Diagnostic Approaches to Low Back Pain - Comparing Maitland, McKenzie and Movement Impairment Syndromes: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Mckenzie Method" to "[[McKenzie Method") |
||
| (44 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editor '''- [[User:Kathryn Priest|Kathryn Priest]], [[User:Katherine Portas|Katherine Portas]], [[User:Lea Cobham|Lea Cobham]] and [[User:Anj Leung|Anj Leung]] as part of the [[Nottingham University Spinal Rehabilitation Project]] | '''Original Editor '''- [[User:Kathryn Priest|Kathryn Priest]], [[User:Katherine Portas|Katherine Portas]], [[User:Lea Cobham|Lea Cobham]] and [[User:Anj Leung|Anj Leung]] as part of the [[Nottingham University Spinal Rehabilitation Project]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
= | == Introduction == | ||
[[File:Lower-back-pain.jpg|thumb|260x260px|Lower-back-pain]] | |||
Physiotherapists use a range of techniques to assess and diagnose [[Low Back Pain|low back pain]]. Three of the commonly used are those of Geoffrey Maitland ([[Maitland's Mobilisations|mobilisations]]), Robin McKenzie ([[McKenzie Method|derangement, dysfunction]]) and Shirley Sahrmann ([[Classification Of Low Back Pain Using Shirley Sahrmann’s Movement System Impairments, An Overview Of The Concept|movement impairment]]). For extensive details on each approach, please see the links above for the relevant Physiopedia pages. | |||
Determining which approach is best to use, in what circumstances and with which patients, can be confusing, especially for students and newly qualified clinicians. Furthermore, clinicians rarely use just one approach, and can often use these in combination with other modalities eg education, [[Back Exercises|exercise]], [[acupuncture]], [[massage]]<ref name="Gross et al, 2010">Gross A, Miller J, D’Sylva J, Burnie SJ, Goldsmith CH, Graham N, Haines T, Brønfort G, Hoving JL. Manipulation or Mobilisation for Neck Pain. Cochrane Database of Systematic Reviews 2010, Issue 1.</ref>. | |||
==Maitland's Mobilisations== | |||
[[File:Central Posteroanterior (PA) Mobilisation Technique.jpg|thumb|Central posteroanterior mobilisation]] | |||
Geoffrey Maitland first described his concept of mobilisations and [[Manipulation of the Lumbar Spine|manipulations]] in 1965<ref>Banks, K. Geoffrey D. Maitland, 1924–2010, Physical Therapy March 2010 vol. 90 no. 3 326 http://ptjournal.apta.org/content/90/3/326.full [accessed online 03/01/2014]</ref>. It is a passive mechanical approach that aims to move [[Synovial Joints|synovial joints]] ("passive [[Arthrokinematics|arthro-kinematic]] motion"; literally 'joint-moving')<ref name="Heiser et al 2013">Heiser R, O’Brien V, Schwartz D. The use of joint mobilization to improve clinical outcomes in hand therapy: A systematic review of the literature, 2013, Journal of Hand Therapy Vol 26, 297-311</ref> and their surrounding tissues. | |||
This can be applied both to the spine and to the extremities, with the goal of reducing [[Pain Behaviours|pain]] and stiffness and restoring correct alignment and function. | |||
For more see [[Maitland's Mobilisations]] | |||
=== Evidence === | |||
*Chiradejnant et al (2003) found that although lumbar spine Maitland mobilisations did have an immediate pain-relieving effect, the specific mobilisation performed was not important. Pain-relieving effects tended to be greater if the mobilisation was performed at lower lumbar levels rather than higher<ref name="Chiradejnant et al, 2003">Chiradejnant A, Maher C, Latimer J, Stepkovitch N. Efficacy of “therapist-selected” versus “randomly selected” mobilisation techniques for the treatment of low back pain: A randomised controlled trial, 2003, Australian Journal of Physiotherapy, Vol. 49 233-241</ref><br> | |||
*In a small trial comparing grade II and grade III mobilisations in 30 patients with sub-acute to chronic lumbar spine pain, Seema (2012) found that both techniques had a significant positive effect (p=0.001) on pain scores. Grade III mobilisations had a greater effect than grade II. <ref>Seema S, Effect of Grade II and Grade III Mobilization by Maitland Technique in Low Back Pain, 2012, Indian Journal of Physiotherapy and Occupational Therapy - An International Journal, Vol 6 (4), p91 - 95</ref> | |||
*In a small trial comparing grade II and grade III mobilisations in 30 patients with sub-acute to chronic lumbar spine pain, Seema (2012) found that both techniques had a significant positive effect (p=0.001) on pain scores. Grade III mobilisations had a greater effect than grade II. <ref>Seema S, Effect of Grade II and Grade III Mobilization by Maitland Technique in Low Back Pain, 2012, Indian Journal of Physiotherapy and Occupational Therapy - An International Journal, Vol 6 (4), p91 - 95</ref> | |||
*Naik et al (2007) suggested that Maitland's mobilisations are more effective at improving range of movement than Mobilisations With Movement (MWMs - Mulligan approach), although MWMs are more effective if pain is the most prominent factor for the patient. They also noted that the group receiving Maitland mobilisations required more sessions before being discharged than the MWM group<ref name="Naik et al, 2007">Naik VC, Chitra J, Khatri S. Effectiveness of Maitland versus Mulligan mobilization technique following post-surgical management of Colles fracture; randomized clinical trial, 2007. Indian Journal of Physiotherapy and Occupational Therapy. Vol 1(4):14-19.</ref>. However it is worth noting that this was a study on mobilisations after a Colles (distal radius) fracture.<br> | *Naik et al (2007) suggested that Maitland's mobilisations are more effective at improving range of movement than Mobilisations With Movement (MWMs - Mulligan approach), although MWMs are more effective if pain is the most prominent factor for the patient. They also noted that the group receiving Maitland mobilisations required more sessions before being discharged than the MWM group<ref name="Naik et al, 2007">Naik VC, Chitra J, Khatri S. Effectiveness of Maitland versus Mulligan mobilization technique following post-surgical management of Colles fracture; randomized clinical trial, 2007. Indian Journal of Physiotherapy and Occupational Therapy. Vol 1(4):14-19.</ref>. However it is worth noting that this was a study on mobilisations after a Colles (distal radius) fracture.<br> | ||
*In a systematic review of randomised controlled trials in five languages, Bronfort et al (2004) found that one treatment of spinal manipulation therapy (SMT) was superior to one treatment of spinal mobilisations for acute low back pain. There was also moderate quality evidence that SMT: | *In a systematic review of randomised controlled trials in five languages, Bronfort et al (2004) found that one treatment of spinal manipulation therapy (SMT) was superior to one treatment of spinal mobilisations for acute low back pain. There was also moderate quality evidence that SMT: | ||
**Is superior to detuned diathermy 1 week after treatment | |||
**Resulted in faster recovery than patients receiving a combination of diathermy, exercise and ergonomic instruction. | |||
**Resulted in a faster recovery time than heat therapy for patients with LBP accompanied by sciatica <ref>Bronfort G, Haas M, Evans R, Bouter L, Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis, 2004, The Spine Journal, Volume 4, Issue 3, P 335–356</ref><br> | |||
= | *A comparison of Maitland mobilisations versus McKenzie -style press ups in 30 patients with non-specific low back pain found that both methods significantly reduced the patient-reported pain rating. However, neither treatment was found to be superior to the other <ref name="Powers">Powers C, Beneck G, Kulig K, Landel R, Fredericson M, Effects of a Single Session of Posterior-to-Anterior Spinal Mobilization andfckLRPress-up Exercise on Pain ResponsefckLRand Lumbar Spine Extension in PeoplefckLRWith Nonspecific Low Back Pain, 2008, Physical Therapy, Vol 88(4) p485-493</ref>.<br> | ||
Other Points to Consider: Clinical Expertise and Practical Application see [https://cdnapisec.kaltura.com/html5/html5lib/v1.9.5/mwEmbedFrame.php/p/1355621/uiconf_id/13724441/entry_id/1_h7iecqfh?wid=_1355621&iframeembed=true&playerId=kaltura_player&entry_id=1_h7iecqfh&wid=1_qxuh12px&flashvars Interview with Heather Reid, Physiotherapy Lecturer at The University of Nottingham] | |||
[ | == The McKenzie Approach == | ||
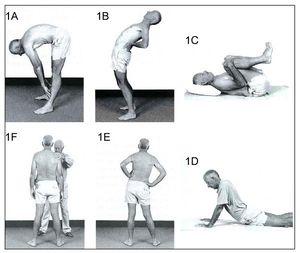
[[File:McKenzie side glide.jpg|thumb|McKenzie side glide]] | |||
Using [[McKenzie Method|McKenzie]] Mechanical Diagnosis and Therapy (MDT) the patient can be classified into one of three mechanical syndromes; Derangement, Dysfunction or Postural Syndrome. If the patient has no symptom improvement after several sessions they will be classified into "Other" <ref name="May et al 2008">May, S. and Donelson, R. Evidence- informed management of chronic low back pain with the McKenzie method. The Spine Journal. 2008;8:134-141</ref>. | |||
The McKenzie approach is a combination of active therapy and education for patients with acute, sub-acute and chronic non-specific low back pain <ref name="Garcia et al">Garcia, A.N., Costa, L.C.M., Silva, T.M., Gondo, F.L.B., Cyrillo, F.N., Costa, F.M., Costa, L.O.P. Effectiveness of Back School Versus McKenzie Exercises in Patients with Chronic Nonspecific Low Back Pain: A Randomized Control Trial.2013;93(6):729-747</ref>. | |||
=== McKenzie Classifications === | |||
{| width="800" cellspacing="1" cellpadding="1" border="3" align="center" | {| width="800" cellspacing="1" cellpadding="1" border="3" align="center" | ||
|- | |- | ||
| Line 222: | Line 57: | ||
|} | |} | ||
<br> For an in depth description of these syndromes please follow | <br> For an in-depth description of these syndromes please follow this [[McKenzie Method|link]]: | ||
=== Evidence === | |||
*Many pain measures showed that the McKenzie method is a successful treatment to decrease chronic low back pain in the short term, while the disability measures determined that the McKenzie method is better in enhancing function in the long term<ref>Namnaqani FI, Mashabi AS, Yaseen KM, Alshehri MA. The effectiveness of McKenzie method compared to manual therapy for treating chronic low back pain: a systematic review. Journal of Musculoskeletal & Neuronal Interactions. 2019;19(4):492.</ref> | |||
| |||
=== | |||
*When a lumbar assessment is performed by a clinician with McKenzie training there is high reliability of classifications (Kappa =0.89)<ref name="Clare et al 2005">Clare,H.A., Adams, R.and Maher, C.G. Reliability of the McKenzie Classification of patients with cervical and lumbar pain. Journal of Manipulative and Physiological Therapeutics. 2005;28(2):122-127</ref>. | *When a lumbar assessment is performed by a clinician with McKenzie training there is high reliability of classifications (Kappa =0.89)<ref name="Clare et al 2005">Clare,H.A., Adams, R.and Maher, C.G. Reliability of the McKenzie Classification of patients with cervical and lumbar pain. Journal of Manipulative and Physiological Therapeutics. 2005;28(2):122-127</ref>. | ||
*Evidence highlights short-term improvements in pain and disability using the McKenzie method however; more research is needed into the long-term benefits<ref name="Machado et al 2006">Machado, L.A.C., Sperling de Souze, M.V., Ferreira, P.H. and Ferreira, M.L. The McKenzie Method for Low Back Pain: A systematic Review of the Literature with a Meta-Analysis Approach. SPINE. 2006;31(9): 254-262</ref>. | *Evidence highlights short-term improvements in pain and disability using the McKenzie method however; more research is needed into the long-term benefits<ref name="Machado et al 2006">Machado, L.A.C., Sperling de Souze, M.V., Ferreira, P.H. and Ferreira, M.L. The McKenzie Method for Low Back Pain: A systematic Review of the Literature with a Meta-Analysis Approach. SPINE. 2006;31(9): 254-262</ref>. | ||
*Directional preference exercises encourage active management and elicit patient empowerment. In health care practice it is perceived as a cost effective intervention<ref name="May et al 2008" />. | *Directional preference exercises encourage active management and elicit patient empowerment. In health care practice it is perceived as a cost effective intervention<ref name="May et al 2008" />. | ||
*MDT primarily treats the mechanical dysfunction, with the intention that the improvement of symptoms may positively affect the psychological presentation of the patient <ref name="Karayannis et al" / | *MDT primarily treats the mechanical dysfunction, with the intention that the improvement of symptoms may positively affect the psychological presentation of the patient <ref name="Karayannis et al">Karayannis, N.V., Jull, G.A. and Hodges, P. Physiotherapy movement based classification approaches to low back pain: comparison of subgroups through review and developer/expert opinion. BioMed Central Musculoskeletal Disorders.2012;13:24</ref>. | ||
< | |||
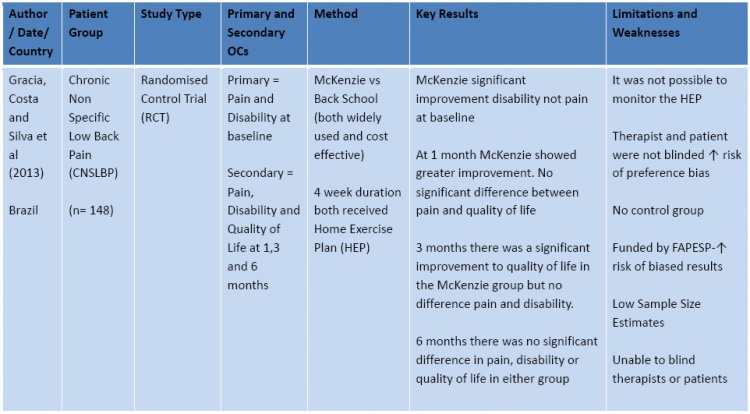
The tables below summarise the evidence since 2009. This summary is not exhaustive, but follows [http://bestbets.org/ca/pdf/trial.pdf the principles of critical assessment for randomised controlled trials] as defined at www.bestbets.org . | The tables below summarise the evidence since 2009. This summary is not exhaustive, but follows [http://bestbets.org/ca/pdf/trial.pdf the principles of critical assessment for randomised controlled trials] as defined at www.bestbets.org . [[Image:McKenzie table 1.jpg|center|750px]][[Image:McKenzie table 2.jpg|center|750px]] | ||
'''ABBREVIATIONS for Tables:''' | '''ABBREVIATIONS for Tables:''' | ||
CNSLBP = Chronic Non-Specific Low Back Pain<br>RCT = Randomised Control Trial<br>Rx = Treatment<br>n= number of participants | CNSLBP = Chronic Non-Specific Low Back Pain<br>RCT = Randomised Control Trial<br>Rx = Treatment<br>n= number of participants | ||
Other points to Consider: Clinical Expertise and Practical Application see [https://cdnapisec.kaltura.com/html5/html5lib/v1.9.5/mwEmbedFrame.php/p/1355621/uiconf_id/13724441/entry_id/1_kie9azzl?wid=_1355621&iframeembed=true&playerId=kaltura_player&entry_id=1_kie9azzl&wid=1_h4pqbvav&flashvars Interview with Jackie Hollowell, Physiotherapy Lecturer at The University of Nottingham:] | |||
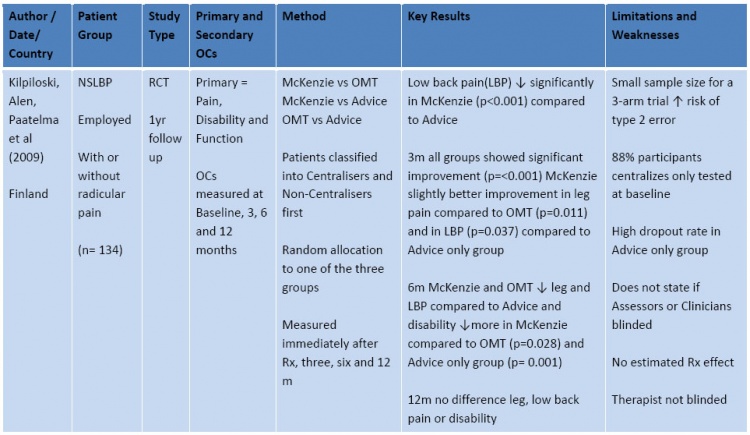
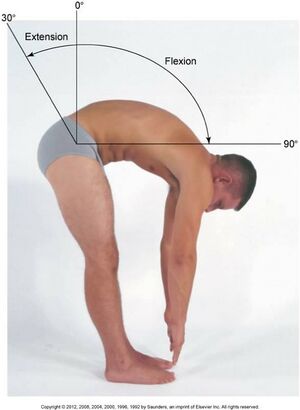
== Movement Impairment Syndromes == | |||
[[File:Lspine rom.jpg|thumb|Lumbar spine flexion ]] | |||
For a more detailed description of this approach and treatment structure visit [[Classification Of Low Back Pain Using Shirley Sahrmann’s Movement System Impairments, An Overview Of The Concept]] | |||
For a more detailed description of this approach and treatment structure | |||
Like McKenzie, Sahrmann’s Movement Impairment Syndromes (MIS) approach to diagnosis of LBP is one of a number of movement based classification systems designed to help therapists categorise patients and inform treatment <ref>Karayannis, N.V., Jull, G.A., and Hodges, P.W. (2012) Physiotherapy movement based classification approaches to low back pain: comparison of subgroups through review and developer/expert survey. BMC Musculoskeletal Disorders.13:24</ref> . | Like McKenzie, Sahrmann’s Movement Impairment Syndromes (MIS) approach to diagnosis of LBP is one of a number of movement based classification systems designed to help therapists categorise patients and inform treatment <ref>Karayannis, N.V., Jull, G.A., and Hodges, P.W. (2012) Physiotherapy movement based classification approaches to low back pain: comparison of subgroups through review and developer/expert survey. BMC Musculoskeletal Disorders.13:24</ref> . | ||
The theory behind the approach revolves around the human ‘Movement System’ and impairments within this system. Impairments are caused by decline in the quality and precision of joint movements in the spine, as a result of repeated habitual movements or prolonged postures. This may result in: | The theory behind the approach revolves around the human ‘Movement System’ and impairments within this system. Impairments are caused by decline in the quality and precision of joint movements in the spine, as a result of repeated habitual movements or prolonged postures. This may result in: | ||
* Muscle length/strength imbalances | |||
* Altered patterns of motor recruitment patterns and timing | |||
* De-recruitment | |||
* Stiffness<br><ref name="Karayannis et al" /><ref>Sahrmann, S.A. (2001) Diagnosis and Treatment of Movement Impairment Syndromes. Mosby.</ref> | |||
These adaptations can cause altered movements resulting in microtrama to tissue that can accumulate to form macro trauma over time. This is because the human movement system works on the principle of the ‘Path of least resistance’. Stiffness in a muscle or joint will result in a compensatory movement elsewhere resulting in a movement strategy that is not mechanically advantageous and can result in pain. | These adaptations can cause altered movements resulting in microtrama to tissue that can accumulate to form macro trauma over time. This is because the human movement system works on the principle of the ‘Path of least resistance’. Stiffness in a muscle or joint will result in a compensatory movement elsewhere resulting in a movement strategy that is not mechanically advantageous and can result in pain. | ||
< | === Evidence Regarding the Effectiveness of the Movement Diagnosis Approach === | ||
* Intertester reliability for diagnosis using the MIS approach had ‘substantial’ agreement (Kappa >60%). But this was dependant on the diagnostic subgroup and training level of testers. The Flexion and Rotation with Flexion diagnosis the most reliably diagnosed<ref name="Karayannis et al" />. | |||
* No clear advantage has been found for having a specific patho-anatomical diagnosis for LBP over a movement based approach, or vice versa. Although Sahrmann acknowledges that a ‘modified approach’ if needed when a patient has a specific medical diagnosis such a stenosis, but how this is to be operationalized is less well defined<ref name="Karayannis et al" />. | |||
* MIS has established itself as an effective diagnostic tool for sub classifying LBP, however there is a sparse amount of literature showing the effectiveness treatment within this approach<ref name="Sahrmann 2012a">Sahrmann Interviewed by L. Payne: 6th December 2012a part 1. Available at: http://www.youtube.com/watch?v=faEzHR5zLjs. [Accessed 13/01/14]</ref> <ref name="Trudelle">Trudelle-Jackson, E., Sarvaiya-Shah, S. and Wang, S. Interrater reliability of a movement impairment-based classification system for lumbar spine syndromes in patients with low back pain. The Journal of Orthopaedic and Sports Physical Therapy 2009;38(6):371-376.</ref>. There have been a few case studies reporting reduction of symptoms <ref name="Harris Hayes">Harris-Hayes, M., Van Dillen, L. and Sahrmann, S. Classification, treatment and outcomes of a patient with lumbar extension syndrome. Physiotherapy Theory and Practice 2005; 21(3):181-196.</ref> <ref name="Van Dillen et al">Van Dillen LR, Sahrmann SA, Norton BJ, et al. Effect of active limb movements on symptoms in patients with low back pain. J Orthop Sports Phys Ther 2001;31:402-413.</ref> and many physiotherapists utilising this approach with their patients have seen positive results anecdotally. | |||
=== Limitations === | |||
* There is little reference to bio-psycho-social factors within the MIS approach, although fear avoidance can be measured, but it is not clear how differently a patient with high fear avoidance would be managed<ref name="Karayannis et al" />. Sahrmann and Van Dillen acknowledge that the bio-psycho-social subtype have not featured strongly in their research<ref name="Karayannis et al" />. | |||
* No acknowledgement of [http://www.youtube.com/watch?v=4b8oB757DKc central sensitisation] within LBP was found in the MIS approach<ref name="Karayannis et al" /> and Sahrmann has eluded to the overuse of this term by therapists as a way of explaining why their patients are not getting better<ref name="Sahrmann 2012b">Sahrmann Interviewed by L. Payne: 6th December 2012b part 3. Available at: http://www.youtube.com/watch?v=TsDbmAyzMd8. [Accessed 13/01/14]</ref>. However, there is a growing amount of strong evidence that LBP, particularly chronic LBP, is fuelled by a combination of bio-psychosocial factors that lead to maladaptive behaviours and physiological changes that cause central sensitisation of the nervous system<ref name="O'Sullivan">O’Sullivan, P. It’s time for change with the management of non-specificfckLRchronic low back pain. Br J Sports Med 2011. Available from: http://bjsm.bmj.com/content/early/2011/08/04/bjsm.2010.081638.full.htmlfckLR[Accessed 11/01/14]</ref>. | |||
* This approach has been criticised for its exclusion of patho-anatomical factors; factors such as tissue healing which are important for effective treatment<ref name="Ford and Hahne">Ford, J. J. and Hahne, A. J. Pathoanatomy and classification of low back disorders. Manual Therapy 2013.18:165-168</ref> | |||
* One final limitation of the MIS approach to diagnosis of LBP is that it takes quite a long time to perform this thorough assessment. In a busy hospital outpatients setting, time constraints may limit the practicality of using this approach.<br> | |||
Other Points to Consider: Clinical Expertise and Practical Application see [https://cdnapisec.kaltura.com/html5/html5lib/v1.9.5/mwEmbedFrame.php/p/1355621/uiconf_id/13724441/entry_id/1_fqyr0cra?wid=_1355621&iframeembed=true&playerId=kaltura_player&entry_id=1_fqyr0cra&wid=1_49c15ib8&flashvars Interview with Catherine Moore, Physiotherapy Lecturer at The University of Nottingham] | |||
Considering a Combined Approach see [https://cdnapisec.kaltura.com/html5/html5lib/v1.9.5/mwEmbedFrame.php/p/1355621/uiconf_id/13724441/entry_id/1_snqizkxp?wid=_1355621&iframeembed=true&playerId=kaltura_player&entry_id=1_snqizkxp&wid=1_owbjb2ml&flashvars Interview with Roger Kerry, Physiotherapy Lecturer at The University of Nottingham] | |||
== Case studies: Applying Approaches to Clinical examples == | |||
==== Patient 1 ==== | |||
A 36-year-old male, presents with a 2-week history of right sided low back pain. Patient works as a shop assistant and recently had to complete extra shifts for Christmas. Whilst bending down to lift a heavy box, he felt a sharp pain and immediately struggled to stand back up. He has been experiencing occasional numbness in his right leg when he has been walking for more than 15 minutes. | A 36-year-old male, presents with a 2-week history of right sided low back pain. Patient works as a shop assistant and recently had to complete extra shifts for Christmas. Whilst bending down to lift a heavy box, he felt a sharp pain and immediately struggled to stand back up. He has been experiencing occasional numbness in his right leg when he has been walking for more than 15 minutes. | ||
| Line 413: | Line 114: | ||
<u>'''Eases:'''</u> sleeping on front with pillows propped up, rest, hot water bottle over back | <u>'''Eases:'''</u> sleeping on front with pillows propped up, rest, hot water bottle over back | ||
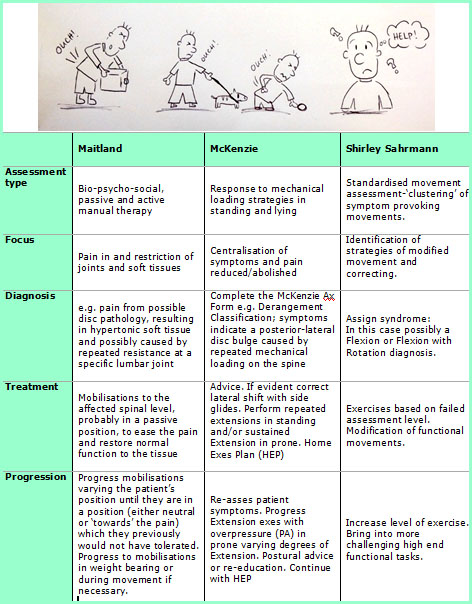
[[Image:Case study 1.jpg|center|Example of how the different approaches would assess and progress this patient]] | [[Image:Case study 1.jpg|center|Example of how the different approaches would assess and progress this patient]] | ||
==== Patient 2 ==== | |||
A 56-year-old female, presents with a 3-month history of central low back pain. She has been experiencing low back pain for the past 18 months but has been gradually getting worse over the last 3 months. She cannot recall any trauma or change in activity to flare up the pain. The patient is an office worker and is currently off work. she denies any leg and buttock symptoms, and has no obvious red flags. <br>She recalls having had 3 sessions of physiotherapy previously, which had some effect but he was too busy to carry on with the exercise regime. She cannot recall any of the exercises she was given previously. | A 56-year-old female, presents with a 3-month history of central low back pain. She has been experiencing low back pain for the past 18 months but has been gradually getting worse over the last 3 months. She cannot recall any trauma or change in activity to flare up the pain. The patient is an office worker and is currently off work. she denies any leg and buttock symptoms, and has no obvious red flags. <br>She recalls having had 3 sessions of physiotherapy previously, which had some effect but he was too busy to carry on with the exercise regime. She cannot recall any of the exercises she was given previously. | ||
<u>'''Aggs:'''</u> bending forward, rotating to L+R, bending to the side L+R | <u>'''Aggs:'''</u> bending forward, rotating to L+R, bending to the side L+R | ||
<u>'''Eases:'''</u> lying flat on back, hot baths, heat rub | <u>'''Eases:'''</u> lying flat on back, hot baths, heat rub<br> [[Image:Case study 2.jpg|center|704px]] | ||
== Conclusions == | |||
As a whole, all three approaches have their strengths and limitations. Clinical opinions on all three show both positives and negatives. Choosing which approach to use tends to depend on the learning experience of a therapist during their time as a student, as well as clinical and personal experiences. | |||
Approaches can be adapted and used in combination; allowing a thorough assessment and diagnosis of a patient’s problem, looking at both mechanical, structural and movement impairments. | |||
== References == | |||
<references /> | |||
<br> | |||
[[Category:Nottingham University Spinal Rehabilitation Project]] | |||
[[Category:Assessment]] | |||
[[Category:Lumbar Spine]] | |||
| |||
[[Category:Lumbar Spine - Assessment and Examination]] | |||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
Latest revision as of 10:28, 13 April 2022
Original Editor - Kathryn Priest, Katherine Portas, Lea Cobham and Anj Leung as part of the Nottingham University Spinal Rehabilitation Project
Top Contributors - Kathryn Priest, Katherine Portas, Angela Hiu-Wai Leung, Kim Jackson, Lea Cobham, Lucinda hampton, Admin, Candace Goh, 127.0.0.1 and Evan Thomas
Introduction [edit | edit source]
Physiotherapists use a range of techniques to assess and diagnose low back pain. Three of the commonly used are those of Geoffrey Maitland (mobilisations), Robin McKenzie (derangement, dysfunction) and Shirley Sahrmann (movement impairment). For extensive details on each approach, please see the links above for the relevant Physiopedia pages.
Determining which approach is best to use, in what circumstances and with which patients, can be confusing, especially for students and newly qualified clinicians. Furthermore, clinicians rarely use just one approach, and can often use these in combination with other modalities eg education, exercise, acupuncture, massage[1].
Maitland's Mobilisations[edit | edit source]
Geoffrey Maitland first described his concept of mobilisations and manipulations in 1965[2]. It is a passive mechanical approach that aims to move synovial joints ("passive arthro-kinematic motion"; literally 'joint-moving')[3] and their surrounding tissues.
This can be applied both to the spine and to the extremities, with the goal of reducing pain and stiffness and restoring correct alignment and function.
For more see Maitland's Mobilisations
Evidence[edit | edit source]
- Chiradejnant et al (2003) found that although lumbar spine Maitland mobilisations did have an immediate pain-relieving effect, the specific mobilisation performed was not important. Pain-relieving effects tended to be greater if the mobilisation was performed at lower lumbar levels rather than higher[4]
- In a small trial comparing grade II and grade III mobilisations in 30 patients with sub-acute to chronic lumbar spine pain, Seema (2012) found that both techniques had a significant positive effect (p=0.001) on pain scores. Grade III mobilisations had a greater effect than grade II. [5]
- Naik et al (2007) suggested that Maitland's mobilisations are more effective at improving range of movement than Mobilisations With Movement (MWMs - Mulligan approach), although MWMs are more effective if pain is the most prominent factor for the patient. They also noted that the group receiving Maitland mobilisations required more sessions before being discharged than the MWM group[6]. However it is worth noting that this was a study on mobilisations after a Colles (distal radius) fracture.
- In a systematic review of randomised controlled trials in five languages, Bronfort et al (2004) found that one treatment of spinal manipulation therapy (SMT) was superior to one treatment of spinal mobilisations for acute low back pain. There was also moderate quality evidence that SMT:
- Is superior to detuned diathermy 1 week after treatment
- Resulted in faster recovery than patients receiving a combination of diathermy, exercise and ergonomic instruction.
- Resulted in a faster recovery time than heat therapy for patients with LBP accompanied by sciatica [7]
- A comparison of Maitland mobilisations versus McKenzie -style press ups in 30 patients with non-specific low back pain found that both methods significantly reduced the patient-reported pain rating. However, neither treatment was found to be superior to the other [8].
Other Points to Consider: Clinical Expertise and Practical Application see Interview with Heather Reid, Physiotherapy Lecturer at The University of Nottingham
The McKenzie Approach [edit | edit source]
Using McKenzie Mechanical Diagnosis and Therapy (MDT) the patient can be classified into one of three mechanical syndromes; Derangement, Dysfunction or Postural Syndrome. If the patient has no symptom improvement after several sessions they will be classified into "Other" [9].
The McKenzie approach is a combination of active therapy and education for patients with acute, sub-acute and chronic non-specific low back pain [10].
McKenzie Classifications[edit | edit source]
| Derangement Syndrome | Dysfunction Syndrome | Postural Syndrome |
|
|
|
For an in-depth description of these syndromes please follow this link:
Evidence [edit | edit source]
- Many pain measures showed that the McKenzie method is a successful treatment to decrease chronic low back pain in the short term, while the disability measures determined that the McKenzie method is better in enhancing function in the long term[11]
- When a lumbar assessment is performed by a clinician with McKenzie training there is high reliability of classifications (Kappa =0.89)[12].
- Evidence highlights short-term improvements in pain and disability using the McKenzie method however; more research is needed into the long-term benefits[13].
- Directional preference exercises encourage active management and elicit patient empowerment. In health care practice it is perceived as a cost effective intervention[9].
- MDT primarily treats the mechanical dysfunction, with the intention that the improvement of symptoms may positively affect the psychological presentation of the patient [14].
The tables below summarise the evidence since 2009. This summary is not exhaustive, but follows the principles of critical assessment for randomised controlled trials as defined at www.bestbets.org .
ABBREVIATIONS for Tables:
CNSLBP = Chronic Non-Specific Low Back Pain
RCT = Randomised Control Trial
Rx = Treatment
n= number of participants
Other points to Consider: Clinical Expertise and Practical Application see Interview with Jackie Hollowell, Physiotherapy Lecturer at The University of Nottingham:
Movement Impairment Syndromes[edit | edit source]
For a more detailed description of this approach and treatment structure visit Classification Of Low Back Pain Using Shirley Sahrmann’s Movement System Impairments, An Overview Of The Concept
Like McKenzie, Sahrmann’s Movement Impairment Syndromes (MIS) approach to diagnosis of LBP is one of a number of movement based classification systems designed to help therapists categorise patients and inform treatment [15] .
The theory behind the approach revolves around the human ‘Movement System’ and impairments within this system. Impairments are caused by decline in the quality and precision of joint movements in the spine, as a result of repeated habitual movements or prolonged postures. This may result in:
- Muscle length/strength imbalances
- Altered patterns of motor recruitment patterns and timing
- De-recruitment
- Stiffness
[14][16]
These adaptations can cause altered movements resulting in microtrama to tissue that can accumulate to form macro trauma over time. This is because the human movement system works on the principle of the ‘Path of least resistance’. Stiffness in a muscle or joint will result in a compensatory movement elsewhere resulting in a movement strategy that is not mechanically advantageous and can result in pain.
Evidence Regarding the Effectiveness of the Movement Diagnosis Approach[edit | edit source]
- Intertester reliability for diagnosis using the MIS approach had ‘substantial’ agreement (Kappa >60%). But this was dependant on the diagnostic subgroup and training level of testers. The Flexion and Rotation with Flexion diagnosis the most reliably diagnosed[14].
- No clear advantage has been found for having a specific patho-anatomical diagnosis for LBP over a movement based approach, or vice versa. Although Sahrmann acknowledges that a ‘modified approach’ if needed when a patient has a specific medical diagnosis such a stenosis, but how this is to be operationalized is less well defined[14].
- MIS has established itself as an effective diagnostic tool for sub classifying LBP, however there is a sparse amount of literature showing the effectiveness treatment within this approach[17] [18]. There have been a few case studies reporting reduction of symptoms [19] [20] and many physiotherapists utilising this approach with their patients have seen positive results anecdotally.
Limitations[edit | edit source]
- There is little reference to bio-psycho-social factors within the MIS approach, although fear avoidance can be measured, but it is not clear how differently a patient with high fear avoidance would be managed[14]. Sahrmann and Van Dillen acknowledge that the bio-psycho-social subtype have not featured strongly in their research[14].
- No acknowledgement of central sensitisation within LBP was found in the MIS approach[14] and Sahrmann has eluded to the overuse of this term by therapists as a way of explaining why their patients are not getting better[21]. However, there is a growing amount of strong evidence that LBP, particularly chronic LBP, is fuelled by a combination of bio-psychosocial factors that lead to maladaptive behaviours and physiological changes that cause central sensitisation of the nervous system[22].
- This approach has been criticised for its exclusion of patho-anatomical factors; factors such as tissue healing which are important for effective treatment[23]
- One final limitation of the MIS approach to diagnosis of LBP is that it takes quite a long time to perform this thorough assessment. In a busy hospital outpatients setting, time constraints may limit the practicality of using this approach.
Other Points to Consider: Clinical Expertise and Practical Application see Interview with Catherine Moore, Physiotherapy Lecturer at The University of Nottingham
Considering a Combined Approach see Interview with Roger Kerry, Physiotherapy Lecturer at The University of Nottingham
Case studies: Applying Approaches to Clinical examples[edit | edit source]
Patient 1[edit | edit source]
A 36-year-old male, presents with a 2-week history of right sided low back pain. Patient works as a shop assistant and recently had to complete extra shifts for Christmas. Whilst bending down to lift a heavy box, he felt a sharp pain and immediately struggled to stand back up. He has been experiencing occasional numbness in his right leg when he has been walking for more than 15 minutes.
Aggs:Bending forwards, walking the dog, walking up hill
Eases: sleeping on front with pillows propped up, rest, hot water bottle over back
Patient 2[edit | edit source]
A 56-year-old female, presents with a 3-month history of central low back pain. She has been experiencing low back pain for the past 18 months but has been gradually getting worse over the last 3 months. She cannot recall any trauma or change in activity to flare up the pain. The patient is an office worker and is currently off work. she denies any leg and buttock symptoms, and has no obvious red flags.
She recalls having had 3 sessions of physiotherapy previously, which had some effect but he was too busy to carry on with the exercise regime. She cannot recall any of the exercises she was given previously.
Aggs: bending forward, rotating to L+R, bending to the side L+R
Eases: lying flat on back, hot baths, heat rub
Conclusions[edit | edit source]
As a whole, all three approaches have their strengths and limitations. Clinical opinions on all three show both positives and negatives. Choosing which approach to use tends to depend on the learning experience of a therapist during their time as a student, as well as clinical and personal experiences.
Approaches can be adapted and used in combination; allowing a thorough assessment and diagnosis of a patient’s problem, looking at both mechanical, structural and movement impairments.
References[edit | edit source]
- ↑ Gross A, Miller J, D’Sylva J, Burnie SJ, Goldsmith CH, Graham N, Haines T, Brønfort G, Hoving JL. Manipulation or Mobilisation for Neck Pain. Cochrane Database of Systematic Reviews 2010, Issue 1.
- ↑ Banks, K. Geoffrey D. Maitland, 1924–2010, Physical Therapy March 2010 vol. 90 no. 3 326 http://ptjournal.apta.org/content/90/3/326.full [accessed online 03/01/2014]
- ↑ Heiser R, O’Brien V, Schwartz D. The use of joint mobilization to improve clinical outcomes in hand therapy: A systematic review of the literature, 2013, Journal of Hand Therapy Vol 26, 297-311
- ↑ Chiradejnant A, Maher C, Latimer J, Stepkovitch N. Efficacy of “therapist-selected” versus “randomly selected” mobilisation techniques for the treatment of low back pain: A randomised controlled trial, 2003, Australian Journal of Physiotherapy, Vol. 49 233-241
- ↑ Seema S, Effect of Grade II and Grade III Mobilization by Maitland Technique in Low Back Pain, 2012, Indian Journal of Physiotherapy and Occupational Therapy - An International Journal, Vol 6 (4), p91 - 95
- ↑ Naik VC, Chitra J, Khatri S. Effectiveness of Maitland versus Mulligan mobilization technique following post-surgical management of Colles fracture; randomized clinical trial, 2007. Indian Journal of Physiotherapy and Occupational Therapy. Vol 1(4):14-19.
- ↑ Bronfort G, Haas M, Evans R, Bouter L, Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis, 2004, The Spine Journal, Volume 4, Issue 3, P 335–356
- ↑ Powers C, Beneck G, Kulig K, Landel R, Fredericson M, Effects of a Single Session of Posterior-to-Anterior Spinal Mobilization andfckLRPress-up Exercise on Pain ResponsefckLRand Lumbar Spine Extension in PeoplefckLRWith Nonspecific Low Back Pain, 2008, Physical Therapy, Vol 88(4) p485-493
- ↑ 9.0 9.1 May, S. and Donelson, R. Evidence- informed management of chronic low back pain with the McKenzie method. The Spine Journal. 2008;8:134-141
- ↑ 10.0 10.1 10.2 10.3 Garcia, A.N., Costa, L.C.M., Silva, T.M., Gondo, F.L.B., Cyrillo, F.N., Costa, F.M., Costa, L.O.P. Effectiveness of Back School Versus McKenzie Exercises in Patients with Chronic Nonspecific Low Back Pain: A Randomized Control Trial.2013;93(6):729-747
- ↑ Namnaqani FI, Mashabi AS, Yaseen KM, Alshehri MA. The effectiveness of McKenzie method compared to manual therapy for treating chronic low back pain: a systematic review. Journal of Musculoskeletal & Neuronal Interactions. 2019;19(4):492.
- ↑ Clare,H.A., Adams, R.and Maher, C.G. Reliability of the McKenzie Classification of patients with cervical and lumbar pain. Journal of Manipulative and Physiological Therapeutics. 2005;28(2):122-127
- ↑ Machado, L.A.C., Sperling de Souze, M.V., Ferreira, P.H. and Ferreira, M.L. The McKenzie Method for Low Back Pain: A systematic Review of the Literature with a Meta-Analysis Approach. SPINE. 2006;31(9): 254-262
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 14.6 Karayannis, N.V., Jull, G.A. and Hodges, P. Physiotherapy movement based classification approaches to low back pain: comparison of subgroups through review and developer/expert opinion. BioMed Central Musculoskeletal Disorders.2012;13:24
- ↑ Karayannis, N.V., Jull, G.A., and Hodges, P.W. (2012) Physiotherapy movement based classification approaches to low back pain: comparison of subgroups through review and developer/expert survey. BMC Musculoskeletal Disorders.13:24
- ↑ Sahrmann, S.A. (2001) Diagnosis and Treatment of Movement Impairment Syndromes. Mosby.
- ↑ Sahrmann Interviewed by L. Payne: 6th December 2012a part 1. Available at: http://www.youtube.com/watch?v=faEzHR5zLjs. [Accessed 13/01/14]
- ↑ Trudelle-Jackson, E., Sarvaiya-Shah, S. and Wang, S. Interrater reliability of a movement impairment-based classification system for lumbar spine syndromes in patients with low back pain. The Journal of Orthopaedic and Sports Physical Therapy 2009;38(6):371-376.
- ↑ Harris-Hayes, M., Van Dillen, L. and Sahrmann, S. Classification, treatment and outcomes of a patient with lumbar extension syndrome. Physiotherapy Theory and Practice 2005; 21(3):181-196.
- ↑ Van Dillen LR, Sahrmann SA, Norton BJ, et al. Effect of active limb movements on symptoms in patients with low back pain. J Orthop Sports Phys Ther 2001;31:402-413.
- ↑ Sahrmann Interviewed by L. Payne: 6th December 2012b part 3. Available at: http://www.youtube.com/watch?v=TsDbmAyzMd8. [Accessed 13/01/14]
- ↑ O’Sullivan, P. It’s time for change with the management of non-specificfckLRchronic low back pain. Br J Sports Med 2011. Available from: http://bjsm.bmj.com/content/early/2011/08/04/bjsm.2010.081638.full.htmlfckLR[Accessed 11/01/14]
- ↑ Ford, J. J. and Hahne, A. J. Pathoanatomy and classification of low back disorders. Manual Therapy 2013.18:165-168