Amyotrophic Lateral Sclerosis: Difference between revisions
No edit summary |
(updated prevalences, symptoms, and references) |
||
| (9 intermediate revisions by 2 users not shown) | |||
| Line 8: | Line 8: | ||
== Introduction == | == Introduction == | ||
[[File:Physicist Stephen Hawking in Zero Gravity NASA.jpg|right|frameless|350x350px]] | [[File:Physicist Stephen Hawking in Zero Gravity NASA.jpg|right|frameless|350x350px]] | ||
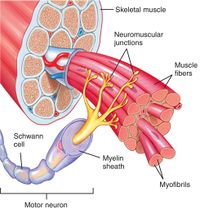
Amyotrophic lateral sclerosis (ALS) is a fatal [[:Category:Neurology|neurological disorder]] with an adult-onset around 54–67 years old, and it belongs to a group of conditions known as [[Motor Neurone Disease MND|Motor Neurone Diseases]] (MND). Its clinical hallmark is the degeneration of both upper and lower motor neurons, leading to progressive muscle atrophy and weakness, and ultimately to paralysis. Death, often resulting from swallowing problems and [[Respiratory Failure|respiratory failure]], usually occurs within 2–4 years from disease onset, although 5–10% of ALS patients survive over 10 years<ref name=":2">Vijayakumar UG, Milla V, Stafford C, Bjourson T, Duddy WJ, Duguez SR. [https://www.frontiersin.org/articles/10.3389/fneur.2019.00400/full A systematic review of suggested molecular strata, biomarkers and their tissue sources in ALS.] Frontiers in neurology. 2019;10:400. Available from: https://www.frontiersin.org/articles/10.3389/fneur.2019.00400/full (last accessed 14.12.2019)</ref>. | Amyotrophic lateral sclerosis (ALS), also know as Lou Gehrig's disease, is a fatal [[:Category:Neurology|neurological disorder]] with an adult-onset around 54–67 years old, and it belongs to a group of conditions known as [[Motor Neurone Disease MND|Motor Neurone Diseases]] (MND). Its clinical hallmark is the degeneration of both upper and lower motor neurons, leading to progressive muscle atrophy and weakness, and ultimately to paralysis. Death, often resulting from swallowing problems and [[Respiratory Failure|respiratory failure]], usually occurs within 2–4 years from disease onset, although 5–10% of ALS patients survive over 10 years<ref name=":2">Vijayakumar UG, Milla V, Stafford C, Bjourson T, Duddy WJ, Duguez SR. [https://www.frontiersin.org/articles/10.3389/fneur.2019.00400/full A systematic review of suggested molecular strata, biomarkers and their tissue sources in ALS.] Frontiers in neurology. 2019;10:400. Available from: https://www.frontiersin.org/articles/10.3389/fneur.2019.00400/full (last accessed 14.12.2019)</ref>. | ||
Image - Noted physicist Stephen Hawking [who suffered from ALS] enjoys zero gravity during a flight aboard a modified Boeing 727 aircraft owned by Zero Gravity Corp. | Image - Noted physicist Stephen Hawking [who suffered from ALS] enjoys zero gravity during a flight aboard a modified Boeing 727 aircraft owned by Zero Gravity Corp. | ||
| Line 14: | Line 14: | ||
Physical therapy is an integral component of the ALS [[Multidisciplinary Care in Pain Management|multidisciplinary]] team and is well-grounded in rehabilitation and active living concepts. Despite the lack of a cure and rapidly progressive nature of the disease, physical therapy that is tailored to the individual’s needs and goals enables the client to live life to the fullest and with quality<ref name=":3">Dal Bello-Haas V. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6065609/ Physical therapy for individuals with amyotrophic lateral sclerosis: current insights.] Degenerative neurological and neuromuscular disease. 2018;8:45. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6065609/ (last accessed 14.12.2019)</ref>. | Physical therapy is an integral component of the ALS [[Multidisciplinary Care in Pain Management|multidisciplinary]] team and is well-grounded in rehabilitation and active living concepts. Despite the lack of a cure and rapidly progressive nature of the disease, physical therapy that is tailored to the individual’s needs and goals enables the client to live life to the fullest and with quality<ref name=":3">Dal Bello-Haas V. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6065609/ Physical therapy for individuals with amyotrophic lateral sclerosis: current insights.] Degenerative neurological and neuromuscular disease. 2018;8:45. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6065609/ (last accessed 14.12.2019)</ref>. | ||
The incidence and prevalence increase with age and reaches a cumulative lifetime risk of 1 in 400 after 80 years old. Due to the projected | The incidence and prevalence increase with age and reaches a cumulative lifetime risk of 1 in 400 after 80 years old. Due to the projected ageing of the global population, ALS cases are expected to increase by 69% in the next 25 years, and there is a need to identify causes, biomarkers and therapeutic targets for ALS<ref name=":2" />. | ||
Descriptions of the disease date back to at least 1824. In 1869, the connection between the symptoms and the underlying neurological problems (involvement of the cortico-spinal tract) | Descriptions of the disease date back to at least 1824. In 1869, the connection between the symptoms and the underlying neurological problems (involvement of the cortico-spinal tract) was first described by Jean-Martin Charcot. In 1874 Charcot began using the term amyotrophic lateral sclerosis (ALS). The disease became widely publicised in the United States when it affected the famous baseball player Lou Gehrig, and later when the ice bucket challenge became popular in 2014. | ||
The 2-minute video below gives a good introduction to ALS. | The 2-minute video below gives a good introduction to ALS. | ||
{{#ev:youtube|https://www.youtube.com/watch?v=kOnk9Hh20eg&app=desktop|width}}<ref>Neuroscientifically Challenged ALS Available from: https://www.youtube.com/watch?v=kOnk9Hh20eg&app=desktop (last accessed 14.12.2019)</ref> | {{#ev:youtube|https://www.youtube.com/watch?v=kOnk9Hh20eg&app=desktop|width}}<ref>Neuroscientifically Challenged ALS Available from: https://www.youtube.com/watch?v=kOnk9Hh20eg&app=desktop (last accessed 14.12.2019)</ref> | ||
== Background Epidemiology | == Background Epidemiology and Prognosis == | ||
ALS is the most common form of | ALS is the most common form of motor neuron disease in adults<ref name="Marsden">Marsden, R. Motor neurone disease: an overview. Primary Health Care 2011; 21;10;31-36 (Accessed 18th May 2015)</ref><ref name=":0">Talbott EO, Malek AM, Lacomis D. The epidemiology of amyotrophic lateral sclerosis. In Handbook of clinical neurology 2016 Jan 1 (Vol. 138, pp. 225-238). Elsevier.</ref> The incidence of ALS is approximately 1-2.6 cases per 100 000 persons annually, with a prevalence of approximately 6 cases per 100 000<ref name="National">National Institute of Neurological Disorders and Stroke. . Amyotrophic Lateral Sclerosis (ALS) Fact Sheet, [https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Amyotrophic-Lateral-Sclerosis-ALS-Fact-Sheet NINDS, Publication date June 2013.NIH Publication No. 16-916] (Accessed 23rd April 2019)</ref><ref name=":0" />. In the UK ALS affects around two in every 100,000 people each year and at any one time, there are about 5,000 people living with the condition.<ref name="NHS">NHS Information http://www.nhs.uk/Conditions/Motor-neurone-disease/Pages/Symptoms.aspx (accessed April 28th at 11:49)</ref> | ||
* For about half of those with the condition the mean life expectancy from the onset of symptoms to death is 2-4 yrs | * For about half of those with the condition the mean life expectancy from the onset of symptoms to death is 2-4 yrs | ||
* Only 20% live beyond 5yrs | * Only 20% live beyond 5yrs | ||
| Line 27: | Line 27: | ||
* Incidence peaks between 55 and 65 years of age | * Incidence peaks between 55 and 65 years of age | ||
* Clinicians are reporting that they are seeing increasing numbers of younger ALS patients. | * Clinicians are reporting that they are seeing increasing numbers of younger ALS patients. | ||
* | * Prognostic indicators<ref name=":4">O’Sullivan SB, Schmitz TJ, Fulk G. Physical rehabilitation. F.A. Davis; 2019. p712-752.</ref> | ||
** Younger patients (less than 35-<u></u>40 years old) have better 5<u></u>-year survival rates | |||
** Individuals with limb symptoms at onset versus bulbar sign<u></u>s have improved 5-year survival rates (37 to 44% versus 9 to 16%) | |||
** Individuals with better psychological well-being and suppo<u></u>rt at onset have longer survival rates | |||
* Disease course varies from several months to 20 years | |||
** <u></u>Average duration of 27 to 43 months | |||
** Five-year survival<u></u> rates from 9% to 40% | |||
** Ten-year survi<u></u>val rate from 8% to 16% | |||
== Aetiology == | |||
The causes of ALS essentially unknown but several factors are thought to be involved including environmental risk factors,<ref name=":1">Martin S, Al Khleifat A, Al-Chalabi A. What causes amyotrophic lateral sclerosis?. F1000Research. 2017;6.</ref> Gene mutations have also been identified in some cases of ALS<ref name="National" /><ref name=":1" / | The <u></u>causes of ALS essentially unknown but several factors are thought to be involved including environmental risk factors,<ref name=":1">Martin S, Al Khleifat A, Al-Chalabi A. What causes amyotrophic lateral sclerosis?. F1000Research. 2017;6.</ref> Gene mutations have also been identified in some cases of ALS<ref name="National" /><ref name=":1" /> | ||
*Genetic – this is not true for all cases but some mutations have been identified in some individuals. In these cases, it is not uncommon to have several cases in one family.<ref name="NHS" /><ref name="Kiernan">Kiernan, M.C., Vucic, S., Cheah, B.C., Turner, M.R., Eisen, A., Hardiman, O., Burrell, J.R., Zoing, M.C. Amyotrophic lateral sclerosis. Lancet 2011; 377; 942-55 http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2810%2961156-7/abstract (accessed 4th May 2015)</ref> | *Genetic – this is not true for all cases but some mutations have been identified in some individuals. In these cases, it is not uncommon to have several cases in one family.<ref name="NHS" /><ref name="Kiernan">Kiernan, M.C., Vucic, S., Cheah, B.C., Turner, M.R., Eisen, A., Hardiman, O., Burrell, J.R., Zoing, M.C. Amyotrophic lateral sclerosis. Lancet 2011; 377; 942-55 http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2810%2961156-7/abstract (accessed 4th May 2015)</ref> | ||
*Biochemistry – it appears that MND mainly occurs through the activation of calcium- | *Biochemistry – it appears that MND mainly occurs through the activation of calcium-dependent enzymatic pathways. | ||
*Premature ageing of some motor cells may lead to damage and destruction if these cells. This then puts pressure on the surviving cells | *Premature ageing of some motor cells may lead to damage and destruction if these cells. This then puts pressure on the surviving cells | ||
*Sporadic MND | *Sporadic MND | ||
** Sporadic ALS (90-95%) constitutes the large majority of cases<ref name=":0" /> | ** Sporadic ALS (90-95%) constitutes the large majority of cases<ref name=":0" /> | ||
| Line 41: | Line 48: | ||
** Family history of either motor neurone disease or a related condition called frontotemporal dementia.<ref name="NHS" /> | ** Family history of either motor neurone disease or a related condition called frontotemporal dementia.<ref name="NHS" /> | ||
** Autosomal dominant | ** Autosomal dominant | ||
** Mean age-onset 47 years of age | ** Mean age-onset 47 years of age | ||
** Represents 5-10% of all ALS occurrences<ref name=":0" /> | ** Represents 5-10% of all ALS occurrences<ref name=":0" /> | ||
| Line 49: | Line 55: | ||
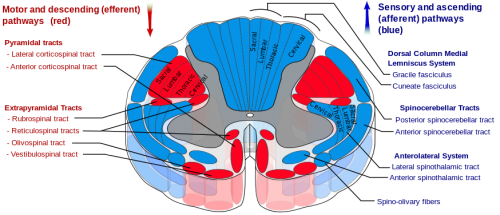
[[Image:Spinal cord cross section.png|right|500px]] | [[Image:Spinal cord cross section.png|right|500px]] | ||
In the progression of the disease, there is a loss of motor neurones from the anterior horn of the [[Spinal cord anatomy|spinal cord]], the primary [[Brain Anatomy|motor cortex]] and from the hypoglossal nucleus in the lower medulla | In the progression of the disease, there is a loss of motor neurones from the anterior horn of the [[Spinal cord anatomy|spinal cord]], the primary [[Brain Anatomy|motor cortex]] and from the hypoglossal nucleus in the lower medulla. Shrinkage and discolouration of the anterior nerve roots in the spinal cord occur because of axonal degeneration of the neurones and the accompanying demyelination.<ref>Jeans, A.F., Ansorge, O. Recent developments in the pathology of Motor Neurone Disease. Advances in Clinical Neuroscience and Rehabilitation; Neuropathology Article 2009; 9; 4; 25-26 http://www.acnr.co.uk/SO09/ACNRSO09_web.pdf (Accessed 4th May 2015)</ref> | ||
The pathophysiology behind the disease appears to be multi-factorial with complex interactions between genetics and molecular pathways.<ref name="Kiernan" /> <br>Potential cellular & molecular mechanisms that contribute to the neurodegeneration of MND:<ref name="Kiernan" /> | The pathophysiology behind the disease appears to be multi-factorial with complex interactions between genetics and molecular pathways.<ref name="Kiernan" /> <br>Potential cellular & molecular mechanisms that contribute to the neurodegeneration of MND:<ref name="Kiernan" /><ref>Mohamed LA, Markandaiah SS, Bonanno S, Pasinelli P, Trotti D. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6506236/ Excess glutamate secreted from astrocytes drives upregulation of P-glycoprotein in endothelial cells in amyotrophic lateral sclerosis.] Exp Neurol [Internet]. 2019;316:27–38</ref> | ||
* Abnormal mitochondria functioning | * Abnormal mitochondria functioning | ||
* Increased oxidative stress | * Increased oxidative stress | ||
| Line 58: | Line 64: | ||
* Sodium-potassium pump dysfunction | * Sodium-potassium pump dysfunction | ||
* Increased inflammatory mediators | * Increased inflammatory mediators | ||
* Increased toxin secretion <br> | * Increased toxin secretion | ||
* Protein mutation affecting RNA metabolism | |||
* Glutamate excitotoxicity - 2x greater than normal plasma levels<br> | |||
Potential gene mutations that are harmful to neurons and could contribute to the disease:<ref name="Kiernan" /> | Potential gene mutations that are harmful to neurons and could contribute to the disease:<ref name="Kiernan" /> | ||
* TARDBP | * TARDBP | ||
* FUS | * FUS | ||
Irrespective of the direct pathways, as the disease progresses there is a demyelinating process which occurs in all areas of the spinal cord except the posterior columns. '''reference''' | |||
== Clinical Manifestations == | == Clinical Manifestations == | ||
| Line 67: | Line 76: | ||
=== Initial Symptoms === | === Initial Symptoms === | ||
Symptoms may vary depending on | Symptoms may vary depending on where it first manifests. However, it presents with a combination of upper and lower motor neuron signs. | ||
Lower motor neuron signs: | |||
* Asymmetric weakness of distal limbs progressing proximally - often first sign | |||
* UE extensors weaker than flexors (especially in hands, also leads to head droop and increased lumbar lordosis | |||
* Bulbar Signs: facial muscle weakness, dysarthria, dysphagia, tongue fasciculations, drooling<ref name=":4" /> | |||
Upper motor neuron signs: | |||
* Spasticity | |||
* Lack of dexterity | |||
* Loss of strength | |||
* Pseudobulbar Affect | |||
* Hyperreflexia | |||
* Positive pathological reflexes (Babinski, Hoffman's sign) | |||
* Clonus<ref name=":4" /> | |||
Typically, the oculomotor nerves are spared in addition to the posterior columns of the spinal cord, which means that eye movements, sensation, bowel and bladder function remain intact. | |||
==== Limb-Onset Disease ==== | ==== Limb-Onset Disease ==== | ||
| Line 75: | Line 102: | ||
*Widespread twitching of the muscles (fasciculations) | *Widespread twitching of the muscles (fasciculations) | ||
*Muscle cramps | *Muscle cramps | ||
*Visible wasting of the muscles with significant weight loss | *Visible wasting of the muscles with significant weight loss | ||
==== Respiratory-Onset Disease ==== | ==== Respiratory-Onset Disease ==== | ||
| Line 102: | Line 125: | ||
*Increasing body paralysis | *Increasing body paralysis | ||
*Significant shortness of breath | *Significant shortness of breath | ||
*Astrocytic Gliosis - cortical involvement seen in later stages of the disease, affecting 50% of individuals resulting in deficits in executive functions, attention, and language comprehension<ref name=":4" /><ref>Goodman CC & Fuller KS. Pathology: Implications for the Physical Therapist. 5th ed. Philadelphia, PA: Saunders; 2021. p1408-1417.</ref> | |||
=== Secondary Symptoms === | === Secondary Symptoms === | ||
| Line 110: | Line 134: | ||
== Diagnosis == | == Diagnosis == | ||
There is no single test that diagnoses an individual with ALS<ref name="Factsheet" />. However, several characteristics of the disease can be identified and therefore used to point practitioners in the right direction. El Escorial Criteria mentions the specific characteristics and features that need to be displayed in an individual for a proper ALS diagnosis; although they are not exclusive. It classifies diagnosis into four different categories depending on severity of upper (UMN) as well as lower motor neuron (LMN) degeneration (which must not be explained by the presence | There is no single test that diagnoses an individual with ALS<ref name="Factsheet" />. However, several characteristics of the disease can be identified and therefore used to point practitioners in the right direction. El Escorial Criteria mentions the specific characteristics and features that need to be displayed in an individual for a proper ALS diagnosis; although they are not exclusive. It classifies diagnosis into four different categories depending on the severity of upper (UMN) as well as lower motor neuron (LMN) degeneration (which must not be explained by the presence of her neurological disorder). Physicians use a combination of a few methods such as electromyography and neuroimaging to identify UMN and LMN degeneration which is the most prominent feature in neurodegenerative disorders. Furthermore, current research is looking into whole-brain magnetic resonance spectroscopic imaging (MRSI) as a source of determining disability levels in ALS in the future.<br> | ||
*With the exception of one genetic test, no definitive diagnostic test or biological marker exists for ALS – however, not all individuals with the disease present with this gene | *With the exception of one genetic test, no definitive diagnostic test or biological marker exists for ALS – however, not all individuals with the disease present with this gene | ||
| Line 133: | Line 157: | ||
=== Physiotherapy === | === Physiotherapy === | ||
Because of the variable clinical presentation of people with ALS [PALS], the great variability in prognosis, and the typically rapid, progressive, and deteriorating nature of ALS, we as physical therapists are constantly challenged when developing the most appropriate intervention plan for PALS. The physical therapist needs an understanding of the nature and course of the disease | Because of the variable clinical presentation of people with ALS [PALS], the great variability in prognosis, and the typically rapid, progressive, and deteriorating nature of ALS, we as physical therapists are constantly challenged when developing the most appropriate intervention plan for PALS. The physical therapist needs an understanding of the nature and course of the disease and needs to consider future problems in addition to current status. In order to make appropriate and effective decisions, the nature and significance of the activity limitations, and participation restrictions need to be determined. Decision-making involves determining which impairments, activity limitations, and participation restrictions: | ||
# Can be restored | # Can be restored | ||
# Require compensatory strategies or interventions | # Require compensatory strategies or interventions | ||
# Require referral to different health care professional(s) and | # Require referral to a different health care professional(s) and | ||
# Cannot be affected by physical therapy interventions at all.<ref name=":3" /> | # Cannot be affected by physical therapy interventions at all.<ref name=":3" /> | ||
Many of the problematic symptoms of ALS can be addressed by appropriate physical therapy interventions<ref name=":3" /> | Many of the problematic symptoms of ALS can be addressed by appropriate physical therapy interventions<ref name=":3" /> | ||
| Line 145: | Line 169: | ||
[[Exercise Therapy in the Rehabilitation of Spondylolisthesis in Fast Bowlers in Cricket|Exercise]]<nowiki/>s should focus on improving posture, preventing [[Joint Classification|joint]] immobility, and slowing the progressive muscle weakening and atrophy. [[Stretching]] and [[Strength and Conditioning|strengthening]] exercises may help reduce [[spasticity]], increase range of motion and improve circulation. | [[Exercise Therapy in the Rehabilitation of Spondylolisthesis in Fast Bowlers in Cricket|Exercise]]<nowiki/>s should focus on improving posture, preventing [[Joint Classification|joint]] immobility, and slowing the progressive muscle weakening and atrophy. [[Stretching]] and [[Strength and Conditioning|strengthening]] exercises may help reduce [[spasticity]], increase range of motion and improve circulation. | ||
The video below gives an example of a simple home exercise plan. | The video below gives an example of a simple home exercise plan. | ||
Physical therapy can enhance an individual’s independence throughout the course of the disease. Gentle, low-impact aerobic exercise such as walking, swimming, and stationary bicycling can strengthen unaffected muscles, improve cardiovascular health, and aid people fight fatigue and depression, contractures of muscles. | |||
{{#ev:youtube|https://www.youtube.com/watch?v=IKxnWbclFic&app=desktop|width}}<ref>ALS hope foundation ALS exercises Available from: https://www.youtube.com/watch?v=IKxnWbclFic&app=desktop (last accessed 14.12.2019)</ref> | {{#ev:youtube|https://www.youtube.com/watch?v=IKxnWbclFic&app=desktop|width}}<ref>ALS hope foundation ALS exercises Available from: https://www.youtube.com/watch?v=IKxnWbclFic&app=desktop (last accessed 14.12.2019)</ref> | ||
| Line 169: | Line 195: | ||
Research options fall largely into three categories: drugs, gene therapy, and stem cells.<ref name="Kiernan" /> | Research options fall largely into three categories: drugs, gene therapy, and stem cells.<ref name="Kiernan" /> | ||
Although evidence from a review in 2019<ref>Tsitkanou S, Della Gatta PA, Foletta VC, Russell AP. [https://www.frontiersin.org/articles/10.3389/fneur.2019.00783/full The role of exercise as a non-pharmacological therapeutic approach for Amyotrophic Lateral Sclerosis: beneficial or detrimental?.] Frontiers in neurology. 2019;10:783. Avaiable from: https://www.frontiersin.org/articles/10.3389/fneur.2019.00783/full (last accessed 15.2.2019)</ref> supports the advantageous impact of exercise in ALS, it is still not clear whether physical activity should be recommended as a treatment option for ALS patients. Even if exercise training per se is not a sufficient intervention to decelerate disease progression or improve patients' survival, it could be an adjunct therapy to other pharmacological treatments of ALS. Considering the lack of treatments at this time in ALS, non-pharma therapeutics, such as physical activity, is likely to be more important than previously appreciated.<br>Clinical trials are testing whether different drugs or interventions are safe and effective in slowing the progression of | Although evidence from a review in 2019<ref>Tsitkanou S, Della Gatta PA, Foletta VC, Russell AP. [https://www.frontiersin.org/articles/10.3389/fneur.2019.00783/full The role of exercise as a non-pharmacological therapeutic approach for Amyotrophic Lateral Sclerosis: beneficial or detrimental?.] Frontiers in neurology. 2019;10:783. Avaiable from: https://www.frontiersin.org/articles/10.3389/fneur.2019.00783/full (last accessed 15.2.2019)</ref> supports the advantageous impact of exercise in ALS, it is still not clear whether physical activity should be recommended as a treatment option for ALS patients. Even if exercise training per se is not a sufficient intervention to decelerate disease progression or improve patients' survival, it could be an adjunct therapy to other pharmacological treatments of ALS. Considering the lack of treatments at this time in ALS, non-pharma therapeutics, such as physical activity, is likely to be more important than previously appreciated.<br>Clinical trials are testing whether different drugs or interventions are safe and effective in slowing the progression of ALS in patient volunteers. <br>Cellular and molecular studies seek to understand the mechanisms that trigger motor neurons to degenerate.<ref name="National" /> | ||
== Presentations == | == Presentations == | ||
<div class="coursebox"> | <div class="coursebox"> | ||
Latest revision as of 06:09, 1 January 2024
Original Editor - Norma Cervera Top Contributors - Laura Ritchie, Lucinda hampton, Kim Jackson, Nikhil Benhur Abburi, Leah Milligan, Evan Thomas, Garima Gedamkar, WikiSysop, Mason Trauger, Admin, Naomi O'Reilly and Norma Cervera
Introduction[edit | edit source]
Amyotrophic lateral sclerosis (ALS), also know as Lou Gehrig's disease, is a fatal neurological disorder with an adult-onset around 54–67 years old, and it belongs to a group of conditions known as Motor Neurone Diseases (MND). Its clinical hallmark is the degeneration of both upper and lower motor neurons, leading to progressive muscle atrophy and weakness, and ultimately to paralysis. Death, often resulting from swallowing problems and respiratory failure, usually occurs within 2–4 years from disease onset, although 5–10% of ALS patients survive over 10 years[1].
Image - Noted physicist Stephen Hawking [who suffered from ALS] enjoys zero gravity during a flight aboard a modified Boeing 727 aircraft owned by Zero Gravity Corp.
Physical therapy is an integral component of the ALS multidisciplinary team and is well-grounded in rehabilitation and active living concepts. Despite the lack of a cure and rapidly progressive nature of the disease, physical therapy that is tailored to the individual’s needs and goals enables the client to live life to the fullest and with quality[2].
The incidence and prevalence increase with age and reaches a cumulative lifetime risk of 1 in 400 after 80 years old. Due to the projected ageing of the global population, ALS cases are expected to increase by 69% in the next 25 years, and there is a need to identify causes, biomarkers and therapeutic targets for ALS[1].
Descriptions of the disease date back to at least 1824. In 1869, the connection between the symptoms and the underlying neurological problems (involvement of the cortico-spinal tract) was first described by Jean-Martin Charcot. In 1874 Charcot began using the term amyotrophic lateral sclerosis (ALS). The disease became widely publicised in the United States when it affected the famous baseball player Lou Gehrig, and later when the ice bucket challenge became popular in 2014.
The 2-minute video below gives a good introduction to ALS.
Background Epidemiology and Prognosis[edit | edit source]
ALS is the most common form of motor neuron disease in adults[4][5] The incidence of ALS is approximately 1-2.6 cases per 100 000 persons annually, with a prevalence of approximately 6 cases per 100 000[6][5]. In the UK ALS affects around two in every 100,000 people each year and at any one time, there are about 5,000 people living with the condition.[7]
- For about half of those with the condition the mean life expectancy from the onset of symptoms to death is 2-4 yrs
- Only 20% live beyond 5yrs
- 5% of those diagnosed had it before they were 47 years old
- Incidence peaks between 55 and 65 years of age
- Clinicians are reporting that they are seeing increasing numbers of younger ALS patients.
- Prognostic indicators[8]
- Younger patients (less than 35-40 years old) have better 5-year survival rates
- Individuals with limb symptoms at onset versus bulbar signs have improved 5-year survival rates (37 to 44% versus 9 to 16%)
- Individuals with better psychological well-being and support at onset have longer survival rates
- Disease course varies from several months to 20 years
- Average duration of 27 to 43 months
- Five-year survival rates from 9% to 40%
- Ten-year survival rate from 8% to 16%
Aetiology[edit | edit source]
The causes of ALS essentially unknown but several factors are thought to be involved including environmental risk factors,[9] Gene mutations have also been identified in some cases of ALS[6][9]
- Genetic – this is not true for all cases but some mutations have been identified in some individuals. In these cases, it is not uncommon to have several cases in one family.[7][10]
- Biochemistry – it appears that MND mainly occurs through the activation of calcium-dependent enzymatic pathways.
- Premature ageing of some motor cells may lead to damage and destruction if these cells. This then puts pressure on the surviving cells
- Sporadic MND
- Sporadic ALS (90-95%) constitutes the large majority of cases[5]
- Most common in men[5]
- Yearly incidence is 1-2 per 100,000[6] Familial MND
- Family history of either motor neurone disease or a related condition called frontotemporal dementia.[7]
- Autosomal dominant
- Mean age-onset 47 years of age
- Represents 5-10% of all ALS occurrences[5]
Pathophysiology[edit | edit source]
In the progression of the disease, there is a loss of motor neurones from the anterior horn of the spinal cord, the primary motor cortex and from the hypoglossal nucleus in the lower medulla. Shrinkage and discolouration of the anterior nerve roots in the spinal cord occur because of axonal degeneration of the neurones and the accompanying demyelination.[11]
The pathophysiology behind the disease appears to be multi-factorial with complex interactions between genetics and molecular pathways.[10]
Potential cellular & molecular mechanisms that contribute to the neurodegeneration of MND:[10][12]
- Abnormal mitochondria functioning
- Increased oxidative stress
- Increased free radicals
- Impaired axonal transport
- Sodium-potassium pump dysfunction
- Increased inflammatory mediators
- Increased toxin secretion
- Protein mutation affecting RNA metabolism
- Glutamate excitotoxicity - 2x greater than normal plasma levels
Potential gene mutations that are harmful to neurons and could contribute to the disease:[10]
- TARDBP
- FUS
Irrespective of the direct pathways, as the disease progresses there is a demyelinating process which occurs in all areas of the spinal cord except the posterior columns. reference
Clinical Manifestations[edit | edit source]
Initial symptoms may be slight and go unnoticed. ALS may start with intermittent muscle twitching, weakness and in some cases slurred speech. The progression of ALS can also vary between individuals.[7][13]
Initial Symptoms[edit | edit source]
Symptoms may vary depending on where it first manifests. However, it presents with a combination of upper and lower motor neuron signs.
Lower motor neuron signs:
- Asymmetric weakness of distal limbs progressing proximally - often first sign
- UE extensors weaker than flexors (especially in hands, also leads to head droop and increased lumbar lordosis
- Bulbar Signs: facial muscle weakness, dysarthria, dysphagia, tongue fasciculations, drooling[8]
Upper motor neuron signs:
- Spasticity
- Lack of dexterity
- Loss of strength
- Pseudobulbar Affect
- Hyperreflexia
- Positive pathological reflexes (Babinski, Hoffman's sign)
- Clonus[8]
Typically, the oculomotor nerves are spared in addition to the posterior columns of the spinal cord, which means that eye movements, sensation, bowel and bladder function remain intact.
Limb-Onset Disease[edit | edit source]
- Weakened grip
- Weakness at shoulder
- Weakness at ankle or hip
- Widespread twitching of the muscles (fasciculations)
- Muscle cramps
- Visible wasting of the muscles with significant weight loss
Respiratory-Onset Disease[edit | edit source]
- Breathing difficulties
- Shortness of breath
- Waking up frequently during the night because the brain is temporarily starved of oxygen when lying down
Advanced Symptoms[edit | edit source]
- Muscle weakness
- Muscle Atrophy
- Movement difficulty
- Spasticity
- Excess saliva from reduced swallowing
- Thicker saliva may sometimes be difficult to clear from the chest or throat due to weakening of muscles
- Excess yawning
- Emotionality
- Difficulties with concentration, planning and use of language
- Fronto-temporal dementia – this affects their ability to problem solve and respond to new situations[4]
- Breathing difficulties, such as shortness of breath
End-Stage Symptoms[edit | edit source]
- Increasing body paralysis
- Significant shortness of breath
- Astrocytic Gliosis - cortical involvement seen in later stages of the disease, affecting 50% of individuals resulting in deficits in executive functions, attention, and language comprehension[8][14]
Secondary Symptoms[edit | edit source]
These are not directly caused by the disease but are related to the stress of living with it.
- Depression
- Insomnia
- Anxiety
Diagnosis[edit | edit source]
There is no single test that diagnoses an individual with ALS[13]. However, several characteristics of the disease can be identified and therefore used to point practitioners in the right direction. El Escorial Criteria mentions the specific characteristics and features that need to be displayed in an individual for a proper ALS diagnosis; although they are not exclusive. It classifies diagnosis into four different categories depending on the severity of upper (UMN) as well as lower motor neuron (LMN) degeneration (which must not be explained by the presence of her neurological disorder). Physicians use a combination of a few methods such as electromyography and neuroimaging to identify UMN and LMN degeneration which is the most prominent feature in neurodegenerative disorders. Furthermore, current research is looking into whole-brain magnetic resonance spectroscopic imaging (MRSI) as a source of determining disability levels in ALS in the future.
- With the exception of one genetic test, no definitive diagnostic test or biological marker exists for ALS – however, not all individuals with the disease present with this gene
- El Escorial Criteria for diagnosis of ALS (revised): [13]
The diagnosis of Amyotrophic Lateral Sclerosis (ALS) requires:
- The presence of:
- Evidence of lower motor neuron (LMN) degeneration by clinical, electrophysiological or neuropathologic examination,
- Evidence of upper motor neuron (UMN) degeneration by clinical examination, and
- Progressive spread of symptoms or signs within a region or to other regions, as determined by history or examination.
Together with:
- The absence of:
- Electrophysiological and pathological evidence of other disease processes that might explain the signs of LMN and/or UMN degeneration, and
- Neuroimaging evidence of other disease processes that might explain the observed clinical and electrophysiological sign
Treatment/Management[edit | edit source]
There is increasing evidence that ALS should be regarded as a multisystem health condition rather than solely a motor disease. There is no cure or standard treatment for ALS so the focus is on supportive treatments that aim to maintain the individuals’ quality of life[7]. Treatment should take a holistic approach as the disease can be very distressing for the individual and their family and it is important not only to focus on the physical aspect of the disease but also the emotional and psychosocial components.[6]
Physiotherapy, respiratory and occupational therapy and social care are important in the care of those with ALS. Dietitians can help ensure that those with ALS eat a balanced diet and receive proper nutrition to help them maintain weight and keep up their strength as individuals can often lose weight as their ability to swallow is impaired. Dietitians can also advise patients as certain foods, such as dairy products could contribute to the production of thicker secretions.[4]
As the disease progresses breathing becomes increasingly difficult and the use of non-invasive ventilation can significantly improve the quality of life and may also increase the patient’s life expectancy by about 7 months.[15]
Physiotherapy[edit | edit source]
Because of the variable clinical presentation of people with ALS [PALS], the great variability in prognosis, and the typically rapid, progressive, and deteriorating nature of ALS, we as physical therapists are constantly challenged when developing the most appropriate intervention plan for PALS. The physical therapist needs an understanding of the nature and course of the disease and needs to consider future problems in addition to current status. In order to make appropriate and effective decisions, the nature and significance of the activity limitations, and participation restrictions need to be determined. Decision-making involves determining which impairments, activity limitations, and participation restrictions:
- Can be restored
- Require compensatory strategies or interventions
- Require referral to a different health care professional(s) and
- Cannot be affected by physical therapy interventions at all.[2]
Many of the problematic symptoms of ALS can be addressed by appropriate physical therapy interventions[2]
- Fatigue (energy conservation)
- muscle stiffness (stretching exercises)
- Muscle cramps (stretching exercises)
- Pain (intervention dependent on the source of pain)
Exercises should focus on improving posture, preventing joint immobility, and slowing the progressive muscle weakening and atrophy. Stretching and strengthening exercises may help reduce spasticity, increase range of motion and improve circulation. The video below gives an example of a simple home exercise plan.
Physical therapy can enhance an individual’s independence throughout the course of the disease. Gentle, low-impact aerobic exercise such as walking, swimming, and stationary bicycling can strengthen unaffected muscles, improve cardiovascular health, and aid people fight fatigue and depression, contractures of muscles.
Other modalities, such as heat application and massage may help relieve pain.
Assistive devices such as supports or braces, orthotics, speech synthesisers, and wheelchairs may help some people retain independence. The video below describes some adaptive devices that may be used.
The following video may also be of help to view when planning a program.
| [20] |
Current and Future Research[edit | edit source]
Research options fall largely into three categories: drugs, gene therapy, and stem cells.[10]
Although evidence from a review in 2019[21] supports the advantageous impact of exercise in ALS, it is still not clear whether physical activity should be recommended as a treatment option for ALS patients. Even if exercise training per se is not a sufficient intervention to decelerate disease progression or improve patients' survival, it could be an adjunct therapy to other pharmacological treatments of ALS. Considering the lack of treatments at this time in ALS, non-pharma therapeutics, such as physical activity, is likely to be more important than previously appreciated.
Clinical trials are testing whether different drugs or interventions are safe and effective in slowing the progression of ALS in patient volunteers.
Cellular and molecular studies seek to understand the mechanisms that trigger motor neurons to degenerate.[6]
Presentations[edit | edit source]
 |
Overview of Amyotrophic Lateral Sclerosis
Dr. Leo McCluskey provides an overview of Amyotrophic Lateral Sclerosis at the February 2012 FTD Caregiver Conference, University of Pennsylvania, Philadelphia, PA. |
References[edit | edit source]
- ↑ 1.0 1.1 Vijayakumar UG, Milla V, Stafford C, Bjourson T, Duddy WJ, Duguez SR. A systematic review of suggested molecular strata, biomarkers and their tissue sources in ALS. Frontiers in neurology. 2019;10:400. Available from: https://www.frontiersin.org/articles/10.3389/fneur.2019.00400/full (last accessed 14.12.2019)
- ↑ 2.0 2.1 2.2 Dal Bello-Haas V. Physical therapy for individuals with amyotrophic lateral sclerosis: current insights. Degenerative neurological and neuromuscular disease. 2018;8:45. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6065609/ (last accessed 14.12.2019)
- ↑ Neuroscientifically Challenged ALS Available from: https://www.youtube.com/watch?v=kOnk9Hh20eg&app=desktop (last accessed 14.12.2019)
- ↑ 4.0 4.1 4.2 Marsden, R. Motor neurone disease: an overview. Primary Health Care 2011; 21;10;31-36 (Accessed 18th May 2015)
- ↑ 5.0 5.1 5.2 5.3 5.4 Talbott EO, Malek AM, Lacomis D. The epidemiology of amyotrophic lateral sclerosis. In Handbook of clinical neurology 2016 Jan 1 (Vol. 138, pp. 225-238). Elsevier.
- ↑ 6.0 6.1 6.2 6.3 6.4 National Institute of Neurological Disorders and Stroke. . Amyotrophic Lateral Sclerosis (ALS) Fact Sheet, NINDS, Publication date June 2013.NIH Publication No. 16-916 (Accessed 23rd April 2019)
- ↑ 7.0 7.1 7.2 7.3 7.4 NHS Information http://www.nhs.uk/Conditions/Motor-neurone-disease/Pages/Symptoms.aspx (accessed April 28th at 11:49)
- ↑ 8.0 8.1 8.2 8.3 O’Sullivan SB, Schmitz TJ, Fulk G. Physical rehabilitation. F.A. Davis; 2019. p712-752.
- ↑ 9.0 9.1 Martin S, Al Khleifat A, Al-Chalabi A. What causes amyotrophic lateral sclerosis?. F1000Research. 2017;6.
- ↑ 10.0 10.1 10.2 10.3 10.4 Kiernan, M.C., Vucic, S., Cheah, B.C., Turner, M.R., Eisen, A., Hardiman, O., Burrell, J.R., Zoing, M.C. Amyotrophic lateral sclerosis. Lancet 2011; 377; 942-55 http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2810%2961156-7/abstract (accessed 4th May 2015)
- ↑ Jeans, A.F., Ansorge, O. Recent developments in the pathology of Motor Neurone Disease. Advances in Clinical Neuroscience and Rehabilitation; Neuropathology Article 2009; 9; 4; 25-26 http://www.acnr.co.uk/SO09/ACNRSO09_web.pdf (Accessed 4th May 2015)
- ↑ Mohamed LA, Markandaiah SS, Bonanno S, Pasinelli P, Trotti D. Excess glutamate secreted from astrocytes drives upregulation of P-glycoprotein in endothelial cells in amyotrophic lateral sclerosis. Exp Neurol [Internet]. 2019;316:27–38
- ↑ 13.0 13.1 13.2 ALS Association. Factsheet: Criteria for the diagnosis of Amyotrophic Lateral Sclerosis. El Escorial World Federation of Neurology. http://www.alsa.org/assets/pdfs/fyi/criteria_for_diagnosis.pdf (Accessed 4 May 2015).
- ↑ Goodman CC & Fuller KS. Pathology: Implications for the Physical Therapist. 5th ed. Philadelphia, PA: Saunders; 2021. p1408-1417.
- ↑ Gent, C. Understanding motor neurone disease. Nursing and Residential Care 2013; 14;12; 646-649. http://dx.doi.org.gcu.idm.oclc.org/10.12968/nrec.2012.14.12.646 (Accessed 18th May 2015).
- ↑ ALS hope foundation ALS exercises Available from: https://www.youtube.com/watch?v=IKxnWbclFic&app=desktop (last accessed 14.12.2019)
- ↑ reference
- ↑ All health TV PT and ALS Available from: https://www.youtube.com/watch?v=Hihu8mi1R5E&app=desktop (last accessed 14.12.2019)
- ↑ ALS hope foundation ALS exercises Available from: https://www.youtube.com/watch?v=IKxnWbclFic&app=desktop (last accessed 14.12.2019)
- ↑ Weyton Tam. Seeking ALS Answers: Range of Motion Therapy. Available from: http://www.youtube.com/watch?v=myoazlf9pdc [last accessed 15/01/16]
- ↑ Tsitkanou S, Della Gatta PA, Foletta VC, Russell AP. The role of exercise as a non-pharmacological therapeutic approach for Amyotrophic Lateral Sclerosis: beneficial or detrimental?. Frontiers in neurology. 2019;10:783. Avaiable from: https://www.frontiersin.org/articles/10.3389/fneur.2019.00783/full (last accessed 15.2.2019)