Congestive Heart Failure: Difference between revisions
Kim Jackson (talk | contribs) m (Categorisation) |
(page link update and reference update) |
||
| (25 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Beau Lawrence|Beau Lawrence]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
CHF | == Introduction == | ||
[[File:Elevated JVP.jpeg|right|frameless]] | |||
Congestive [[Heart Failure|heart failure]] (CHF) refers to the clinical syndrome caused by inherited or acquired abnormalities of heart structure and function, causing a constellation of symptoms and signs that lead to decreased [[Quality of Life|quality]] and quantity of life<ref name=":1">Radiopedia [https://radiopaedia.org/articles/congestive-cardiac-failure?lang=us CHF] Available: https://radiopaedia.org/articles/congestive-cardiac-failure?lang=us<nowiki/>(accessed 2.6.2021)</ref>. | |||
Congestive heart failure (CHF) is a growing public health problem and is now the most common cause of hospitalizations in the U.S. among patients 65 years and [[Older People - An Introduction|older]]. The increasing prevalence of heart failure in the population is most likely secondary to the aging of the population, increased risk factors, better outcomes for [[Acute Coronary Syndrome|acute coronary syndrome]] survivors, and a reduction in mortality from other [[Chronic Disease|chronic conditions]].<ref name=":0">King KC, Goldstein S. [https://www.statpearls.com/ArticleLibrary/viewarticle/19880 Congestive Heart Failure and Pulmonary Edema]. StatPearls [Internet]. 2021 Jan 20.Available: https://www.statpearls.com/ArticleLibrary/viewarticle/19880<nowiki/>(accessed 2.6.2021)</ref> | |||
It is important to understand that congestive heart failure is a type of heart failure and not a totally different condition. | |||
# The failure of the left half causes a distinct set of symptoms and signs which is called left heart failure (see [[Heart Failure]]). | |||
# The failure of the right half causes a distinct set of features collectively called right heart failure (see [[Heart Failure]]). | |||
# The combination of the two is known as congestive heart failure.<ref name=":0" /> | |||
Image 1: A person with congestive heart failure with an exceedingly elevated jugular venous pressure external JVD (external jugular vein is marked by the arrow, JVD is measured by the internal jugular vein which can also be seen here). | |||
== Epidemiology == | |||
CHF is an epidemic spread across the entire world; it is estimated that 23 million people in the world are afflicted with CHF, approximately. | |||
* Risk factors for developing CHF include coronary artery disease, hypertension, [[diabetes]], [[obesity]] (BMI>30), and 65 years old or greater<ref>Komanduri S, Jadhao Y, Guduru SS, Cheriyath P, Wert Y. [https://www.tandfonline.com/doi/abs/10.1080/20009666.2016.1264696 Prevalence and risk factors of heart failure in the USA: NHANES 2013–2014 epidemiological follow-up study]. Journal of Community Hospital Internal Medicine Perspectives. 2017 Jan 2;7(1):15-20.</ref>. | |||
* The total cost of care for those with CHF is approximately $30.7 billion, and that value is expected to reach $69.8 billion by 2030. About 1% of people aged 55-64 and 17.4% of people 85 and older suffer from heart failure<ref>Dunlay SM, Pereira NL, Kushwaha SS. [https://www.sciencedirect.com/science/article/pii/S0025619614000536 Contemporary strategies in the diagnosis and management of heart failure]. InMayo Clinic Proceedings 2014 May 1 (Vol. 89, No. 5, pp. 662-676). Elsevier.</ref>. | |||
== Signs And Symptoms == | |||
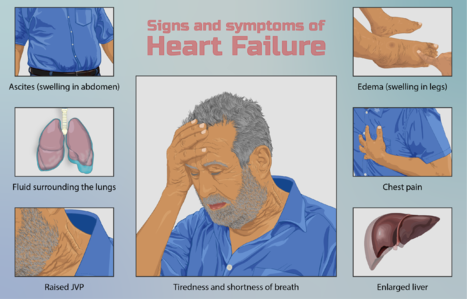
[[File:Depiction of a person suffering from heart failure.png|right|frameless|467x467px]] | |||
Symptoms of heart failure include those due to excess fluid accumulation ([[Dyspnoea|dyspnea]], orthopnea, [[Oedema Assessment|edema]], pain from [[Liver Disease|hepatic]] congestion, and abdominal distention from ascites) and those due to a reduction in cardiac output (fatigue, weakness) that is most pronounced with [[Physical Activity|physical activity]]. | |||
# Acute and subacute presentations (days to weeks) are characterized by shortness of breath at rest and/or with exertion, orthopnea, paroxysmal nocturnal dyspnea, and right upper quadrant discomfort due to acute hepatic congestion (right heart failure). Palpitations, with or without lightheadedness can occur if patient develops atrial or ventricular [[Pulse rate|tachyarrhythmias]] | |||
# Chronic presentations (months) differ in that fatigue, anorexia, abdominal distension, and [[Peripheral Edema|peripheral edema]] may be more pronounced than dyspnea. The anorexia is secondary to several factors eg poor perfusion of the splanchnic circulation, bowel edema, and nausea induced by hepatic congestion.<ref>Malik A, Brito D, Chhabra L. [https://www.ncbi.nlm.nih.gov/books/NBK430873/ Congestive Heart Failure] (CHF). StatPearls [Internet]. 2020 Jun 7. Available: https://www.ncbi.nlm.nih.gov/books/NBK430873/ (accessed 2.6.2021)</ref> | |||
== Physiotherapy Management == | |||
[[File:Treadmill walk.jpg|right|frameless|532x532px]] | |||
Physiotherapy is important in the management of heart failure. The cornerstone of physiotherapy management is [[Cardiac Rehabilitation|cardiac rehabilitation]], see link. In patients undergoing heart surgery, physiotherapy can also help with recovery after surgery. | |||
Up until the late 1980s, exercise was considered unsafe for the patient with HF. It was unclear whether any benefit could be gained from rehabilitation, and concern also existed regarding patient safety, with the belief that additional myocardial stress would cause further harm. Since this time, considerable research has been completed and the evidence resoundingly suggests that exercise for this patient group is not only safe but also provides substantial physiological and psychological benefits. As such, exercise is now considered an integral component of the non pharmacological management of these patients. eg Patients who have a biventricular [[Cardiac Implantable Electronic Devices (CIEDs)|pacemaker]] implant are often cleared for [[Therapeutic Exercise|therapeutic exercise]]. | |||
Benefits include | |||
* Reducing the incidence of heart failure-related hospital re-admissions | |||
* [[Aerobic Exercise|Aerobic]] and [[Resistance exercises|resistance]] training have a significant effect of on peak oxygen consumption, and [[muscle]] strength<ref>Gomes-Neto M, Durães AR, Conceição LS, Roever L, Silva CM, Alves IG, Ellingsen Ø, Carvalho VO. [https://pubmed.ncbi.nlm.nih.gov/31345646/ Effect of combined aerobic and resistance training on peak oxygen consumption, muscle strength and health-related quality of life in patients with heart failure with reduced left ventricular ejection fraction: a systematic review and meta-analysis.] International journal of cardiology. 2019 Oct 15;293:165-75.</ref>[[Heart Failure|.]] | |||
* Improving the well-being and quality of life for patients. | |||
* Modified group-based High-intensity aerobic interval training (HIAIT) intervention showed more considerable improvement as compared to moderate-intensity continuous training (MICT) in the rehabilitation of patients with chronic heart failure (CHF). <ref>MEDICA EM. [https://pubmed.ncbi.nlm.nih.gov/31976639/ Group-based cardiac rehabilitation interventions. A challenge for physical and rehabilitation medicine physicians: a randomized controlled trial.] European Journal of Physical and Rehabilitation Medicine. 2020 Jan 23.</ref> | |||
== Treatment == | |||
Treatment involves a multidisciplinary team and incorporates lifestyle, allied health, pharmacological, and even surgical therapies, often specific to the underlying etiology . General principles include: | |||
# Treatment of comorbidities and complications (e.g. [[obesity]], [[hypertension]], [[depression]]). | |||
# Lifestyle interventions: education, [[Smoking Cessation and Brief Intervention|cessation of smoking]] and [[Alcoholism|alcohol consumption]], increase in isotonic exercise, improve [[Nutrition|diet]], [[Adherence to Home Exercise Programs|home exercise program]] and [[Therapeutic Exercise|exercise]].<ref name=":1" /> | |||
# Pharmacotherapy ([[Beta-Blockers|Beta-blockers]], [[ACE Inhibitors: Congestive Heart Failure|ACE inhibitors]], [[Glycosides and Congestive Heart Failure|glycosides]], and [[Diuretics in the Treatment of Hypertension|diuretics]] are the key medications used for managing congestive heart failure through regulating [[Renal Rehabilitation|renal]] function and the [[Sympathetic Nervous System|sympathetic]] [[Introduction to Neuroanatomy|nervous system]]. For more information on medications used to manage CHF see [[Congestive Heart Failure - Pharmacotherapy|here)]] | |||
== Prognosis == | |||
[[File:Palliative care.jpg|right|frameless]] | |||
The diagnosis of heart failure alone can be associated with a mortality rate greater than many cancers. Despite advances made in heart failure treatments, the prognosis of the condition worsens over time, resulting in frequent hospital admissions and premature death<ref name=":0" />. Prognosis remains poor | |||
* 30-40% of patients dying within 1 year, and up to 70% dying within 5 years <ref name=":1" /> | |||
* Worse for heart failure patients who are hospitalized. Heart failure patients commonly require repeat hospitalizations and develop an intolerance for standard treatments as the disease progresses. Data from U.S.<ref name=":0" /> | |||
Below is a short video on CHF> | |||
{{#ev:youtube|https://www.youtube.com/watch?v=b3OHSA7Tz7U|width}}<ref>Alila Medical Media Congestive Heart Failure: Left-sided vs Right-sided, Systolic vs Diastolic, Animation Available from: https://www.youtube.com/watch?v=b3OHSA7Tz7U (last accessed 16.6.2019)</ref> | |||
== References == | |||
<references /> | <references /> | ||
[[Category:Cardiopulmonary]] | [[Category:Cardiopulmonary]] | ||
[[Category:Cardiovascular Disease]] | [[Category:Cardiovascular Disease]] | ||
[[Category:Cardiovascular Conditions | [[Category:Cardiovascular Disease - Conditions]] | ||
Latest revision as of 06:59, 8 February 2023
Introduction[edit | edit source]
Congestive heart failure (CHF) refers to the clinical syndrome caused by inherited or acquired abnormalities of heart structure and function, causing a constellation of symptoms and signs that lead to decreased quality and quantity of life[1].
Congestive heart failure (CHF) is a growing public health problem and is now the most common cause of hospitalizations in the U.S. among patients 65 years and older. The increasing prevalence of heart failure in the population is most likely secondary to the aging of the population, increased risk factors, better outcomes for acute coronary syndrome survivors, and a reduction in mortality from other chronic conditions.[2]
It is important to understand that congestive heart failure is a type of heart failure and not a totally different condition.
- The failure of the left half causes a distinct set of symptoms and signs which is called left heart failure (see Heart Failure).
- The failure of the right half causes a distinct set of features collectively called right heart failure (see Heart Failure).
- The combination of the two is known as congestive heart failure.[2]
Image 1: A person with congestive heart failure with an exceedingly elevated jugular venous pressure external JVD (external jugular vein is marked by the arrow, JVD is measured by the internal jugular vein which can also be seen here).
Epidemiology[edit | edit source]
CHF is an epidemic spread across the entire world; it is estimated that 23 million people in the world are afflicted with CHF, approximately.
- Risk factors for developing CHF include coronary artery disease, hypertension, diabetes, obesity (BMI>30), and 65 years old or greater[3].
- The total cost of care for those with CHF is approximately $30.7 billion, and that value is expected to reach $69.8 billion by 2030. About 1% of people aged 55-64 and 17.4% of people 85 and older suffer from heart failure[4].
Signs And Symptoms[edit | edit source]
Symptoms of heart failure include those due to excess fluid accumulation (dyspnea, orthopnea, edema, pain from hepatic congestion, and abdominal distention from ascites) and those due to a reduction in cardiac output (fatigue, weakness) that is most pronounced with physical activity.
- Acute and subacute presentations (days to weeks) are characterized by shortness of breath at rest and/or with exertion, orthopnea, paroxysmal nocturnal dyspnea, and right upper quadrant discomfort due to acute hepatic congestion (right heart failure). Palpitations, with or without lightheadedness can occur if patient develops atrial or ventricular tachyarrhythmias
- Chronic presentations (months) differ in that fatigue, anorexia, abdominal distension, and peripheral edema may be more pronounced than dyspnea. The anorexia is secondary to several factors eg poor perfusion of the splanchnic circulation, bowel edema, and nausea induced by hepatic congestion.[5]
Physiotherapy Management[edit | edit source]
Physiotherapy is important in the management of heart failure. The cornerstone of physiotherapy management is cardiac rehabilitation, see link. In patients undergoing heart surgery, physiotherapy can also help with recovery after surgery.
Up until the late 1980s, exercise was considered unsafe for the patient with HF. It was unclear whether any benefit could be gained from rehabilitation, and concern also existed regarding patient safety, with the belief that additional myocardial stress would cause further harm. Since this time, considerable research has been completed and the evidence resoundingly suggests that exercise for this patient group is not only safe but also provides substantial physiological and psychological benefits. As such, exercise is now considered an integral component of the non pharmacological management of these patients. eg Patients who have a biventricular pacemaker implant are often cleared for therapeutic exercise.
Benefits include
- Reducing the incidence of heart failure-related hospital re-admissions
- Aerobic and resistance training have a significant effect of on peak oxygen consumption, and muscle strength[6].
- Improving the well-being and quality of life for patients.
- Modified group-based High-intensity aerobic interval training (HIAIT) intervention showed more considerable improvement as compared to moderate-intensity continuous training (MICT) in the rehabilitation of patients with chronic heart failure (CHF). [7]
Treatment[edit | edit source]
Treatment involves a multidisciplinary team and incorporates lifestyle, allied health, pharmacological, and even surgical therapies, often specific to the underlying etiology . General principles include:
- Treatment of comorbidities and complications (e.g. obesity, hypertension, depression).
- Lifestyle interventions: education, cessation of smoking and alcohol consumption, increase in isotonic exercise, improve diet, home exercise program and exercise.[1]
- Pharmacotherapy (Beta-blockers, ACE inhibitors, glycosides, and diuretics are the key medications used for managing congestive heart failure through regulating renal function and the sympathetic nervous system. For more information on medications used to manage CHF see here)
Prognosis[edit | edit source]
The diagnosis of heart failure alone can be associated with a mortality rate greater than many cancers. Despite advances made in heart failure treatments, the prognosis of the condition worsens over time, resulting in frequent hospital admissions and premature death[2]. Prognosis remains poor
- 30-40% of patients dying within 1 year, and up to 70% dying within 5 years [1]
- Worse for heart failure patients who are hospitalized. Heart failure patients commonly require repeat hospitalizations and develop an intolerance for standard treatments as the disease progresses. Data from U.S.[2]
Below is a short video on CHF>
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Radiopedia CHF Available: https://radiopaedia.org/articles/congestive-cardiac-failure?lang=us(accessed 2.6.2021)
- ↑ 2.0 2.1 2.2 2.3 King KC, Goldstein S. Congestive Heart Failure and Pulmonary Edema. StatPearls [Internet]. 2021 Jan 20.Available: https://www.statpearls.com/ArticleLibrary/viewarticle/19880(accessed 2.6.2021)
- ↑ Komanduri S, Jadhao Y, Guduru SS, Cheriyath P, Wert Y. Prevalence and risk factors of heart failure in the USA: NHANES 2013–2014 epidemiological follow-up study. Journal of Community Hospital Internal Medicine Perspectives. 2017 Jan 2;7(1):15-20.
- ↑ Dunlay SM, Pereira NL, Kushwaha SS. Contemporary strategies in the diagnosis and management of heart failure. InMayo Clinic Proceedings 2014 May 1 (Vol. 89, No. 5, pp. 662-676). Elsevier.
- ↑ Malik A, Brito D, Chhabra L. Congestive Heart Failure (CHF). StatPearls [Internet]. 2020 Jun 7. Available: https://www.ncbi.nlm.nih.gov/books/NBK430873/ (accessed 2.6.2021)
- ↑ Gomes-Neto M, Durães AR, Conceição LS, Roever L, Silva CM, Alves IG, Ellingsen Ø, Carvalho VO. Effect of combined aerobic and resistance training on peak oxygen consumption, muscle strength and health-related quality of life in patients with heart failure with reduced left ventricular ejection fraction: a systematic review and meta-analysis. International journal of cardiology. 2019 Oct 15;293:165-75.
- ↑ MEDICA EM. Group-based cardiac rehabilitation interventions. A challenge for physical and rehabilitation medicine physicians: a randomized controlled trial. European Journal of Physical and Rehabilitation Medicine. 2020 Jan 23.
- ↑ Alila Medical Media Congestive Heart Failure: Left-sided vs Right-sided, Systolic vs Diastolic, Animation Available from: https://www.youtube.com/watch?v=b3OHSA7Tz7U (last accessed 16.6.2019)