Hypocalcemia: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
Hypocalcemia, a low bood calcium level, occurs when the concentration of free calcium ions in the blood falls below 4.4 mg/dL. | [[File:Nursing Home limited sun.jpg|thumb|Nursing home, limited sun exposure.]] | ||
Hypocalcemia, a low bood calcium level, occurs when the concentration of free calcium ions in the blood falls below 4.4 mg/dL. <ref>The Medical Dictionary. Available at http://medical-dictionary.thefreedictionary.com/hypocalcemia. Accessed on 2013 April 7</ref><ref name="medscape">Medscape Reference. Hypocalcemia. Available at http://emedicine.medscape.com/article/241893-overview. Accessed 2013 April 7.</ref> It can cause symptoms like tingling, muscle cramps, and [[Heart Arrhythmias: Assessment|heart arrhythmia]]<nowiki/>s, that can range from mild to life-threatening. | |||
Hypocalcemia is particularly a problem for people who are hospitalized or institutionalised.<ref name=":0" /> | |||
== Epidemiolgy == | == Epidemiolgy == | ||
Incidence and prevalence are difficult to estimate because hypocalcemia is a multifactorial diagnosis<ref name="clinicalkey">ClinicalKey. Hypocalcemia. Available at https://www.clinicalkey.com/topics/endocrinology/hypocalcemia.html. Accessed 2013 April 7</ref>. | Incidence and prevalence are difficult to estimate because hypocalcemia is a multifactorial diagnosis<ref name="clinicalkey">ClinicalKey. Hypocalcemia. Available at https://www.clinicalkey.com/topics/endocrinology/hypocalcemia.html. Accessed 2013 April 7</ref>. | ||
Hypocalcemia is particularly a problem for people who are hospitalized.<ref name=":0">Very well health Hypocalcemia Available: https://www.verywellhealth.com/hypocalcemia-overview-4774539<nowiki/>(accessed 3.4.2022)</ref>A 2018 study | Hypocalcemia is particularly a problem for people who are hospitalized.<ref name=":0">Very well health Hypocalcemia Available: https://www.verywellhealth.com/hypocalcemia-overview-4774539<nowiki/>(accessed 3.4.2022)</ref>A 2018 study found 27.72% of inpatients had Hypocalcemia<ref>Catalano A, Chilà D, Bellone F, Nicocia G, Martino G, Loddo I, Morabito N, Benvenga S, Loddo S. [https://www.sciencedirect.com/science/article/pii/S2214623718300413 Incidence of hypocalcemia and hypercalcemia in hospitalized patients: Is it changing?.] Journal of clinical & translational endocrinology. 2018 Sep 1;13:9-13. Available: https://www.sciencedirect.com/science/article/pii/S2214623718300413<nowiki/>(accessed 3.4.2022)</ref>. | ||
== Etiology == | == Etiology == | ||
Chronic hypocalcemia is commonly due to inadequate levels of parathyroid hormone (PTH) or [[Vitamin D Deficiency|vitamin D]] (from food or limited sun exposure) or due to resistance to these [[hormones]].<ref name=":1">Fong J, Khan A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3279267/ Hypocalcemia: updates in diagnosis and management for primary care]. Canadian family physician. 2012 Feb 1;58(2):158-62. Available;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3279267/ (accessed 3.4.2022)</ref>Low levels of PTH can be due to injury to the parathyroid gland from surgery or radiation treatment, autoimmune disease, or a genetic disease leading to low PTH. | Chronic hypocalcemia is commonly due to inadequate levels of parathyroid hormone (PTH) or [[Vitamin D Deficiency|vitamin D]] (from food or limited sun exposure) or due to resistance to these [[hormones]].<ref name=":1">Fong J, Khan A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3279267/ Hypocalcemia: updates in diagnosis and management for primary care]. Canadian family physician. 2012 Feb 1;58(2):158-62. Available;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3279267/ (accessed 3.4.2022)</ref>Low levels of PTH can be due to injury to the parathyroid gland from surgery or radiation treatment, autoimmune disease, or a genetic disease leading to low PTH. | ||
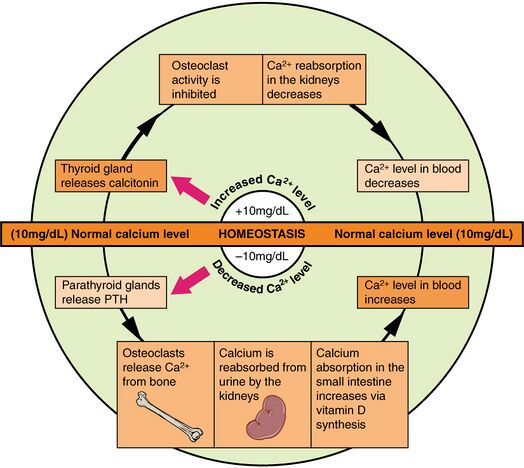
Other causes include:Medical conditions eg Celiac disease, pancreatitis, and kidney or liver disease; Certain medicines, eg diuretics, proton pump inhibitors, medicines to prevent seizures<ref name=":0" /> | Other causes include:Medical conditions eg Celiac disease, pancreatitis, and kidney or liver disease; Certain medicines, eg diuretics, proton pump inhibitors, medicines to prevent seizures<ref name=":0" />[[File:Calcium Homeostasis.jpeg|thumb|Calcium Homeostasis|alt=|center|524x524px]] | ||
== Clinical Presentation == | == Clinical Presentation == | ||
Sometimes symptoms are relatively mild, other times they may cause life-threatening problems. In someone who is already critically ill, having hypocalcemia may increase a person’s risk of death.<ref name=":0" /> | Sometimes symptoms are relatively mild, other times they may cause life-threatening problems. In someone who is already critically ill, having hypocalcemia may increase a person’s risk of death.<ref name=":0" /> | ||
Revision as of 07:21, 3 April 2022
Original Editors - Robbie Esterle & Ryan Hamilton from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Robert Esterle, Ryan Hamilton, Lucinda hampton, Admin, Elaine Lonnemann, Kim Jackson, Wendy Walker and 127.0.0.1
Introduction[edit | edit source]
Hypocalcemia, a low bood calcium level, occurs when the concentration of free calcium ions in the blood falls below 4.4 mg/dL. [1][2] It can cause symptoms like tingling, muscle cramps, and heart arrhythmias, that can range from mild to life-threatening.
Hypocalcemia is particularly a problem for people who are hospitalized or institutionalised.[3]
Epidemiolgy[edit | edit source]
Incidence and prevalence are difficult to estimate because hypocalcemia is a multifactorial diagnosis[4].
Hypocalcemia is particularly a problem for people who are hospitalized.[3]A 2018 study found 27.72% of inpatients had Hypocalcemia[5].
Etiology[edit | edit source]
Chronic hypocalcemia is commonly due to inadequate levels of parathyroid hormone (PTH) or vitamin D (from food or limited sun exposure) or due to resistance to these hormones.[6]Low levels of PTH can be due to injury to the parathyroid gland from surgery or radiation treatment, autoimmune disease, or a genetic disease leading to low PTH.
Other causes include:Medical conditions eg Celiac disease, pancreatitis, and kidney or liver disease; Certain medicines, eg diuretics, proton pump inhibitors, medicines to prevent seizures[3]
Clinical Presentation[edit | edit source]
Sometimes symptoms are relatively mild, other times they may cause life-threatening problems. In someone who is already critically ill, having hypocalcemia may increase a person’s risk of death.[3]
- Acute hypocalcemia can result in severe symptoms requiring hospitalization
- Patients who gradually develop hypocalcemia are more likely to be asymptomatic.
- Symptoms of hypocalcemia most commonly include paresthesia, muscle spasms, cramps, tetany, circumoral numbness, and seizures.
- Hypocalcemia can also present with laryngospasm, neuromuscular irritability, cognitive impairment, personality disturbances, prolonged QT intervals, electrocardiographic changes that mimic myocardial infarction, or heart failure[6]
Diagnosis[edit | edit source]
Involves
- Evaluation of signs, symptoms, and the medicines history.
- Objective: Chvostek sign, facial twitch obtained by tapping the distribution of the facial nerve in front of the tragus. Caused by mechanical irritability of peripheral nerves. It is indicative of hypocalcaemia and is the most reliable test for hypocalcaemia.
- Blood tests to check calcium, magnesium, and hormone levels.
Treatment[edit | edit source]
Treatment focuses on oral calcium and vitamin D supplements, as well as magnesium if deficiency is present. Treatment can be further intensified with thiazide diuretics, phosphate binders, and a low-salt and low-phosphorus diet when treating hypocalcemia secondary to hypoparathyroidism. Acute and life-threatening calcium deficit requires treatment with intravenous calcium.[6]
Physiotherapy[edit | edit source]
Due to the nature of hypocalcemia being secondary to a primary disease state, physical therapy management includes recognition of the signs and symptoms thereof. Appropriate action taken and appropriate referral.
Case Reports/ Case Studies[edit | edit source]
- Fong J, Khan A. Hypocalcemia: updates in diagnosis and management for primary care. Can Fam Physician. 2012;58(2):158-62. www.cfp.ca/content/58/2/158.full
References[edit | edit source]
- ↑ The Medical Dictionary. Available at http://medical-dictionary.thefreedictionary.com/hypocalcemia. Accessed on 2013 April 7
- ↑ Medscape Reference. Hypocalcemia. Available at http://emedicine.medscape.com/article/241893-overview. Accessed 2013 April 7.
- ↑ 3.0 3.1 3.2 3.3 Very well health Hypocalcemia Available: https://www.verywellhealth.com/hypocalcemia-overview-4774539(accessed 3.4.2022)
- ↑ ClinicalKey. Hypocalcemia. Available at https://www.clinicalkey.com/topics/endocrinology/hypocalcemia.html. Accessed 2013 April 7
- ↑ Catalano A, Chilà D, Bellone F, Nicocia G, Martino G, Loddo I, Morabito N, Benvenga S, Loddo S. Incidence of hypocalcemia and hypercalcemia in hospitalized patients: Is it changing?. Journal of clinical & translational endocrinology. 2018 Sep 1;13:9-13. Available: https://www.sciencedirect.com/science/article/pii/S2214623718300413(accessed 3.4.2022)
- ↑ 6.0 6.1 6.2 Fong J, Khan A. Hypocalcemia: updates in diagnosis and management for primary care. Canadian family physician. 2012 Feb 1;58(2):158-62. Available;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3279267/ (accessed 3.4.2022)