Joint Range of Motion During Gait: Difference between revisions
No edit summary |
No edit summary |
||
| Line 36: | Line 36: | ||
* 0% of gait cycle | * 0% of gait cycle | ||
* previously referred to as "heel strike", but in some pathological gaits heel strike may not be the initial instant<ref name=":4" /> | |||
*Function: | *Function: | ||
Revision as of 11:05, 12 September 2022
Top Contributors - Rachel Celentano, Wanda van Niekerk and Jess Bell
Introduction[edit | edit source]
Merriam-Webster dictionary defines gait as “a manner of walking or moving on foot."[1] It involves the interaction between the nervous, musculoskeletal, and cardiorespiratory systems and is heavily impacted by human age, personality, mood, and sociocultural factors.[2][3] Normal gait function is determined by the optimal operation of the following: “locomotor function (for initiating and sustaining rhythmic gait), balance, postural reflexes, sensory function and sensorimotor integration, motor control, the musculoskeletal apparatus and cardiopulmonary functions."[2][4]
Stance Versus Swing Phase[edit | edit source]
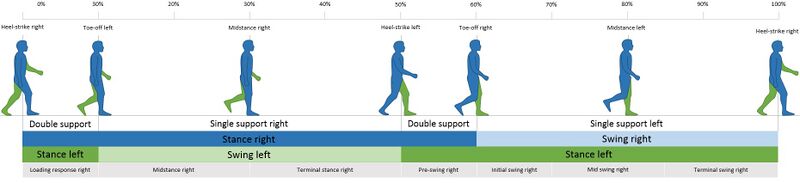
The normal forward stride consists of two phases: the stance phase and the swing phase.[5]
- The stance phase occupies 0-60% of the gait cycle, during which one leg and foot are bearing most or all of the body weight.[6]
- The swing phase occupies 60-100% (total 40%) of the gait cycle, during which the foot is not touching the walking surface and the bodyweight is borne by the other leg and foot.[7]
- In a complete two-step cycle, both feet are in contact with the floor at the same time for about 25% of the time. This part of the cycle is called the double-support phase.[6]
- Gait cycle phases: the stance phase and the swing phase involves a combination of open and close chain activities.[8][9]
Read more: The Gait Cycle
Phases of Gait[edit | edit source]
The stance and swing phases of gait can be subdivided into eight sub-phases.[6][9]
- Initial contact (Heel strike)
- Foot flat (Loading response)
- Midstance (Single-leg support)
- Heel off (Terminal stance)
- Toe off (Preswing)
- Initial swing
- Mid swing
- Late swing (Deceleration)
See below for a diagram of the gait cycle:
The video below shares a 90-second description of the basics of the gait cycle:
Range of Motion Involved in Gait Phases[edit | edit source]
Initial contact (Heel strike)
- 0% of gait cycle
- previously referred to as "heel strike", but in some pathological gaits heel strike may not be the initial instant[6]
- Function:
- To establish contact with surface and initiate weight acceptance[11]
| Body part | ROM requirements |
|---|---|
| Ankle | 0° (neutral position) |
| Knee | 0° (full extension) |
| Hip | average 20° of flexion |
Foot flat
- 8-10% of gait cycle
- Function:
- weight acceptance and shock absorption
| Body part | ROM requirements |
|---|---|
| Ankle | 0-5° plantarflexion |
| Knee | 15° of flexion |
| Hip | 15° of flexion (hip is moving into extension) |
Midstance
- The greater trochanter is vertically above the mid-point of the foot
- Function:
- Single limb support and stability
| Body part | ROM requirements |
|---|---|
| Ankle | 5° of dorsiflexion |
| Knee | 5° of flexion |
| Hip | 0° of flexion (neutral position) |
Heel off
- 30-40% of gait cycle
- Function
- Single limb support, stability, and propulsion
| Body part | ROM requirements |
|---|---|
| Ankle | 0° (neutral position) |
| Knee | 0° of flexion (complete extension) |
| Hip | 10-20° of hyperextension |
Toe off
- 60% of gait cycle (final phase of stance)
- Function
- Final burst of propulsion to propel the body forward
| Body part | ROM requirements |
|---|---|
| Ankle | 20° of plantarflexion |
| Knee | 30° of flexion |
| Hip | 10-20° of hyperextension |
Early swing
- 60-75% of gait cycle (beginning of swing phase)
- Toe off until the swinging limb is even with the stance limb
- Function
- To propel the lower extremity forward and shorten the stance limb
| Body part | ROM requirements |
|---|---|
| Ankle | 10° of plantarflexion |
| Knee | 60° of flexion |
| Hip | moves into 20° of flexion |
Mid swing
- 75-85% of gait cycle
- Swinging limb is opposite the stance limb
- Function
- To clear lower extremity from the ground in order to advance into initial contact
| Body part | ROM requirements |
|---|---|
| Ankle | 0° (neutral position) |
| Knee | moves into 30° of flexion |
| Hip | 30° of flexion (hip is moving into extension) |
Late swing
- 85-100% of gait cycle
- Tibia vertical to initial contact
- Function
- To decelerate lower extremity to establish contact with the ground
- To decelerate lower extremity to establish contact with the ground
| Body part | ROM requirements |
|---|---|
| Ankle | 0° (neutral position) |
| Knee | 0° (complete extension) |
| Hip | 30° of flexion |
The following video describes the range of motion requirements involved in the different gait phases:
Range of Motion during Gait [12]
Maximum Values[edit | edit source]
Maximum range of motion values is the minimum prerequisites for a normal gait pattern.[13]
| Body part | Maximum ROM values |
|---|---|
| Hip | 20° of extension; 20° of flexion |
| Knee | 0° (complete extension); 60° of flexion |
| Ankle | 5° of dorsiflexion; 20° of plantarflexion |
Gait Kinetics[edit | edit source]
Definitions
- Ground reaction force (GRF)
- creates an external plantarflexion or dorsiflexion torque
- If GRF anterior to joint axis - causes anterior motion of the proximal segment
- If GRF is posterior to joint axis - causes posterior motion of the proximal segment
- Lower extremity gait musculature - creates an internal torque.
- Centre of pressure - point of application of pressure to the foot segment
Initial contact
- Ankle
- At initial contact - lateral calcaneus strikes the ground first.
- Point of application of GRF is slightly posterior to the axis of rotation of the foot and ankle joint - creates a plantarflexion moment at the ankle.[9]
- Utilise dorsiflexors to oppose plantarflexor torque - internal torque controlled by tibialis anterior, extensor digitorum longus and extensor hallucis.
- Knee
- At initial contact - GRF is anterior to the knee joint creating anterior rotation of the femur.[9]
- GRF wants to move into extension.
- Utilise flexor musculature - hamstrings - in order to control progression.
- Hip
- GRF is anterior to hip joint - creating an external torque (anterior rotation) at the pelvis.[9]
- Utilise extensor musculature - gluteal musculature - to oppose/control the progression or external torque.
Foot flat
- Ankle
- Centre of pressure remains at the posterior calcaneus - GRF remains posterior to the ankle.[9]
- Utilise dorsiflexors to prevent plantarflexion from occurring at the ankle.
- Hip
- Centre of pressure and GRF remains the same - anterior to the axis of rotation.[9]
- Anterior pelvic tilt creates a flexion torque.
- Utilise extensor musculature to control this torque.
- Knee
- Range of motion moves from 0-15°
- GRF posterior to the axis of rotation of the knee joint - creates a flexion torque.[9]
- Utilise extensor musculature to control knee from moving into flexion.
Mid-stance
- Ankle
- GRF creates a clockwise torque of the proximal segment (on top of distal segment) - causing a dorsiflexion moment at the talocrural joint.[9]
- Utilise plantarflexors to oppose the external torque.
- Knee
- GRF creates an anterior (clockwise) torque of proximal segment (on top of distal segment) - wants to move into extension by femur moving anteriorly on tibia.[9]
- Utilise flexors to oppose this torque - activates hamstrings.
- Hip
- GRF is posterior to the axis of rotation - wants pelvis to move into a posterior pelvic tilt (extension).[9]
- Utilise flexors to oppose extension torque.
Heel off
- Ankle
- GRF is anterior to the axis of rotation of ankle joint - wants tibia to flex on talus.[9]
- Creates external dorsiflexion moment at talocrural joint.
- Utilise plantarflexors to oppose this moment.
- Knee
- GRF is anterior to knee joint - pulls femur into extension, creating an external extensor torque.[9]
- Counteracted by internal flexor torque.
- Hip
- GRF is posterior to hip joint - creates an external extensor moment.[9]
- Counteracted by internal flexor moment.
Toe off
- Ankle
- Centre of pressure/GRF stay anterior to axis of rotation of ankle joint.[9]
- Creates an external dorsiflexion moment.
- Counteracted by internal plantarflexion moment.
- Knee
- GRF is posterior to axis of rotation of knee joint as knee is moving into flexion.[9]
- Creates an external flexion moment.
- Counteracted by an internal extensor (quadricep musculature) moment.
- Hip
- GRF is posterior to axis of rotation of hip joint as hip is moving into extension.[9]
- Creates a posterior pelvic tilt.
- Utilise flexor musculature (iliopsoas) to counteract this moment.
Internal Torque Peaks[edit | edit source]
Hip:
- Foot flat - extensor torque
- Heel off - flexor torque
Knee:
- Initial contact - flexor torque (hamstring musculature active)
- Foot flat - extensor torque (quadriceps musculature active)
- Heel off - flexor torque (hamstring musculature active)
Ankle:
- Initial contact/Foot flat - dorsiflexion torque
- Heel off - plantarflexion torque (gastrocnemius/soleus active)
References[edit | edit source]
- ↑ Merriam-Webster. Gait. Available from: https://www.merriam-webster.com/dictionary/gait [last accessed 23.6.2022]
- ↑ 2.0 2.1 Pirker W, Katzenschlager R. Gait disorders in adults and the elderly. Wiener Klinische Wochenschrift. 2017 Feb 1;129(3-4):81-95. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5318488/ [last accessed 25.6.2022]
- ↑ Das R, Paul S, Mourya GK, Kumar N, Hussain M. Recent Trends and Practices Toward Assessment and Rehabilitation of Neurodegenerative Disorders: Insights From Human Gait. Frontiers in Neuroscience. 2022;16.
- ↑ Mirelman A, Shema S, Maidan I, Hausdorff JM. Gait. Handbook of clinical neurology. 2018 Jan 1;159:119-34.
- ↑ Cicirelli G, Impedovo D, Dentamaro V, Marani R, Pirlo G, D’Orazio TR. Human gait analysis in neurodegenerative diseases: a review. IEEE Journal of Biomedical and Health Informatics. 2021 Jun 28;26(1):229-42.
- ↑ 6.0 6.1 6.2 6.3 Magee DJ, Manske RC. Orthopedic physical assessment-E-Book. Elsevier Health Sciences; 2020 Dec 11.
- ↑ Loudon J, et al. The clinical orthopedic assessment guide. 2nd ed. Kansas: Human Kinetics, 2008. p.395-408.
- ↑ Shultz SJ et al. Examination of musculoskeletal injuries. 2nd ed, North Carolina: Human Kinetics, 2005. p55-60.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 9.13 9.14 9.15 9.16 Hazari A, Maiya AG, Nagda TV. Kinematics and Kinetics of Gait. InConceptual Biomechanics and Kinesiology 2021 (pp. 181-196). Springer, Singapore.
- ↑ Nicole Comninellis. The Gait Cycle Animation. Available from: https://www.youtube.com/watch?time_continue=35&v=DP5-um6SvQI [last accessed 19.7.2022]
- ↑ Webster JB, Darter BJ. Principles of normal and pathologic gait. InAtlas of Orthoses and Assistive Devices 2019 Jan 1 (pp. 49-62). Elsevier.
- ↑ Alexandra Kopelovich. Gait Range of Motion. Available from: https://www.youtube.com/watch?v=5Z6shSu96CM [last accessed 19.7.2022]
- ↑ Kopelovich, A. Joint Range of Motion during Gait. Course. Plus. 2022
- Gait
- Assessment
- Falls
- Hip - Assessment and Examination
- Knee - Assessment and Examination
- Ankle - Assessment and Examination
- Foot - Assessment and Examination
- Movement Analysis
- Older People/Geriatrics
- Older People/Geriatrics - Assessment and Examination
- Older People/Geriatrics - Outcome Measures
- Older People/Geriatrics - Physical Activity
- Balance
- Stroke
- Rehabilitation
- Course Pages