Male Sexual Dysfunction: Difference between revisions
mNo edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
== Introduction == | == Introduction == | ||
[[File:Sexual activity.png|thumb|400x400px|Three parts of sexual activity]] | [[File:Sexual activity.png|thumb|400x400px|Three parts of sexual activity]] | ||
When treating sexual dysfunction, a medical professional must look at the broader prospective of the patient's sexual activity in order to accurately diagnose and treat the underlying causes of the dysfunction. | When treating sexual dysfunction, a medical professional must look at the broader prospective of the patient's sexual activity in order to accurately diagnose and treat the underlying causes of the dysfunction. Sexual activity includes a patient's physiological sexual functioning, their sexual identity, and their sexual relationship. | ||
It is imperative to have open and respectful conversations with the patient regarding these very personal issues order to provide quality and appropriate care. | It is imperative to have open and respectful conversations with the patient regarding these very personal issues in order to provide quality and appropriate care. A medical professional working in this specialised field must be inclusive and make all patients feel comfortable and respected. This extends from the words a therapist uses to describe a patient's sexual orientation, gender identity, and or expression, to how the clinic is setup to provide maximal privacy during patient evaluations, treatments, and consultations. Please read this article for recommendations on how to [[Introduction to Men's Health Physiotherapy#Physiotherapy Scope of Practice|setup a men's health clinic.]] | ||
=== Sexuality === | === Sexuality === | ||
<blockquote>'''Sexuality''' is a central aspect of being human throughout life and encompasses sex, gender identities and roles, sexual orientation, eroticism, pleasure, intimacy and reproduction. Sexuality is experienced and expressed in thoughts, fantasies, desires, beliefs, attitudes, values, behaviours, practices, roles and relationships. While sexuality can include all of these dimensions, not all of them are always experienced or expressed. Sexuality is influenced by the interaction of biological, psychological, social, economic, political, cultural, ethical, legal, historical, religious and spiritual factors.<ref>World Health Organization. Gender and human rights. Available from: https://www.who.int/reproductivehealth/topics/gender_rights/sexual_health/en/ (accessed 14/03/2022).</ref></blockquote>Just as an understanding of pelvic anatomy is needed for proper pelvic floor physiotherapy, an understanding of appropriate terminology to use for gender identity and sexual orientation is needed when providing pelvic health physiotherapy. | <blockquote>'''Sexuality''' is a central aspect of being human throughout life and encompasses sex, gender identities and roles, sexual orientation, eroticism, pleasure, intimacy and reproduction. Sexuality is experienced and expressed in thoughts, fantasies, desires, beliefs, attitudes, values, behaviours, practices, roles and relationships. While sexuality can include all of these dimensions, not all of them are always experienced or expressed. Sexuality is influenced by the interaction of biological, psychological, social, economic, political, cultural, ethical, legal, historical, religious and spiritual factors.<ref>World Health Organization. Gender and human rights. Available from: https://www.who.int/reproductivehealth/topics/gender_rights/sexual_health/en/ (accessed 14/03/2022).</ref></blockquote>Just as an understanding of pelvic anatomy is needed for proper pelvic floor physiotherapy, an understanding of appropriate terminology to use for gender identity and sexual orientation is needed when providing pelvic health physiotherapy. It is also important to know the appropriate pronouns to use, especially when working with gender nonbinary and transgender patients. Please read this article for more in-depth information on [https://www.physio-pedia.com/Considerations_for_Working_with_LGBTQIA+_Refugees?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#Terminology sexual orientation, gender identity, and gender expression]. | ||
The term ''sex'' is used to refer to a person’s biological maleness or femaleness, and the term ''gender'' to the nonphysiological aspects of being male or female– the cultural expectations and roles for femininity and masculinity.<ref>Lips HM. [https://www.google.com/books/edition/Sex_and_Gender/xgjaDwAAQBAJ?hl=en&gbpv=1&dq=Lips+HM.+Sex+and+gender:+An+introduction.+Waveland+Press%3B+2020+Apr+10.&pg=PR1&printsec=frontcover#v=onepage&q=Lips%20HM.%20Sex%20and%20gender%3A%20An%20introduction.%20Waveland%20Press%3B%202020%20Apr%2010.&f=false Sex and gender: An introduction]. Waveland Press; 2020 Apr 10.</ref> | The term ''sex'' is used to refer to a person’s biological maleness or femaleness, and the term ''gender'' to the nonphysiological aspects of being male or female– the cultural expectations and roles for femininity and masculinity.<ref>Lips HM. [https://www.google.com/books/edition/Sex_and_Gender/xgjaDwAAQBAJ?hl=en&gbpv=1&dq=Lips+HM.+Sex+and+gender:+An+introduction.+Waveland+Press%3B+2020+Apr+10.&pg=PR1&printsec=frontcover#v=onepage&q=Lips%20HM.%20Sex%20and%20gender%3A%20An%20introduction.%20Waveland%20Press%3B%202020%20Apr%2010.&f=false Sex and gender: An introduction]. Waveland Press; 2020 Apr 10.</ref> This article will focus on male sexual dysfunction and how it can be addressed by men's health physiotherapy. The term “men” will refer to biological males and “women” for biological females for the remainder of this page. | ||
== Male Sexual Dysfunction == | == Male Sexual Dysfunction == | ||
| Line 23: | Line 23: | ||
* Orgasmic ability and quality | * Orgasmic ability and quality | ||
When discussing sexual dysfunction, a physiotherapy patient interview may uncover a change or alteration in one of these four basic sexual functions. | When discussing sexual dysfunction, a physiotherapy patient interview may uncover a change or alteration in one of these four basic sexual functions. The treatment of male sexual dysfunction often requires a multidisciplinary approach, involving multiple treatment techniques and interventions from various healthcare and mental health providers.<ref name=":0">Roscher, P, Men's Health. Male Sexual Dysfunction. Physioplus. March 2022.</ref> | ||
=== Hypoactive Sexual Desire === | === Hypoactive Sexual Desire === | ||
| Line 33: | Line 33: | ||
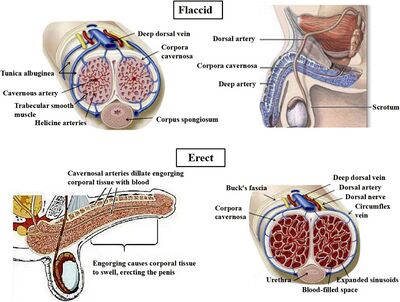
There are different types of erections; reflexogenic, psychogenic and nocturnal: | There are different types of erections; reflexogenic, psychogenic and nocturnal: | ||
* Reflexogenic erections occur when the penis is physically stimulated | * Reflexogenic erections occur when the penis is physically stimulated. | ||
* Psychogenic erections from other stimulation such as visual, auditory or psychological inputs. | * Psychogenic erections from other stimulation such as visual, auditory or psychological inputs. | ||
* Nocturnal erections occur in men every night with about 5-8 per night and can last up to 30 minutes each. | * Nocturnal erections occur in men every night with about 5-8 per night and can last up to 30 minutes each. | ||
| Line 42: | Line 42: | ||
* Problems with erectile function can come from physical and psychological problems. | * Problems with erectile function can come from physical and psychological problems. | ||
* When a man’s nocturnal erections stop it can be used as a diagnostic factor in determining a physical cause of the erectile dysfunction | * When a man’s nocturnal erections stop, it can be used as a diagnostic factor in determining a physical cause of the erectile dysfunction<span class="reference" id="cite_ref-4"></span>.<ref>Briganti A, Salonia A, Zanni G, Fabbri F, Saccà A, Bertini R, Suardi N, Fantini GV, Rigatti P, Montorsi F. [http://www.sciencedirect.com/science/article/pii/S1570912404000212 Erectile dysfunction and radical prostatectomy: an update]. EAU update series. 2004 Jun 1;2(2):84-92.</ref> | ||
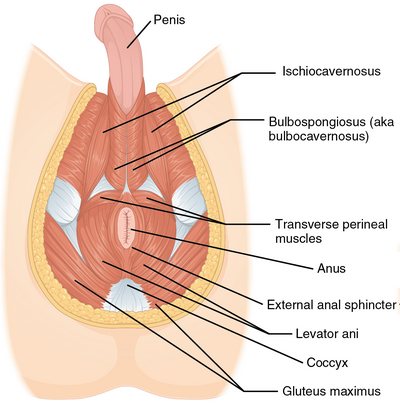
* [[File:Male pelvic floor superficial.png|thumb|417x417px|Male superficial pelvic floor muscles]]The [[Pelvic Floor Anatomy|pelvic floor]] muscles, in particular, the bulbospongiosus and ischiocavernosus, play an important role in penile rigidity and injury or weakness can play a role in erectile dysfunction<span class="reference" id="cite_ref-:2_5-0"></span>.<ref name=":2">Cohen D, Gonzalez J, Goldstein I. [http://www.smr.jsexmed.org/article/S2050-0521(15)00002-5/fulltext The role of pelvic floor muscles in male sexual dysfunction and pelvic pain]. Sexual medicine reviews. 2016 Jan 1;4(1):53-62.</ref> | * [[File:Male pelvic floor superficial.png|thumb|417x417px|Male superficial pelvic floor muscles]]The [[Pelvic Floor Anatomy|pelvic floor]] muscles, in particular, the bulbospongiosus and ischiocavernosus, play an important role in penile rigidity and injury or weakness can play a role in erectile dysfunction<span class="reference" id="cite_ref-:2_5-0"></span>.<ref name=":2">Cohen D, Gonzalez J, Goldstein I. [http://www.smr.jsexmed.org/article/S2050-0521(15)00002-5/fulltext The role of pelvic floor muscles in male sexual dysfunction and pelvic pain]. Sexual medicine reviews. 2016 Jan 1;4(1):53-62.</ref> | ||
| Line 48: | Line 48: | ||
'''Aspects of erectile dysfunction''': | '''Aspects of erectile dysfunction''': | ||
# | # Ability to achieve an erection | ||
# | # Ability to maintain an erection | ||
# | # Ability to achieve adequate erection quality e.g. hardness | ||
<ref name=":0" /> | <ref name=":0" /> | ||
=== Ejaculation | === Ejaculation Issues === | ||
'''Ejaculation''' occurs when the smooth muscle of the prostate contract and the urethra smooth muscles relax to allow the ejaculate to enter the urethra. Thereafter a strong involuntary contraction of the bulbospongiosus expels the ejaculate.<ref name=":2" /> | '''Ejaculation''' occurs when the smooth muscle of the prostate contract and the urethra smooth muscles relax to allow the ejaculate to enter the urethra. Thereafter a strong involuntary contraction of the bulbospongiosus expels the ejaculate.<ref name=":2" /> | ||
| Line 63: | Line 63: | ||
'''Types of ejaculation issues''': | '''Types of ejaculation issues''': | ||
* ''Retrograde ejaculation'' results in a reduced volume of anterograde ejaculate during sexual climax or the detection of semen in the post-ejaculatory urine.<ref>Gild P, Dahlem R, Pompe RS, Soave A, Vetterlein MW, Ludwig TA, Maurer V, Marks P, Ahyai SA, Chun FK, Lenke L. [https://onlinelibrary.wiley.com/doi/full/10.1111/andr.12887 Retrograde ejaculation after holmium laser enucleation of the prostate (HoLEP)—Impact on sexual function and evaluation of patient bother using validated questionnaires]. Andrology. 2020 Nov;8(6):1779-86.</ref> | * ''Retrograde ejaculation'' results in a reduced volume of anterograde ejaculate during sexual climax or the detection of semen in the post-ejaculatory urine.<ref>Gild P, Dahlem R, Pompe RS, Soave A, Vetterlein MW, Ludwig TA, Maurer V, Marks P, Ahyai SA, Chun FK, Lenke L. [https://onlinelibrary.wiley.com/doi/full/10.1111/andr.12887 Retrograde ejaculation after holmium laser enucleation of the prostate (HoLEP)—Impact on sexual function and evaluation of patient bother using validated questionnaires]. Andrology. 2020 Nov;8(6):1779-86.</ref> It can be a consequence of a prostatectomy due to the removal of the internal urethral sphincter allowing semen to move into the bladder rather than into the urethra.<ref name=":0" /> | ||
* ''Premature ejaculation'' is the most common type of ejaculation dysfunction. | * ''Premature ejaculation'' is the most common type of ejaculation dysfunction. It involves ejaculation within 30 seconds of either sexual stimulation or penetration.<ref name=":0" /> | ||
* ''Delayed ejaculation'' involves an extended amount of time needed prior to ejaculation.<ref name=":0" /> | * ''Delayed ejaculation'' involves an extended amount of time needed prior to ejaculation.<ref name=":0" /> | ||
| Line 75: | Line 75: | ||
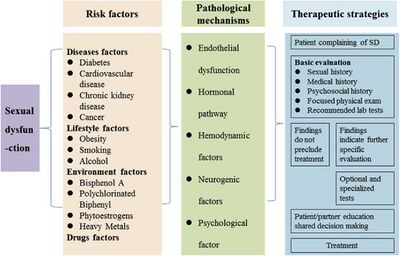
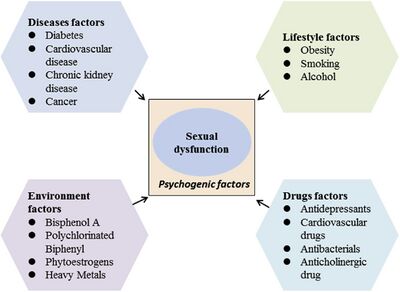
== Sexual Dysfunction Risk Factors == | == Sexual Dysfunction Risk Factors == | ||
[[File:Sexual dysfunction risk factors.jpeg|thumb|400x400px|Sexual dysfunction risk factors]] | [[File:Sexual dysfunction risk factors.jpeg|thumb|400x400px|Sexual dysfunction risk factors]] | ||
'''Health | '''Health conditions that increase the risk of sexual dysfunction in men:''' | ||
* [[Diabetes]]<ref name=":0" /> | * [[Diabetes]]<ref name=":0" /> | ||
* [[ | * [[Cardiovascular Disease|Cardiovascular disease]]<ref name=":0" /><ref name=":3">Chen L, Shi GR, Huang DD, Li Y, Ma CC, Shi M, Su BX, Shi GJ. [https://www.sciencedirect.com/science/article/pii/S0753332218353289?via%3Dihub Male sexual dysfunction: a review of literature on its pathological mechanisms, potential risk factors, and herbal drug intervention.] Biomedicine & Pharmacotherapy. 2019 Apr 1;112:108585.</ref> | ||
* [[Hypertension]]<ref name=":3" /> | * [[Hypertension]]<ref name=":3" /> | ||
* [[Hyperlipidemia]]<ref name=":3" /> | * [[Hyperlipidemia]]<ref name=":3" /> | ||
* Chronic kidney disease<ref name=":0" /><ref name=":3" /> | * Chronic kidney disease<ref name=":0" /><ref name=":3" /> | ||
* Cancer, especially [[Prostate Cancer|prostate cancer]]<ref name=":0" /><ref name=":3" /> | * Cancer, especially [[Prostate Cancer|prostate cancer]]<ref name=":0" /><ref name=":3" /> | ||
* [[Obesity]] | * [[Obesity]] - has a significant relationship with ED<ref name=":0" /> | ||
* Drug side-effects<ref name=":3" /> | * Drug side-effects<ref name=":3" /> | ||
'''Lifestyle factors that increase risk of sexual dysfunction in men:''' | '''Lifestyle factors that increase the risk of sexual dysfunction in men:''' | ||
* Smoking<ref name=":0" /> | * Smoking<ref name=":0" /> | ||
| Line 94: | Line 94: | ||
* Stress<ref name=":3" /> | * Stress<ref name=":3" /> | ||
'''Age''' also plays a factor in sexual dysfunction development. | '''Age''' also plays a factor in sexual dysfunction development. Younger patients tend to present with premature ejaculation, hard flaccid syndrome, pelvic pain, pain with orgasm. Older patients tend to present with ED and many of the above listed health conditions, which increase their risk for developing sexual dysfunction such as cardiovascular disease or prostate issues.<ref name=":0" /> | ||
[[File:Sexual dysfunction psychogenic factors.jpeg|thumb|400x400px|Sexual dysfunction psychogenic factors]] | [[File:Sexual dysfunction psychogenic factors.jpeg|thumb|400x400px|Sexual dysfunction psychogenic factors]] | ||
'''Pathological mechanisms of male sexual dysfunction:''' | '''Pathological mechanisms of male sexual dysfunction:''' | ||
| Line 105: | Line 105: | ||
== Biopsychosocial Model and Healthcare Professional Training == | == Biopsychosocial Model and Healthcare Professional Training == | ||
Please read here for more in-depth information on the [[Male Pelvic Pain|biopsychosocial model with regards to men's health]]. Please read here for more general information | Please read here for more in-depth information on the [[Male Pelvic Pain|biopsychosocial model with regards to men's health]]. Please read here for more general information on the [[Biopsychosocial Model|biopsychosocial model]]. | ||
Sexual health needs are more neglected by medical professionals than mental health.<ref name=":0" />A 2019 systematic review | Sexual health needs are more neglected by medical professionals than mental health.<ref name=":0" /> A 2019 systematic review<ref name=":4" /> suggests that sexual health education provided by nurses to patients was affected by: | ||
* Lack of knowledge about sexual health | * Lack of knowledge about sexual health | ||
* The healthcare providers' attitudes and beliefs that sexual health care is private and not a priority | * The healthcare providers' attitudes and beliefs that sexual health care is private and not a priority | ||
* The healthcare providers’ comfort discussing sexual health | * The healthcare providers’ comfort discussing sexual health | ||
* Perceived barriers related to time, responsibility and organisational support<ref>Fennell R, Grant B. [https://onlinelibrary.wiley.com/doi/abs/10.1111/jocn.14900 Discussing sexuality in health care: A systematic review.] Journal of clinical nursing. 2019 Sep;28(17-18):3065-76.</ref> | * Perceived barriers related to time, responsibility and organisational support<ref name=":4">Fennell R, Grant B. [https://onlinelibrary.wiley.com/doi/abs/10.1111/jocn.14900 Discussing sexuality in health care: A systematic review.] Journal of clinical nursing. 2019 Sep;28(17-18):3065-76.</ref> | ||
The healthcare providers' ability to comfortably and professionally ask in-depth questions | The healthcare providers' ability to comfortably and professionally ask in-depth questions about a patient's sexual activity can be vital in providing appropriate pelvic health care and interventions. For example: when evaluating and treating a patient with complaints of ED, it is important to know if their sexual partner is male or female. This is due to the amount of penile quality needed to penetrate an anus vs a vagina.<ref name=":0" /> | ||
== Male Pelvic Floor Physiotherapy == | == Male Pelvic Floor Physiotherapy == | ||
Pelvic floor physiotherapy treatments and interventions are: | Pelvic floor physiotherapy treatments and interventions are: | ||
* | * Conservative | ||
* | * Modifiable | ||
* | * Noninvasive | ||
* | * Non-pharmacological | ||
* | * Non-surgical | ||
* | * Can be used for a wide range of men's sexual health conditions | ||
<ref name=":0" /> | <ref name=":0" /> | ||
=== Pelvic Floor Assessment Overview === | === Pelvic Floor Assessment Overview === | ||
90% of men's sexual health physiotherapy involves treatment of the pelvic floor. Proper assessment is needed to determine | 90% of men's sexual health physiotherapy involves treatment of the pelvic floor. Proper assessment is needed to determine the tone and neuromuscular control of the male pelvic floor muscles. Often, when asked about pelvic floor exercises, most people think about Kegel exercises, which are designed to strengthen weakened pelvic floor muscles. However, what if the source of sexual dysfunction is a hypertrophic muscle rather than a weakened one? Thus, proper pelvic floor physiotherapy assessment is key. The functional muscle length of the pelvic floor muscles can be shortened when they are hypertrophic, and continuing to strengthen an already tight pelvic floor muscle can lead to further dysfunction.<ref name=":0" /> | ||
In the following video, the physical therapist discusses how assessment of | In the following video, the physical therapist discusses how assessment of pelvic floor tone can help determine treatments for ED. | ||
{{#ev:youtube| HvrCm8EJcF0 |500}}<ref>YouTube. Erectile Dysfunction and Your Pelvic Floor | Pelvic Health & Rehabilitation Center. Available from: https://www.youtube.com/watch?v=HvrCm8EJcF0 [last accessed 16/03/2022]</ref> | {{#ev:youtube| HvrCm8EJcF0 |500}}<ref>YouTube. Erectile Dysfunction and Your Pelvic Floor | Pelvic Health & Rehabilitation Center. Available from: https://www.youtube.com/watch?v=HvrCm8EJcF0 [last accessed 16/03/2022]</ref> | ||
The gold standard to assessment pelvic floor tone is through an internal assessment. | The gold standard to assessment pelvic floor tone is through an internal assessment. ''This is a highly skilled procedure which requires specialisation and advanced training. An internal assessment should not be performed until the physiotherapist is clinically competent.'' | ||
When performing an internal assessment, the physiotherapist is assessing: | When performing an internal assessment, the physiotherapist is assessing: | ||
* | * Muscle strength | ||
* | * Muscle tone | ||
* | * Muscle support | ||
* | * Neuromuscular control | ||
* | * Trigger point sensitivity | ||
<ref name=":0" /> | <ref name=":0" /> | ||
Real-time ultrasound, when taken from the transperineal view, allows the physiotherapist to assess pelvic floor muscle activity in real time. | Real-time ultrasound, when taken from the transperineal view, allows the physiotherapist to assess pelvic floor muscle activity in real time. Real-time ultrasound can also be used to provide visual cues for the patient during therapy interventions.<ref name=":0" /> | ||
The following short video is a demonstration of real-time ultrasound visualisation of | The following short video is a demonstration of a real-time ultrasound visualisation of male pelvic floor muscle contractions. | ||
{{#ev:youtube| E4dx8f1V1Zs |500}}<ref>YouTube. Men's Health Ultrasound - Male Pelvic Floor Contraction. Available from: https://www.youtube.com/watch?v=E4dx8f1V1Zs [last accessed 16/03/2022]</ref> | {{#ev:youtube| E4dx8f1V1Zs |500}}<ref>YouTube. Men's Health Ultrasound - Male Pelvic Floor Contraction. Available from: https://www.youtube.com/watch?v=E4dx8f1V1Zs [last accessed 16/03/2022]</ref> | ||
=== Pelvic Floor Treatment Overview === | === Pelvic Floor Treatment Overview === | ||
Treatments will be multifaceted and may involve: | Treatments will be multifaceted and may involve:<ref name=":0" /> | ||
* Education on the connection between sexual dysfunction and pelvic floor impairments | * Education on the connection between sexual dysfunction and pelvic floor impairments | ||
| Line 160: | Line 160: | ||
* Behavioral considerations | * Behavioral considerations | ||
* Mindfulness training and exercises | * Mindfulness training and exercises | ||
* | * The inclusion of the patient's partner | ||
Working with an interdisciplinary team provides the patient with support and proper treatment. | Working with an interdisciplinary team provides the patient with support and proper treatment. Having strong referral sources is important to provide the holistic care needed by this patient population. | ||
Sexual recovery takes time, patience, and hard work by both the patient, their partner, and their treatment team.<ref name=":0" /> | Sexual recovery takes time, patience, and hard work by both the patient, their partner, and their treatment team.<ref name=":0" /> | ||
| Line 184: | Line 184: | ||
[[Category:Physioplus Content]] | [[Category:Physioplus Content]] | ||
[[Category:Mens Health]] | [[Category:Mens Health]] | ||
[[Category:Pelvic Health]] | |||
Revision as of 11:03, 22 March 2022
Top Contributors - Stacy Schiurring, Kim Jackson, Lucinda hampton and Jess Bell
This page aims to provide an introductory discussion of men's health physiotherapy with regards to male sexual dysfunction. Please note that further training is required through a reputable pelvic health education company before attempting the techniques discussed in this page. See the Resources section at the bottom of this page for links to pelvic and men's health special interest groups.
Introduction[edit | edit source]
When treating sexual dysfunction, a medical professional must look at the broader prospective of the patient's sexual activity in order to accurately diagnose and treat the underlying causes of the dysfunction. Sexual activity includes a patient's physiological sexual functioning, their sexual identity, and their sexual relationship.
It is imperative to have open and respectful conversations with the patient regarding these very personal issues in order to provide quality and appropriate care. A medical professional working in this specialised field must be inclusive and make all patients feel comfortable and respected. This extends from the words a therapist uses to describe a patient's sexual orientation, gender identity, and or expression, to how the clinic is setup to provide maximal privacy during patient evaluations, treatments, and consultations. Please read this article for recommendations on how to setup a men's health clinic.
Sexuality[edit | edit source]
Sexuality is a central aspect of being human throughout life and encompasses sex, gender identities and roles, sexual orientation, eroticism, pleasure, intimacy and reproduction. Sexuality is experienced and expressed in thoughts, fantasies, desires, beliefs, attitudes, values, behaviours, practices, roles and relationships. While sexuality can include all of these dimensions, not all of them are always experienced or expressed. Sexuality is influenced by the interaction of biological, psychological, social, economic, political, cultural, ethical, legal, historical, religious and spiritual factors.[1]
Just as an understanding of pelvic anatomy is needed for proper pelvic floor physiotherapy, an understanding of appropriate terminology to use for gender identity and sexual orientation is needed when providing pelvic health physiotherapy. It is also important to know the appropriate pronouns to use, especially when working with gender nonbinary and transgender patients. Please read this article for more in-depth information on sexual orientation, gender identity, and gender expression.
The term sex is used to refer to a person’s biological maleness or femaleness, and the term gender to the nonphysiological aspects of being male or female– the cultural expectations and roles for femininity and masculinity.[2] This article will focus on male sexual dysfunction and how it can be addressed by men's health physiotherapy. The term “men” will refer to biological males and “women” for biological females for the remainder of this page.
Male Sexual Dysfunction[edit | edit source]
Normal sexual function in men relies on the complex interaction between biological, emotional, cognitive, behavioural, contextual and interpersonal factors.[3]
There are multiple physiological processes involved in male sexual function to include:
- Sexual desire (libido)
- Erectile functioning
- Ejaculation
- Orgasmic ability and quality
When discussing sexual dysfunction, a physiotherapy patient interview may uncover a change or alteration in one of these four basic sexual functions. The treatment of male sexual dysfunction often requires a multidisciplinary approach, involving multiple treatment techniques and interventions from various healthcare and mental health providers.[4]
Hypoactive Sexual Desire[edit | edit source]
Sexual desire relies on a variety of factors both physical and psychological. Testosterone levels play an important role in physiological libido.[5]
Erectile Dysfunction[edit | edit source]
Erectile function forms an important part of a man’s sexual function, but it is only a part of the picture. A normal erection depends on a sequence of physiological, neural, vascular, metabolic and endocrine events.
There are different types of erections; reflexogenic, psychogenic and nocturnal:
- Reflexogenic erections occur when the penis is physically stimulated.
- Psychogenic erections from other stimulation such as visual, auditory or psychological inputs.
- Nocturnal erections occur in men every night with about 5-8 per night and can last up to 30 minutes each.
Erectile dysfunction (ED) is a component of male sexual dysfunction and can be defined as the persistent inability to achieve or maintain an erection firm enough or lasting long enough to participate in sexual activities.[6]
- Problems with erectile function can come from physical and psychological problems.
- When a man’s nocturnal erections stop, it can be used as a diagnostic factor in determining a physical cause of the erectile dysfunction.[7]
- The pelvic floor muscles, in particular, the bulbospongiosus and ischiocavernosus, play an important role in penile rigidity and injury or weakness can play a role in erectile dysfunction.[8]
Aspects of erectile dysfunction:
- Ability to achieve an erection
- Ability to maintain an erection
- Ability to achieve adequate erection quality e.g. hardness
Ejaculation Issues[edit | edit source]
Ejaculation occurs when the smooth muscle of the prostate contract and the urethra smooth muscles relax to allow the ejaculate to enter the urethra. Thereafter a strong involuntary contraction of the bulbospongiosus expels the ejaculate.[8]
- The prostate is responsible for the production of seminal fluid which makes up the majority of the ejaculate.
- When the prostate is removed or affected by radiation there is often a significant loss or absence of ejaculate.[5]
Types of ejaculation issues:
- Retrograde ejaculation results in a reduced volume of anterograde ejaculate during sexual climax or the detection of semen in the post-ejaculatory urine.[9] It can be a consequence of a prostatectomy due to the removal of the internal urethral sphincter allowing semen to move into the bladder rather than into the urethra.[4]
- Premature ejaculation is the most common type of ejaculation dysfunction. It involves ejaculation within 30 seconds of either sexual stimulation or penetration.[4]
- Delayed ejaculation involves an extended amount of time needed prior to ejaculation.[4]
Orgasmic Dysfunction[edit | edit source]
- Mediated by the autonomic nervous system but there is also cortical involvement.
- The pelvic floor muscles play an important role in orgasm.
- Damage to the nerves and spasm of the muscles can play a role in the orgasmic dysfunction.[5]
Sexual Dysfunction Risk Factors[edit | edit source]
Health conditions that increase the risk of sexual dysfunction in men:
- Diabetes[4]
- Cardiovascular disease[4][10]
- Hypertension[10]
- Hyperlipidemia[10]
- Chronic kidney disease[4][10]
- Cancer, especially prostate cancer[4][10]
- Obesity - has a significant relationship with ED[4]
- Drug side-effects[10]
Lifestyle factors that increase the risk of sexual dysfunction in men:
- Smoking[4]
Age also plays a factor in sexual dysfunction development. Younger patients tend to present with premature ejaculation, hard flaccid syndrome, pelvic pain, pain with orgasm. Older patients tend to present with ED and many of the above listed health conditions, which increase their risk for developing sexual dysfunction such as cardiovascular disease or prostate issues.[4]
Pathological mechanisms of male sexual dysfunction:
- Endothelial dysfunction[4][10]
- Neurogenic factors[4][10]
- Hormonal pathway[4][10]
- Haemodynamic factors[4][10]
- Psychosocial factors[4]
Biopsychosocial Model and Healthcare Professional Training[edit | edit source]
Please read here for more in-depth information on the biopsychosocial model with regards to men's health. Please read here for more general information on the biopsychosocial model.
Sexual health needs are more neglected by medical professionals than mental health.[4] A 2019 systematic review[11] suggests that sexual health education provided by nurses to patients was affected by:
- Lack of knowledge about sexual health
- The healthcare providers' attitudes and beliefs that sexual health care is private and not a priority
- The healthcare providers’ comfort discussing sexual health
- Perceived barriers related to time, responsibility and organisational support[11]
The healthcare providers' ability to comfortably and professionally ask in-depth questions about a patient's sexual activity can be vital in providing appropriate pelvic health care and interventions. For example: when evaluating and treating a patient with complaints of ED, it is important to know if their sexual partner is male or female. This is due to the amount of penile quality needed to penetrate an anus vs a vagina.[4]
Male Pelvic Floor Physiotherapy[edit | edit source]
Pelvic floor physiotherapy treatments and interventions are:
- Conservative
- Modifiable
- Noninvasive
- Non-pharmacological
- Non-surgical
- Can be used for a wide range of men's sexual health conditions
Pelvic Floor Assessment Overview[edit | edit source]
90% of men's sexual health physiotherapy involves treatment of the pelvic floor. Proper assessment is needed to determine the tone and neuromuscular control of the male pelvic floor muscles. Often, when asked about pelvic floor exercises, most people think about Kegel exercises, which are designed to strengthen weakened pelvic floor muscles. However, what if the source of sexual dysfunction is a hypertrophic muscle rather than a weakened one? Thus, proper pelvic floor physiotherapy assessment is key. The functional muscle length of the pelvic floor muscles can be shortened when they are hypertrophic, and continuing to strengthen an already tight pelvic floor muscle can lead to further dysfunction.[4]
In the following video, the physical therapist discusses how assessment of pelvic floor tone can help determine treatments for ED.
The gold standard to assessment pelvic floor tone is through an internal assessment. This is a highly skilled procedure which requires specialisation and advanced training. An internal assessment should not be performed until the physiotherapist is clinically competent.
When performing an internal assessment, the physiotherapist is assessing:
- Muscle strength
- Muscle tone
- Muscle support
- Neuromuscular control
- Trigger point sensitivity
Real-time ultrasound, when taken from the transperineal view, allows the physiotherapist to assess pelvic floor muscle activity in real time. Real-time ultrasound can also be used to provide visual cues for the patient during therapy interventions.[4]
The following short video is a demonstration of a real-time ultrasound visualisation of male pelvic floor muscle contractions.
Pelvic Floor Treatment Overview[edit | edit source]
Treatments will be multifaceted and may involve:[4]
- Education on the connection between sexual dysfunction and pelvic floor impairments
- Musculoskeletal treatments going up and or down the kinetic chain as the pelvis does not function in isolation
- Behavioral considerations
- Mindfulness training and exercises
- The inclusion of the patient's partner
Working with an interdisciplinary team provides the patient with support and proper treatment. Having strong referral sources is important to provide the holistic care needed by this patient population.
Sexual recovery takes time, patience, and hard work by both the patient, their partner, and their treatment team.[4]
Resources[edit | edit source]
Clinical References:
Gender Pronouns: A Provider’s Guide to Referring to Transgender Patients
Professional Associations and formal continuing education courses:
- American Physical Therapy Association: Academy of Pelvic Health
- American Physical Therapy Association: On-Demand: Male Pelvic Pain Course
- Herman & Wallace Pelvic Rehabilitation Institute
- Australian Physiotherapy Association: Men's Health
- Australian Physiotherapy Association: Male Pelvic Health
References[edit | edit source]
- ↑ World Health Organization. Gender and human rights. Available from: https://www.who.int/reproductivehealth/topics/gender_rights/sexual_health/en/ (accessed 14/03/2022).
- ↑ Lips HM. Sex and gender: An introduction. Waveland Press; 2020 Apr 10.
- ↑ Hatzichristou D, Kirana PS, Banner L, Althof SE, Lonnee-Hoffmann RA, Dennerstein L, Rosen RC. Diagnosing sexual dysfunction in men and women: sexual history taking and the role of symptom scales and questionnaires. The journal of sexual medicine. 2016 Aug 1;13(8):1166-82.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 4.25 4.26 Roscher, P, Men's Health. Male Sexual Dysfunction. Physioplus. March 2022.
- ↑ 5.0 5.1 5.2 Elliott S, Matthew A. Sexual recovery following prostate cancer: recommendations from 2 established Canadian sexual rehabilitation clinics. Sexual medicine reviews. 2018 Apr 1;6(2):279-94.
- ↑ Hackett G, Kirby M, Wylie K, Heald A, Ossei-Gerning N, Edwards D, Muneer A. British Society for Sexual Medicine guidelines on the management of erectile dysfunction in men—2017. The journal of sexual medicine. 2018 Apr 1;15(4):430-57.
- ↑ Briganti A, Salonia A, Zanni G, Fabbri F, Saccà A, Bertini R, Suardi N, Fantini GV, Rigatti P, Montorsi F. Erectile dysfunction and radical prostatectomy: an update. EAU update series. 2004 Jun 1;2(2):84-92.
- ↑ 8.0 8.1 Cohen D, Gonzalez J, Goldstein I. The role of pelvic floor muscles in male sexual dysfunction and pelvic pain. Sexual medicine reviews. 2016 Jan 1;4(1):53-62.
- ↑ Gild P, Dahlem R, Pompe RS, Soave A, Vetterlein MW, Ludwig TA, Maurer V, Marks P, Ahyai SA, Chun FK, Lenke L. Retrograde ejaculation after holmium laser enucleation of the prostate (HoLEP)—Impact on sexual function and evaluation of patient bother using validated questionnaires. Andrology. 2020 Nov;8(6):1779-86.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 Chen L, Shi GR, Huang DD, Li Y, Ma CC, Shi M, Su BX, Shi GJ. Male sexual dysfunction: a review of literature on its pathological mechanisms, potential risk factors, and herbal drug intervention. Biomedicine & Pharmacotherapy. 2019 Apr 1;112:108585.
- ↑ 11.0 11.1 Fennell R, Grant B. Discussing sexuality in health care: A systematic review. Journal of clinical nursing. 2019 Sep;28(17-18):3065-76.
- ↑ YouTube. Erectile Dysfunction and Your Pelvic Floor | Pelvic Health & Rehabilitation Center. Available from: https://www.youtube.com/watch?v=HvrCm8EJcF0 [last accessed 16/03/2022]
- ↑ YouTube. Men's Health Ultrasound - Male Pelvic Floor Contraction. Available from: https://www.youtube.com/watch?v=E4dx8f1V1Zs [last accessed 16/03/2022]