Pulmonary Oedema: Difference between revisions
No edit summary |
No edit summary |
||
| Line 58: | Line 58: | ||
* Inspiratory muscle training (IMT) | * Inspiratory muscle training (IMT) | ||
* Exercise (aerobic, strength, flexibility, posture, breathing) to return to prior level of function | * Exercise (aerobic, strength, flexibility, posture, breathing) to return to prior level of function | ||
* Monitor blood pressure. check medications taken as prescribed | |||
* Educate re - Eating a healthy diet. Check if on a reduced salt diet. Refer to dietician if needed. | |||
* Maintaining a healthy weight and exercising - implement a home exercise plan. | |||
== Resources == | == Resources == | ||
Revision as of 08:11, 23 September 2020
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (23/09/2020)
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Kim Jackson, Aminat Abolade and Kapil Narale
Introduction[edit | edit source]
Pulmonary oedema is a broad descriptive term and is usually defined as an abnormal accumulation of fluid in the extravascular compartments of the lung parenchyma. This process leads to diminished gas exchange at the alveolar level, progressing to potentially causing respiratory failure.
- Its etiology is either due to a cardiogenic process with the inability to remove sufficient blood away from the pulmonary circulation or non-cardiogenic precipitated by injury to the lung parenchyma.
- It is an important pathologic feature in many disease processes
- Determining the underlying disease process is crucial to guide its management.
- Clinical features include progressive worsening dyspnea, rales on lung auscultation, and worsening hypoxia[1]
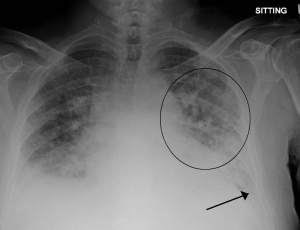
- Image R: circled area on Xray showing region of pulmonary oedema
Clinical Presentation[edit | edit source]
The clinical presentation of pulmonary oedema includes:
- Progressively worsening dyspnea, tachypnea, and rales (or crackles) on examination with associated hypoxia.
- Acute breathlessness
- Orthopnoea
- Paroxysmal nocturnal dyspnoea (PND)
- Cough, with pink foaming at the mouth (due to hypoxemia from alveolar flooding).
- Distress
Auscultation - mainstay of bedside assessment in all patients with respiratory symptoms. Specifically, hearing of either fine or coarse crackles is very crucial to management.
- Fine crackles are heard in cardiogenic pulmonary edema. They exclusively heard in the inspiratory phase when the small airways, which were shut during expiration, open abruptly[1][2]
Management[edit | edit source]
Therapeutic goals in patients with pulmonary edema include alleviation of symptoms and treatment of the underlying pathologic condition.
- Management consists of the improvement of gas exchange by methods that range from supplemental oxygen administration to mechanical ventilatory support with PEEP, depending on the severity of the disturbance in lung function.
- Diuretics remain the mainstay of treatment, and furosemide being the most commonly used medication. Higher doses are associated with more improvement in dyspnea, however, also associated with transient worsening of renal function.
2. Vasodilators can be added as an adjuvant therapy to the diuretics in the management of pulmonary edema.
- IV nitroglycerin (NTG) is the drug of choice, and it lowers preload and pulmonary congestion.
- NTG should only be used when the systolic blood pressure (SBP) is > 110 mm Hg.
- Nesiritide is a recombinant brain natriuretic peptide which has vasodilatory properties.
- Newer drugs like serelaxin, or Clevidipine may also be used
- Nifedipine has been utilized in the prophylaxis and treatment of high altitude pulmonary edema (HAPE). This calcium channel blocker counteracts the hypoxia-mediated vasoconstriction of the pulmonary vasculature.
3. Inotropes, such as dobutamine and dopamine, are used in the management of pulmonary congestion when associated with low SBP and signs of tissue hypoperfusion.
- Significant adverse events include tachyarrhythmias, ischemia, and hypotension.
- Ionotropes - Influence the force or speed of muscular contractility. Inotropic agents are used to improve the output of the heart in the treatment of eg heart failure[3].
4. Morphine reduces systemic vascular resistance and acts as an analgesic and anxiolytic. It has been used in the management of pulmonary edema secondary to acute coronary syndrome. However, it may cause respiratory depression needing intubation and generally not recommended.
5. Ventilatory support, both noninvasive and invasive, is used to improve oxygenation, direct alveolar, and interstitial fluids back into the capillaries, improve hypercarbia and hence reverse respiratory acidosis, and lastly, tissue oxygenation. It also aims at reducing the work of breathing.
- The decision to provide ventilatory support is based on clinical improvement with a trial of the above-mentioned drugs, patient's mental status, overall energy, or lack of such.
- In patients on invasive mechanical ventilation, continuous monitoring of hemodynamics is essential as a reduction in preload can lead to reduced cardiac output and thus a fall in SBP.
- Noninvasive mechanical ventilation, when initiated early in the management of pulmonary edema, has been associated with lower occurrences of respiratory muscle fatigue and, thus, reduction in invasive ventilation[1]
Physiotherapy[edit | edit source]
May Involve:
- Oxygen therapy and ventilation
- Rest
- Fluid intake - educating client to follow eg fluid restrictions
- Smoking cessation
- Pulmonary rehabilitation (PR) to improve exercise capacity
- Inspiratory muscle training (IMT)
- Exercise (aerobic, strength, flexibility, posture, breathing) to return to prior level of function
- Monitor blood pressure. check medications taken as prescribed
- Educate re - Eating a healthy diet. Check if on a reduced salt diet. Refer to dietician if needed.
- Maintaining a healthy weight and exercising - implement a home exercise plan.
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 King KC, Goldstein S. Congestive Heart Failure And Pulmonary Edema. InStatPearls [Internet] 2020 Jan 30. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK557611/ (last accessed 23.9.2020)
- ↑ Radiopedia Pulmonary oedema Available from:https://www.statpearls.com/kb/viewarticle/80517 (last accessed 23.8.2020)
- ↑ Collins Dictionary of Medicine © Robert M. Youngson 2004, 2005 Available from:https://medical-dictionary.thefreedictionary.com/inotropic (last accessed 23.9.20)