Common Women's Pelvic Health Conditions: Difference between revisions
No edit summary |
No edit summary |
||
| (32 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Jess Bell|Jess Bell]] based on the course by [https://members.physio-pedia.com/course_tutor/ibukun-afolabi/ Ibukun Afolabi]<br> | <div class="editorbox"> '''Original Editor '''- [[User:Jess Bell|Jess Bell]] based on the course by [https://members.physio-pedia.com/course_tutor/ibukun-afolabi/ Ibukun Afolabi]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
Women may seek help from pelvic health physiotherapists for [[Overview and Introduction to Women's Pelvic Health| | Women may seek help from pelvic health physiotherapists for [[Overview and Introduction to Women's Pelvic Health|many reasons]]. This page will explore some common conditions that pelvic health physiotherapists might encounter in clinical practice. Evaluation and management strategies are discussed [[Physiotherapy Assessment and Treatment of the Pelvic Floor|here]]. | ||
== Pelvic Floor States == | |||
The pelvic floor muscles work [[Overview of Female Pelvic Floor Muscle Anatomy and Physiology#The Nine S.27s of Pelvic Floor Muscle Physiology|synergistically]] with the diaphragm by contracting and lengthening with every breath. The amount of movement depends on the size of the breath.<ref name=":0">Afolabi I. Common Women's Pelvic Health Conditions Course. | The pelvic floor muscles work [[Overview of Female Pelvic Floor Muscle Anatomy and Physiology#The Nine S.27s of Pelvic Floor Muscle Physiology|synergistically]] with the diaphragm by contracting and lengthening with every breath. The amount of movement depends on the size of the breath.<ref name=":0">Afolabi I. Common Women's Pelvic Health Conditions Course. Plus , 2022.</ref> However, like any skeletal muscle, the pelvic floor muscles can become tight. Reduced range of motion in the pelvic floor can affect bowel and bladder function, sexual pleasure, core support, and athletic performance.<ref name=":0" /> | ||
There are two extremes of pelvic floor states:<ref name=":0" /> | There are two extremes of pelvic floor states:<ref name=":0" /> | ||
'''1. Underactive Pelvic Floor''' | |||
* | * “Low in position, lax, unsupportive, hypotonic, long or lengthened, disconnected”<ref name=":0" /> | ||
In reality, these states exist along a continuum. Some women may experience elements of both overactivity and underactivity and, thus, have a mixed pelvic floor.<ref name=":0" /> Signs associated with underactive and overactive pelvic floors are summarised in Table 1. | * Characterised “by an inability to meet the demands of maintaining continence or pelvic organ support due to deficits in power, endurance, or correctly timed coordination of contraction.”<ref name=":1">Siracusa C, Gray A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7641036/ Pelvic floor considerations in COVID-19]. J Womens Health Phys Therap. 2020;44(4):144-51.</ref> | ||
* The pelvic floor muscles:<ref name=":0" /> | |||
** May be sluggish | |||
** May or may not have tender areas | |||
** Will have difficulty lifting and contracting | |||
** Will likely be weak | |||
'''2. Overactive Pelvic Floor''' | |||
* "High, tight, stiff/rigid, short, hypertonic, non-relaxing”<ref name=":0" /> | |||
* Characterised “by an inability to fully relax and lengthen. Most frequently, the overactive pelvic floor is associated with symptoms of pelvic pain, urinary frequency/urgency, and defecatory dysfunction.”<ref name=":1" /> | |||
* The overactive pelvic floor:<ref name=":0" /> | |||
** May be tender to the touch | |||
** May possibly be painful or sensitive | |||
** Might have difficulty lifting and contracting | |||
** Is often considered weak | |||
In reality, these pelvic floor states exist along a continuum. Some women may experience elements of both overactivity and underactivity and, thus, have a mixed pelvic floor.<ref name=":0" /> Signs associated with underactive and overactive pelvic floors are summarised in Table 1. | |||
{| class="wikitable" | {| class="wikitable" | ||
|+Table 1. Signs associated with underactive or overactive pelvic floor muscles<ref name=":0" /> | |+Table 1. Signs associated with underactive or overactive pelvic floor muscles<ref name=":0" /> | ||
| Line 44: | Line 45: | ||
|- | |- | ||
|Pelvic floor contractions feel weak | |Pelvic floor contractions feel weak | ||
|Pelvic floor contractions | |Pelvic floor contractions feel weak or low endurance | ||
|- | |- | ||
|Tampons or menstrual cups may fall out | |Tampons or menstrual cups may fall out | ||
| Line 52: | Line 53: | ||
|Pain with penetration | |Pain with penetration | ||
|- | |- | ||
|Feeling of heaviness | |Feeling of heaviness, pressure or dragging | ||
|Pain during or after intercourse | |Pain during or after intercourse | ||
|- | |- | ||
|Feeling of sitting on an egg or a golf ball between legs | |Feeling of sitting on an egg or with a golf ball between legs | ||
|Persistent pain in pelvic, abdominal, groin, or genital region | |Persistent pain in pelvic, abdominal, groin, or genital region | ||
|- | |- | ||
| Line 73: | Line 74: | ||
|Chronic constipation | |Chronic constipation | ||
|} | |} | ||
Because there is some crossover in symptoms, it is essential to perform a careful initial assessment and ongoing evaluation to select the correct treatment | Because there is some crossover in symptoms, it is essential to perform a careful initial [[Physiotherapy Assessment and Treatment of the Pelvic Floor|assessment]] and ongoing evaluation to select the correct treatment. | ||
== Common Pelvic Health Conditions == | == Common Pelvic Health Conditions == | ||
Pelvic floor conditions | Pelvic floor conditions might be categorised as:<ref name=":0" /> | ||
* Pressure conditions | * Pressure conditions | ||
| Line 93: | Line 94: | ||
* Stress UI:<ref name=":2">Sountoulidis P. Stress urinary incontinence [Internet]. ICS Committees. 2018 [cited 2 January 2022]. Available from: https://www.ics.org/committees/standardisation/terminologydiscussions/sui </ref> | * Stress UI:<ref name=":2">Sountoulidis P. Stress urinary incontinence [Internet]. ICS Committees. 2018 [cited 2 January 2022]. Available from: https://www.ics.org/committees/standardisation/terminologydiscussions/sui </ref> | ||
** An involuntary loss of urine that occurs during movements / activities | ** An involuntary loss of urine that occurs during movements / activities, such as coughing, sneezing, laughing, running, heavy lifting, that increase abdominal pressure (i.e. stress) on the bladder | ||
* Urge UI:<ref name=":2" /> | * Urge UI:<ref name=":2" /> | ||
** An unintentional loss of urine | ** An unintentional loss of urine that can occur when the bladder muscle contracts | ||
** There is often a sense of urgency | ** There is often a sense of urgency | ||
* Mixed UI:<ref>Sung VW, Borello-France D, Newman DK, Richter HE, Lukacz ES, Moalli P et al. [https://jamanetwork.com/journals/jama/article-abstract/2749872 Effect of behavioral and pelvic floor muscle therapy combined with surgery vs surgery alone on incontinence symptoms among women with mixed urinary incontinence: The ESTEEM randomized clinical trial]. JAMA. 2019;322(11):1066-76. </ref> | * Mixed UI:<ref>Sung VW, Borello-France D, Newman DK, Richter HE, Lukacz ES, Moalli P et al. [https://jamanetwork.com/journals/jama/article-abstract/2749872 Effect of behavioral and pelvic floor muscle therapy combined with surgery vs surgery alone on incontinence symptoms among women with mixed urinary incontinence: The ESTEEM randomized clinical trial]. JAMA. 2019;322(11):1066-76. </ref> | ||
** An individual has both stress and | ** An individual has both stress and urge UI | ||
* Overflow incontinence:<ref>Mangir N, Chapple C. [https://wchh.onlinelibrary.wiley.com/doi/full/10.1002/tre.740 Management of urinary incontinence in men]. Trends in Urology and Men's Health. 2020;11(2):18-22.</ref> | * Overflow incontinence:<ref>Mangir N, Chapple C. [https://wchh.onlinelibrary.wiley.com/doi/full/10.1002/tre.740 Management of urinary incontinence in men]. Trends in Urology and Men's Health. 2020;11(2):18-22.</ref> | ||
** | ** UI occurs when the bladder is excessively full, with no cause identified | ||
* Functional incontinence:<ref>Khandelwal C, Kistler C. [https://www.aafp.org/afp/2013/0415/p543.html Diagnosis of urinary incontinence]. Am Fam Physician. 2013;87(8):543-50.</ref> | * Functional incontinence:<ref>Khandelwal C, Kistler C. [https://www.aafp.org/afp/2013/0415/p543.html Diagnosis of urinary incontinence]. Am Fam Physician. 2013;87(8):543-50.</ref> | ||
** | ** Occurs when there are cognitive, functional, or mobility issues that affect an individual’s ability to use the toilet | ||
** No bladder / neurological causes | ** No bladder / neurological causes | ||
** Also referred to as “toileting difficulty” | ** Also referred to as “toileting difficulty” | ||
The following video provides a detailed discussion of incontinence. {{#ev:youtube|vsLBApSlPMo}}<ref>Osmosis. Urinary incontinence - causes, symptoms, diagnosis, treatment, pathology. Available from: https://www.youtube.com/watch?v=vsLBApSlPMo [last accessed 3/1/2022]</ref> | |||
The prevalence of UI varies widely in different studies.<ref>Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019;22(3):217-22. </ref> It is estimated that between one in two and one in three women experience incontinence.<ref>Minassian VA, Stewart WF, Wood GC. Urinary incontinence in women: variation in prevalence estimates and risk factors. Obstet Gynecol. 2008;111(2 Pt 1):324-31.</ref><ref>NHS England. [https://www.england.nhs.uk/wp-content/uploads/2018/07/excellence-in-continence-care.pdf Excellence in continence care: Practical guidance for commissioners, and leaders in health and social care]. Leeds: NHS England, 2018.</ref> Yet many individuals do not seek out treatment.<ref name=":0" /> Lukacz et al.<ref>Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary Incontinence in Women: A Review. JAMA. 2017;318(16):1592-1604.</ref> found that only 25 percent of affected women receive treatment. Possible reasons for not seeking care include:<ref name=":0" /> | The prevalence of UI varies widely in different studies.<ref>Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019;22(3):217-22. </ref> It is estimated that between one in two and one in three women experience incontinence.<ref>Minassian VA, Stewart WF, Wood GC. Urinary incontinence in women: variation in prevalence estimates and risk factors. Obstet Gynecol. 2008;111(2 Pt 1):324-31.</ref><ref>NHS England. [https://www.england.nhs.uk/wp-content/uploads/2018/07/excellence-in-continence-care.pdf Excellence in continence care: Practical guidance for commissioners, and leaders in health and social care]. Leeds: NHS England, 2018.</ref> Yet many individuals do not seek out treatment.<ref name=":0" /> Lukacz et al.<ref>Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary Incontinence in Women: A Review. JAMA. 2017;318(16):1592-1604.</ref> found that only 25 percent of affected women receive treatment. Possible reasons for not seeking care include:<ref name=":0" /> | ||
| Line 118: | Line 122: | ||
* Abnormal voiding patterns | * Abnormal voiding patterns | ||
* Uncoordinated inner core system | * Uncoordinated inner core system | ||
* Behavioural factors (going “just in case” | * Behavioural factors (e.g. going “just in case”) | ||
=== Other Bladder Conditions === | === Other Bladder Conditions === | ||
| Line 133: | Line 137: | ||
* Pain with urination | * Pain with urination | ||
See [[Overview and Introduction to Women's Pelvic Health#Who Do Women.E2.80.99s Pelvic Health Physiotherapists Work With.3F|here]] for more information on these conditions. | |||
=== Faecal Incontinence === | === Faecal Incontinence === | ||
Faecal incontinence is an involuntary loss of gas or stool (ranging from staining / smearing on underwear to stool).<ref name=":0" /> Other bowel | Faecal incontinence is an involuntary loss of gas or stool (ranging from staining / smearing on underwear to full loss of control of stool).<ref name=":0" /> One in eight women experience faecal incontinence<ref name=":0" /> and it is often caused by obstetric anal sphincter injuries (OASIS) that occur during childbirth.<ref name=":0" /> OASIS injuries are also referred to as '''third''' or '''fourth''' degree perineal tears:<ref name=":7">Darmody E, Bradshaw C, Atkinson S Dr. [https://www.sciencedirect.com/science/article/pii/S0266613820301923?via%3Dihub Women's experience of obstetric anal sphincter injury following childbirth: An integrated review]. Midwifery. 2020;91:102820.</ref> | ||
* First degree tears affect the skin of the perineum, but these tears tend to heal naturally and do not need to be sutured | |||
* Second degree tears involve both the skin and muscle of the perineum | |||
* Third degree tears affect the anal sphincter complex | |||
* Fourth degree tears extend to the anal mucosa | |||
The incidence of OASIS injuries following vaginal deliveries is said to be increasing.<ref name=":7" /> In addition to faecal incontinence, an OASIS injury can lead to:<ref name=":7" /> | |||
* Pain | |||
* Urinary incontinence | |||
* Sexual dysfunction | |||
* Depression / anxiety | |||
* Decreased emotional health and quality of life | |||
=== Other Bowel Dysfunctions === | |||
Other bowel issues that women may experience include:<ref name=":0" /> | |||
* [[Constipation|Chronic constipation]] | |||
* Haemorrhoids | |||
* [[Irritable Bowel Syndrome|Irritable bowel syndrome]] | |||
* Defecation dyssynergia (i.e. incoordination during the process of defecation)<ref>Rao SS, Patcharatrakul T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4930297/ Diagnosis and treatment of dyssynergic defecation]. J Neurogastroenterol Motil. 2016;22(3):423-35. </ref> | |||
== Pelvic Organ Prolapse == | == Pelvic Organ Prolapse == | ||
Pelvic organ prolapse occurs when the pelvic organs (i.e. the uterus, rectum and bladder in women) move from their optimal position.<ref name=":0" /><ref>The American College of Obstetricians and Gynecologists and the American Urogynecologic Society INTERIM UPDATE: This Practice Bulletin is updated as highlighted to reflect the US Food and Drug Administration order to stop the sale of transvaginal synthetic mesh products for the repair of pelvic organ prolapse. [https://journals.lww.com/fpmrs/Fulltext/2019/11000/Pelvic_Organ_Prolapse.1.aspx Pelvic Organ Prolapse]. Female Pelvic Medicine & Reconstructive Surgery. 2019;25(6):397-408. </ref> | [[File:Uterine Prolapse shutterstock 1878468127.jpg|thumb|550x550px|Figure 1. Uterine prolapse. ]] | ||
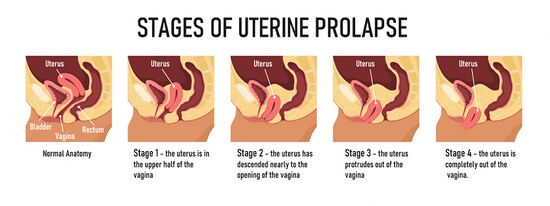
Pelvic organ prolapse (POP) occurs when the pelvic organs (i.e. the uterus, rectum and bladder in women) move from their optimal position. Figure 1 illustrates the stages of a uterine prolapse.<ref name=":0" /><ref>The American College of Obstetricians and Gynecologists and the American Urogynecologic Society INTERIM UPDATE: This Practice Bulletin is updated as highlighted to reflect the US Food and Drug Administration order to stop the sale of transvaginal synthetic mesh products for the repair of pelvic organ prolapse. [https://journals.lww.com/fpmrs/Fulltext/2019/11000/Pelvic_Organ_Prolapse.1.aspx Pelvic Organ Prolapse]. Female Pelvic Medicine & Reconstructive Surgery. 2019;25(6):397-408. </ref> | |||
Symptoms include:<ref name=":0" /><ref>Crowle A, Harley C. [https://eprints.whiterose.ac.uk/152560/ Development of a biotensegrity focused therapy for the treatment of pelvic organ prolapse: A retrospective case series]. J Bodyw Mov Ther. 2020;24(1):115-25. </ref> | Symptoms include:<ref name=":0" /><ref>Crowle A, Harley C. [https://eprints.whiterose.ac.uk/152560/ Development of a biotensegrity focused therapy for the treatment of pelvic organ prolapse: A retrospective case series]. J Bodyw Mov Ther. 2020;24(1):115-25. </ref> | ||
| Line 149: | Line 175: | ||
* Discomfort during intercourse | * Discomfort during intercourse | ||
Physical signs might include a bulge or protrusion at the entrance to the vagina.<ref name=":0" /> | Physical signs might include a bulge or protrusion at the entrance to the vagina.<ref name=":0" /> In general, an individual’s symptoms are aggravated in positions where gravity acts on the body (e.g. standing, walking, lifting). Positions where gravity is eliminated (e.g. lying down) tend to be relieving.<ref name=":0" /> | ||
In general, an individual’s symptoms are aggravated in positions where gravity acts on the body (e.g. standing, walking, lifting). Positions where gravity is eliminated (e.g. lying down) tend to be relieving.<ref name=":0" /> | |||
POP is a subjective experience. Some clients may have a mild prolapse but experience severe symptoms, whereas others have a significant prolapse but report minimal or no symptoms.<ref name=":0" /><ref name=":3">Weintraub AY, Glinter H, Marcus-Braun N. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6968909/ Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic organ prolapse]. Int Braz J Urol. 2020;46(1):5-14. </ref> Diagnosis is made based on the clinical examination and subjective symptoms, such as:<ref name=":0" /> | POP is a subjective experience. Some clients may have a mild prolapse but experience severe symptoms, whereas others have a significant prolapse but report minimal or no symptoms.<ref name=":0" /><ref name=":3">Weintraub AY, Glinter H, Marcus-Braun N. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6968909/ Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic organ prolapse]. Int Braz J Urol. 2020;46(1):5-14. </ref> Diagnosis is made based on the clinical examination and subjective symptoms, such as:<ref name=":0" /> | ||
| Line 161: | Line 185: | ||
* Recurrent UTIs | * Recurrent UTIs | ||
According to the '''Biomechanical / Pelvic Support Model''', the pelvic floor holds up the pelvic organs. POP occurs when:<ref name=":0" /><ref name=":3" /> | |||
* Fascia and ligaments which suspend the organs in place become lax, tear or lose integrity | * Fascia and ligaments which suspend the organs in place become lax, tear or lose integrity | ||
* The pelvic organs, thus, lose suspensory support from above | * The pelvic organs, thus, lose suspensory support from above | ||
* If the pelvic floor muscles are compromised / weak, it can mean that there is a lack of pelvic support from below | * If the pelvic floor muscles are compromised / weak, it can mean that there is a lack of pelvic support from below | ||
* When combined with poorly managed pressures in the abdominal canister (i.e. the area from the diaphragm to the pelvic floor<ref>Emerich K, Reed O. [https://www.researchgate.net/publication/328948499_The_Role_of_the_Pelvic_Floor_in_Respiration_A_Multidisciplinary_Literature_Review The role of the pelvic floor in respiration: a multidisciplinary literature review]. Journal of Voice. 2018;34(2):243-9.</ref>), | * When combined with poorly managed pressures in the abdominal canister (i.e. the area from the diaphragm to the pelvic floor<ref>Emerich K, Reed O. [https://www.researchgate.net/publication/328948499_The_Role_of_the_Pelvic_Floor_in_Respiration_A_Multidisciplinary_Literature_Review The role of the pelvic floor in respiration: a multidisciplinary literature review]. Journal of Voice. 2018;34(2):243-9.</ref>), there can be descent of the pelvic organs | ||
* More significant prolapses can bulge / protrude from the vaginal opening | * More significant prolapses can bulge / protrude from the vaginal opening | ||
=== Levator Ani Muscle Avulsion === | === Levator Ani Muscle Avulsion === | ||
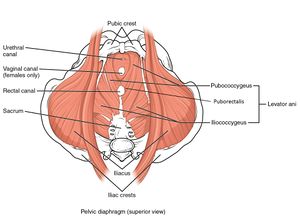
It is important to note that levator ani muscle avulsion may also be implicated in the development of POP. | [[File:Muscles of the Pelvic Floor.jpg|thumb|Figure 2. Levator ani muscle.]]It is important to note that levator ani muscle avulsion may also be implicated in the development of POP. This type of avulsion fracture occurs when the levator ani muscle (see Figure 2) is detached from its origins in the pubis.<ref name=":6" /> | ||
It occurs in 10 to 30 percent of vaginal deliveries<ref name=":6">Handa VL, Roem J, Blomquist JL, Dietz HP, Muñoz A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6592735/ Pelvic organ prolapse as a function of levator ani avulsion, hiatus size, and strength]. ''Am J Obstet Gynecol''. 2019;221(1):41.e1-41.e7. </ref> and is more common when forceps are used or when there is a prolonged pushing stage.<ref name=":0" /> | |||
=== Types of Prolapse === | === Types of Prolapse === | ||
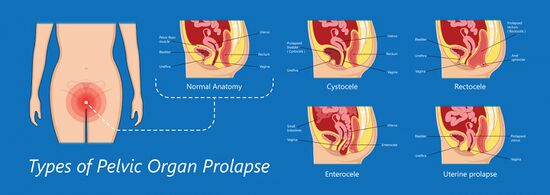
Traditionally POP has been categorised as:<ref name=":0" /> <ref>The American College of Obstetricians and Gynecologists. Surgery for pelvic organ prolapse. Available from: https://www.acog.org/womens-health/faqs/surgery-for-pelvic-organ-prolapse (accessed 2 January 2022).</ref> | Traditionally, POP has been categorised as:<ref name=":0" /> <ref>The American College of Obstetricians and Gynecologists. Surgery for pelvic organ prolapse. Available from: https://www.acog.org/womens-health/faqs/surgery-for-pelvic-organ-prolapse (accessed 2 January 2022).</ref> | ||
* Cystocele (prolapsed bladder) | * [[File:Types of prolapse shutterstock 1484216519.jpg|thumb|550x550px|Figure 3. Types of pelvic organ prolapse. |alt=]]Cystocele (prolapsed bladder) | ||
* Rectocele (prolapsed rectum) | * Rectocele (prolapsed rectum) | ||
* Uterine prolapse (prolapsed uterus) | * Uterine prolapse (prolapsed uterus) | ||
* Urethrocele (prolapsed urethra) | * Urethrocele (prolapsed urethra) | ||
* Enterocele (prolapsed intestine) | * Enterocele (prolapsed intestine) | ||
* Vaginal vault prolapse | * Vaginal vault prolapse (top of the vagina prolapses - only occurs after a hysterectomy) | ||
While these terms are still | While these terms are still used, health care professionals are increasingly moving towards a more anatomically-based classification system and are adopting terminology such as:<ref name=":4">Persu C, Chapple CR, Cauni V, Gutue S, Geavlete P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056425/ Pelvic Organ Prolapse Quantification System (POP-Q) - a new era in pelvic prolapse staging]. ''J Med Life''. 2011;4(1):75-81.</ref> | ||
* Anterior vaginal wall prolapse | * Anterior vaginal wall prolapse | ||
| Line 200: | Line 211: | ||
* Apical prolapse | * Apical prolapse | ||
Prolapse can be measured / graded using various systems | Prolapse can be measured / graded using various systems, but one of the most commonly used staging systems is the [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056425/ POP-Q (Pelvic Organ Prolapse Quantification System)]. The POP-Q uses a four-point system to determine the degree of prolapse:<ref name=":0" /><ref name=":4" /> | ||
* Stage 0 = no prolapse | * Stage 0 = no prolapse | ||
* Stage 1 = prolapse is 1cm above the vaginal opening or higher | * Stage 1 = prolapse is 1cm above the vaginal opening or higher | ||
* Stage 2 = prolapse is 1cm away from vaginal opening or has protruded up to 1cm out of the vagina | * Stage 2 = prolapse is 1cm away from the vaginal opening or has protruded up to 1cm out of the vagina | ||
* Stage 3 = prolapse protrudes more than 1cm out of the vagina | * Stage 3 = prolapse protrudes more than 1cm, but less than 2cm out of the vagina | ||
* Stage 4 = vaginal walls have completely everted, and the prolapse | * Stage 4 = the vaginal walls have completely everted, and the prolapse is maximally protruded | ||
Physiotherapy can be an effective treatment for individuals who have stage 1 to 3 prolapses.<ref name=":0" /> | Physiotherapy can be an effective treatment for individuals who have stage 1 to 3 prolapses.<ref name=":0" /> | ||
However, | However, it is important to note that a prolapse may be graded differently depending on factors such as the time of day, position of evaluation and method of evaluation. Therefore, physiotherapists may instead choose to rate a prolapse as mild, moderate, significant or severe.<ref name=":0" /> | ||
== Persistent Pelvic Pain == | |||
Persistent pelvic pain is defined as pain that has been present in the pelvic area for more than three months.<ref name=":5">The Mama's Physio. Persistent pelvic pain. Available from: https://themamasphysio.com/persistent-pelvic-pain/ (accessed 2 January 2022).</ref> Individuals may experience pain in their lower abdomen, pelvic floor, pelvic organs, hips, groin, buttocks, low back, coccyx, perineal region, vulvovaginal area, rectum, and genitalia.<ref name=":5" /> | |||
They may describe this pain as:<ref name=":5" /> | |||
* Constant or intermittent | |||
* Deep or superficial | |||
* Provoked by touch or present regardless of touch | |||
* Dull, sharp or burning | |||
* And the type of pain may change depending on the activity (e.g. urinating, sitting, intercourse) | |||
Types of pelvic pain that a pelvic floor physiotherapist may treat include:<ref name=":5" /> | Types of pelvic pain that a pelvic floor physiotherapist may treat include:<ref name=":5" /> | ||
* Dyspareunia (painful intercourse) | * [[Dyspareunia]] (painful intercourse) | ||
* Vaginismus (involuntary spasm of pelvic floor muscles | * Vaginismus (involuntary spasm of pelvic floor muscles when attempting penetration) | ||
* Vulvodynia (generalised pain | * Vulvodynia (generalised vulva pain) | ||
* Vestibulodynia ( | * Vestibulodynia / vulva vestibulitis (pain in the vestibule region of the vulva) | ||
* Clitroidynia ( | * Clitroidynia (clitoral region pain) | ||
* Coccydynia (pain | * Coccydynia (coccyx pain) | ||
* Dysmenorrhea (painful periods) | * [[Primary Dysmenorrhea|Dysmenorrhea]] (painful periods) | ||
* Endometriosis (pain | * [[Endometriosis]] (pain resulting from inflamed endometrial-like tissue, which is situated outside of the uterus) | ||
* Adenomyosis (pain | * Adenomyosis (pain resulting from inflamed endometrial-like tissue, which is situated inside the muscular lining of the uterus) | ||
* Painful bladder syndrome (hypersensitivity and inflammation | * Painful bladder syndrome (has a similar presentation to interstitial cystitis - causes hypersensitivity and inflammation of the bladder wall lining) | ||
* Levator ani syndrome or proctalgia fugax (tension | * Levator ani syndrome or proctalgia fugax (occurs when there is tension / spasm in one major pelvic floor muscle group) | ||
* Pudendal neuralgia or pudendal nerve entrapment (irritation | * [[Pudendal Neuralgia|Pudendal neuralgia]] or pudendal nerve entrapment (occurs when there is compression or irritation of the pudendal nerve) | ||
* Persistent genital arousal disorder ( | * Persistent genital arousal disorder (persistent or recurrent, unwanted or intrusive, distressing, abnormal sensations that are not associated with sexual interest. Also called genitopelvic dysesthesia) | ||
* Chronic pelvic pain syndrome | * Chronic pelvic pain syndrome (a descriptive diagnosis) | ||
* Other types of pain | * Other types of pain which can be caused by: hormonal changes, menopause, abdominal or pelvic surgery, autoimmune disorders, internal scar tissue, gut or bladder dysfunction, pelvic girdle pain, sacroiliac joint pain, labral tears of the hip, myofascial / connective tissue dysfunction, trauma, or hypertonicity and overactivity of pelvic floor muscles | ||
Additional information on some of these conditions is available [[Overview and Introduction to Women's Pelvic Health|here]]. In order to treat pelvic pain successfully, a physiotherapist needs to do a careful evaluation from a bio-psycho-social-spiritual and integrative framework. | Additional information on some of these conditions is available [[Overview and Introduction to Women's Pelvic Health|here]]. In order to treat pelvic pain successfully, a physiotherapist needs to do a careful evaluation from a bio-psycho-social-spiritual and integrative framework. More information on treatment is available [[Physiotherapy Assessment and Treatment of the Pelvic Floor|here]]. | ||
== References == | == References == | ||
<references /> | |||
[[Category:Plus Content]] | |||
[[Category:Course Pages]] | |||
[[Category:Pelvic Health]] | |||
[[Category:Womens Health]] | |||
Latest revision as of 00:51, 27 September 2022
Top Contributors - Jess Bell, Kim Jackson and Olajumoke Ogunleye
Introduction[edit | edit source]
Women may seek help from pelvic health physiotherapists for many reasons. This page will explore some common conditions that pelvic health physiotherapists might encounter in clinical practice. Evaluation and management strategies are discussed here.
Pelvic Floor States[edit | edit source]
The pelvic floor muscles work synergistically with the diaphragm by contracting and lengthening with every breath. The amount of movement depends on the size of the breath.[1] However, like any skeletal muscle, the pelvic floor muscles can become tight. Reduced range of motion in the pelvic floor can affect bowel and bladder function, sexual pleasure, core support, and athletic performance.[1]
There are two extremes of pelvic floor states:[1]
1. Underactive Pelvic Floor
- “Low in position, lax, unsupportive, hypotonic, long or lengthened, disconnected”[1]
- Characterised “by an inability to meet the demands of maintaining continence or pelvic organ support due to deficits in power, endurance, or correctly timed coordination of contraction.”[2]
- The pelvic floor muscles:[1]
- May be sluggish
- May or may not have tender areas
- Will have difficulty lifting and contracting
- Will likely be weak
2. Overactive Pelvic Floor
- "High, tight, stiff/rigid, short, hypertonic, non-relaxing”[1]
- Characterised “by an inability to fully relax and lengthen. Most frequently, the overactive pelvic floor is associated with symptoms of pelvic pain, urinary frequency/urgency, and defecatory dysfunction.”[2]
- The overactive pelvic floor:[1]
- May be tender to the touch
- May possibly be painful or sensitive
- Might have difficulty lifting and contracting
- Is often considered weak
In reality, these pelvic floor states exist along a continuum. Some women may experience elements of both overactivity and underactivity and, thus, have a mixed pelvic floor.[1] Signs associated with underactive and overactive pelvic floors are summarised in Table 1.
| Underactive pelvic floor | Overactive pelvic floor |
|---|---|
| Leaking with running, jumping, coughing, sneezing, laughing (i.e. anything that places pressure on the bladder) | Leaking with running, jumping, coughing, sneezing, laughing (i.e. anything that places pressure on the bladder) |
| Sudden urgency of bladder or bowels | Sudden urgency of bladder or bowels |
| Difficulty lifting the pelvic floor | Difficulty lifting the pelvic floor |
| Pelvic floor contractions feel weak | Pelvic floor contractions feel weak or low endurance |
| Tampons or menstrual cups may fall out | Difficulty starting to void or fully emptying the bladder |
| Sex might be described as "not feeling like it used to before kids" | Pain with penetration |
| Feeling of heaviness, pressure or dragging | Pain during or after intercourse |
| Feeling of sitting on an egg or with a golf ball between legs | Persistent pain in pelvic, abdominal, groin, or genital region |
| Noticing a protrusion at the entrance to the vagina | Ongoing low back, hip, or groin pain |
| Inability to make it to the bathroom in time | Trauma, tearing, or assisted delivery during childbirth |
| Inability to entirely empty bowels or bladder | Doing Kegels or holding Kegels makes symptoms worse |
| Sacroiliac joint pain, hip pain | Diagnosis of endometriosis, interstitial cystitis, vaginismus, dyspareunia |
| Chronic constipation | Chronic constipation |
Because there is some crossover in symptoms, it is essential to perform a careful initial assessment and ongoing evaluation to select the correct treatment.
Common Pelvic Health Conditions[edit | edit source]
Pelvic floor conditions might be categorised as:[1]
- Pressure conditions
- Pelvic support conditions
- Neuromuscular or myofascial conditions
- Pain conditions
- Mixed conditions
Common conditions are discussed below.
Incontinence[edit | edit source]
Incontinence is the uncontrolled loss of urine, gas, or stool of any amount.[1]
Urinary Incontinence[edit | edit source]
Urinary incontinence (UI) can be categorised as:
- Stress UI:[3]
- An involuntary loss of urine that occurs during movements / activities, such as coughing, sneezing, laughing, running, heavy lifting, that increase abdominal pressure (i.e. stress) on the bladder
- Urge UI:[3]
- An unintentional loss of urine that can occur when the bladder muscle contracts
- There is often a sense of urgency
- Mixed UI:[4]
- An individual has both stress and urge UI
- Overflow incontinence:[5]
- UI occurs when the bladder is excessively full, with no cause identified
- Functional incontinence:[6]
- Occurs when there are cognitive, functional, or mobility issues that affect an individual’s ability to use the toilet
- No bladder / neurological causes
- Also referred to as “toileting difficulty”
The following video provides a detailed discussion of incontinence.
The prevalence of UI varies widely in different studies.[8] It is estimated that between one in two and one in three women experience incontinence.[9][10] Yet many individuals do not seek out treatment.[1] Lukacz et al.[11] found that only 25 percent of affected women receive treatment. Possible reasons for not seeking care include:[1]
- Embarrassment
- Lack of awareness about treatment options
- A belief that it is a “normal” part of ageing
It is important to note that, rather than a diagnosis, incontinence is a symptom that is caused by underlying issues in the continence system. These issues include:[1]
- Poor pressure management
- Pelvic floor muscle dysfunction
- Postural or movement dysfunctions
- Abnormal voiding patterns
- Uncoordinated inner core system
- Behavioural factors (e.g. going “just in case”)
Other Bladder Conditions[edit | edit source]
Other bladder conditions include:[1]
- Frequency
- Urgency (i.e. overactive bladder)
- Voiding hesitancy
- Urinary retention
- Pain or burning with urination
- A sensation of incomplete emptying
- Frequent night-time voiding
- Recurrent urinary tract infections (UTI)
- Pain with urination
See here for more information on these conditions.
Faecal Incontinence[edit | edit source]
Faecal incontinence is an involuntary loss of gas or stool (ranging from staining / smearing on underwear to full loss of control of stool).[1] One in eight women experience faecal incontinence[1] and it is often caused by obstetric anal sphincter injuries (OASIS) that occur during childbirth.[1] OASIS injuries are also referred to as third or fourth degree perineal tears:[12]
- First degree tears affect the skin of the perineum, but these tears tend to heal naturally and do not need to be sutured
- Second degree tears involve both the skin and muscle of the perineum
- Third degree tears affect the anal sphincter complex
- Fourth degree tears extend to the anal mucosa
The incidence of OASIS injuries following vaginal deliveries is said to be increasing.[12] In addition to faecal incontinence, an OASIS injury can lead to:[12]
- Pain
- Urinary incontinence
- Sexual dysfunction
- Depression / anxiety
- Decreased emotional health and quality of life
Other Bowel Dysfunctions[edit | edit source]
Other bowel issues that women may experience include:[1]
- Chronic constipation
- Haemorrhoids
- Irritable bowel syndrome
- Defecation dyssynergia (i.e. incoordination during the process of defecation)[13]
Pelvic Organ Prolapse[edit | edit source]
Pelvic organ prolapse (POP) occurs when the pelvic organs (i.e. the uterus, rectum and bladder in women) move from their optimal position. Figure 1 illustrates the stages of a uterine prolapse.[1][14]
- A feeling of pressure / heaviness in the perineum
- Altered flow of urine
- A feeling of falling out
- Constipation / straining
- Discomfort during intercourse
Physical signs might include a bulge or protrusion at the entrance to the vagina.[1] In general, an individual’s symptoms are aggravated in positions where gravity acts on the body (e.g. standing, walking, lifting). Positions where gravity is eliminated (e.g. lying down) tend to be relieving.[1]
POP is a subjective experience. Some clients may have a mild prolapse but experience severe symptoms, whereas others have a significant prolapse but report minimal or no symptoms.[1][16] Diagnosis is made based on the clinical examination and subjective symptoms, such as:[1]
- Bulge sensation
- A feeling of pelvic pressure
- Bladder storage symptoms
- Urinary incontinence
- Recurrent UTIs
According to the Biomechanical / Pelvic Support Model, the pelvic floor holds up the pelvic organs. POP occurs when:[1][16]
- Fascia and ligaments which suspend the organs in place become lax, tear or lose integrity
- The pelvic organs, thus, lose suspensory support from above
- If the pelvic floor muscles are compromised / weak, it can mean that there is a lack of pelvic support from below
- When combined with poorly managed pressures in the abdominal canister (i.e. the area from the diaphragm to the pelvic floor[17]), there can be descent of the pelvic organs
- More significant prolapses can bulge / protrude from the vaginal opening
Levator Ani Muscle Avulsion[edit | edit source]
It is important to note that levator ani muscle avulsion may also be implicated in the development of POP. This type of avulsion fracture occurs when the levator ani muscle (see Figure 2) is detached from its origins in the pubis.[18]
It occurs in 10 to 30 percent of vaginal deliveries[18] and is more common when forceps are used or when there is a prolonged pushing stage.[1]
Types of Prolapse[edit | edit source]
Traditionally, POP has been categorised as:[1] [19]
- Cystocele (prolapsed bladder)
- Rectocele (prolapsed rectum)
- Uterine prolapse (prolapsed uterus)
- Urethrocele (prolapsed urethra)
- Enterocele (prolapsed intestine)
- Vaginal vault prolapse (top of the vagina prolapses - only occurs after a hysterectomy)
While these terms are still used, health care professionals are increasingly moving towards a more anatomically-based classification system and are adopting terminology such as:[20]
- Anterior vaginal wall prolapse
- Posterior vaginal wall prolapse
- Apical prolapse
Prolapse can be measured / graded using various systems, but one of the most commonly used staging systems is the POP-Q (Pelvic Organ Prolapse Quantification System). The POP-Q uses a four-point system to determine the degree of prolapse:[1][20]
- Stage 0 = no prolapse
- Stage 1 = prolapse is 1cm above the vaginal opening or higher
- Stage 2 = prolapse is 1cm away from the vaginal opening or has protruded up to 1cm out of the vagina
- Stage 3 = prolapse protrudes more than 1cm, but less than 2cm out of the vagina
- Stage 4 = the vaginal walls have completely everted, and the prolapse is maximally protruded
Physiotherapy can be an effective treatment for individuals who have stage 1 to 3 prolapses.[1]
However, it is important to note that a prolapse may be graded differently depending on factors such as the time of day, position of evaluation and method of evaluation. Therefore, physiotherapists may instead choose to rate a prolapse as mild, moderate, significant or severe.[1]
Persistent Pelvic Pain[edit | edit source]
Persistent pelvic pain is defined as pain that has been present in the pelvic area for more than three months.[21] Individuals may experience pain in their lower abdomen, pelvic floor, pelvic organs, hips, groin, buttocks, low back, coccyx, perineal region, vulvovaginal area, rectum, and genitalia.[21]
They may describe this pain as:[21]
- Constant or intermittent
- Deep or superficial
- Provoked by touch or present regardless of touch
- Dull, sharp or burning
- And the type of pain may change depending on the activity (e.g. urinating, sitting, intercourse)
Types of pelvic pain that a pelvic floor physiotherapist may treat include:[21]
- Dyspareunia (painful intercourse)
- Vaginismus (involuntary spasm of pelvic floor muscles when attempting penetration)
- Vulvodynia (generalised vulva pain)
- Vestibulodynia / vulva vestibulitis (pain in the vestibule region of the vulva)
- Clitroidynia (clitoral region pain)
- Coccydynia (coccyx pain)
- Dysmenorrhea (painful periods)
- Endometriosis (pain resulting from inflamed endometrial-like tissue, which is situated outside of the uterus)
- Adenomyosis (pain resulting from inflamed endometrial-like tissue, which is situated inside the muscular lining of the uterus)
- Painful bladder syndrome (has a similar presentation to interstitial cystitis - causes hypersensitivity and inflammation of the bladder wall lining)
- Levator ani syndrome or proctalgia fugax (occurs when there is tension / spasm in one major pelvic floor muscle group)
- Pudendal neuralgia or pudendal nerve entrapment (occurs when there is compression or irritation of the pudendal nerve)
- Persistent genital arousal disorder (persistent or recurrent, unwanted or intrusive, distressing, abnormal sensations that are not associated with sexual interest. Also called genitopelvic dysesthesia)
- Chronic pelvic pain syndrome (a descriptive diagnosis)
- Other types of pain which can be caused by: hormonal changes, menopause, abdominal or pelvic surgery, autoimmune disorders, internal scar tissue, gut or bladder dysfunction, pelvic girdle pain, sacroiliac joint pain, labral tears of the hip, myofascial / connective tissue dysfunction, trauma, or hypertonicity and overactivity of pelvic floor muscles
Additional information on some of these conditions is available here. In order to treat pelvic pain successfully, a physiotherapist needs to do a careful evaluation from a bio-psycho-social-spiritual and integrative framework. More information on treatment is available here.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 Afolabi I. Common Women's Pelvic Health Conditions Course. Plus , 2022.
- ↑ 2.0 2.1 Siracusa C, Gray A. Pelvic floor considerations in COVID-19. J Womens Health Phys Therap. 2020;44(4):144-51.
- ↑ 3.0 3.1 Sountoulidis P. Stress urinary incontinence [Internet]. ICS Committees. 2018 [cited 2 January 2022]. Available from: https://www.ics.org/committees/standardisation/terminologydiscussions/sui
- ↑ Sung VW, Borello-France D, Newman DK, Richter HE, Lukacz ES, Moalli P et al. Effect of behavioral and pelvic floor muscle therapy combined with surgery vs surgery alone on incontinence symptoms among women with mixed urinary incontinence: The ESTEEM randomized clinical trial. JAMA. 2019;322(11):1066-76.
- ↑ Mangir N, Chapple C. Management of urinary incontinence in men. Trends in Urology and Men's Health. 2020;11(2):18-22.
- ↑ Khandelwal C, Kistler C. Diagnosis of urinary incontinence. Am Fam Physician. 2013;87(8):543-50.
- ↑ Osmosis. Urinary incontinence - causes, symptoms, diagnosis, treatment, pathology. Available from: https://www.youtube.com/watch?v=vsLBApSlPMo [last accessed 3/1/2022]
- ↑ Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019;22(3):217-22.
- ↑ Minassian VA, Stewart WF, Wood GC. Urinary incontinence in women: variation in prevalence estimates and risk factors. Obstet Gynecol. 2008;111(2 Pt 1):324-31.
- ↑ NHS England. Excellence in continence care: Practical guidance for commissioners, and leaders in health and social care. Leeds: NHS England, 2018.
- ↑ Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary Incontinence in Women: A Review. JAMA. 2017;318(16):1592-1604.
- ↑ 12.0 12.1 12.2 Darmody E, Bradshaw C, Atkinson S Dr. Women's experience of obstetric anal sphincter injury following childbirth: An integrated review. Midwifery. 2020;91:102820.
- ↑ Rao SS, Patcharatrakul T. Diagnosis and treatment of dyssynergic defecation. J Neurogastroenterol Motil. 2016;22(3):423-35.
- ↑ The American College of Obstetricians and Gynecologists and the American Urogynecologic Society INTERIM UPDATE: This Practice Bulletin is updated as highlighted to reflect the US Food and Drug Administration order to stop the sale of transvaginal synthetic mesh products for the repair of pelvic organ prolapse. Pelvic Organ Prolapse. Female Pelvic Medicine & Reconstructive Surgery. 2019;25(6):397-408.
- ↑ Crowle A, Harley C. Development of a biotensegrity focused therapy for the treatment of pelvic organ prolapse: A retrospective case series. J Bodyw Mov Ther. 2020;24(1):115-25.
- ↑ 16.0 16.1 Weintraub AY, Glinter H, Marcus-Braun N. Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic organ prolapse. Int Braz J Urol. 2020;46(1):5-14.
- ↑ Emerich K, Reed O. The role of the pelvic floor in respiration: a multidisciplinary literature review. Journal of Voice. 2018;34(2):243-9.
- ↑ 18.0 18.1 Handa VL, Roem J, Blomquist JL, Dietz HP, Muñoz A. Pelvic organ prolapse as a function of levator ani avulsion, hiatus size, and strength. Am J Obstet Gynecol. 2019;221(1):41.e1-41.e7.
- ↑ The American College of Obstetricians and Gynecologists. Surgery for pelvic organ prolapse. Available from: https://www.acog.org/womens-health/faqs/surgery-for-pelvic-organ-prolapse (accessed 2 January 2022).
- ↑ 20.0 20.1 Persu C, Chapple CR, Cauni V, Gutue S, Geavlete P. Pelvic Organ Prolapse Quantification System (POP-Q) - a new era in pelvic prolapse staging. J Med Life. 2011;4(1):75-81.
- ↑ 21.0 21.1 21.2 21.3 The Mama's Physio. Persistent pelvic pain. Available from: https://themamasphysio.com/persistent-pelvic-pain/ (accessed 2 January 2022).