Thermoregulation and Exercise in the Heat and Cold: Difference between revisions
No edit summary |
m (Protected "Thermoregulation and Exercise in the Heat and Cold": Course Page ([Edit=⧼protect-level-ppadmin⧽] (indefinite) [Move=⧼protect-level-ppadmin⧽] (indefinite))) |
||
| (12 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Wanda van Niekerk|Wanda van Niekerk]] based on the course by [https://members.physio-pedia.com/instructor/dr-james-laskin// James Laskin]<br> | '''Original Editor '''- [[User:Wanda van Niekerk|Wanda van Niekerk]] based on the course by [https://members.physio-pedia.com/instructor/dr-james-laskin// James Laskin]<br> | ||
| Line 14: | Line 10: | ||
* Humans are homeothermic - this means that the internal body temperature is physiologically regulated and kept nearly constant despite environmental temperature changes.<ref name=":0">Cramer MN, Gagnon D, Laitano O, Crandall CG. [https://journals.physiology.org/doi/full/10.1152/physrev.00047.2021?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org Human temperature regulation under heat stress in health, disease, and injury.] Physiological reviews. 2022 Oct 1;102(4):1907-89.</ref> | * Humans are homeothermic - this means that the internal body temperature is physiologically regulated and kept nearly constant despite environmental temperature changes.<ref name=":0">Cramer MN, Gagnon D, Laitano O, Crandall CG. [https://journals.physiology.org/doi/full/10.1152/physrev.00047.2021?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org Human temperature regulation under heat stress in health, disease, and injury.] Physiological reviews. 2022 Oct 1;102(4):1907-89.</ref> | ||
* Fluctuations in body temperature are usually no more than 1. | * Fluctuations in body temperature are usually no more than 1.0° C (degrees Celsius) or 1.8° F (degrees Fahrenheit) | ||
* Body temperature is a reflection of the balance between heat production and heat loss. If this balance is disturbed, | * Body temperature is a reflection of the balance between heat production and heat loss. If this balance is disturbed, there will be body temperature changes.<ref name=":0" /> | ||
* Normal baseline range of body temperature | * Normal baseline range of body temperature is 36.1° to 37.8 C (97.0° - 100.0° F) | ||
** | ** situations that will cause a change in normal baseline temperatures: | ||
*** | *** fever due to illness | ||
*** | *** extreme conditions of heat or cold | ||
*** | *** prolonged heavy exercise | ||
== Transfer of Heat between Body and Environment == | == Transfer of Heat between Body and Environment == | ||
* Metabolic heat is produced by active tissues<ref name=":0" /> | * [[File:Thermoregulation Scale.jpg|thumb|alt=|400x400px|Figure 1. Thermoregulation Scale]]Metabolic heat is produced by active tissues<ref name=":0" /> | ||
* Heat moves from the body core (deep within the body) to the body shell (skin) via blood | * Heat moves from the body core (deep within the body) to the body shell (skin) via the blood | ||
* When the heat reaches the skin it can be dissipated by conduction, convection, radiation and evaporation | * When the heat reaches the skin it can be dissipated by conduction, convection, radiation and evaporation | ||
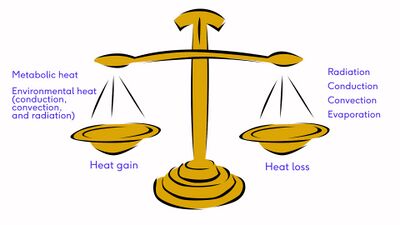
* Maintaining a constant internal body temperature is dependent on the body's ability to balance heat gain (from metabolic processes and the environment) with heat loss. Figure 1. demonstrates this balance: | * Maintaining a constant internal body temperature is dependent on the body's ability to balance heat gain (from metabolic processes and the environment) with heat loss. Figure 1. demonstrates this balance: | ||
** | ** heat gain: metabolic heat and environmental heat (conduction, convection, radiation) | ||
** | ** heat loss: radiation, conduction, convection, evaporation | ||
* Conduction | * Conduction = heat transfer from one material to another through direct contact<ref name=":0" /> | ||
** | ** example: sitting on cold or hot metal bleachers watching a sports event | ||
* Convection | * Convection = heat transfer by the movement of gas or liquid across a surface<ref name=":0" /> | ||
** | ** during movement, such as playing sports, the air around us passes over our skin and heat is exchanged with air molecules | ||
** | ** greater movement of air results in greater heat exchange | ||
** | ** major daily thermoregulatory factor | ||
* Radiation<ref name=":0" /> | * Radiation = heat transfer in the form of infrared rays<ref name=":0" /> | ||
** | ** the body can give off or receive radiant heat | ||
** | ** major daily thermoregulatory factor | ||
* Evaporation<ref name=":0" /> | * Evaporation = heat loss via phase change from liquid to gas<ref name=":0" /> | ||
** | ** primary way for heat loss during exercise | ||
** | ** as body core temperature increases, sweat production increases, sweat turns into vapour when it reaches the skin and cooling occurs | ||
** | ** sweat must evaporate to have a cooling effect, dripping sweat provides little or no cooling effect | ||
=== Challenges with the Transfer of Body Heat === | === Challenges with the Transfer of Body Heat === | ||
* Humidity and heat loss<ref>Griggs KE, Stephenson BT, Price MJ, Goosey-Tolfrey VL. Heat-related issues and practical applications for Paralympic athletes at Tokyo 2020. Temperature. 2020 Jan 2;7(1):37-57.</ref> | * Humidity and heat loss<ref>Griggs KE, Stephenson BT, Price MJ, Goosey-Tolfrey VL. Heat-related issues and practical applications for Paralympic athletes at Tokyo 2020. Temperature. 2020 Jan 2;7(1):37-57.</ref> | ||
** | ** high humidity limits the evaporation of sweat as the air contains many H<sub>2</sub>O molecules | ||
** | ** low humidity provides an ideal opportunity for evaporation | ||
* Prolonged sweat evaporation without adequate fluid intake can cause dehydration | * Prolonged sweat evaporation without adequate fluid intake can cause dehydration | ||
* Temperature of skin greater than the temperature of the environment | * Temperature of the skin is greater than the temperature of the environment = heat loss through conduction, convection and radiation and evaporation | ||
* Temperature of the environment greater than skin temperature | * Temperature of the environment is greater than skin temperature = heat can only be removed through evaporation | ||
* In hot humid situations, evaporation of sweat is limited and convection occurs from the environment to the skin (thus heat is gained) | * In hot humid situations, evaporation of sweat is limited and convection occurs from the environment to the skin (thus heat is gained) | ||
== Thermoregulatory Control == | == Thermoregulatory Control == | ||
The body's thermoregulatory responses are very effective for normal ranges of body and air temperature. Core body temperature at rest is regulated at approximately | The body's thermoregulatory responses are very effective for normal ranges of body and air temperature. Core body temperature at rest is regulated at approximately 37° C (98.6° F). If the internal (core) body temperature exceeds 40° C (104°F), physiological function will be inhibited. Humans are able to briefly withstand core temperatures below 35° C (95° F) or above 41° C (105.8° F) . | ||
* Body's thermoregulatory centre - preoptic anterior hypothalamus (POAH)<ref name=":4">Xu X, Rioux TP, Castellani MP. [https://www.sciencedirect.com/science/article/pii/S0306456523000323 Three dimensional models of human thermoregulation: A review.] Journal of Thermal Biology. 2023 Feb 4:103491.</ref> | * Body's thermoregulatory centre - preoptic anterior hypothalamus (POAH)<ref name=":4">Xu X, Rioux TP, Castellani MP. [https://www.sciencedirect.com/science/article/pii/S0306456523000323 Three dimensional models of human thermoregulation: A review.] Journal of Thermal Biology. 2023 Feb 4:103491.</ref> | ||
| Line 69: | Line 65: | ||
**** vasodilation to enhance heat loss | **** vasodilation to enhance heat loss | ||
** eccrine sweat glands | ** eccrine sweat glands | ||
*** sufficient rise in core and skin temperature - POAH sends a signal via the sympathetic nervous system to eccrine sweat glands, leading to active secretion of sweat. Read more on the Physiology of Sweat | *** sufficient rise in core and skin temperature - POAH sends a signal via the sympathetic nervous system to eccrine sweat glands, leading to active secretion of sweat. Read more on the [[Physiology of Sweat]] | ||
** endocrine glands | ** endocrine glands | ||
*** the effect of various hormones results in an increased cellular metabolic rate, and increased metabolism leads to an increase in heat production | *** the effect of various hormones results in an increased cellular metabolic rate, and increased metabolism leads to an increase in heat production | ||
| Line 79: | Line 75: | ||
=== Cardiovascular Response === | === Cardiovascular Response === | ||
Independent | Independent of the environment, exercise increases heat load due to muscle work and increased metabolism. The POAH sends signals via the sympathetic nervous system to the skin arterioles to vasodilate, which increases conductive and evaporative heat loss. Vasoconstriction occurs to direct blood from non-essential tissue such as the gut, liver and kidneys. Cardiac output further increases via an increase in heart rate and changes in contractility to maintain the cardiac output to working muscle. Due to sweating, blood volume decreases and the ability to increase stroke volume is also limited due to peripheral blood pooling. Heart rate increases to compensate for the decrease in stroke volume (a phenomenon known as cardiovascular drift).<ref name=":1" /> | ||
=== Fluid Balance === | === Fluid Balance === | ||
Hot environmental temperatures and strenuous physical activity increase skin and core temperatures. The POAH controls the sweat glands. Sweat forms in the coiled section of the sweat gland and initially the electrolyte composition is the same as that of blood as plasma is the source of sweat formation. The filtrate of plasma moves through the duct of the sweat gland and sodium and chloride are reabsorbed back into the tissue and then into the blood. | Hot environmental temperatures and strenuous physical activity increase skin and core temperatures. The POAH controls the sweat glands. Sweat forms in the coiled section of the sweat gland and initially the electrolyte composition is the same as that of blood as plasma is the source of sweat formation. The filtrate of plasma moves through the duct of the sweat gland and sodium and chloride are reabsorbed back into the tissue and then into the blood. Thus, the sweat that is released onto the skin has fewer electrolytes than plasma.<ref name=":1" /> | ||
* Light sweating - filtrate travels slowly through the duct | * Light sweating - filtrate travels slowly through the duct, so there is more time for reabsorption of sodium and chloride and sweat is very diluted | ||
* Heavy sweating - less time for reabsorption of sodium and chloride as filtrate moves | * Heavy sweating - there is less time for reabsorption of sodium and chloride as filtrate moves more quickly through the sweat duct, so the sodium and chloride content of sweat is higher | ||
There is a difference in the electrolyte concentration of sweat in trained versus untrained individuals. With training and heat acclimation more sodium and chloride are reabsorbed and sweat is more dilute. Concentrations of potassium, calcium and magnesium stay more or less the same. Exercise in hot and humid conditions can result in a loss of 2.5 % to 3.2 % of body weight through sweat. High rates of sweating reduce blood volume. This leads to an increased heart rate and eventually leads to a decrease in cardiac output and this affects athletic performance.<ref name=":1" /> | There is a difference in the electrolyte concentration of sweat in trained versus untrained individuals. With training and heat acclimation, more sodium and chloride are reabsorbed and sweat is more dilute. Concentrations of potassium, calcium and magnesium stay more or less the same. Exercise in hot and humid conditions can result in a loss of 2.5 % to 3.2 % of body weight through sweat. High rates of sweating reduce blood volume. This leads to an increased heart rate and eventually leads to a decrease in cardiac output and this affects athletic performance.<ref name=":1" /> | ||
Read this article: | Read this article: [https://journals.lww.com/acsm-msse/Fulltext/2007/02000/Exercise_and_Fluid_Replacement.22.aspx Exercise and Fluid Replacement]<ref>Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, Stachenfeld NS, American College of Sports Medicine. American College of Sports Medicine position stand. [https://journals.lww.com/acsm-msse/Fulltext/2007/02000/Exercise_and_Fluid_Replacement.22.aspx Exercise and fluid replacement.] Medicine and science in sports and exercise. 2007 Feb;39(2):377-90.</ref> | ||
== Health Risks with Exercise in the Heat == | == Health Risks with Exercise in the Heat == | ||
| Line 100: | Line 96: | ||
* air velocity | * air velocity | ||
* radiant heat sources | * radiant heat sources | ||
* clothing | * clothing<ref name=":2" /> | ||
** athletes and officials with low metabolic heat production: wear light-coloured, loose-fitting, sun-protective clothing | |||
** athletes with high metabolic heat production: clothing should not impair direct sweat evaporation from the skin | |||
** Read: [https://sportsmedicine-open.springeropen.com/articles/10.1186/s40798-022-00449-4 The role of sports clothing in thermoregulation, comfort, and performance during exercise in the heat: a narrative review]<ref>Di Domenico I, Hoffmann SM, Collins PK. [https://sportsmedicine-open.springeropen.com/articles/10.1186/s40798-022-00449-4 The Role of Sports Clothing in Thermoregulation, Comfort, and Performance During Exercise in the Heat: A Narrative Review.] Sports Medicine-Open. 2022 Dec;8(1):58.</ref> | |||
=== Thermal Stress === | === Thermal Stress === | ||
External heat stress can be measured with: | External heat stress can be measured with: | ||
* | * heat index | ||
* | **[https://www.calculator.net/heat-index-calculator.html heat index calculator] | ||
* wet-bulb globe temperature (WBGT)<ref>Hosokawa Y, Adams WM, Casa DJ, Vanos JK, Cooper ER, Grundstein AJ, Jay O, McDermott BP, Otani H, Raukar NP, Stearns RL. [https://europepmc.org/article/pmc/8063664 Roundtable on preseason heat safety in secondary school athletics: environmental monitoring during activities in the heat.] Journal of athletic training. 2021 Apr 1;56(4):362-71.</ref> | |||
=== Health Consequences of Heat === | === Health Consequences of Heat === | ||
Exposure to heat stress from the environment and metabolically generated heat can cause<ref>Nowak AS, Kennelley GE, Krabak BJ, Roberts WO, Tenforde KM, Tenforde AS. Endurance athletes and climate change. The Journal of Climate Change and Health. 2022 Feb 1:100118.</ref>: | Exposure to heat stress from the environment and metabolically generated heat can cause<ref>Nowak AS, Kennelley GE, Krabak BJ, Roberts WO, Tenforde KM, Tenforde AS. Endurance athletes and climate change. The Journal of Climate Change and Health. 2022 Feb 1:100118.</ref>: | ||
* | * heat cramps | ||
* | * heat exhaustion | ||
* | * heatstroke | ||
Read more about [[Heat Illness in Sports]] | Read more about [[Heat Illness in Sports]] | ||
=== Guidelines for | === Guidelines for Practising and Competing in Heat === | ||
* Events should not take place during the hottest time of the day, avoid WBGT higher than | * Events should not take place during the hottest time of the day, avoid WBGT higher than 28°C<ref name=":1">Kenney WL, Wilmore JH, Costill DL. Exercise in Hot and Cold Environments. In Physiology of sport and exercise. Human kinetics; 2021 Oct 26.</ref> | ||
* Adequate supply of palatable fluids<ref name=":2" /> | * Adequate supply of palatable fluids<ref name=":2" /> | ||
* Customise fluid intake based on fluid losses (1 litre of sweat loss = 1-kilogram weight loss)<ref name=":1" /> | * Customise fluid intake based on fluid losses (1 litre of sweat loss = 1-kilogram weight loss)<ref name=":1" /> | ||
* | * Be aware of signs of heat illness<ref name=":1" /><ref name=":2" /> | ||
* Event organisers should have the final call on stopping events and prevent athletes with signs of heat illness | * Event organisers should have the final call on stopping events and prevent athletes with signs of heat illness from continued participation<ref name=":1" /> | ||
Read: [https://bjsm.bmj.com/content/bjsports/57/1/8.full.pdf IOC Consensus statement on recommendation and regulations for sport events in the heat]<ref name=":2">Racinais S, Hosokawa Y, Akama T, Bermon S, Bigard X, Casa DJ, Grundstein A, Jay O, Massey A, Migliorini S, Mountjoy M. IOC consensus statement on recommendations and regulations for sport events in the heat. British Journal of Sports Medicine. 2023 Jan 1;57(1):8-25.</ref> | Read: [https://bjsm.bmj.com/content/bjsports/57/1/8.full.pdf IOC Consensus statement on recommendation and regulations for sport events in the heat]<ref name=":2">Racinais S, Hosokawa Y, Akama T, Bermon S, Bigard X, Casa DJ, Grundstein A, Jay O, Massey A, Migliorini S, Mountjoy M. IOC consensus statement on recommendations and regulations for sport events in the heat. British Journal of Sports Medicine. 2023 Jan 1;57(1):8-25.</ref> | ||
== Heat Acclimation and Acclimatisation == | == Heat Acclimation and Acclimatisation == | ||
Repeated exercise in the heat facilitates changes that improve performance in hot conditions.<ref name=":3">Gibson OR, James CA, Mee JA, Willmott AG, Turner G, Hayes M, Maxwell NS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7053966/pdf/ktmp-07-01-1666624.pdf Heat alleviation strategies for athletic performance: a review and practitioner guidelines.] Temperature. 2020 Jan 2;7(1):3-6.</ref> This process is called heat acclimation (short-term 9 to 14 days) and acclimatisation (long-term months/years). The benefits of acclimation include<ref name=":3" />: | Repeated exercise in the heat facilitates changes that improve performance in hot conditions.<ref name=":3">Gibson OR, James CA, Mee JA, Willmott AG, Turner G, Hayes M, Maxwell NS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7053966/pdf/ktmp-07-01-1666624.pdf Heat alleviation strategies for athletic performance: a review and practitioner guidelines.] Temperature. 2020 Jan 2;7(1):3-6.</ref> This process is called heat acclimation (short-term 9 to 14 days) and [[Acclimatisation|acclimatisation]] (long-term months/years). The benefits of acclimation include<ref name=":3" />: | ||
* changes in sweating rate, sweat distribution and sweat content | * changes in sweating rate, sweat distribution and sweat content | ||
| Line 134: | Line 134: | ||
* initial increase in plasma volume, this returns to normal levels after about 10 days | * initial increase in plasma volume, this returns to normal levels after about 10 days | ||
* decrease in end-exercise heart rate and increase in cardiac output | * decrease in end-exercise heart rate and increase in cardiac output | ||
** this supports | ** this supports increased blood flow to the skin, which aids in greater heat loss and lowering of core temperature | ||
* widespread sweating earlier and sweat is more dilute | * widespread sweating earlier and sweat is more dilute | ||
** this prevents dangerous sodium loss and optimises evaporative heat loss | ** this prevents dangerous sodium loss and optimises evaporative heat loss | ||
Read: Exertional heat illness during training and competition | Read: [https://journals.lww.com/acsm-msse/Fulltext/2007/03000/Exertional_Heat_Illness_during_Training_and.20.aspx Exertional heat illness during training and competition]<ref>Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, Roberts WO. [https://journals.lww.com/acsm-msse/Fulltext/2007/03000/Exertional_Heat_Illness_during_Training_and.20.aspx Exertional heat illness during training and competition.] Medicine & Science in Sports & Exercise. 2007 Mar 1;39(3):556-72.</ref> and [[Heat Acclimation]] | ||
=== Recommendations for Athletes and Acclimation === | |||
* Athletes should acclimate before competing in hot environments<ref name=":2" /> | |||
* Preferred method for acclimation<ref name=":2" />: | |||
** train in a similar hot environment to the competition (if the athlete is unable to do this, other methods such as overdressed training, passive heat exposure that increase the core and skin temperature can be used) | |||
** optimal duration of heat training to acclimate is 60 to 90 minutes per day for at least 2 weeks (consider that shorter duration can still lead to positive acclimation changes) | |||
** optimal frequency of heat acclimation sessions: at least 4 sessions per week to induce heat acclimation and 2 sessions per week to maintain heat acclimation. | |||
== Exercise in the Cold == | == Exercise in the Cold == | ||
Cold stress is any environmental situation that causes a loss of body heat and threatens homeostasis. A decrease in the skin or core temperature provides the POAH with information to activate various mechanisms to conserve body heat and increase heat production. These measures are: | Cold stress is any environmental situation that causes a loss of body heat and threatens homeostasis. A decrease in the skin or core temperature provides the POAH with information to activate various mechanisms to conserve body heat and increase heat production. These measures are<ref name=":1" />: | ||
* peripheral vasoconstriction | * peripheral vasoconstriction | ||
| Line 161: | Line 167: | ||
* Body size and composition | * Body size and composition | ||
* Windchill | * Windchill | ||
** read more on windchill [[Cold-Related Injuries#Types|here]] | |||
=== Physiological Response to Exercise in the Cold === | === Physiological Response to Exercise in the Cold === | ||
* Muscle function decreases<ref name=":1" /> | * Muscle function decreases:<ref name=":1" /> | ||
** muscle fibre recruitment is altered and contractile forces are reduced | ** muscle fibre recruitment is altered and contractile forces are reduced | ||
** muscle shortening velocity and power decreases | ** muscle shortening velocity and power decreases | ||
** large deep muscles are not affected as much as superficial muscles | ** large deep muscles are not affected as much as superficial muscles | ||
* With an increase in fatigue there is also a decrease in metabolic heat production and during endurance exercise the depletion of the athlete's energy reserve may be a potential risk for hypothermia. | * With an increase in fatigue there is also a decrease in metabolic heat production and during endurance exercise, the depletion of the athlete's energy reserve may be a potential risk for hypothermia. | ||
=== Health Consequences | === Health Consequences of Cold === | ||
* Hypothermia<ref name=":1" /> | * [[Cold-Related Injuries#Hypothermia|Hypothermia]]<ref name=":1" /> | ||
** If the body's core temperature drops below 34. | ** If the body's core temperature drops below 34.5° C (94.1° F) the POAH loses its ability to regulate body temperature. At body temperatures of 29.5° C (85.1° F), the POAH has completely lost the ability to thermoregulate and metabolism slows and there is a loss of function that leads to drowsiness, lethargy and even coma. | ||
** Low core body temperature affects the sino-atrial node of the heart and decreases heart rate. | ** Low core body temperature affects the sino-atrial node of the heart and decreases heart rate. | ||
** Breathing cold air does not damage the ventilatory tissue, as inhaled air is progressively warmed as it moves through the respiratory tract. Extreme cold will reduce ventilation (decreased respiratory rate and volume). | ** Breathing cold air does not damage the ventilatory tissue, as inhaled air is progressively warmed as it moves through the respiratory tract. Extreme cold will reduce ventilation (decreased respiratory rate and volume). | ||
** Treatment for mild hypothermia | ** Treatment for mild hypothermia: | ||
*** | *** remove the individual from the cold | ||
*** | *** provide dry clothing, blankets and warm beverages | ||
** Treatment for severe hypothermia | ** Treatment for severe hypothermia | ||
*** | *** gentle handling to avoid cardiac arrhythmias | ||
*** | *** gradual rewarming, hospital facilities and medical care is necessary | ||
* | * [[Cold-Related Injuries#Frostnip|Frostbite]]<ref>Castellani JW, Eglin CM, Ikäheimo TM, Montgomery H, Paal P, Tipton MJ. ACSM expert consensus statement: injury prevention and exercise performance during cold-weather exercise. Current Sports Medicine Reports. 2021 Nov 1;20(11):594-607.</ref> | ||
* Read more: [[Cold-Related Injuries]] | * Read more: [[Cold-Related Injuries]] | ||
* Read more regarding sports performance: [[Cold Acclimation|Cold Acclimation and the Effect on Sport Performance]] | |||
* | |||
== References == | == References == | ||
Latest revision as of 19:54, 7 January 2024
Original Editor - Wanda van Niekerk based on the course by James Laskin
Top Contributors - Wanda van Niekerk, Kapil Narale, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Exercise in the heat or cold can influence the body's ability to regulate body temperature. Although these processes are effective and well-functioning in normal conditions, in extremely hot or cold conditions thermoregulation (regulation of body temperature around a physiological set point) can be inadequate. The human body is able to adapt to these environmental thermal conditions with continued exposure over time. Acclimation refers to the body's short-term adaptations (days/weeks) to these environmental stressors, whereas acclimatisation refers to long-term adaptations (months/ years) to environmental stressors.
Regulation of Body Temperature[edit | edit source]
- Humans are homeothermic - this means that the internal body temperature is physiologically regulated and kept nearly constant despite environmental temperature changes.[1]
- Fluctuations in body temperature are usually no more than 1.0° C (degrees Celsius) or 1.8° F (degrees Fahrenheit)
- Body temperature is a reflection of the balance between heat production and heat loss. If this balance is disturbed, there will be body temperature changes.[1]
- Normal baseline range of body temperature is 36.1° to 37.8 C (97.0° - 100.0° F)
- situations that will cause a change in normal baseline temperatures:
- fever due to illness
- extreme conditions of heat or cold
- prolonged heavy exercise
- situations that will cause a change in normal baseline temperatures:
Transfer of Heat between Body and Environment[edit | edit source]
- Metabolic heat is produced by active tissues[1]
- Heat moves from the body core (deep within the body) to the body shell (skin) via the blood
- When the heat reaches the skin it can be dissipated by conduction, convection, radiation and evaporation
- Maintaining a constant internal body temperature is dependent on the body's ability to balance heat gain (from metabolic processes and the environment) with heat loss. Figure 1. demonstrates this balance:
- heat gain: metabolic heat and environmental heat (conduction, convection, radiation)
- heat loss: radiation, conduction, convection, evaporation
- Conduction = heat transfer from one material to another through direct contact[1]
- example: sitting on cold or hot metal bleachers watching a sports event
- Convection = heat transfer by the movement of gas or liquid across a surface[1]
- during movement, such as playing sports, the air around us passes over our skin and heat is exchanged with air molecules
- greater movement of air results in greater heat exchange
- major daily thermoregulatory factor
- Radiation = heat transfer in the form of infrared rays[1]
- the body can give off or receive radiant heat
- major daily thermoregulatory factor
- Evaporation = heat loss via phase change from liquid to gas[1]
- primary way for heat loss during exercise
- as body core temperature increases, sweat production increases, sweat turns into vapour when it reaches the skin and cooling occurs
- sweat must evaporate to have a cooling effect, dripping sweat provides little or no cooling effect
Challenges with the Transfer of Body Heat[edit | edit source]
- Humidity and heat loss[2]
- high humidity limits the evaporation of sweat as the air contains many H2O molecules
- low humidity provides an ideal opportunity for evaporation
- Prolonged sweat evaporation without adequate fluid intake can cause dehydration
- Temperature of the skin is greater than the temperature of the environment = heat loss through conduction, convection and radiation and evaporation
- Temperature of the environment is greater than skin temperature = heat can only be removed through evaporation
- In hot humid situations, evaporation of sweat is limited and convection occurs from the environment to the skin (thus heat is gained)
Thermoregulatory Control[edit | edit source]
The body's thermoregulatory responses are very effective for normal ranges of body and air temperature. Core body temperature at rest is regulated at approximately 37° C (98.6° F). If the internal (core) body temperature exceeds 40° C (104°F), physiological function will be inhibited. Humans are able to briefly withstand core temperatures below 35° C (95° F) or above 41° C (105.8° F) .
- Body's thermoregulatory centre - preoptic anterior hypothalamus (POAH)[3]
- acts as a thermostat - monitors temperature and accelerates heat loss or heat generation when necessary
- Sensory thermoreceptors provide information to POAH
- skin - peripheral thermoreceptors
- brain and spinal cord - central thermoreceptors
- central thermoreceptors are more sensitive to temperature changes than peripheral thermoreceptors
- When POAH senses deviation in body temperature (below or above normal), it sends signals through the sympathetic nervous system to the following thermoregulatory effectors[3]:
- skin arterioles
- POAH sends a signal via the sympathetic nervous system to smooth muscle in arteriole walls resulting in either vasodilation or vasoconstriction
- vasoconstriction to minimise heat loss
- vasodilation to enhance heat loss
- POAH sends a signal via the sympathetic nervous system to smooth muscle in arteriole walls resulting in either vasodilation or vasoconstriction
- eccrine sweat glands
- sufficient rise in core and skin temperature - POAH sends a signal via the sympathetic nervous system to eccrine sweat glands, leading to active secretion of sweat. Read more on the Physiology of Sweat
- endocrine glands
- the effect of various hormones results in an increased cellular metabolic rate, and increased metabolism leads to an increase in heat production
- skeletal muscle
- increased skeletal muscle activity increases body temperature by increasing metabolic heat production
- muscle actions can be voluntary or involuntary (for example when a person is shivering because of being cold)
- skin arterioles
Physiological Responses to Exercise in the Heat[edit | edit source]
Cardiovascular Response[edit | edit source]
Independent of the environment, exercise increases heat load due to muscle work and increased metabolism. The POAH sends signals via the sympathetic nervous system to the skin arterioles to vasodilate, which increases conductive and evaporative heat loss. Vasoconstriction occurs to direct blood from non-essential tissue such as the gut, liver and kidneys. Cardiac output further increases via an increase in heart rate and changes in contractility to maintain the cardiac output to working muscle. Due to sweating, blood volume decreases and the ability to increase stroke volume is also limited due to peripheral blood pooling. Heart rate increases to compensate for the decrease in stroke volume (a phenomenon known as cardiovascular drift).[4]
Fluid Balance[edit | edit source]
Hot environmental temperatures and strenuous physical activity increase skin and core temperatures. The POAH controls the sweat glands. Sweat forms in the coiled section of the sweat gland and initially the electrolyte composition is the same as that of blood as plasma is the source of sweat formation. The filtrate of plasma moves through the duct of the sweat gland and sodium and chloride are reabsorbed back into the tissue and then into the blood. Thus, the sweat that is released onto the skin has fewer electrolytes than plasma.[4]
- Light sweating - filtrate travels slowly through the duct, so there is more time for reabsorption of sodium and chloride and sweat is very diluted
- Heavy sweating - there is less time for reabsorption of sodium and chloride as filtrate moves more quickly through the sweat duct, so the sodium and chloride content of sweat is higher
There is a difference in the electrolyte concentration of sweat in trained versus untrained individuals. With training and heat acclimation, more sodium and chloride are reabsorbed and sweat is more dilute. Concentrations of potassium, calcium and magnesium stay more or less the same. Exercise in hot and humid conditions can result in a loss of 2.5 % to 3.2 % of body weight through sweat. High rates of sweating reduce blood volume. This leads to an increased heart rate and eventually leads to a decrease in cardiac output and this affects athletic performance.[4]
Read this article: Exercise and Fluid Replacement[5]
Health Risks with Exercise in the Heat[edit | edit source]
Factors that need to be considered as stressors when exercising in the heat include[4]:
- metabolic heat production
- air temperature
- humidity
- air velocity
- radiant heat sources
- clothing[6]
- athletes and officials with low metabolic heat production: wear light-coloured, loose-fitting, sun-protective clothing
- athletes with high metabolic heat production: clothing should not impair direct sweat evaporation from the skin
- Read: The role of sports clothing in thermoregulation, comfort, and performance during exercise in the heat: a narrative review[7]
Thermal Stress[edit | edit source]
External heat stress can be measured with:
- heat index
- wet-bulb globe temperature (WBGT)[8]
Health Consequences of Heat[edit | edit source]
Exposure to heat stress from the environment and metabolically generated heat can cause[9]:
- heat cramps
- heat exhaustion
- heatstroke
Read more about Heat Illness in Sports
Guidelines for Practising and Competing in Heat[edit | edit source]
- Events should not take place during the hottest time of the day, avoid WBGT higher than 28°C[4]
- Adequate supply of palatable fluids[6]
- Customise fluid intake based on fluid losses (1 litre of sweat loss = 1-kilogram weight loss)[4]
- Be aware of signs of heat illness[4][6]
- Event organisers should have the final call on stopping events and prevent athletes with signs of heat illness from continued participation[4]
Read: IOC Consensus statement on recommendation and regulations for sport events in the heat[6]
Heat Acclimation and Acclimatisation[edit | edit source]
Repeated exercise in the heat facilitates changes that improve performance in hot conditions.[10] This process is called heat acclimation (short-term 9 to 14 days) and acclimatisation (long-term months/years). The benefits of acclimation include[10]:
- changes in sweating rate, sweat distribution and sweat content
- cardiovascular function is optimised
- lower core temperature during exercise
- initial increase in plasma volume, this returns to normal levels after about 10 days
- decrease in end-exercise heart rate and increase in cardiac output
- this supports increased blood flow to the skin, which aids in greater heat loss and lowering of core temperature
- widespread sweating earlier and sweat is more dilute
- this prevents dangerous sodium loss and optimises evaporative heat loss
Read: Exertional heat illness during training and competition[11] and Heat Acclimation
Recommendations for Athletes and Acclimation[edit | edit source]
- Athletes should acclimate before competing in hot environments[6]
- Preferred method for acclimation[6]:
- train in a similar hot environment to the competition (if the athlete is unable to do this, other methods such as overdressed training, passive heat exposure that increase the core and skin temperature can be used)
- optimal duration of heat training to acclimate is 60 to 90 minutes per day for at least 2 weeks (consider that shorter duration can still lead to positive acclimation changes)
- optimal frequency of heat acclimation sessions: at least 4 sessions per week to induce heat acclimation and 2 sessions per week to maintain heat acclimation.
Exercise in the Cold[edit | edit source]
Cold stress is any environmental situation that causes a loss of body heat and threatens homeostasis. A decrease in the skin or core temperature provides the POAH with information to activate various mechanisms to conserve body heat and increase heat production. These measures are[4]:
- peripheral vasoconstriction
- non-shivering thermogenesis
- skeletal muscle shivering
- behavioural responses such as putting on more clothes
Cold Habituation[edit | edit source]
- Cold habituation occurs with regular exposure to repeated cold environments without significant heat loss. This is seen in vasoconstriction and shivering being blunted and the core temperatures dropping further than before the chronic exposure to cold.[12]
- Metabolic acclimation occurs after repeated cold exposures with heat loss and enhanced metabolic and shivering heat production develop.[12]
- Insulative acclimation occurs when an increase in metabolism cannot prevent heat loss. In this scenario, enhanced skin vasoconstriction occurs and this increases peripheral tissue insulation and reduces heat loss.[12]
Factors Affecting Body Heat Loss[edit | edit source]
- Body size and composition
- Windchill
- read more on windchill here
Physiological Response to Exercise in the Cold[edit | edit source]
- Muscle function decreases:[4]
- muscle fibre recruitment is altered and contractile forces are reduced
- muscle shortening velocity and power decreases
- large deep muscles are not affected as much as superficial muscles
- With an increase in fatigue there is also a decrease in metabolic heat production and during endurance exercise, the depletion of the athlete's energy reserve may be a potential risk for hypothermia.
Health Consequences of Cold[edit | edit source]
- Hypothermia[4]
- If the body's core temperature drops below 34.5° C (94.1° F) the POAH loses its ability to regulate body temperature. At body temperatures of 29.5° C (85.1° F), the POAH has completely lost the ability to thermoregulate and metabolism slows and there is a loss of function that leads to drowsiness, lethargy and even coma.
- Low core body temperature affects the sino-atrial node of the heart and decreases heart rate.
- Breathing cold air does not damage the ventilatory tissue, as inhaled air is progressively warmed as it moves through the respiratory tract. Extreme cold will reduce ventilation (decreased respiratory rate and volume).
- Treatment for mild hypothermia:
- remove the individual from the cold
- provide dry clothing, blankets and warm beverages
- Treatment for severe hypothermia
- gentle handling to avoid cardiac arrhythmias
- gradual rewarming, hospital facilities and medical care is necessary
- Frostbite[13]
- Read more: Cold-Related Injuries
- Read more regarding sports performance: Cold Acclimation and the Effect on Sport Performance
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Cramer MN, Gagnon D, Laitano O, Crandall CG. Human temperature regulation under heat stress in health, disease, and injury. Physiological reviews. 2022 Oct 1;102(4):1907-89.
- ↑ Griggs KE, Stephenson BT, Price MJ, Goosey-Tolfrey VL. Heat-related issues and practical applications for Paralympic athletes at Tokyo 2020. Temperature. 2020 Jan 2;7(1):37-57.
- ↑ 3.0 3.1 Xu X, Rioux TP, Castellani MP. Three dimensional models of human thermoregulation: A review. Journal of Thermal Biology. 2023 Feb 4:103491.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 Kenney WL, Wilmore JH, Costill DL. Exercise in Hot and Cold Environments. In Physiology of sport and exercise. Human kinetics; 2021 Oct 26.
- ↑ Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, Stachenfeld NS, American College of Sports Medicine. American College of Sports Medicine position stand. Exercise and fluid replacement. Medicine and science in sports and exercise. 2007 Feb;39(2):377-90.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Racinais S, Hosokawa Y, Akama T, Bermon S, Bigard X, Casa DJ, Grundstein A, Jay O, Massey A, Migliorini S, Mountjoy M. IOC consensus statement on recommendations and regulations for sport events in the heat. British Journal of Sports Medicine. 2023 Jan 1;57(1):8-25.
- ↑ Di Domenico I, Hoffmann SM, Collins PK. The Role of Sports Clothing in Thermoregulation, Comfort, and Performance During Exercise in the Heat: A Narrative Review. Sports Medicine-Open. 2022 Dec;8(1):58.
- ↑ Hosokawa Y, Adams WM, Casa DJ, Vanos JK, Cooper ER, Grundstein AJ, Jay O, McDermott BP, Otani H, Raukar NP, Stearns RL. Roundtable on preseason heat safety in secondary school athletics: environmental monitoring during activities in the heat. Journal of athletic training. 2021 Apr 1;56(4):362-71.
- ↑ Nowak AS, Kennelley GE, Krabak BJ, Roberts WO, Tenforde KM, Tenforde AS. Endurance athletes and climate change. The Journal of Climate Change and Health. 2022 Feb 1:100118.
- ↑ 10.0 10.1 Gibson OR, James CA, Mee JA, Willmott AG, Turner G, Hayes M, Maxwell NS. Heat alleviation strategies for athletic performance: a review and practitioner guidelines. Temperature. 2020 Jan 2;7(1):3-6.
- ↑ Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, Roberts WO. Exertional heat illness during training and competition. Medicine & Science in Sports & Exercise. 2007 Mar 1;39(3):556-72.
- ↑ 12.0 12.1 12.2 Yurkevicius BR, Alba BK, Seeley AD, Castellani JW. Human cold habituation: Physiology, timeline, and modifiers. Temperature. 2022 Apr 3;9(2):122-57.
- ↑ Castellani JW, Eglin CM, Ikäheimo TM, Montgomery H, Paal P, Tipton MJ. ACSM expert consensus statement: injury prevention and exercise performance during cold-weather exercise. Current Sports Medicine Reports. 2021 Nov 1;20(11):594-607.