Tackling Overprescription: Difference between revisions
Debbie Kenny (talk | contribs) mNo edit summary |
No edit summary |
||
| (131 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|Debbie Kenny]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
=='''Introduction'''== | =='''Introduction'''== | ||
[[File:Polypharmacy.jpeg|thumb|399x399px|Polypharmacy]] | |||
Over the last 30 years, people have been prescribed increasing number of medicines, in particular [[Medication and Older People|older people]]. The reasons are manifold and include: | |||
* A rise in [[multimorbidity]] and ageing populations | |||
* Use of [[Evidence Based Practice (EBP)|evidence-based practice]] | |||
* Greater expectations for outcomes from patients and their families<ref name=":0">NHS UK [https://www.sps.nhs.uk/articles/understanding-polypharmacy-overprescribing-and-deprescribing/ Understanding polypharmacy, overprescribing and deprescribing] Available:https://www.sps.nhs.uk/articles/understanding-polypharmacy-overprescribing-and-deprescribing/ (accessed 29.12.2022)</ref> | |||
The dangers of using multiple medicines include greater chances of: | |||
* Adverse drug experiences | |||
* Hospital admissions and health care costs | |||
* Non-adherence to medication<ref name=":0" /> | |||
Overprescribing may occur when: | |||
* A better alternative is available but not suggested | |||
* The drug is suitable for a condition but not the individual. | |||
* A condition alters and the medicine is no longer suitable/relevant. | |||
* The patient has ceased needing the medicine but it continues to be prescribed.<ref>BBC news [https://www.bbc.com/news/health-58639253 Overprescribing of medicines must stop, says government] Available:https://www.bbc.com/news/health-58639253 (accessed 28.12.2022)</ref> | |||
== Deprescribing == | |||
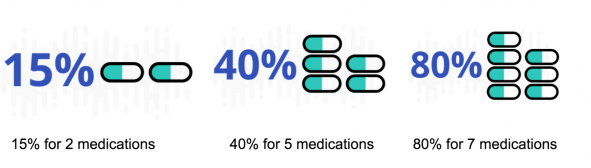
[[File:Drug interaction .png|591x591px|alt=|thumb|Chance of adverse reactions with multiple medications]] | |||
Deprescribing is the complicated process undertaken for the safe and effective withdrawal of inappropriate medication. A lot of of the evidence underpinning deprescribing is from observation, being based on the patient’s physical functioning, co-morbidities, preferences and lifestyle. | |||
Deprescribing: | |||
* Should be part of good prescribing, with re-evaluation of dosages periodically. | |||
* Involves health care professional direction and supervision with the same level of expertise and attention that prescribing entails <ref name=":6">Reeve E, Thompson W, Farrell B. Deprescribing: A narrative review of the evidence and practical recommendations for recognizing opportunities and taking action. European Journal of Internal Medicine.2017;38:3-11. | |||
</ref>. | |||
The following videos provides an easy to follow in-depth discussion regarding the concept (6 minutes){{#ev:youtube|zjUsqABxaEs}} | |||
== Overprescribing == | |||
[[File:Pill organising safe.png|thumb|384x384px|Medications: review regularly]] | |||
Overprescribing is when people are prescribed medicines: | |||
* They no longer need or want | |||
* The medicine has greater possible harmful than beneficial effects. | |||
* When a more effective alternative is not prescribed | |||
* Where the medicine is correct for a condition but not the individual. | |||
* When a condition alters and the medicine is no longer appropriate.<ref name=":0" /> | |||
The extensiveness of polypharmacy reported in literature differs, being between 10% to 90% according to the age group, definition used, healthcare and geographical setting of the study.<ref name=":1" /> | |||
== Patient Engagement == | |||
Medication reviews, joint decision-making and deprescribing rely on people becoming involved in decisions regarding their health care. Information to give patients and their carers about the medicines they are taking should be a priority, taking into account language, culture and level of health literacy.<ref>UK Government [https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1019475/good-for-you-good-for-us-good-for-everybody.pdf Good for you, good for us, good for everybody] Available:https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1019475/good-for-you-good-for-us-good-for-everybody.pdf (accessed 29.12.20220</ref> | |||
== Common Populations at Risk == | |||
[[File:Elderly woman.jpeg|thumb|Age: risk factor for over medicated.]] | |||
The use of multiple drugs is not always an indicator of poor drug treatment or overmedication<ref name=":12">Tamminga C. When Is Polypharmacy an Advantage?. American Journal of Psychiatry. 2011;168(7):663-663.</ref>. Appropriate medication depends on whether or not the advantages outweigh the disadvantages which is subjective to both the individual and their given condition(s). It can be very hard to predict the side-effects or clinical effects of a drug combination without testing it on the specific individual as the effects all very based on the individual's genome-specific pharmocokinetics<ref name=":12" />. | |||
At risk populations include: | |||
* [[Introduction to Frailty|Frail]] | |||
* [[Obesity]] | |||
* [[Older People - Patterns of Illness, Physiological Changes and Multiple Pathology|Elderly Populations]] | |||
* [[Mental Health]] Patients | |||
* [[Multimorbidity]] | |||
* Recent hospitalizations/major [[Surgery and General Anaesthetic|surgery]] | |||
* People seeing multiple doctors | |||
* [[Oncology and Palliative Care|Terminally ill patients]] | |||
Sex, educational level, and [[Smoking Cessation and Brief Intervention|smoking]] apparently appear not to be related to polypharmacy.<ref name=":1">FAQs clear [https://www.faqsclear.com/what-population-is-at-risk-for-polypharmacy/ What Population Is At Risk For Polypharmacy?] Available:https://www.faqsclear.com/what-population-is-at-risk-for-polypharmacy/ (accessed 29.11.2022)</ref> | |||
==The Potential Role of the Physiotherapist in Deprescribing== | |||
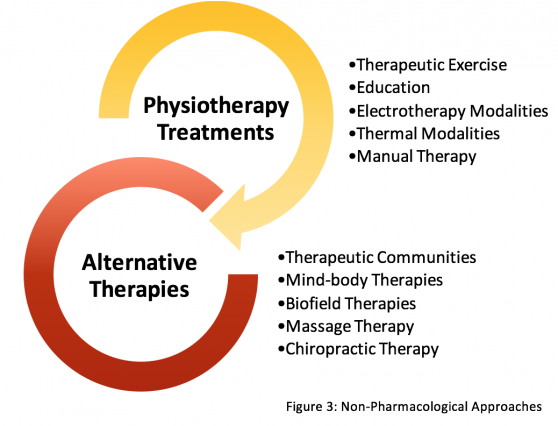
[[File:Non-pharma approaches.png|frameless|558x558px|alt=|right]] | |||
Available literature linking physiotherapy with deprescribing has focused only on the role of physiotherapy as a supplementary treatment for pain relief when reducing opioid dosage. | |||
General advice that may be given on the effects of medication. For example the general side effects of non-steroidal anti-inflammatory drugs (NSAIDs). While providing advice it should also be recommended that the patient should seek advice from a pharmacist or independent prescriber before altering any medication they currently take<ref name=":33">Chartered Society of Physiotherapy. Medicines, prescribing and physiotherapy [Internet]. CSP; 2016. Available from: <nowiki>http://www.csp.org.uk/publications/medicines-prescribing-physiotherapy-4th-edition</nowiki></ref>. | |||
'''Is patient taking their medication incorrectly?:''' If a non-prescriber physiotherapist notices a patient is not taking their medication correctly, they can refer the patient to the medications instructions and remind them how and when/ dose they should be taking their medication as prescribed<ref name=":33" />. This can also apply to medication devices, e.g. an inhaler, advice can be given how to use it according to guidelines. | |||
Adverse Effects:Physiotherapists can refer the patient back to the GP/pharmacists or can contact the GP directly providing information on their concerns re adverse effects <ref name=":3">Reznik J, Keren O, Morris J, Biran I. ''Pharmacology Handbook for Physiotherapists.'' Australia: Elsevier; 2016. | |||
</ref>. | |||
== Non-Pharmacological Interventions== | == Non-Pharmacological Interventions== | ||
Physiotherapists are reminded to stay within their scope of practice and always discuss any treatment options preferred as an alternative to drug therapies with the patient’s multidisciplinary team (MDT) or general practitioner (GP). Non-clinical readers are advised to discuss any preferable options with their GP before seeking treatment<ref>[[Non Pharmacological Interventions|Non-Pharmacological Approaches to Deprescription]]</ref>. See this page for more: [[Non Pharmacological Interventions|Non-Pharmacological Interventions]] | |||
== References == | |||
<references /> | |||
[[Category:Pharmacology]] | |||
[[Category:Falls]] | |||
[[Category:Interventions]] | |||
[[Category:Pharmacology for Older People]] | |||
[[Category:Older People/Geriatrics]] | |||
[[Category:Older People/Geriatrics - Interventions]] | |||
[[Category:Mental Health]] | |||
[[Category:Mental Health - Interventions]] | |||
[[Category:Cardiopulmonary]] | |||
[[Category:Cardiopulmonary - Interventions]] | |||
Latest revision as of 00:19, 20 February 2023
Introduction[edit | edit source]
Over the last 30 years, people have been prescribed increasing number of medicines, in particular older people. The reasons are manifold and include:
- A rise in multimorbidity and ageing populations
- Use of evidence-based practice
- Greater expectations for outcomes from patients and their families[1]
The dangers of using multiple medicines include greater chances of:
- Adverse drug experiences
- Hospital admissions and health care costs
- Non-adherence to medication[1]
Overprescribing may occur when:
- A better alternative is available but not suggested
- The drug is suitable for a condition but not the individual.
- A condition alters and the medicine is no longer suitable/relevant.
- The patient has ceased needing the medicine but it continues to be prescribed.[2]
Deprescribing[edit | edit source]
Deprescribing is the complicated process undertaken for the safe and effective withdrawal of inappropriate medication. A lot of of the evidence underpinning deprescribing is from observation, being based on the patient’s physical functioning, co-morbidities, preferences and lifestyle.
Deprescribing:
- Should be part of good prescribing, with re-evaluation of dosages periodically.
- Involves health care professional direction and supervision with the same level of expertise and attention that prescribing entails [3].
The following videos provides an easy to follow in-depth discussion regarding the concept (6 minutes)
Overprescribing[edit | edit source]
Overprescribing is when people are prescribed medicines:
- They no longer need or want
- The medicine has greater possible harmful than beneficial effects.
- When a more effective alternative is not prescribed
- Where the medicine is correct for a condition but not the individual.
- When a condition alters and the medicine is no longer appropriate.[1]
The extensiveness of polypharmacy reported in literature differs, being between 10% to 90% according to the age group, definition used, healthcare and geographical setting of the study.[4]
Patient Engagement[edit | edit source]
Medication reviews, joint decision-making and deprescribing rely on people becoming involved in decisions regarding their health care. Information to give patients and their carers about the medicines they are taking should be a priority, taking into account language, culture and level of health literacy.[5]
Common Populations at Risk[edit | edit source]
The use of multiple drugs is not always an indicator of poor drug treatment or overmedication[6]. Appropriate medication depends on whether or not the advantages outweigh the disadvantages which is subjective to both the individual and their given condition(s). It can be very hard to predict the side-effects or clinical effects of a drug combination without testing it on the specific individual as the effects all very based on the individual's genome-specific pharmocokinetics[6].
At risk populations include:
- Frail
- Obesity
- Elderly Populations
- Mental Health Patients
- Multimorbidity
- Recent hospitalizations/major surgery
- People seeing multiple doctors
- Terminally ill patients
Sex, educational level, and smoking apparently appear not to be related to polypharmacy.[4]
The Potential Role of the Physiotherapist in Deprescribing[edit | edit source]
Available literature linking physiotherapy with deprescribing has focused only on the role of physiotherapy as a supplementary treatment for pain relief when reducing opioid dosage.
General advice that may be given on the effects of medication. For example the general side effects of non-steroidal anti-inflammatory drugs (NSAIDs). While providing advice it should also be recommended that the patient should seek advice from a pharmacist or independent prescriber before altering any medication they currently take[7].
Is patient taking their medication incorrectly?: If a non-prescriber physiotherapist notices a patient is not taking their medication correctly, they can refer the patient to the medications instructions and remind them how and when/ dose they should be taking their medication as prescribed[7]. This can also apply to medication devices, e.g. an inhaler, advice can be given how to use it according to guidelines.
Adverse Effects:Physiotherapists can refer the patient back to the GP/pharmacists or can contact the GP directly providing information on their concerns re adverse effects [8].
Non-Pharmacological Interventions[edit | edit source]
Physiotherapists are reminded to stay within their scope of practice and always discuss any treatment options preferred as an alternative to drug therapies with the patient’s multidisciplinary team (MDT) or general practitioner (GP). Non-clinical readers are advised to discuss any preferable options with their GP before seeking treatment[9]. See this page for more: Non-Pharmacological Interventions
References[edit | edit source]
- ↑ 1.0 1.1 1.2 NHS UK Understanding polypharmacy, overprescribing and deprescribing Available:https://www.sps.nhs.uk/articles/understanding-polypharmacy-overprescribing-and-deprescribing/ (accessed 29.12.2022)
- ↑ BBC news Overprescribing of medicines must stop, says government Available:https://www.bbc.com/news/health-58639253 (accessed 28.12.2022)
- ↑ Reeve E, Thompson W, Farrell B. Deprescribing: A narrative review of the evidence and practical recommendations for recognizing opportunities and taking action. European Journal of Internal Medicine.2017;38:3-11.
- ↑ 4.0 4.1 FAQs clear What Population Is At Risk For Polypharmacy? Available:https://www.faqsclear.com/what-population-is-at-risk-for-polypharmacy/ (accessed 29.11.2022)
- ↑ UK Government Good for you, good for us, good for everybody Available:https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1019475/good-for-you-good-for-us-good-for-everybody.pdf (accessed 29.12.20220
- ↑ 6.0 6.1 Tamminga C. When Is Polypharmacy an Advantage?. American Journal of Psychiatry. 2011;168(7):663-663.
- ↑ 7.0 7.1 Chartered Society of Physiotherapy. Medicines, prescribing and physiotherapy [Internet]. CSP; 2016. Available from: http://www.csp.org.uk/publications/medicines-prescribing-physiotherapy-4th-edition
- ↑ Reznik J, Keren O, Morris J, Biran I. Pharmacology Handbook for Physiotherapists. Australia: Elsevier; 2016.
- ↑ Non-Pharmacological Approaches to Deprescription