ICF Model and Goal Writing in Paediatrics: Difference between revisions
No edit summary |
No edit summary |
||
| (35 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
= | <div class="editorbox"> '''Original Editor '''- [[User:Robin Tacchetti|Robin Tacchetti]] based on the course by | ||
[https://members.physio-pedia.com/course_tutor/krista-eskay/ Krista Eskay]<br> | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== Introduction == | |||
The [[Overview of the ICF and Clinical Practice|International Classification of Functioning, Disability and Health (ICF)]] is a World Health Organization classification of health and health-related domains. This framework measures health and disability at both the individual and population levels while also looking at environmental factors.<ref>Barlett CP, Madison CS, Heath JB, DeWitt CC. Please browse responsibly: [https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health A correlational examination of technology access and time spent online in the Barlett Gentile Cyberbullying Model]. Computers in Human Behavior. 2019 Mar 1;92:250-5.</ref> This framework emphasises function, impact and health rather than disability and cause.<ref>World Health Organization. [https://cdn.who.int/media/docs/default-source/classification/icf/icfbeginnersguide.pdf?sfvrsn=eead63d3_4&download=true Towards a common language for functioning, disability, and health]: ICF. The international classification of functioning, disability and health. 2002.</ref> Understanding the functional deficits associated with a health condition promotes better patient management. The [[Overview of the ICF and Clinical Practice|ICF]] offers a more holistic model of health, which utilises goal setting, and requires the evaluation of outcomes and communication among colleagues.<ref name=":0">Jiandani MP, Mhatre BS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5954814/ Physical therapy diagnosis: How is it different?]. Journal of postgraduate medicine. 2018 Apr;64(2):69.</ref> | |||
== ICF Model == | |||
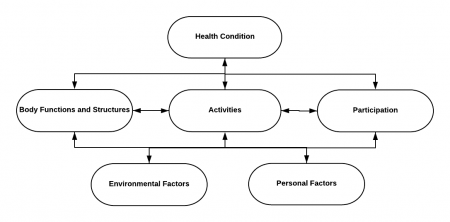
[[File:ICF Model Generic (correct version).png|thumb|450x450px|Figure 1. ICF Model.]] | |||
The ICF framework is a biopsychosocial model, which intertwines medical and social models of disability. The ICF framework recognises that one's health is shaped by environmental and personal factors. The ICF can be separated into three components of health: | |||
individual | # Body functions and structures | ||
# Activities | |||
# Participation | |||
Then, there are contextual factors that influence an individual's life: | |||
# Environmental factors | |||
# Personal factors | |||
Body functions refers to the physiological functions of body systems. Body structures refers to the anatomical parts of the body (e.g. organs, limbs etc). Activities and participation refer to involvement in life events and the implementation of various tasks. Environmental factors are the attitudinal, social and physical environments where people conduct and live their lives. Personal factors might relate to the individual and their family.<ref name=":3" /><ref>Eskay K. ICF Model and Goal Writing Course. Plus. 2022.</ref><blockquote> | |||
==== Special Topic: the ICF and Paediatric Rehabilitation ==== | |||
"The ICF describes the relationship between health conditions diagnosed and coded in the ICD [International Classification of Diseases] and the personal and environmental factors that act as facilitators or barriers to functioning. There are 3 identified levels of functioning: the body part or organ system, the person, and the person in social situations. These levels correspond to body functions, activities, and participation, respectively. Disability is the umbrella term for impairments at the body part or organ system level, activity restrictions at the person level, and participation restrictions at the person-in-society level. The WHO defines impairments as “problems in body function or structure such as a significant deviation or loss,” activity limitations as “difficulties an individual may have in executing a task,” and participation restrictions as “problems an individual may experience in involvement in life situations.” | |||
The ICF also includes the concepts of capacity and performance. Capacity is the individual’s intrinsic ability to perform a task or an action in a standardized environment, whereas performance is how well the individual is able to actually perform the task in his or her own real-life environment. These concepts are important in understanding the role of habilitative and rehabilitative therapies for children with disabilities, because achievement of skill requires extensive practice and must be integrated into the child’s routine for the successful enhancement of participation in life events. In addition, the ICF framework highlights the importance of a child’s environment on his or her functional outcomes. The environment includes not just the physical world, such as the town where the child lives or the topography of the community, but also includes the attitudes and values of the family, community, and society at large and the technologies, services, supports, laws, and policies where the child lives. Access to health and therapeutic services, the physical environment, and social supports all affect how well a child with disabilities functions in his or her daily life."<ref name=":4" /> | |||
-Houtrow et al 2019</blockquote> | |||
== Functional Limitations == | |||
It is important during rehabilitation evaluation to determine what functional limitations the individual has. For example, physiotherapists are interested in learning how the individual's functional limitations are inhibiting or restricting their activity and participation; occupational therapists are interested in how their ability to complete activities of daily living are effected. Activity refers to the ability of the individual to execute a task or action, whereas participation is the ability to fulfill a socially defined role. Participation can relate to activities with family, at work and/or with peer groups. The [[ICF and Application in Clinical Practice|ICF]] framework considers immediate or distant factors that might facilitate or hinder overall functioning, including: | |||
* Environmental factors | |||
** Setting at home | |||
** Setting at school | |||
** Motivation of the individual | |||
** Amount of family support | |||
** Accessibility to assistive devices<ref name=":0" /> | |||
* Personal factors | |||
** Age | |||
** Gender | |||
** Lifestyle | |||
** Fitness | |||
** Coping styles | |||
** Cultural beliefs | |||
** Pain experience<ref name=":0" /> | |||
== Interventions == | |||
The plan of care is created once the impairments, functional limitations and activity limitations have been identified. Interventions are targeted at minimising disability and using function as an outcome.<ref name=":0" /> Within the paediatric population, the [[ICF and Application in Clinical Practice|ICF]] emphasises the importance of a child's environment on their functional outcomes. The environment encompasses not just the physical world, but the values and attitudes of the family and community. Accessibility to services and support will affect overall daily function for a child with functional impairments.<ref name=":4">Houtrow A, Murphy N, Kuo DZ, Apkon S, Brei TJ, Davidson LF, Davis BE, Ellerbeck KA, Hyman SL, Leppert MO, Noritz GH. [https://publications.aap.org/pediatrics/article/143/4/e20190285/37233/Prescribing-Physical-Occupational-and-Speech Prescribing physical, occupational, and speech therapy services for children with disabilities]. Pediatrics. 2019 Apr 1;143(4).</ref> | |||
== Goal-Setting == | |||
The [[ICF and Application in Clinical Practice|ICF]] framework can be helpful for goal-setting. Goals are created to increase activity and participation, which are impacted by functional impairments.<ref name=":1" /> <ref name=":2">Eskay, K. ICF Model and Goal-Writing Course. Physioplus. 2022</ref> Goal creation favours the strengths of the child and focuses on how to build on these strengths to accomplish new tasks.<ref name=":2" /> Within the paediatric population, a family-centred approach is adopted when setting goals.<ref name=":1">Rast FM, Labruyère R. I[https://onlinelibrary.wiley.com/doi/full/10.1111/dmcn.14471 CF mobility and self‐care goals of children in inpatient rehabilitation]. Developmental Medicine & Child Neurology. 2020 Apr;62(4):483-8</ref> This sort of collaboration enables the patient and family to highlight their interests and provide assistance in intervention planning.<ref name=":3" /> Research has shown that a family-/patient-centred approach can increase patient motivation and improve therapy outcomes.<ref name=":3" /> | |||
== SMART Goals == | |||
When creating meaningful functional goals, the SMART method is recommended. The acronym SMART stands for: | |||
* S: specific | |||
* M: measurable | |||
* A: attainable | |||
* R: realistic | |||
* T: time-limited<ref name=":3">Angeli JM, Schwab SM, Huijs L, Sheehan A, Harpster K. [https://pubmed.ncbi.nlm.nih.gov/31766925/ ICF-inspired goal-setting in developmental rehabilitation: an innovative framework for pediatric therapists]. Physiotherapy theory and practice. 2021 Nov 2;37(11):1167-76.</ref> | |||
Using the SMART acronym, rehabilitation professionals can ensure they have set realistic goals for the child that are attainable. Goals are typically geared for the short term or long term depending on the particular task.<ref name=":2" /> | |||
== Resources == | |||
* [[Introduction to the International Classification of Functioning, Disability and Health (ICF)]] | |||
* [[ICF Educational and Clinical Resources]] | |||
* [[ICF and RPS within Cerebral Palsy]] | |||
* [[International Classification of Functioning, Disability and Health (ICF)]] | |||
the | * [[Overview of the ICF and Clinical Practice|Overview of the ICF in Clinical Practice]] | ||
== References == | |||
<references /> | |||
[[Category:Rehabilitation]] | |||
[[Category:ReLAB-HS Course Page]] | |||
[[Category:Course Pages]] | |||
[[Category:Paediatrics]] | |||
Latest revision as of 07:40, 19 May 2024
Introduction[edit | edit source]
The International Classification of Functioning, Disability and Health (ICF) is a World Health Organization classification of health and health-related domains. This framework measures health and disability at both the individual and population levels while also looking at environmental factors.[1] This framework emphasises function, impact and health rather than disability and cause.[2] Understanding the functional deficits associated with a health condition promotes better patient management. The ICF offers a more holistic model of health, which utilises goal setting, and requires the evaluation of outcomes and communication among colleagues.[3]
ICF Model[edit | edit source]
The ICF framework is a biopsychosocial model, which intertwines medical and social models of disability. The ICF framework recognises that one's health is shaped by environmental and personal factors. The ICF can be separated into three components of health:
- Body functions and structures
- Activities
- Participation
Then, there are contextual factors that influence an individual's life:
- Environmental factors
- Personal factors
Body functions refers to the physiological functions of body systems. Body structures refers to the anatomical parts of the body (e.g. organs, limbs etc). Activities and participation refer to involvement in life events and the implementation of various tasks. Environmental factors are the attitudinal, social and physical environments where people conduct and live their lives. Personal factors might relate to the individual and their family.[4][5]
Special Topic: the ICF and Paediatric Rehabilitation[edit | edit source]
"The ICF describes the relationship between health conditions diagnosed and coded in the ICD [International Classification of Diseases] and the personal and environmental factors that act as facilitators or barriers to functioning. There are 3 identified levels of functioning: the body part or organ system, the person, and the person in social situations. These levels correspond to body functions, activities, and participation, respectively. Disability is the umbrella term for impairments at the body part or organ system level, activity restrictions at the person level, and participation restrictions at the person-in-society level. The WHO defines impairments as “problems in body function or structure such as a significant deviation or loss,” activity limitations as “difficulties an individual may have in executing a task,” and participation restrictions as “problems an individual may experience in involvement in life situations.”
The ICF also includes the concepts of capacity and performance. Capacity is the individual’s intrinsic ability to perform a task or an action in a standardized environment, whereas performance is how well the individual is able to actually perform the task in his or her own real-life environment. These concepts are important in understanding the role of habilitative and rehabilitative therapies for children with disabilities, because achievement of skill requires extensive practice and must be integrated into the child’s routine for the successful enhancement of participation in life events. In addition, the ICF framework highlights the importance of a child’s environment on his or her functional outcomes. The environment includes not just the physical world, such as the town where the child lives or the topography of the community, but also includes the attitudes and values of the family, community, and society at large and the technologies, services, supports, laws, and policies where the child lives. Access to health and therapeutic services, the physical environment, and social supports all affect how well a child with disabilities functions in his or her daily life."[6]
-Houtrow et al 2019
Functional Limitations[edit | edit source]
It is important during rehabilitation evaluation to determine what functional limitations the individual has. For example, physiotherapists are interested in learning how the individual's functional limitations are inhibiting or restricting their activity and participation; occupational therapists are interested in how their ability to complete activities of daily living are effected. Activity refers to the ability of the individual to execute a task or action, whereas participation is the ability to fulfill a socially defined role. Participation can relate to activities with family, at work and/or with peer groups. The ICF framework considers immediate or distant factors that might facilitate or hinder overall functioning, including:
- Environmental factors
- Setting at home
- Setting at school
- Motivation of the individual
- Amount of family support
- Accessibility to assistive devices[3]
- Personal factors
- Age
- Gender
- Lifestyle
- Fitness
- Coping styles
- Cultural beliefs
- Pain experience[3]
Interventions[edit | edit source]
The plan of care is created once the impairments, functional limitations and activity limitations have been identified. Interventions are targeted at minimising disability and using function as an outcome.[3] Within the paediatric population, the ICF emphasises the importance of a child's environment on their functional outcomes. The environment encompasses not just the physical world, but the values and attitudes of the family and community. Accessibility to services and support will affect overall daily function for a child with functional impairments.[6]
Goal-Setting[edit | edit source]
The ICF framework can be helpful for goal-setting. Goals are created to increase activity and participation, which are impacted by functional impairments.[7] [8] Goal creation favours the strengths of the child and focuses on how to build on these strengths to accomplish new tasks.[8] Within the paediatric population, a family-centred approach is adopted when setting goals.[7] This sort of collaboration enables the patient and family to highlight their interests and provide assistance in intervention planning.[4] Research has shown that a family-/patient-centred approach can increase patient motivation and improve therapy outcomes.[4]
SMART Goals[edit | edit source]
When creating meaningful functional goals, the SMART method is recommended. The acronym SMART stands for:
- S: specific
- M: measurable
- A: attainable
- R: realistic
- T: time-limited[4]
Using the SMART acronym, rehabilitation professionals can ensure they have set realistic goals for the child that are attainable. Goals are typically geared for the short term or long term depending on the particular task.[8]
Resources[edit | edit source]
References[edit | edit source]
- ↑ Barlett CP, Madison CS, Heath JB, DeWitt CC. Please browse responsibly: A correlational examination of technology access and time spent online in the Barlett Gentile Cyberbullying Model. Computers in Human Behavior. 2019 Mar 1;92:250-5.
- ↑ World Health Organization. Towards a common language for functioning, disability, and health: ICF. The international classification of functioning, disability and health. 2002.
- ↑ 3.0 3.1 3.2 3.3 Jiandani MP, Mhatre BS. Physical therapy diagnosis: How is it different?. Journal of postgraduate medicine. 2018 Apr;64(2):69.
- ↑ 4.0 4.1 4.2 4.3 Angeli JM, Schwab SM, Huijs L, Sheehan A, Harpster K. ICF-inspired goal-setting in developmental rehabilitation: an innovative framework for pediatric therapists. Physiotherapy theory and practice. 2021 Nov 2;37(11):1167-76.
- ↑ Eskay K. ICF Model and Goal Writing Course. Plus. 2022.
- ↑ 6.0 6.1 Houtrow A, Murphy N, Kuo DZ, Apkon S, Brei TJ, Davidson LF, Davis BE, Ellerbeck KA, Hyman SL, Leppert MO, Noritz GH. Prescribing physical, occupational, and speech therapy services for children with disabilities. Pediatrics. 2019 Apr 1;143(4).
- ↑ 7.0 7.1 Rast FM, Labruyère R. ICF mobility and self‐care goals of children in inpatient rehabilitation. Developmental Medicine & Child Neurology. 2020 Apr;62(4):483-8
- ↑ 8.0 8.1 8.2 Eskay, K. ICF Model and Goal-Writing Course. Physioplus. 2022