resources and cost for patients and service providers without compromising the effects of the treatment.