Physiotherapy for Morton's Neuroma: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Extracorporeal Shockwave Therapy (ESWT)" to "[[Extracorporeal Shockwave Therapy ") |
||
| (26 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User: | |||
<div class="editorbox"> '''Original Editor '''- [[User:Ewa Jaraczewska|Ewa Jaraczewska]] <br> | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
Civinini Morton’s Syndrome (CMS) is more commonly known as Morton’s neuroma. | Civinini Morton’s Syndrome (CMS) is more commonly known as Morton’s neuroma. Weinfield and Myerson<ref>Weinfeld SB, Myerson MS. Interdigital Neuritis: Diagnosis and Treatment. J Am Acad Orthop Surg. 1996 Nov;4(6):328-335.</ref> have also proposed the term "interdigital neuritis", which better describes the pathology of this condition. Neural degeneration and perineural fibrosis are typical of Morton's neuroma<ref>Riddick DA, Riddick DH, Jorge M. 7 - Footwear: foundation for lower extremity orthoses. In: Chui KK, Jorge M, Yen S-C, Lusardi MM, editors. Orthotics and prosthetics in rehabilitation (Fourth Edition). Elsevier, 2020. p164-82.</ref>; the presence of inflammatory tissue in histological examination justifies the description of Morton's neuroma as perineural fibrosis.<ref name=":10" /> Clinical symptoms that can help with diagnosis include pain and abnormal forefoot sensation. Conservative treatment, including lifestyle adjustment, may not always be practical. Thus, patients may choose to have surgery or various types of ultrasound-guided percutaneous injections to manage this condition. | ||
[[File:Foot Inneravtion.gif|thumb|Foot innervation]] | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
Magnetic resonance imaging (MRI) shows the medial and lateral plantar nerves | Magnetic resonance imaging (MRI) shows the [[Medial Plantar Nerve|medial]] and [[Lateral Plantar Nerve|lateral plantar nerves]] arise from the posterior [[Tibial Nerve|tibial nerve]].<ref name=":7">Govsa F, Bilge O, Ozer MA. Anatomical study of the communicating branches between the medial and lateral plantar nerves. Surgical and Radiologic Anatomy. 2005 Dec;27(5):377-81.</ref> The bifurcation of the tibial nerve occurs inside the retinaculum or proximal to the flexor retinaculum.<ref name=":8">Torres AL, Ferreira MC. [https://www.scielo.br/j/aob/a/3PgtjmSVwWMDmCYZgbPhghq/?format=pdf&lang=en Study of the anatomy of the tibial nerve and its branches in the distal medial leg]. Acta ortopedica brasileira. 2012;20:157-64.</ref> The two plantar nerves penetrate the tunnel made of the deep fascia of the [[Abductor Hallucis|abductor hallucis muscle]] and the fibrous septum, which connects the fascia to the bone.<ref name=":8" /> | ||
The [[Medial Plantar Nerve|medial plantar nerve]] (MPN) is the larger of the two plantar nerves. It originates under the flexor retinaculum (also known as the laciniate ligament) and passes between [[Abductor Hallucis|abductor hallucis]] and [[Flexor Digitorum Brevis|flexor digitorum brevis]]. Upon reaching the metatarsal bases, it divides into three common digital plantar nerves.<ref name=":9">Koo GB, Lee JH, Jang JH, Song IH, Kim JY. Superficial course of the medial plantar nerve: case report. Anatomy & cell biology. 2019 Mar 1;52(1):87-9.</ref> The MPN innervates the abductor hallucis, [[Flexor Hallucis Brevis|flexor hallucis brevis]], flexor digitorum brevis and the first lumbrical of the foot. | |||
The [[ | The [[Lateral Plantar Nerve|lateral plantar nerve]] (LPN) innervates [[Abductor Digiti Minimi (Foot)|abductor digiti minimi]], [[Flexor Digiti Minimi Brevis|flexor digiti minimi brevis]], [[Quadratus Plantae|quadratus plantae]], the three lateral lumbricals of the foot, [[Adductor Hallucis|adductor hallucis]], the plantar interossei, and the [[Dorsal Interossei of the Foot|dorsal interossei]]. | ||
The [[ | The common plantar digital (CPD) nerves pass under the intermetatarsal ligaments. They go through the plantar [[aponeurosis]] and divide into two branches, which supply the plantar skin of the toes. Smaller portions of the CPD nerves innervate the adjacent [[metatarsals]], metatarsophalangeal joints and plantar skin under the metatarsal heads.<ref name=":5">Colò G, Rava A, Samaila EM, Palazzolo A, Talesa G, Schiraldi M, Magnan B, Ferracini R, Felli L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7944831/pdf/ACTA-91-60.pdf The effectiveness of shoe modifications and orthotics in the conservative treatment of Civinini-Morton syndrome: state of the art.] Acta Biomed. 2020 May 30;91(4-S):60-68.</ref> | ||
The ''third common digital'' nerve begins as the medial plantar nerve and receives a communicating branch from the lateral plantar nerve. Because it passes through the narrow space deep to the transverse metatarsal ligament, it becomes less mobile, especially during weight-bearing activities.<ref name=":5" /> | |||
The branches of the common digital nerve in the third | The branches of the common digital nerve in the third plantar webspace are most commonly affected in Morton's neuroma. It has been proposed that the location of this nerve (i.e. near the narrow space of the transverse metatarsal ligament) may be why Morton's neuroma often occurs within the third intermetatarsal space.<ref name=":5" /> | ||
[[File:Mortons-neuroma-1.gif|thumb|Morton's neuroma]] | |||
=== Neuroma === | === Neuroma === | ||
A neuroma is also referred to as a pinched nerve. Morton's neuroma is a compressive neuropathy of the common plantar digital nerve caused by an entrapment of the nerve between the intermetatarsal ligaments. | |||
== Aetiology == | == Aetiology == | ||
There are several aetiopathogenetic theories behind the development of Morton's neuroma. | There are several aetiopathogenetic theories behind the development of Morton's neuroma. These include: | ||
* | * Chronic traction damage<ref name=":6">Hassouna H, Singh D. Morton's metatarsalgia: pathogenesis, aetiology and current management. Acta Orthop Belg. 2005 Dec;71(6):646-55. </ref> | ||
* | * Chronic, repetitive trauma<ref name=":6" /> | ||
* | * Ischaemia of vasa nervorum (Vasa nervorum = nutrient vessels that provide blood supply to each peripheral nerve from adjacent blood vessels)<ref name=":5" /><ref name=":6" /> | ||
* | * Entrapment or mechanical compression<ref name=":10">Jain S, Mannan K. The diagnosis and management of Morton's neuroma: a literature review. Foot Ankle Spec. 2013 Aug;6(4):307-17. | ||
</ref><ref name=":0">Bencardino J, Rosenberg ZS, Beltran J, Liu X, Marty-Delfaut E. [https://www.ajronline.org/doi/epdf/10.2214/ajr.175.3.1750649 Morton's neuroma: is it always symptomatic?]. American journal of roentgenology. 2000 Sep;175(3):649-53.</ref> | </ref><ref name=":0">Bencardino J, Rosenberg ZS, Beltran J, Liu X, Marty-Delfaut E. [https://www.ajronline.org/doi/epdf/10.2214/ajr.175.3.1750649 Morton's neuroma: is it always symptomatic?]. American journal of roentgenology. 2000 Sep;175(3):649-53.</ref> | ||
* | * Inflammation due to intermetatarsal bursitis<ref name=":10" /> | ||
'''Anatomical considerations:''' | |||
* The third common digital nerve is thicker than the others due to an anastomosis between two nerve trunks<ref name=":5" /> | |||
* The fourth ray is more mobile than the third, which might lead to inflammation<ref name=":5" /> | |||
* The plantar nerve is compressed by the distal metatarsal transverse ligament<ref name=":10" /> | |||
=== Epidemiology === | === Epidemiology === | ||
Morton's neuroma | More females than males develop Morton's neuroma, with a female-to-male ratio of 5:1.<ref name=":5" /> It affects around 30% of the population. The average age for Morton's neuroma is 50 years. It affects both feet, and in most cases, the third intermetatarsal space is involved, followed by the second (Hauser’s neuroma).<ref name=":1">Mak MS, Chowdhury R, Johnson R. Morton's neuroma: a review of anatomy, pathomechanism, and imaging. Clinical Radiology. 2021 Mar 1;76(3):235-e15.</ref> Multiple locations are scarce.<ref name=":5" /> | ||
== Mechanism of Injury / Pathological Process == | == Mechanism of Injury / Pathological Process == | ||
According to the literature, the most frequent mechanism of injury is nerve entrapment.<ref name=":0" /> As the third common digital nerve is thicker due to the fusion of the medial and lateral plantar nerves, it can be entrapped by the surrounding ligament.<ref name=":0" /> Entrapment neuropathy causes perineural fibrosis and nerve degeneration.<ref name=":0" /> The thickening of the nerve progresses due to vascular hyalinisation, which causes more nerve trauma and entrapment. Wearing high-heel shoes can also add to the pathological process as these shoes cause excessive weight bearing through the forefoot.<ref name=":0" /> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
Individuals with Morton's neuroma can be clinically symptomatic or asymptomatic. Persons with clinically symptomatic Morton's neuroma may present with the following symptoms:<ref name=":0" /> | |||
* Pain or paresthesias in the intermetatarsal region, toes, and dorsal web space. Pain is worsened by weight-bearing or the use of high-heeled shoes. Removing shoes and gently massaging the forefoot can usually relieve the pain. | |||
* Pain is usually sharp and can become debilitating to the point that the patient is afraid or anxious about walking or even putting their foot on the ground.<ref name=":5" /> | |||
* The patient may complain of a burning sensation in the intermetatarsal spaces.<ref name=":11">Mahadevan D, Venkatesan M, Bhatt R, Bhatia M. Diagnostic Accuracy of Clinical Tests for Morton's Neuroma Compared With Ultrasonography. J Foot Ankle Surg. 2015 Jul-Aug;54(4):549-53. </ref> | |||
* A mass can be palpated. | |||
* Symptoms can be present as a result of trauma. | |||
* Patients may describe altered sensation and report that it feels like they have a “pebble in the shoe”.<ref name=":2">Bhatia M, Thomson L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7211826/ Morton’s neuroma–current concepts review]. Journal of Clinical Orthopaedics and Trauma. 2020 May 1;11(3):406-9.</ref> | |||
* Pain worsens with walking or running.<ref name=":2" /> | |||
The presence of [[Hallux Valgus|hallux valgus]] is considered a predisposing factor in the development of Morton's neuroma.<ref name=":2" /> | |||
== Diagnostic Tests == | |||
* [[Metatarsal Squeeze Test|Web space compression test]] (also known as the metatarsal squeeze test): The clinician grasps the medial and lateral aspects of the patient's forefoot and squeezes them with one hand while the other hand palpates the tender area. The aggravation of pain indicates a positive test. | |||
{{#ev:youtube|v=yJ7LUCCmFAU|300}}<ref>The Physio Channel. Metatarsal Squeeze Test for Mortons Neuroma and Mulders Sign. 2019. Available from: https://www.youtube.com/watch?v=yJ7LUCCmFAU[last accessed 15/10/2022]</ref> | |||
* Mulder's sign: a painful, palpable click<ref>Skalina T, Weerakkody Y. Mulder sign. Reference article, Radiopaedia.org. Available from https://radiopaedia.org/articles/mulder-sign (accessed on 14 Oct 2022) </ref> that occurs when pressing and rubbing a neuroma between the metatarsal heads | |||
* Digital nerve stretch test<ref>Cashley DG, Cochrane L. Manipulation in the Treatment of Plantar Digital Neuralgia: A Retrospective Study of 38 Cases. J Chiropr Med. 2015 Jun;14(2):90-8</ref>: The clinician passively holds both ankles in full dorsiflexion while extending the posterior toes of the suspected web space. The test is positive if the patient complains of discomfort in the web space of the affected foot. | |||
[[File:Morton's-MRI.png|thumb|MRI of Morton's neuroma]] | |||
[[File:Morton's-Xray.png|thumb|X-ray of Morton's neuroma]] | |||
[[File:Morton's-US.png|thumb|Ultrasound of Morton's neuroma]] | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
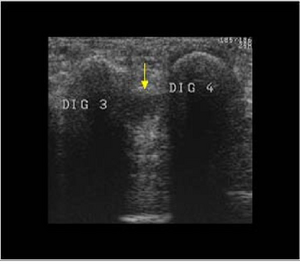
* Ultrasound (US): high diagnostic accuracy. | * Ultrasound (US): high diagnostic accuracy. Proper diagnosis depends on the technique and experience of the person performing the test.<ref name=":5" /><ref name=":1" /> | ||
* Magnetic resonance imaging (MRI) | * Magnetic resonance imaging (MRI) is the gold standard for neuroma identification.<ref name=":2" /> Primary indications for MRI are unclear clinical assessment and cases when more than one intermetatarsal space (IMS) is affected.<ref name=":5" /> | ||
* X-rays | * X-rays are essential as a first-line imaging approach to rule out tarsal–matarsal joint pathologies.<ref>Zaleski M, Tondelli T, Hodel S, Rigling D, Wirth S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8642935/pdf/13047_2021_Article_502.pdf The interphalangeal angle as a novel radiological measurement tool for Morton's neuroma - a matched case-control study]. J Foot Ankle Res. 2021 Dec 4;14(1):62.</ref> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 72: | Line 86: | ||
* Intermetatarsal bursitis | * Intermetatarsal bursitis | ||
* True neuroma | * True neuroma | ||
* Inflammatory arthritis | * [[Arthritis|Inflammatory arthritis]] | ||
* Pigmented villonodular synovitis | * [[Pigmeted Villonodular Synovitis|Pigmented villonodular synovitis]] | ||
* Osteomyelitis | * [[Osteomyelitis]] | ||
* Foreign body granuloma | * Foreign body granuloma | ||
* Stress fracture | * [[Stress Fractures|Stress fracture]] | ||
* Freiberg's infraction | * Freiberg's infraction | ||
* Metatarsophalangeal joint dislocation | * Metatarsophalangeal joint dislocation | ||
== Physiotherapy Management / Interventions == | == Physiotherapy Management / Interventions == | ||
=== Footwear === | === Footwear === | ||
''The goal is to limit nerve compression in the early stages of Morton's neuroma.'' | |||
Tools: patient | |||
Tools: patient education, footwear modification.<blockquote>According to Colò et al.,<ref name=":5" /> if an individual is more than 4.5 months post-diagnosis and the neuroma is larger than 5-6 mm, orthotics and/or shoe modifications are no longer effective for symptom management. At this stage, they offer a palliative solution to achieve an "''acceptable life with pain''."<ref name=":5" /></blockquote> | |||
==== Patient Education ==== | ==== Patient Education ==== | ||
The patient should receive education on the following: | |||
* | * Avoiding narrow and high-heeled shoes | ||
* | * Staying compliant with footwear prescription | ||
* | * Activity modification<ref name=":13">Simpson H. Morton's Neuroma Course. Plus 2022</ref> | ||
[[File:Rocker sole shoe.jpeg|thumb|Rocker sole shoe]] | |||
==== Footwear | ==== Footwear Modification ==== | ||
The most appropriate footwear | The most appropriate footwear will have the following features:<ref name=":5" /><ref name=":3">Matthews BG, Hurn SE, Harding MP, Henry RA, Ware RS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6375221/pdf/13047_2019_Article_320.pdf The effectiveness of non-surgical interventions for common plantar digital compressive neuropathy (Morton's neuroma): a systematic review and meta-analysis]. J Foot Ankle Res. 2019 Feb 13;12:12</ref> | ||
* | * Sufficiently long<ref name=":5" /> | ||
* | * Wide toe box<ref name=":5" /> | ||
* | * Low heel<ref name=":5" /> | ||
* | * Thick external sole, which should not be excessively flexible<ref name=":5" /> | ||
* | * Metatarsal padding<ref name=":3" /> | ||
* A rocker-bottom sole may be helpful<ref>Janisse DJ, Janisse E. Shoe modification and the use of orthoses in | * A rocker-bottom sole may be helpful<ref>Janisse DJ, Janisse E. Shoe modification and the use of orthoses in treating foot and ankle pathology. J Am Acad Orthop Surg. 2008 Mar;16(3):152-8. </ref> | ||
[[File:Metatarsal Pad - Shutterstock Image - ID 1603933129.jpg|thumb|Metatarsal pad]] | |||
=== Orthotics === | === Orthotics === | ||
''The goals of prescribing orthotics are the following:'' | |||
# To displace | # To displace pressure sites | ||
# To provide pain relief | # To provide pain relief | ||
* The most common | * The most common orthotic provided initially is''' the metatarsal bar'''. It aims to: | ||
** | ** Spread the heads of the metatarsals to relieve pressure | ||
** | ** Improve symptoms | ||
* | * There is limited to no evidence of improvement in patient-reported outcomes with the use of ''inversion or eversion insoles'' (varus/valgus foot wedge).<ref name=":2" /> | ||
* According to de Oliveira et al <ref name=":12">de Oliveira HAV, Natour J, Vassalli M, Rosenfeld A, Jennings F, Jones A. Effectiveness of customized insoles in patients with Morton's neuroma: a randomized, controlled, double-blind clinical trial. Clin Rehabil. 2019 Dec;33(12):1898-1907. </ref> | * According to de Oliveira et al.,<ref name=":12">de Oliveira HAV, Natour J, Vassalli M, Rosenfeld A, Jennings F, Jones A. Effectiveness of customized insoles in patients with Morton's neuroma: a randomized, controlled, double-blind clinical trial. Clin Rehabil. 2019 Dec;33(12):1898-1907. </ref> a '''customised insole with metatarsal and arch support''' offers pain relief during ambulation and improves function. | ||
* '''Custom-made toe inserts''' | * '''Custom-made toe inserts '''modelled in silicone rubber can be added when a claw-toe deformity is present.<ref name=":0" /> | ||
* Custom '''orthotics through foam impression methods'''. | * Custom ''' orthotics through foam impression methods'''. The foot is placed in a neutral subtalar position, with a prolonged longitudinal vault to support the first metatarsal (flat support). The goal is to mimic the physiological pattern of metatarsal weight bearing, from lateral to medial, before pressure moves to the big toe.<ref name=":5" /> | ||
=== Steroid Injections === | === Steroid Injections === | ||
The | ''The goal is to provide pain relief.'' | ||
Steroid injections are fairly standard in the management of Morton's neuroma. The injection method varies: they can be guided by ultrasound or a landmark technique. | |||
* A randomised controlled trial by Mahadevan et al.<ref>Mahadevan D, Attwal M, Bhatt R, Bhatia M. [https://online.boneandjoint.org.uk/doi/pdf/10.1302/0301-620X.98B4.36880 Corticosteroid injection for Morton's neuroma with or without ultrasound guidance: a randomised controlled trial]. Bone Joint J. 2016 Apr;98-B(4):498-503.</ref> found no statistical difference in patient outcomes after a steroid injection guided by ultrasound versus an injection not guided by ultrasound. | |||
* Choi et al.<ref name=":15">Choi JY, Lee HI, Hong WH, Suh JS, Hur JW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8173242/pdf/cios-13-266.pdf Corticosteroid Injection for Morton's Interdigital Neuroma: A Systematic Review.] Clin Orthop Surg. 2021 Jun;13(2):266-277.</ref> demonstrated that there was a "satisfactory clinical outcome"<ref name=":15" /> in terms of pain reduction in patients after corticosteroid injections, but 30% of patients eventually required surgery for pain management. | |||
* Lizano-Diez et al.<ref>Lizano-Díez X, Ginés-Cespedosa A, Alentorn-Geli E, Pérez-Prieto D, González-Lucena G, Gamba C, de Zabala S, Solano-López A, Rigol-Ramón P. Corticosteroid Injection for the Treatment of Morton's Neuroma: A Prospective, Double-Blinded, Randomized, Placebo-Controlled Trial. Foot Ankle Int. 2017 Sep;38(9):944-951.</ref> found no difference in pain and function in participants who received an injection of a corticosteroid plus a local anaesthetic versus those who received a local anaesthetic only. | |||
=== Modality === | === Modality === | ||
* [[Extracorporeal Shockwave Therapy |Extracorporeal shockwave therapy (ESWT)]]<ref name=":4">Seok H, Kim SH, Lee SY, Park SW. Extracorporeal Shockwave Therapy in Patients with Morton's Neuroma A Randomized, Placebo-Controlled Trial. J Am Podiatr Med Assoc. 2016 Mar;106(2):93-9.</ref> may reduce pain in patients with Morton's neuroma.<ref name=":4" /> | |||
* [[Transcutaneous Electrical Nerve Stimulation (TENS)|Transcutaneous Electrical Stimulation (TENS)]] can help with pain management.<ref name=":13" /> | |||
=== Manipulation/Mobilisation === | === Manipulation/Mobilisation === | ||
Manipulation/mobilisation | According to Cashley and Cochrane<ref name=":14">Cashley DG, Cochrane L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4523570/pdf/main.pdf Manipulation in the Treatment of Plantar Digital Neuralgia: A Retrospective Study of 38 Cases]. J Chiropr Med. 2015 Jun;14(2):90-8.</ref>, manipulation and mobilisation of the other foot and ankle joints can decrease foot pain in patients diagnosed with plantar digital neuralgia (Morton's neuroma). The authors recommend performing joint manipulation once a week for four weeks, followed by two more visits at 14-day intervals.<ref name=":14" /> | ||
=== Strengthening Exercises === | |||
According to Helene Simpson,<ref name=":13" /> strengthening exercises for the toe flexors and the intrinsics can help with muscle activation during the mid-stance of the gait cycle and prevent the metatarsal heads from dropping. | |||
== | == Other Treatment Options == | ||
Surgery is considered when conservative treatment fails or the patient is no longer willing to adjust their lifestyle to manage symptoms of Morton's neuroma. The following operative and non-operative treatment options are available: | |||
* Surgical nerve excision (neurectomy)<ref name=":16">Samaila EM, Ambrosini C, Negri S, Maluta T, Valentini R, Magnan B. Can percutaneous alcoholization of Morton's neuroma with phenol by electrostimulation guidance be an alternative to surgical excision? Long-term results. Foot Ankle Surg. 2020 Apr;26(3):314-319.</ref> | |||
* Surgical nerve decompression<ref>Jain S, Mannan K. The diagnosis and management of Morton’s neuroma: a literature review. Foot & Ankle Specialist. 2013 Aug;6(4):307-17.</ref> | |||
* Ultrasound-guided percutaneous radio-frequency <ref>Masala S, Cuzzolino A, Morini M, Raguso M, Fiori R. Ultrasound-Guided Percutaneous Radiofrequency for the Treatment of Morton's Neuroma. Cardiovasc Intervent Radiol. 2018 Jan;41(1):137-144.</ref> | |||
** Reduction of pain intensity within one week | |||
** Stabilisation of pain symptoms one month and one year following the procedure | |||
** Quality of life improvement within six months | |||
* Alcohol injection<ref>Hughes RJ, Ali K, Jones H, Kendall S, Connell DA. [https://ajronline.org/doi/epdf/10.2214/AJR.06.1463 Treatment of Morton's neuroma with alcohol injection under sonographic guidance: follow-up of 101 cases.] AJR Am J Roentgenol. 2007 Jun;188(6):1535-9.</ref> | |||
** Partial or total pain symptoms were improved | |||
** Decreased neuroma size within six months | |||
* Percutaneous electrostimulation-guided alcoholisation with phenol<ref name=":16" /> | |||
** Minimally invasive procedure | |||
** Complications may include temporary pain at the site of injection that resolves within the first 48 hours and a risk of developing necrotic complications<ref>Ortu S, Fiori E, Bagnoli I,Valente a, Pisanu F, Caggiari G, Doria C, Milano L. [https://journals.sagepub.com/doi/epub/10.1177/22104917221116392 Complications of alcohol injections for Morton’s neuroma]. Journal of Orthopaedics, Trauma and Rehabilitation. 2022;29(2). </ref> | |||
== | == Conclusion == | ||
# Appropriate footwear should limit nerve compression. | |||
# Orthotics are prescribed for pain relief. | |||
# Steroid injections are standard pain relieving procedures in Morton's neuroma. | |||
# TENS and Shockwave therapy assist with pain management. | |||
# Manipulation and mobilisation of the other foot and ankle joints decrease pain. | |||
# Strengthening exercises program for the toe flexors and the intrinsics assist with muscle activation during the gait cycle. | |||
== Resources | == Resources == | ||
# [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6375221/pdf/13047_2019_Article_320.pdf The effectiveness of non-surgical interventions for common plantar digital compressive neuropathy (Morton’s neuroma): a systematic review and meta-analysis] | |||
# [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7944831/pdf/ACTA-91-60.pdf The effectiveness of shoe modifications and orthotics in the conservative treatment of Civinini-Morton syndrome: state of the art] | |||
# [https://www.ajronline.org/doi/epdf/10.2214/AJR.16.17276 Second and Third Metatarsophalangeal Plantar Plate Tears: Diagnostic Performance of Direct and Indirect MRI Features Using Surgical Findings as the Reference Standard] | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Foot - Conditions]] | |||
[[Category:Foot - Anatomy]] | |||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
Latest revision as of 18:25, 9 January 2024
Introduction[edit | edit source]
Civinini Morton’s Syndrome (CMS) is more commonly known as Morton’s neuroma. Weinfield and Myerson[1] have also proposed the term "interdigital neuritis", which better describes the pathology of this condition. Neural degeneration and perineural fibrosis are typical of Morton's neuroma[2]; the presence of inflammatory tissue in histological examination justifies the description of Morton's neuroma as perineural fibrosis.[3] Clinical symptoms that can help with diagnosis include pain and abnormal forefoot sensation. Conservative treatment, including lifestyle adjustment, may not always be practical. Thus, patients may choose to have surgery or various types of ultrasound-guided percutaneous injections to manage this condition.
Clinically Relevant Anatomy[edit | edit source]
Magnetic resonance imaging (MRI) shows the medial and lateral plantar nerves arise from the posterior tibial nerve.[4] The bifurcation of the tibial nerve occurs inside the retinaculum or proximal to the flexor retinaculum.[5] The two plantar nerves penetrate the tunnel made of the deep fascia of the abductor hallucis muscle and the fibrous septum, which connects the fascia to the bone.[5]
The medial plantar nerve (MPN) is the larger of the two plantar nerves. It originates under the flexor retinaculum (also known as the laciniate ligament) and passes between abductor hallucis and flexor digitorum brevis. Upon reaching the metatarsal bases, it divides into three common digital plantar nerves.[6] The MPN innervates the abductor hallucis, flexor hallucis brevis, flexor digitorum brevis and the first lumbrical of the foot.
The lateral plantar nerve (LPN) innervates abductor digiti minimi, flexor digiti minimi brevis, quadratus plantae, the three lateral lumbricals of the foot, adductor hallucis, the plantar interossei, and the dorsal interossei.
The common plantar digital (CPD) nerves pass under the intermetatarsal ligaments. They go through the plantar aponeurosis and divide into two branches, which supply the plantar skin of the toes. Smaller portions of the CPD nerves innervate the adjacent metatarsals, metatarsophalangeal joints and plantar skin under the metatarsal heads.[7]
The third common digital nerve begins as the medial plantar nerve and receives a communicating branch from the lateral plantar nerve. Because it passes through the narrow space deep to the transverse metatarsal ligament, it becomes less mobile, especially during weight-bearing activities.[7]
The branches of the common digital nerve in the third plantar webspace are most commonly affected in Morton's neuroma. It has been proposed that the location of this nerve (i.e. near the narrow space of the transverse metatarsal ligament) may be why Morton's neuroma often occurs within the third intermetatarsal space.[7]
Neuroma[edit | edit source]
A neuroma is also referred to as a pinched nerve. Morton's neuroma is a compressive neuropathy of the common plantar digital nerve caused by an entrapment of the nerve between the intermetatarsal ligaments.
Aetiology[edit | edit source]
There are several aetiopathogenetic theories behind the development of Morton's neuroma. These include:
- Chronic traction damage[8]
- Chronic, repetitive trauma[8]
- Ischaemia of vasa nervorum (Vasa nervorum = nutrient vessels that provide blood supply to each peripheral nerve from adjacent blood vessels)[7][8]
- Entrapment or mechanical compression[3][9]
- Inflammation due to intermetatarsal bursitis[3]
Anatomical considerations:
- The third common digital nerve is thicker than the others due to an anastomosis between two nerve trunks[7]
- The fourth ray is more mobile than the third, which might lead to inflammation[7]
- The plantar nerve is compressed by the distal metatarsal transverse ligament[3]
Epidemiology[edit | edit source]
More females than males develop Morton's neuroma, with a female-to-male ratio of 5:1.[7] It affects around 30% of the population. The average age for Morton's neuroma is 50 years. It affects both feet, and in most cases, the third intermetatarsal space is involved, followed by the second (Hauser’s neuroma).[10] Multiple locations are scarce.[7]
Mechanism of Injury / Pathological Process[edit | edit source]
According to the literature, the most frequent mechanism of injury is nerve entrapment.[9] As the third common digital nerve is thicker due to the fusion of the medial and lateral plantar nerves, it can be entrapped by the surrounding ligament.[9] Entrapment neuropathy causes perineural fibrosis and nerve degeneration.[9] The thickening of the nerve progresses due to vascular hyalinisation, which causes more nerve trauma and entrapment. Wearing high-heel shoes can also add to the pathological process as these shoes cause excessive weight bearing through the forefoot.[9]
Clinical Presentation[edit | edit source]
Individuals with Morton's neuroma can be clinically symptomatic or asymptomatic. Persons with clinically symptomatic Morton's neuroma may present with the following symptoms:[9]
- Pain or paresthesias in the intermetatarsal region, toes, and dorsal web space. Pain is worsened by weight-bearing or the use of high-heeled shoes. Removing shoes and gently massaging the forefoot can usually relieve the pain.
- Pain is usually sharp and can become debilitating to the point that the patient is afraid or anxious about walking or even putting their foot on the ground.[7]
- The patient may complain of a burning sensation in the intermetatarsal spaces.[11]
- A mass can be palpated.
- Symptoms can be present as a result of trauma.
- Patients may describe altered sensation and report that it feels like they have a “pebble in the shoe”.[12]
- Pain worsens with walking or running.[12]
The presence of hallux valgus is considered a predisposing factor in the development of Morton's neuroma.[12]
Diagnostic Tests[edit | edit source]
- Web space compression test (also known as the metatarsal squeeze test): The clinician grasps the medial and lateral aspects of the patient's forefoot and squeezes them with one hand while the other hand palpates the tender area. The aggravation of pain indicates a positive test.
- Mulder's sign: a painful, palpable click[14] that occurs when pressing and rubbing a neuroma between the metatarsal heads
- Digital nerve stretch test[15]: The clinician passively holds both ankles in full dorsiflexion while extending the posterior toes of the suspected web space. The test is positive if the patient complains of discomfort in the web space of the affected foot.
Diagnostic Procedures[edit | edit source]
- Ultrasound (US): high diagnostic accuracy. Proper diagnosis depends on the technique and experience of the person performing the test.[7][10]
- Magnetic resonance imaging (MRI) is the gold standard for neuroma identification.[12] Primary indications for MRI are unclear clinical assessment and cases when more than one intermetatarsal space (IMS) is affected.[7]
- X-rays are essential as a first-line imaging approach to rule out tarsal–matarsal joint pathologies.[16]
Differential Diagnosis[edit | edit source]
The differential diagnosis includes the following conditions:[9]
- Intermetatarsal bursitis
- True neuroma
- Inflammatory arthritis
- Pigmented villonodular synovitis
- Osteomyelitis
- Foreign body granuloma
- Stress fracture
- Freiberg's infraction
- Metatarsophalangeal joint dislocation
Physiotherapy Management / Interventions[edit | edit source]
Footwear[edit | edit source]
The goal is to limit nerve compression in the early stages of Morton's neuroma.
Tools: patient education, footwear modification.
According to Colò et al.,[7] if an individual is more than 4.5 months post-diagnosis and the neuroma is larger than 5-6 mm, orthotics and/or shoe modifications are no longer effective for symptom management. At this stage, they offer a palliative solution to achieve an "acceptable life with pain."[7]
Patient Education[edit | edit source]
The patient should receive education on the following:
- Avoiding narrow and high-heeled shoes
- Staying compliant with footwear prescription
- Activity modification[17]
Footwear Modification[edit | edit source]
The most appropriate footwear will have the following features:[7][18]
- Sufficiently long[7]
- Wide toe box[7]
- Low heel[7]
- Thick external sole, which should not be excessively flexible[7]
- Metatarsal padding[18]
- A rocker-bottom sole may be helpful[19]
Orthotics[edit | edit source]
The goals of prescribing orthotics are the following:
- To displace pressure sites
- To provide pain relief
- The most common orthotic provided initially is the metatarsal bar. It aims to:
- Spread the heads of the metatarsals to relieve pressure
- Improve symptoms
- There is limited to no evidence of improvement in patient-reported outcomes with the use of inversion or eversion insoles (varus/valgus foot wedge).[12]
- According to de Oliveira et al.,[20] a customised insole with metatarsal and arch support offers pain relief during ambulation and improves function.
- Custom-made toe inserts modelled in silicone rubber can be added when a claw-toe deformity is present.[9]
- Custom orthotics through foam impression methods. The foot is placed in a neutral subtalar position, with a prolonged longitudinal vault to support the first metatarsal (flat support). The goal is to mimic the physiological pattern of metatarsal weight bearing, from lateral to medial, before pressure moves to the big toe.[7]
Steroid Injections[edit | edit source]
The goal is to provide pain relief.
Steroid injections are fairly standard in the management of Morton's neuroma. The injection method varies: they can be guided by ultrasound or a landmark technique.
- A randomised controlled trial by Mahadevan et al.[21] found no statistical difference in patient outcomes after a steroid injection guided by ultrasound versus an injection not guided by ultrasound.
- Choi et al.[22] demonstrated that there was a "satisfactory clinical outcome"[22] in terms of pain reduction in patients after corticosteroid injections, but 30% of patients eventually required surgery for pain management.
- Lizano-Diez et al.[23] found no difference in pain and function in participants who received an injection of a corticosteroid plus a local anaesthetic versus those who received a local anaesthetic only.
Modality[edit | edit source]
- Extracorporeal shockwave therapy (ESWT)[24] may reduce pain in patients with Morton's neuroma.[24]
- Transcutaneous Electrical Stimulation (TENS) can help with pain management.[17]
Manipulation/Mobilisation[edit | edit source]
According to Cashley and Cochrane[25], manipulation and mobilisation of the other foot and ankle joints can decrease foot pain in patients diagnosed with plantar digital neuralgia (Morton's neuroma). The authors recommend performing joint manipulation once a week for four weeks, followed by two more visits at 14-day intervals.[25]
Strengthening Exercises[edit | edit source]
According to Helene Simpson,[17] strengthening exercises for the toe flexors and the intrinsics can help with muscle activation during the mid-stance of the gait cycle and prevent the metatarsal heads from dropping.
Other Treatment Options[edit | edit source]
Surgery is considered when conservative treatment fails or the patient is no longer willing to adjust their lifestyle to manage symptoms of Morton's neuroma. The following operative and non-operative treatment options are available:
- Surgical nerve excision (neurectomy)[26]
- Surgical nerve decompression[27]
- Ultrasound-guided percutaneous radio-frequency [28]
- Reduction of pain intensity within one week
- Stabilisation of pain symptoms one month and one year following the procedure
- Quality of life improvement within six months
- Alcohol injection[29]
- Partial or total pain symptoms were improved
- Decreased neuroma size within six months
- Percutaneous electrostimulation-guided alcoholisation with phenol[26]
- Minimally invasive procedure
- Complications may include temporary pain at the site of injection that resolves within the first 48 hours and a risk of developing necrotic complications[30]
Conclusion[edit | edit source]
- Appropriate footwear should limit nerve compression.
- Orthotics are prescribed for pain relief.
- Steroid injections are standard pain relieving procedures in Morton's neuroma.
- TENS and Shockwave therapy assist with pain management.
- Manipulation and mobilisation of the other foot and ankle joints decrease pain.
- Strengthening exercises program for the toe flexors and the intrinsics assist with muscle activation during the gait cycle.
Resources[edit | edit source]
- The effectiveness of non-surgical interventions for common plantar digital compressive neuropathy (Morton’s neuroma): a systematic review and meta-analysis
- The effectiveness of shoe modifications and orthotics in the conservative treatment of Civinini-Morton syndrome: state of the art
- Second and Third Metatarsophalangeal Plantar Plate Tears: Diagnostic Performance of Direct and Indirect MRI Features Using Surgical Findings as the Reference Standard
References[edit | edit source]
- ↑ Weinfeld SB, Myerson MS. Interdigital Neuritis: Diagnosis and Treatment. J Am Acad Orthop Surg. 1996 Nov;4(6):328-335.
- ↑ Riddick DA, Riddick DH, Jorge M. 7 - Footwear: foundation for lower extremity orthoses. In: Chui KK, Jorge M, Yen S-C, Lusardi MM, editors. Orthotics and prosthetics in rehabilitation (Fourth Edition). Elsevier, 2020. p164-82.
- ↑ 3.0 3.1 3.2 3.3 Jain S, Mannan K. The diagnosis and management of Morton's neuroma: a literature review. Foot Ankle Spec. 2013 Aug;6(4):307-17.
- ↑ Govsa F, Bilge O, Ozer MA. Anatomical study of the communicating branches between the medial and lateral plantar nerves. Surgical and Radiologic Anatomy. 2005 Dec;27(5):377-81.
- ↑ 5.0 5.1 Torres AL, Ferreira MC. Study of the anatomy of the tibial nerve and its branches in the distal medial leg. Acta ortopedica brasileira. 2012;20:157-64.
- ↑ Koo GB, Lee JH, Jang JH, Song IH, Kim JY. Superficial course of the medial plantar nerve: case report. Anatomy & cell biology. 2019 Mar 1;52(1):87-9.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 7.14 7.15 7.16 7.17 7.18 Colò G, Rava A, Samaila EM, Palazzolo A, Talesa G, Schiraldi M, Magnan B, Ferracini R, Felli L. The effectiveness of shoe modifications and orthotics in the conservative treatment of Civinini-Morton syndrome: state of the art. Acta Biomed. 2020 May 30;91(4-S):60-68.
- ↑ 8.0 8.1 8.2 Hassouna H, Singh D. Morton's metatarsalgia: pathogenesis, aetiology and current management. Acta Orthop Belg. 2005 Dec;71(6):646-55.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 Bencardino J, Rosenberg ZS, Beltran J, Liu X, Marty-Delfaut E. Morton's neuroma: is it always symptomatic?. American journal of roentgenology. 2000 Sep;175(3):649-53.
- ↑ 10.0 10.1 Mak MS, Chowdhury R, Johnson R. Morton's neuroma: a review of anatomy, pathomechanism, and imaging. Clinical Radiology. 2021 Mar 1;76(3):235-e15.
- ↑ Mahadevan D, Venkatesan M, Bhatt R, Bhatia M. Diagnostic Accuracy of Clinical Tests for Morton's Neuroma Compared With Ultrasonography. J Foot Ankle Surg. 2015 Jul-Aug;54(4):549-53.
- ↑ 12.0 12.1 12.2 12.3 12.4 Bhatia M, Thomson L. Morton’s neuroma–current concepts review. Journal of Clinical Orthopaedics and Trauma. 2020 May 1;11(3):406-9.
- ↑ The Physio Channel. Metatarsal Squeeze Test for Mortons Neuroma and Mulders Sign. 2019. Available from: https://www.youtube.com/watch?v=yJ7LUCCmFAU[last accessed 15/10/2022]
- ↑ Skalina T, Weerakkody Y. Mulder sign. Reference article, Radiopaedia.org. Available from https://radiopaedia.org/articles/mulder-sign (accessed on 14 Oct 2022)
- ↑ Cashley DG, Cochrane L. Manipulation in the Treatment of Plantar Digital Neuralgia: A Retrospective Study of 38 Cases. J Chiropr Med. 2015 Jun;14(2):90-8
- ↑ Zaleski M, Tondelli T, Hodel S, Rigling D, Wirth S. The interphalangeal angle as a novel radiological measurement tool for Morton's neuroma - a matched case-control study. J Foot Ankle Res. 2021 Dec 4;14(1):62.
- ↑ 17.0 17.1 17.2 Simpson H. Morton's Neuroma Course. Plus 2022
- ↑ 18.0 18.1 Matthews BG, Hurn SE, Harding MP, Henry RA, Ware RS. The effectiveness of non-surgical interventions for common plantar digital compressive neuropathy (Morton's neuroma): a systematic review and meta-analysis. J Foot Ankle Res. 2019 Feb 13;12:12
- ↑ Janisse DJ, Janisse E. Shoe modification and the use of orthoses in treating foot and ankle pathology. J Am Acad Orthop Surg. 2008 Mar;16(3):152-8.
- ↑ de Oliveira HAV, Natour J, Vassalli M, Rosenfeld A, Jennings F, Jones A. Effectiveness of customized insoles in patients with Morton's neuroma: a randomized, controlled, double-blind clinical trial. Clin Rehabil. 2019 Dec;33(12):1898-1907.
- ↑ Mahadevan D, Attwal M, Bhatt R, Bhatia M. Corticosteroid injection for Morton's neuroma with or without ultrasound guidance: a randomised controlled trial. Bone Joint J. 2016 Apr;98-B(4):498-503.
- ↑ 22.0 22.1 Choi JY, Lee HI, Hong WH, Suh JS, Hur JW. Corticosteroid Injection for Morton's Interdigital Neuroma: A Systematic Review. Clin Orthop Surg. 2021 Jun;13(2):266-277.
- ↑ Lizano-Díez X, Ginés-Cespedosa A, Alentorn-Geli E, Pérez-Prieto D, González-Lucena G, Gamba C, de Zabala S, Solano-López A, Rigol-Ramón P. Corticosteroid Injection for the Treatment of Morton's Neuroma: A Prospective, Double-Blinded, Randomized, Placebo-Controlled Trial. Foot Ankle Int. 2017 Sep;38(9):944-951.
- ↑ 24.0 24.1 Seok H, Kim SH, Lee SY, Park SW. Extracorporeal Shockwave Therapy in Patients with Morton's Neuroma A Randomized, Placebo-Controlled Trial. J Am Podiatr Med Assoc. 2016 Mar;106(2):93-9.
- ↑ 25.0 25.1 Cashley DG, Cochrane L. Manipulation in the Treatment of Plantar Digital Neuralgia: A Retrospective Study of 38 Cases. J Chiropr Med. 2015 Jun;14(2):90-8.
- ↑ 26.0 26.1 Samaila EM, Ambrosini C, Negri S, Maluta T, Valentini R, Magnan B. Can percutaneous alcoholization of Morton's neuroma with phenol by electrostimulation guidance be an alternative to surgical excision? Long-term results. Foot Ankle Surg. 2020 Apr;26(3):314-319.
- ↑ Jain S, Mannan K. The diagnosis and management of Morton’s neuroma: a literature review. Foot & Ankle Specialist. 2013 Aug;6(4):307-17.
- ↑ Masala S, Cuzzolino A, Morini M, Raguso M, Fiori R. Ultrasound-Guided Percutaneous Radiofrequency for the Treatment of Morton's Neuroma. Cardiovasc Intervent Radiol. 2018 Jan;41(1):137-144.
- ↑ Hughes RJ, Ali K, Jones H, Kendall S, Connell DA. Treatment of Morton's neuroma with alcohol injection under sonographic guidance: follow-up of 101 cases. AJR Am J Roentgenol. 2007 Jun;188(6):1535-9.
- ↑ Ortu S, Fiori E, Bagnoli I,Valente a, Pisanu F, Caggiari G, Doria C, Milano L. Complications of alcohol injections for Morton’s neuroma. Journal of Orthopaedics, Trauma and Rehabilitation. 2022;29(2).