Tetanus: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) (Removed copyright violation image) |
||
| (125 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- Natalie Gutmann [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | '''Original Editors '''- Natalie Gutmann [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
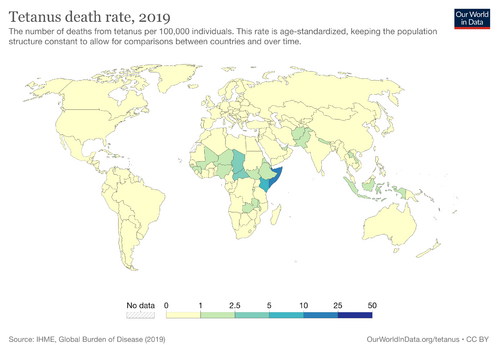
[[File:Tetanus-death-rate.png|alt=|right|frameless|499x499px]] | |||
Tetanus is an infection causing generalised [[Hypertonia Assessment Tool|hypertonia]] presenting with painful muscle spasms of the jaw and neck. Tetanus commonly occurs in the unvaccinated or in the [[Older People Introduction|elderly]] with reduced immunity. | |||
* Vaccination campaigns have decreased the incidence and prevalence of tetanus worldwide. | |||
* Symptoms are caused by toxins produced by the [[Bacterial Infections|bacterium]], Clostridium tetani.<ref name=":0">Bae C, Bourget D. [https://www.statpearls.com/articlelibrary/viewarticle/29997/ Tetanus].[Updated 2020 May 28]. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2021.Available:https://www.statpearls.com/articlelibrary/viewarticle/29997/ (accessed 17.12.2022)</ref> | |||
== | == Etiology == | ||
The most common way the bacterium enters the body is through [[Wound Assessment|wounds]] which are susceptible to infection if they are: contaminated with soil, feces, or saliva; puncture wounds including unsterile injection sites; devitalized tissue including [[Burns Overview|burns]], avulsions and degloving injuries. | |||
When in the body the bacterium secretes toxin,<ref name="Ewcombe">Ewcombe P. Treating and preventing tetanus in A&E. Emergency Nurse. October 2004;12(6):23-29.</ref>Tetanus toxin causes the typical clinical manifestations of tetanus by interfering with the release of neurotransmitters and blocking inhibitor impulses. This leads to unopposed muscle contraction and spasm. Seizures may occur, and the autonomic nervous system may also be affected.<ref>NSN search How does tetanus affect muscle contraction? Available: https://nsnsearch.com/how-to/how-does-tetanus-affect-muscle-contraction/ (accessed 18.12.20220</ref> | |||
The two toxins secreted into the bloodstream are: | |||
# Tetanospasmin affects the [[Neurone|nerve]] and muscle motor endplate interaction, causing the clinical syndrome of rigidity, muscle spasms, and autonomic instability. | |||
# Tetanolysin damages the tissues.<ref name=":0" /> | |||
== Epidemiology == | |||
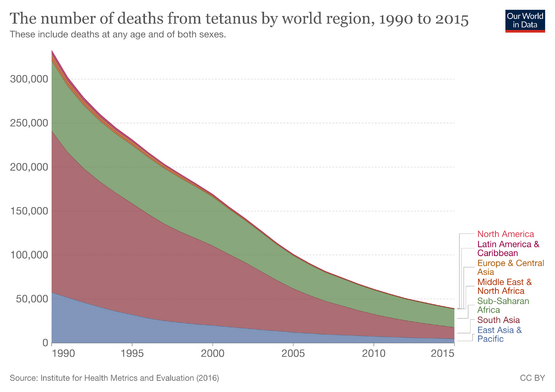
[[File:The-number-of-deaths-from-tetanus-by-world-region.png|right|frameless|555x555px|Number of-deaths-from-tetanus]] | |||
The highest prevalence is seen in newborns and young persons. | |||
* The World Health Organization (WHO) reports improvement in mortality rates from tetanus, due to vaccination campaigns in recent years. | |||
* The WHO estimates worldwide tetanus deaths in 1997 at around 275,000 with improved rates in 2011 at 14,132 cases.<ref name=":0" /> | |||
== Presentation == | |||
The incubation period of tetanus varies between 3 and 21 days after infection, with most cases occur within 14 days. | |||
Symptoms can include: | |||
* Jaw cramping/inability to open the mouth | |||
* Muscle spasms commonly in torso, abdomen and extremities | |||
* Painful muscle spasms triggered by eg sudden noises | |||
* Dysphagia | |||
* Seizures | |||
* Headache | |||
* Fever | |||
* Unstable [[Blood Pressure|blood pressure]] or [[tachycardia]].<ref name=":1">World Health Organisation [https://www.who.int/news-room/fact-sheets/detail/tetanus Tetanus] Available:https://www.who.int/news-room/fact-sheets/detail/tetanus (accessed 17.12.2022)</ref> | |||
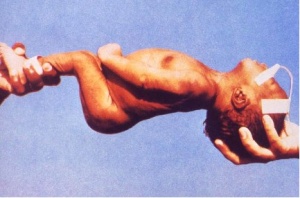
[[Image:Neonatal tetanus.jpg|thumb|right|Neonatal muscluar rigidity and spasms]]Neonatal tetanus causes more than 50% of deaths from tetanus worldwide but is very rare in developed countries. Neonates present within a week of birth with a short history of failure to feed, vomiting, and ‘convulsions’. Spasms are generalized and mortality is high. Poor umbilical hygiene is the cause of the disease which is preventable by maternal [[Vaccines|vaccination]], even during pregnancy.<ref>Cook TM, Protheroe RT, Handel JM. Tetanus: a review of the literature. British Journal of Anaesthesia. 2001 Sep 1;87(3):477-87. Available: https://academic.oup.com/bja/article/87/3/477/333174?login=false<nowiki/>(accessed 18.12.2022)</ref> | |||
== Treatment == | |||
Tetanus, a medical emergency, requires | |||
< | * Hospitalisation | ||
* Early intramuscular or intravenous administration of the human tetanus immunoglobulin (HTIG). | |||
* Combative wound care | |||
* Antispasmodics eg benzodiazepines, baclofen, vecuronium, pancuronium, and propofol | |||
* Antibiotic therapy (metronidazole, slows progression of disease)<ref name=":0" /> | |||
* Tetanus vaccination. | |||
Patients with severe symptoms need to be admitted to the ICU for close monitoring and mechanical ventilation. Healthcare providers need to provide supportive care, especially for patients with autonomic instability. | |||
Rehabilitation may take weeks or months.<ref name=":1" /> | |||
< | == Diagnosis == | ||
There are no specific laboratory or diagnostic tests used to diagnosis tetanus. The diagnosis is made based on clinical signs and symptoms and not on the confirmation of the bacteria C. tetani in the body. <ref name="CDC">CDC. Tetanus: Questions and Answers. November 2010.www.immunize.org.</ref><ref name="Grunau">Grunau BE, Olson J. [https://pubmed.ncbi.nlm.nih.gov/20078924/ An interesting presentation of pediatric tetanus.] Canadian Journal of Emergency Medicine. 2010 Jan;12(1):69-72. Available:https://pubmed.ncbi.nlm.nih.gov/20078924/ (accessed 23.12.2022)</ref>“C. tetani is recovered from the wound in only 30% of cases and can be isolated from patients who do not have tetanus.”<sup><ref name="CDC" /></sup> | |||
== Physical Therapy Management == | |||
= | Currently research is limited on the Physical therapy management of individuals with tetanus. Cardiopulmonary physical therapy can be used to help in the prevention of respiratory complications.<ref name="Cook">Cook T, Protheroe R, Handel J. Tetanus: a review of the literature. British Journal Of Anaesthesia. September 2001;87(3):477-487. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2011.</ref> Physical therapy can also be used to help with muscle rigidity and spasms. | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
Latest revision as of 15:19, 23 July 2023
Original Editors - Natalie Gutmann from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Natalie Gutmann, Elaine Lonnemann, Lucinda hampton, Admin, Kim Jackson, WikiSysop, Wendy Walker and 127.0.0.1
Introduction[edit | edit source]
Tetanus is an infection causing generalised hypertonia presenting with painful muscle spasms of the jaw and neck. Tetanus commonly occurs in the unvaccinated or in the elderly with reduced immunity.
- Vaccination campaigns have decreased the incidence and prevalence of tetanus worldwide.
- Symptoms are caused by toxins produced by the bacterium, Clostridium tetani.[1]
Etiology[edit | edit source]
The most common way the bacterium enters the body is through wounds which are susceptible to infection if they are: contaminated with soil, feces, or saliva; puncture wounds including unsterile injection sites; devitalized tissue including burns, avulsions and degloving injuries.
When in the body the bacterium secretes toxin,[2]Tetanus toxin causes the typical clinical manifestations of tetanus by interfering with the release of neurotransmitters and blocking inhibitor impulses. This leads to unopposed muscle contraction and spasm. Seizures may occur, and the autonomic nervous system may also be affected.[3]
The two toxins secreted into the bloodstream are:
- Tetanospasmin affects the nerve and muscle motor endplate interaction, causing the clinical syndrome of rigidity, muscle spasms, and autonomic instability.
- Tetanolysin damages the tissues.[1]
Epidemiology[edit | edit source]
The highest prevalence is seen in newborns and young persons.
- The World Health Organization (WHO) reports improvement in mortality rates from tetanus, due to vaccination campaigns in recent years.
- The WHO estimates worldwide tetanus deaths in 1997 at around 275,000 with improved rates in 2011 at 14,132 cases.[1]
Presentation[edit | edit source]
The incubation period of tetanus varies between 3 and 21 days after infection, with most cases occur within 14 days.
Symptoms can include:
- Jaw cramping/inability to open the mouth
- Muscle spasms commonly in torso, abdomen and extremities
- Painful muscle spasms triggered by eg sudden noises
- Dysphagia
- Seizures
- Headache
- Fever
- Unstable blood pressure or tachycardia.[4]
Neonatal tetanus causes more than 50% of deaths from tetanus worldwide but is very rare in developed countries. Neonates present within a week of birth with a short history of failure to feed, vomiting, and ‘convulsions’. Spasms are generalized and mortality is high. Poor umbilical hygiene is the cause of the disease which is preventable by maternal vaccination, even during pregnancy.[5]
Treatment[edit | edit source]
Tetanus, a medical emergency, requires
- Hospitalisation
- Early intramuscular or intravenous administration of the human tetanus immunoglobulin (HTIG).
- Combative wound care
- Antispasmodics eg benzodiazepines, baclofen, vecuronium, pancuronium, and propofol
- Antibiotic therapy (metronidazole, slows progression of disease)[1]
- Tetanus vaccination.
Patients with severe symptoms need to be admitted to the ICU for close monitoring and mechanical ventilation. Healthcare providers need to provide supportive care, especially for patients with autonomic instability.
Rehabilitation may take weeks or months.[4]
Diagnosis[edit | edit source]
There are no specific laboratory or diagnostic tests used to diagnosis tetanus. The diagnosis is made based on clinical signs and symptoms and not on the confirmation of the bacteria C. tetani in the body. [6][7]“C. tetani is recovered from the wound in only 30% of cases and can be isolated from patients who do not have tetanus.”[6]
Physical Therapy Management[edit | edit source]
Currently research is limited on the Physical therapy management of individuals with tetanus. Cardiopulmonary physical therapy can be used to help in the prevention of respiratory complications.[8] Physical therapy can also be used to help with muscle rigidity and spasms.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Bae C, Bourget D. Tetanus.[Updated 2020 May 28]. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2021.Available:https://www.statpearls.com/articlelibrary/viewarticle/29997/ (accessed 17.12.2022)
- ↑ Ewcombe P. Treating and preventing tetanus in A&E. Emergency Nurse. October 2004;12(6):23-29.
- ↑ NSN search How does tetanus affect muscle contraction? Available: https://nsnsearch.com/how-to/how-does-tetanus-affect-muscle-contraction/ (accessed 18.12.20220
- ↑ 4.0 4.1 World Health Organisation Tetanus Available:https://www.who.int/news-room/fact-sheets/detail/tetanus (accessed 17.12.2022)
- ↑ Cook TM, Protheroe RT, Handel JM. Tetanus: a review of the literature. British Journal of Anaesthesia. 2001 Sep 1;87(3):477-87. Available: https://academic.oup.com/bja/article/87/3/477/333174?login=false(accessed 18.12.2022)
- ↑ 6.0 6.1 CDC. Tetanus: Questions and Answers. November 2010.www.immunize.org.
- ↑ Grunau BE, Olson J. An interesting presentation of pediatric tetanus. Canadian Journal of Emergency Medicine. 2010 Jan;12(1):69-72. Available:https://pubmed.ncbi.nlm.nih.gov/20078924/ (accessed 23.12.2022)
- ↑ Cook T, Protheroe R, Handel J. Tetanus: a review of the literature. British Journal Of Anaesthesia. September 2001;87(3):477-487. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2011.