Menarche to Menopause: Difference between revisions
Carin Hunter (talk | contribs) No edit summary |
mNo edit summary |
||
| (23 intermediate revisions by 4 users not shown) | |||
| Line 2: | Line 2: | ||
== Introduction == | == Introduction == | ||
A female will spend approximately 12% of her life from birth to menarche, approximately 40% after menarche and through her reproductive years, and approximately 40% from menopause through her post-menopausal years.<ref name=":0">Piché S. Menarche to Menopause Course. Plus , 2022.</ref> Pregnancy and the postpartum period can take from 12 to 21 months, for a complicated case, which works out to possibly 2% of a woman's life. Women spend a great deal of time preparing for and understanding pregnancy and birth, but often do not apply the same understanding and consideration to the other aspects of their health, including menarche and menopause. It is important that we focus understanding on these transitions in life and encourage women to adequately prepare for them. | |||
==== Complex Female Developmental Process ==== | |||
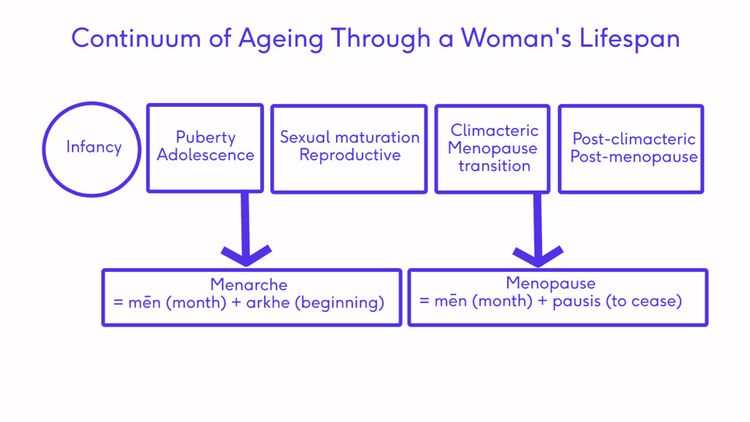
[[File:Continuum of Aging Female-CreatedbyDaphneXuan.jpg|center|frameless|750x750px]] | |||
The diagram above shows the transitions a female will pass through in an average life span. The onset of these transitions can be estimated by looking at common signs and symptoms. | |||
== Diagnosis of Stages == | |||
Transitional phases are not "diseases" that need a specific diagnosis.<ref name=":0" /> But a functional diagnosis can be made based on the signs and symptoms a women is experiencing. The aim of making a "diagnosis" is to offer the person support, care and education. Not all women pass through the stages in life in a completely linear process. They might move back and forth between stages or even skip a stage. This does not always indicate a problem or that the woman is not healthy. Rather, it shows that these stages and transitions should be understood by the individual, so they can care for themselves appropriately based on the phase they are currently in.<ref name=":0" /> | |||
* | ===== Common considerations ===== | ||
* Age of female | |||
* | ** Younger (8-16 years) for menarche transition | ||
** Older (45-54 years) for menopause transition | |||
* | * Character of menses | ||
** Regularity | |||
** Duration | |||
* | ** Flow heaviness | ||
* Physical changes | |||
** Breast budding | |||
** Growth spurt | |||
** Low energy / fatigue | |||
** Acne, bloating | |||
** Fluid retention | |||
* Mental changes | |||
** Moodiness | |||
** Short temperedness | |||
** Difficulty concentrating | |||
=== Puberty === | |||
Puberty is the transitional stage from childhood up to menarche. <ref>Howard SR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9291332/pdf/CEN-95-702.pdf Interpretation of reproductive hormones before, during and after the pubertal transition-Identifying health and disordered puberty.] Clin Endocrinol (Oxf). 2021 Nov;95(5):702-715. </ref> Regular monitoring<ref>Mendle J, Beltz AM, Carter R, Dorn LD. [https://onlinelibrary.wiley.com/doi/abs/10.1111/jora.12371 Understanding puberty and its measurement: ideas for research in a new generation.] Journal of Research on Adolescence. 2019 Mar;29(1):82-95.</ref> using a Health Client Check should be conducted during this phase, with regular educational conversations from the age of approximately 6 years old.<ref name=":0" /> | |||
During this phase, fertility cannot be assumed as there is no definitive point at which eggs become viable. This knowledge can only be assumed after the onset of menarche. Education regarding contraception is essential to the health of a female in this transitional time.<ref name=":0" /> | |||
Puberty happens to everyone between the ages of 6-16 yrs, but menarche is unique to females. It occurs approximately 2 years after the onset of secondary sex characteristic changes (specifically breast budding), at an approximate age of 12.4 years. This age has been decreasing, presumably due to nutrition and lifestyle changes, but further research is required on this topic.<ref name=":0" /> | |||
===== HPG Axis ===== | |||
The structures involved in this stage are the HPG axis and the adrenal glands. The HPG axis consists of the hypothalamus, pituitary gland and the ovaries. A pulsing release of gonadotropin-releasing hormone stimulates the pituitary gland to release two important hormones: luteinising hormone (LH), and follicle-stimulating hormone (FSH). This initiates the production of oestrogen, which is needed to stimulate the secondary sexual characteristics, along with the adrenals. Adrenal gland maturation is an independent but interrelated process. Other hormones are also involved before puberty to mature the eggs in the ovaries and they become key to maintaining the cyclic reproductive function.<ref name=":0" /> | |||
puberty is the | ===== Health Client Check ===== | ||
The onset of puberty for a female should be identified and monitored to support good health or to identify disease processes that may require treatment. Regular health visit monitoring should include a visual examination of external primary sex characteristics, including the external genitalia. When a female is sexually active, an examination of the internal primary sex characteristics should be advised. A Health Client Check also entails a height and weight measurement with the identification of the appearance of any secondary sex characteristics.<ref name=":0" /> These basic markers should be reviewed at each health visit:<ref name=":0" /> | |||
* Visual examination for external primary sex characteristics | |||
* Height / weight | |||
* Identification of appearance of secondary sex characteristics | |||
* Prepubertal genital exam by a doctor | |||
===== Sexual Maturity Rating (SMR) - Tanner Stages ===== | |||
Sexual Maturity Rating (SMR), better known as the Tanner Stages, is an objective classification system that providers use to document and track the development and sequence of secondary sex characteristics of children during puberty. In females, the most important characteristics are breast development and pubic hair growth. There are other characteristics that are noteworthy: a rounded or hourglass figure; increased hip girth; an increased body fat composition; and comparatively to our male counterparts, a slower ability to generate muscle mass and less upper body strength. | |||
Approximately 2 to 2.5 years after a female is Tanner stage 2, a female will start to have her period. This is known as menarche, and when she begins to bleed, this is the start of the menstrual cycle and the reproductive stage.<ref name=":0" /> | |||
Please click here to see a [https://quizlet.com/514600861/tanner-stages-flash-cards/ Tanner Stages Image]. | |||
=== Menarche === | |||
Menarche occurs at the beginning of the reproductive stage and is marked by the first menstrual period. It occurs during the late stages of puberty and signals the probability of ovulation and the beginning of a woman’s reproductive years.<ref>Lacroix AE, Gondal H, Langaker MD. [https://www.ncbi.nlm.nih.gov/books/NBK470216/ Physiology, menarche]. InStatPearls [Internet] 2021 Mar 27. StatPearls Publishing.</ref> Chronological age is not a useful predictor; the Tanner Stages and signs and symptoms are more accurate.<ref name=":0" /> | |||
'''Important definitions:''' | |||
* '''Precocious puberty''' - the early onset of puberty before the age of 8 in females<ref>Kota AS, Ejaz S. [https://www.ncbi.nlm.nih.gov/books/NBK544313/ Precocious puberty.] InStatPearls [Internet] 2021 Jul 25. StatPearls publishing.</ref> | |||
* '''Amenorrhea''' is the absence of menarche onset; can be indicative other disease processes in the body<ref name=":0" /> | |||
** '''Primary amenorrhea''' is a failure to reach menarche - evaluation is required in the following situations:<ref name=":2">Gasner A, Rehman A. [https://www.statpearls.com/articlelibrary/viewarticle/17440/ Primary amenorrhea]. 2022 Mar 20. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 32119356.</ref> | |||
*** Client is 13 years old and has no secondary sex characteristics | |||
*** Menarche does not occur after five years of initial breast development | |||
*** Client is 15 years or older and menarche has not occurred | |||
** '''Secondary amenorrhea''' - "cessation of previous menses for more than 6 months"<ref name=":2" /> | |||
=== Menstruation === | |||
A menstrual period is defined as “the monthly shedding of the functional layer (the endometrial lining) of the uterus.”<ref name=":0" /> | |||
the | At the beginning of menstruation, there are erratic hormone fluctuations which eventually stabilise. Follicles are present in a high percentage of girls, but ovulation does not occur until the girl has had an average of six regular menstrual cycles and monthly ovulation does not become regular for several years.<ref name=":0" /> | ||
An "ideal" menstrual cycle is 28 days long. Day one is the menses, or when the bleeding starts. This commonly lasts for five to seven days and menses is included in the follicular phase. After the cessation of bleeding, the endometrial lining, which is the inner lining of the uterus, begins to thicken until the egg is released. Ovulation, which is the release of the egg, then occurs. The following phase is the luteal phase. The egg could either be fertilised and implanted in the thickened endometrium, or if it is not fertilised, the the egg and the thickened portion of the endometrium are broken down and expelled. This is the beginning of Menses Day 1.<ref name=":0" /> | |||
'''Schedule a medical check up if:'''<ref name=":0" /> | |||
* The girl has not started menstruating within 3 years of breast growth or by the age of 15 | |||
* | * Breasts have not started to grow by the age of 13 | ||
* | * A period lasts more than 7 days | ||
* There is severe pain during periods | |||
* There is bleeding between periods | |||
* The girl / woman gets sick or has a sudden onset of fever after using a tampon | |||
* A period occurs more frequently than 21 days or less frequently than 45 days | |||
* A girl / woman goes 3 months without a period after beginning menstruation | |||
For more information, please see [[Menstruation and Menstrual Rehab]] | |||
=== Menopause === | |||
This stage occurs at the end of the reproductive stage and is marked by the final menstrual period (FMP).<ref>Talaulikar V. [https://www.sciencedirect.com/science/article/abs/pii/S1521693422000426 Menopause transition: Physiology and symptoms.] Best Practice & Research Clinical Obstetrics & Gynaecology. 2022 Mar 16.</ref> Exact timing of this period cannot be forecast and is pinpointed retrospectively when 12 months have passed without a period. The beginning of this transition is referred to as perimenopause and is triggered by the ovaries. The number of viable follicles drops to less than 1,000 and various signs and symptoms can begin to disrupt life.<ref>Santoro N, Kravitz HM. [https://www.obgyn.theclinics.com/article/S0889-8545(18)30074-3/fulltext The Disruptive Changes of Midlife: A Biopsychosocial Adventure]. Obstetrics and Gynecology Clinics. 2018 Dec 1;45(4):xv-ii.</ref> This phase usually occurs between the ages of 45-58 years, but chronological age is not an accurate predictor. The STRAW+10 Staging Scale and common signs and symptoms are a far more useful predictor.<ref name=":0" /> | |||
After a female has had no menstrual cycles for 12 months, she enters the post-menopause stage.<ref name=":0" /> | |||
< | '''<u>Schedule a medical check up if the woman:</u>''' | ||
* Has lengthening or skipped cycles (3 or more) before age 40 | |||
* Has a period that lasts more than 7 days | |||
* Has unusual or severe pain during / between periods, or in post-menopause | |||
* Has vaginal dryness, pain or blood when wiping after toileting | |||
* Has difficulty sleeping and / or feels tired all the time | |||
* Is experiencing decreased quality of life due to symptoms | |||
* Is bleeding in post-menopause | |||
For more information, please see [[Menopause|Menopause.]] | |||
=== | ===== Signs & Symptoms ===== | ||
Health care providers should be approaching menopause in the same way as menarche:<ref name=":0" /> | |||
* Monitoring for regular functioning | |||
* Identifying issues early and treating accordingly | |||
Health | * Initiating conversations prior to transitions | ||
* Encouraging clients to make ‘healthy choices’ within their capability | |||
The following table summarises the signs associated with the transitions between puberty and menarche, and perimenopause and menopause. | |||
* | |||
* | |||
{| | {| | ||
|+ | |+ | ||
Table 1. Signs associated with puberty to menarche and perimenopause to menopause. | |||
!Puberty to Menarche | !'''<u>Puberty to Menarche</u>''' | ||
!Perimenopause to Menopause | !'''<u>Perimenopause to Menopause</u>''' | ||
|- | |- | ||
|Secondary sex characteristics more pronounced | |||
|Vasomotor symptoms VMS (hot flashes/ night sweats) | |||
|- | |- | ||
|Growth spurt | |||
|Vaginal dryness or Genitourinary Syndrome of Menopause (GSM) | |||
|- | |- | ||
|Moodiness, short-tempered, emotional | |||
|Moodiness, short-tempered, emotional | |||
|- | |- | ||
|Low energy / fatigue | |||
|Low energy / fatigue | |||
|- | |- | ||
|Breast tenderness | |||
|Breast tenderness | |||
|- | |- | ||
|Muscle aches | |||
|Muscle aches | |||
|- | |- | ||
|Headaches | |||
|Headaches | |||
|- | |- | ||
| | |Abdominal cramps | ||
|Abdominal cramps | |||
| | |||
|- | |- | ||
| | |Lower back pain | ||
|Lower back pain | |||
| | |||
|- | |- | ||
| | |Difficulty concentrating | ||
|Difficulty concentrating | |||
| | |||
|- | |- | ||
| | |Bloating, fluid retention | ||
|Bloating, fluid retention | |||
| | |||
|- | |- | ||
| | |Joint pain | ||
|Joint pain | |||
| | |||
|- | |- | ||
| | |Food cravings | ||
|Food cravings | |||
| | |||
|- | |- | ||
| | |Acne | ||
| | |Acne | ||
|- | |- | ||
| | |Diarrhoea / constipation | ||
|Diarrhoea / constipation | |||
| | |||
|- | |- | ||
| | |Trouble sleeping | ||
|Trouble sleeping | |||
| | |||
|} | |} | ||
===== Common Medical Concerns during the Menopause Transition ===== | |||
* Primary Ovarian Insufficiency | |||
** This is diagnosed when the ovaries stop working before the age of 40 | |||
* Genitourinary Syndrome in Menopause | |||
** A condition in which the vaginal walls and the vulva become thin and easily break down. Symptoms often include: feeling hot and rough, bleeding when wiping after toileting and discomfort. This condition can be treated with topical creams. | |||
* Diseases which increase in risk post-menopause: | |||
**[[Cardiovascular Disease|Cardiovascular disease]] | |||
**[[Diabetes]] / [[obesity]] | |||
**[[Osteoporosis]] | |||
**[[Dementia]] | |||
** [[Oncology|Cancer]], mainly breast and uterine | |||
===== Regular Assessments ===== | |||
The following assessments should be included:<ref name=":0" /> | |||
* Blood work | |||
** To establish baselines or to eliminate conditions such as thyroid disease and diabetes | |||
==== Regular Assessments | ** Test lipid levels every 2-3 years starting at the age of 40 (but more often if this is a risk of [[Cardiovascular Disease|cardiovascular disease]]) | ||
* Blood work | ** ONLY if there is an indication, it might be recommended to test levels of calcium, vitamin D and hormones | ||
* Height | * Height and weight | ||
* Bone density scan | * ECG baseline | ||
* Assess for sleep/rest habits | * Bone density scan is recommended from the age of 40 for a baseline, with a repeat every 5 years | ||
* Assess for depression as | * Assess for sleep / rest habits | ||
* Assess for depression as its prevalence increases | |||
* Pap test | * Pap test | ||
* | * A mammogram is recommended from the age 40, with monitoring every 3 years | ||
* Colonoscopy age 55 | * Colonoscopy is recommended from the age of 55 | ||
* Encourage clients to track signs and symptoms to facilitate and direct care - this information should be reviewed regularly | |||
* Encourage | |||
==== Healthy Choices ==== | ===== Healthy Choices ===== | ||
* Exercise should include aerobic, strengthening and balance exercises | |||
* Diet/ | * Diet / nutrition for maintenance of health | ||
* | * Do not smoke | ||
* | * Moderate intake of alcohol | ||
* Sleep | * Sleep 8 hours per day | ||
* | * Relaxation techniques | ||
=== | === Stages of Reproductive Aging Workshop (STRAW) === | ||
* | |||
In 2001, the Stages of Reproductive Aging Workshop, otherwise known as STRAW, put together a standard for reproductive ageing. In 2011, STRAW was updated and modified to STRAW+10, which is the gold standard to identify stages within the sexual reproductive periods of a woman's lifespan.<ref name=":0" /> | |||
In | |||
STRAW identifies the stages within the sexual reproductive periods of a woman's lifespan. It divides the adult female life into three broad phases: reproductive, menopausal transition, and post-menopause. These three phases include seven stages which centre on the final menstrual period, which is called Stage 0.<ref name=":1">Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, Sherman S, Sluss PM, De Villiers TJ, STRAW+ 10 Collaborative Group. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3340903/pdf/nihms361103.pdf Executive summary of the Stages of Reproductive Aging Workshop+ 10: addressing the unfinished agenda of staging reproductive aging.] The Journal of Clinical Endocrinology & Metabolism. 2012 Apr 1;97(4):1159-68.</ref> | |||
STRAW divides the reproductive phase into Stages -5 (which is early), -4, (which is classified as peak), and -3 (which is late). Stage–3 is characterised by regular menstrual cycles, as well as increasing levels of follicle-stimulating hormone (FSH).<ref name=":1" /> | |||
The menopausal transition phase includes Stage -2 (early) and Stage -1 (late). During Stage –2, there is variability in the length of the menstrual cycle and increased levels of FSH. During Stage –1, there is the onset of skipped cycles / amenorrhea which lasts at least 60 days, as well as continued elevation of FSH.<ref name=":1" /><ref>Woods NF, Mitchell ES, Coslov N, Richardson MK. [https://journals.lww.com/menopausejournal/Abstract/2021/04000/Transitioning_to_the_menopausal_transition__a.16.aspx Transitioning to the menopausal transition: a scoping review of research on the late reproductive stage in reproductive aging.] Menopause. 2021 Apr 1;28(4):447-66.</ref> | |||
The post-menopause phase includes Stages +1 (early) and +2 (late).<ref name=":1" /> | |||
Please see Harlow et al.'s article: [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3340903/ Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging] for more information. | |||
== Links to Helpful Pages == | |||
== Links to | |||
* [[Menstruation and Menstrual Rehab]] | * [[Menstruation and Menstrual Rehab]] | ||
* [[Menopause]] | * [[Menopause]] | ||
== | == Additional Resources == | ||
===== Videos: ===== | |||
# [https://www.nhs.uk/conditions/periods/fertility-in-the-menstrual-cycle/ Menstrual cycle] an NHS site video | |||
# Dr Jen Gunter, TED Talks on [https://www.ted.com/talks/jen_gunter_what_really_happens_to_your_body_during_menopause?language=en What really happens to your body during Menopause?] | |||
# Video: [https://kidshealth.org/en/kids/puberty-normal-video.html Am I Normal?] (Girls and Puberty) | |||
# What is Menarche? Everything you need to know | |||
{{#ev:youtube|kNlmOe-e23k}} | |||
===== Recommended for Providers ===== | |||
# [https://www.jeanhailes.org.au/health-professionals/tools Menopause Health Tool], Dr Jean Hailes | |||
# [https://www.monash.edu/medicine/sphpm/units/womenshealth/toolkit-management-of-the-menopause Practitioner’s Toolkit], Monash University 2014 | |||
# [https://swhr.org/swhr_resource/menopause-preparedness-fact-sheet/ Menopause Preparedness Fact Sheet], The Society of Women’s Health Research -October 2021. | |||
===== Recommended for Clients and Parents / Guardians ===== | |||
# [https://www.jeanhailes.org.au/resources/menopause-multilingual-fact-sheets Menopause Fact Sheet], August 2019, Dr Jean Hailes, Women’s Health, Available in English, Arabic, Chinese (Simplified), Farsi, Greek, Hindi, Italian, Turkish and Vietnamese. (This project was funded by the Victorian Government) | |||
# [http://www.menopause.org/docs/default-source/2015/menonote-menstrual-calendar-english.pdf Menstrual Calendar], for tracking perimenopause phase, NAMS, 2015 | |||
# [https://redhotmamas.org/ Red Hot Mamas] | |||
# [https://vajenda.substack.com/about The Vajenda] | |||
# [https://www.menopause.org/for-women The North American Menopause Society] | |||
# [https://www.womenshealth.gov/menopause/menopause-symptoms-and-relief US Department of Health and Human Services] | |||
# [https://www.healthywomen.org/content/blog-entry/7-effective-ways-deal-menopause Healthy Women] | |||
# [https://www.menopauseandu.ca/ Canadian Society of Obstetricians and Gynaecologists] | |||
# [https://www.yourperiod.ca/normal-periods/menstruation-around-the-world/ Menstruation Around the World] | |||
# [https://www.hormone.org/menopausemap/index.html Menopause Map] is a great interactive tool to start with to personalise your journey. | |||
Menopause Fact Sheet, August 2019, Dr Jean Hailes, Women’s Health, Available in English, Arabic, Chinese (Simplified), Farsi, Greek, Hindi, Italian, Turkish and Vietnamese. (This project was funded by the Victorian Government) | |||
Red Hot Mamas | |||
The | |||
== References == | |||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category: | [[Category:Plus Content]] | ||
<references /> | |||
[[Category:Womens Health]] | |||
[[Category:Pelvic Health]] | |||
Latest revision as of 15:16, 23 March 2023
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson, Wanda van Niekerk and Ewa Jaraczewska
Introduction[edit | edit source]
A female will spend approximately 12% of her life from birth to menarche, approximately 40% after menarche and through her reproductive years, and approximately 40% from menopause through her post-menopausal years.[1] Pregnancy and the postpartum period can take from 12 to 21 months, for a complicated case, which works out to possibly 2% of a woman's life. Women spend a great deal of time preparing for and understanding pregnancy and birth, but often do not apply the same understanding and consideration to the other aspects of their health, including menarche and menopause. It is important that we focus understanding on these transitions in life and encourage women to adequately prepare for them.
Complex Female Developmental Process[edit | edit source]
The diagram above shows the transitions a female will pass through in an average life span. The onset of these transitions can be estimated by looking at common signs and symptoms.
Diagnosis of Stages[edit | edit source]
Transitional phases are not "diseases" that need a specific diagnosis.[1] But a functional diagnosis can be made based on the signs and symptoms a women is experiencing. The aim of making a "diagnosis" is to offer the person support, care and education. Not all women pass through the stages in life in a completely linear process. They might move back and forth between stages or even skip a stage. This does not always indicate a problem or that the woman is not healthy. Rather, it shows that these stages and transitions should be understood by the individual, so they can care for themselves appropriately based on the phase they are currently in.[1]
Common considerations[edit | edit source]
- Age of female
- Younger (8-16 years) for menarche transition
- Older (45-54 years) for menopause transition
- Character of menses
- Regularity
- Duration
- Flow heaviness
- Physical changes
- Breast budding
- Growth spurt
- Low energy / fatigue
- Acne, bloating
- Fluid retention
- Mental changes
- Moodiness
- Short temperedness
- Difficulty concentrating
Puberty[edit | edit source]
Puberty is the transitional stage from childhood up to menarche. [2] Regular monitoring[3] using a Health Client Check should be conducted during this phase, with regular educational conversations from the age of approximately 6 years old.[1]
During this phase, fertility cannot be assumed as there is no definitive point at which eggs become viable. This knowledge can only be assumed after the onset of menarche. Education regarding contraception is essential to the health of a female in this transitional time.[1]
Puberty happens to everyone between the ages of 6-16 yrs, but menarche is unique to females. It occurs approximately 2 years after the onset of secondary sex characteristic changes (specifically breast budding), at an approximate age of 12.4 years. This age has been decreasing, presumably due to nutrition and lifestyle changes, but further research is required on this topic.[1]
HPG Axis[edit | edit source]
The structures involved in this stage are the HPG axis and the adrenal glands. The HPG axis consists of the hypothalamus, pituitary gland and the ovaries. A pulsing release of gonadotropin-releasing hormone stimulates the pituitary gland to release two important hormones: luteinising hormone (LH), and follicle-stimulating hormone (FSH). This initiates the production of oestrogen, which is needed to stimulate the secondary sexual characteristics, along with the adrenals. Adrenal gland maturation is an independent but interrelated process. Other hormones are also involved before puberty to mature the eggs in the ovaries and they become key to maintaining the cyclic reproductive function.[1]
Health Client Check[edit | edit source]
The onset of puberty for a female should be identified and monitored to support good health or to identify disease processes that may require treatment. Regular health visit monitoring should include a visual examination of external primary sex characteristics, including the external genitalia. When a female is sexually active, an examination of the internal primary sex characteristics should be advised. A Health Client Check also entails a height and weight measurement with the identification of the appearance of any secondary sex characteristics.[1] These basic markers should be reviewed at each health visit:[1]
- Visual examination for external primary sex characteristics
- Height / weight
- Identification of appearance of secondary sex characteristics
- Prepubertal genital exam by a doctor
Sexual Maturity Rating (SMR) - Tanner Stages[edit | edit source]
Sexual Maturity Rating (SMR), better known as the Tanner Stages, is an objective classification system that providers use to document and track the development and sequence of secondary sex characteristics of children during puberty. In females, the most important characteristics are breast development and pubic hair growth. There are other characteristics that are noteworthy: a rounded or hourglass figure; increased hip girth; an increased body fat composition; and comparatively to our male counterparts, a slower ability to generate muscle mass and less upper body strength.
Approximately 2 to 2.5 years after a female is Tanner stage 2, a female will start to have her period. This is known as menarche, and when she begins to bleed, this is the start of the menstrual cycle and the reproductive stage.[1]
Please click here to see a Tanner Stages Image.
Menarche [edit | edit source]
Menarche occurs at the beginning of the reproductive stage and is marked by the first menstrual period. It occurs during the late stages of puberty and signals the probability of ovulation and the beginning of a woman’s reproductive years.[4] Chronological age is not a useful predictor; the Tanner Stages and signs and symptoms are more accurate.[1]
Important definitions:
- Precocious puberty - the early onset of puberty before the age of 8 in females[5]
- Amenorrhea is the absence of menarche onset; can be indicative other disease processes in the body[1]
- Primary amenorrhea is a failure to reach menarche - evaluation is required in the following situations:[6]
- Client is 13 years old and has no secondary sex characteristics
- Menarche does not occur after five years of initial breast development
- Client is 15 years or older and menarche has not occurred
- Secondary amenorrhea - "cessation of previous menses for more than 6 months"[6]
- Primary amenorrhea is a failure to reach menarche - evaluation is required in the following situations:[6]
Menstruation[edit | edit source]
A menstrual period is defined as “the monthly shedding of the functional layer (the endometrial lining) of the uterus.”[1]
At the beginning of menstruation, there are erratic hormone fluctuations which eventually stabilise. Follicles are present in a high percentage of girls, but ovulation does not occur until the girl has had an average of six regular menstrual cycles and monthly ovulation does not become regular for several years.[1]
An "ideal" menstrual cycle is 28 days long. Day one is the menses, or when the bleeding starts. This commonly lasts for five to seven days and menses is included in the follicular phase. After the cessation of bleeding, the endometrial lining, which is the inner lining of the uterus, begins to thicken until the egg is released. Ovulation, which is the release of the egg, then occurs. The following phase is the luteal phase. The egg could either be fertilised and implanted in the thickened endometrium, or if it is not fertilised, the the egg and the thickened portion of the endometrium are broken down and expelled. This is the beginning of Menses Day 1.[1]
Schedule a medical check up if:[1]
- The girl has not started menstruating within 3 years of breast growth or by the age of 15
- Breasts have not started to grow by the age of 13
- A period lasts more than 7 days
- There is severe pain during periods
- There is bleeding between periods
- The girl / woman gets sick or has a sudden onset of fever after using a tampon
- A period occurs more frequently than 21 days or less frequently than 45 days
- A girl / woman goes 3 months without a period after beginning menstruation
For more information, please see Menstruation and Menstrual Rehab
Menopause[edit | edit source]
This stage occurs at the end of the reproductive stage and is marked by the final menstrual period (FMP).[7] Exact timing of this period cannot be forecast and is pinpointed retrospectively when 12 months have passed without a period. The beginning of this transition is referred to as perimenopause and is triggered by the ovaries. The number of viable follicles drops to less than 1,000 and various signs and symptoms can begin to disrupt life.[8] This phase usually occurs between the ages of 45-58 years, but chronological age is not an accurate predictor. The STRAW+10 Staging Scale and common signs and symptoms are a far more useful predictor.[1]
After a female has had no menstrual cycles for 12 months, she enters the post-menopause stage.[1]
Schedule a medical check up if the woman:
- Has lengthening or skipped cycles (3 or more) before age 40
- Has a period that lasts more than 7 days
- Has unusual or severe pain during / between periods, or in post-menopause
- Has vaginal dryness, pain or blood when wiping after toileting
- Has difficulty sleeping and / or feels tired all the time
- Is experiencing decreased quality of life due to symptoms
- Is bleeding in post-menopause
For more information, please see Menopause.
Signs & Symptoms[edit | edit source]
Health care providers should be approaching menopause in the same way as menarche:[1]
- Monitoring for regular functioning
- Identifying issues early and treating accordingly
- Initiating conversations prior to transitions
- Encouraging clients to make ‘healthy choices’ within their capability
The following table summarises the signs associated with the transitions between puberty and menarche, and perimenopause and menopause.
| Puberty to Menarche | Perimenopause to Menopause |
|---|---|
| Secondary sex characteristics more pronounced | Vasomotor symptoms VMS (hot flashes/ night sweats) |
| Growth spurt | Vaginal dryness or Genitourinary Syndrome of Menopause (GSM) |
| Moodiness, short-tempered, emotional | Moodiness, short-tempered, emotional |
| Low energy / fatigue | Low energy / fatigue |
| Breast tenderness | Breast tenderness |
| Muscle aches | Muscle aches |
| Headaches | Headaches |
| Abdominal cramps | Abdominal cramps |
| Lower back pain | Lower back pain |
| Difficulty concentrating | Difficulty concentrating |
| Bloating, fluid retention | Bloating, fluid retention |
| Joint pain | Joint pain |
| Food cravings | Food cravings |
| Acne | Acne |
| Diarrhoea / constipation | Diarrhoea / constipation |
| Trouble sleeping | Trouble sleeping |
Common Medical Concerns during the Menopause Transition[edit | edit source]
- Primary Ovarian Insufficiency
- This is diagnosed when the ovaries stop working before the age of 40
- Genitourinary Syndrome in Menopause
- A condition in which the vaginal walls and the vulva become thin and easily break down. Symptoms often include: feeling hot and rough, bleeding when wiping after toileting and discomfort. This condition can be treated with topical creams.
- Diseases which increase in risk post-menopause:
- Cardiovascular disease
- Diabetes / obesity
- Osteoporosis
- Dementia
- Cancer, mainly breast and uterine
Regular Assessments[edit | edit source]
The following assessments should be included:[1]
- Blood work
- To establish baselines or to eliminate conditions such as thyroid disease and diabetes
- Test lipid levels every 2-3 years starting at the age of 40 (but more often if this is a risk of cardiovascular disease)
- ONLY if there is an indication, it might be recommended to test levels of calcium, vitamin D and hormones
- Height and weight
- ECG baseline
- Bone density scan is recommended from the age of 40 for a baseline, with a repeat every 5 years
- Assess for sleep / rest habits
- Assess for depression as its prevalence increases
- Pap test
- A mammogram is recommended from the age 40, with monitoring every 3 years
- Colonoscopy is recommended from the age of 55
- Encourage clients to track signs and symptoms to facilitate and direct care - this information should be reviewed regularly
Healthy Choices[edit | edit source]
- Exercise should include aerobic, strengthening and balance exercises
- Diet / nutrition for maintenance of health
- Do not smoke
- Moderate intake of alcohol
- Sleep 8 hours per day
- Relaxation techniques
Stages of Reproductive Aging Workshop (STRAW)[edit | edit source]
In 2001, the Stages of Reproductive Aging Workshop, otherwise known as STRAW, put together a standard for reproductive ageing. In 2011, STRAW was updated and modified to STRAW+10, which is the gold standard to identify stages within the sexual reproductive periods of a woman's lifespan.[1]
STRAW identifies the stages within the sexual reproductive periods of a woman's lifespan. It divides the adult female life into three broad phases: reproductive, menopausal transition, and post-menopause. These three phases include seven stages which centre on the final menstrual period, which is called Stage 0.[9]
STRAW divides the reproductive phase into Stages -5 (which is early), -4, (which is classified as peak), and -3 (which is late). Stage–3 is characterised by regular menstrual cycles, as well as increasing levels of follicle-stimulating hormone (FSH).[9]
The menopausal transition phase includes Stage -2 (early) and Stage -1 (late). During Stage –2, there is variability in the length of the menstrual cycle and increased levels of FSH. During Stage –1, there is the onset of skipped cycles / amenorrhea which lasts at least 60 days, as well as continued elevation of FSH.[9][10]
The post-menopause phase includes Stages +1 (early) and +2 (late).[9]
Please see Harlow et al.'s article: Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging for more information.
Links to Helpful Pages[edit | edit source]
Additional Resources[edit | edit source]
Videos:[edit | edit source]
- Menstrual cycle an NHS site video
- Dr Jen Gunter, TED Talks on What really happens to your body during Menopause?
- Video: Am I Normal? (Girls and Puberty)
- What is Menarche? Everything you need to know
Recommended for Providers[edit | edit source]
- Menopause Health Tool, Dr Jean Hailes
- Practitioner’s Toolkit, Monash University 2014
- Menopause Preparedness Fact Sheet, The Society of Women’s Health Research -October 2021.
Recommended for Clients and Parents / Guardians[edit | edit source]
- Menopause Fact Sheet, August 2019, Dr Jean Hailes, Women’s Health, Available in English, Arabic, Chinese (Simplified), Farsi, Greek, Hindi, Italian, Turkish and Vietnamese. (This project was funded by the Victorian Government)
- Menstrual Calendar, for tracking perimenopause phase, NAMS, 2015
- Red Hot Mamas
- The Vajenda
- The North American Menopause Society
- US Department of Health and Human Services
- Healthy Women
- Canadian Society of Obstetricians and Gynaecologists
- Menstruation Around the World
- Menopause Map is a great interactive tool to start with to personalise your journey.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 Piché S. Menarche to Menopause Course. Plus , 2022.
- ↑ Howard SR. Interpretation of reproductive hormones before, during and after the pubertal transition-Identifying health and disordered puberty. Clin Endocrinol (Oxf). 2021 Nov;95(5):702-715.
- ↑ Mendle J, Beltz AM, Carter R, Dorn LD. Understanding puberty and its measurement: ideas for research in a new generation. Journal of Research on Adolescence. 2019 Mar;29(1):82-95.
- ↑ Lacroix AE, Gondal H, Langaker MD. Physiology, menarche. InStatPearls [Internet] 2021 Mar 27. StatPearls Publishing.
- ↑ Kota AS, Ejaz S. Precocious puberty. InStatPearls [Internet] 2021 Jul 25. StatPearls publishing.
- ↑ 6.0 6.1 Gasner A, Rehman A. Primary amenorrhea. 2022 Mar 20. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 32119356.
- ↑ Talaulikar V. Menopause transition: Physiology and symptoms. Best Practice & Research Clinical Obstetrics & Gynaecology. 2022 Mar 16.
- ↑ Santoro N, Kravitz HM. The Disruptive Changes of Midlife: A Biopsychosocial Adventure. Obstetrics and Gynecology Clinics. 2018 Dec 1;45(4):xv-ii.
- ↑ 9.0 9.1 9.2 9.3 Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, Sherman S, Sluss PM, De Villiers TJ, STRAW+ 10 Collaborative Group. Executive summary of the Stages of Reproductive Aging Workshop+ 10: addressing the unfinished agenda of staging reproductive aging. The Journal of Clinical Endocrinology & Metabolism. 2012 Apr 1;97(4):1159-68.
- ↑ Woods NF, Mitchell ES, Coslov N, Richardson MK. Transitioning to the menopausal transition: a scoping review of research on the late reproductive stage in reproductive aging. Menopause. 2021 Apr 1;28(4):447-66.