Cervical Radiculopathy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 45: | Line 45: | ||
Simply defined cervical radiculopathy is a dysfunction of a nerve root in the cervical spine, <span style="line-height: 1.5em;">a</span><span style="line-height: 1.5em;">s this is such a broad disorder with several mechanisms of pathology people of any age can be affected</span><ref name="Young IA">Young IA,Michener LA,Cleland JA,Aguilera AJ,Snyder AR.Manual therapy, exercise, and traction for patients with cervical radiculopathy: a randomize clinical trial.Physical Therapy 2009;89:632-642 (B)</ref><span style="line-height: 1.5em;">, with peak prominence between the ages of 40-50</span><ref name="Eubanks,JD" /><ref>Radhakrishnan K, Litchy WJ, O'Fallon M, et al. Epidemiology of cervical radiculopathy: A population-based study from Rochester, Minnesota, 1976 through 1990. Brain 1994; 117:325-335.</ref><ref name="Bogduk">Bogduk N. Twomey CT. Clinically Relevant Anatomy for the Lumbar Spine. 2ed. Edinburgh UK: Churchill Livingston. 1991</ref> with a reported prevelance of 83 people per 100,000 people<ref name="Bogduk" /><br> | Simply defined cervical radiculopathy is a dysfunction of a nerve root in the cervical spine, <span style="line-height: 1.5em;">a</span><span style="line-height: 1.5em;">s this is such a broad disorder with several mechanisms of pathology people of any age can be affected</span><ref name="Young IA">Young IA,Michener LA,Cleland JA,Aguilera AJ,Snyder AR.Manual therapy, exercise, and traction for patients with cervical radiculopathy: a randomize clinical trial.Physical Therapy 2009;89:632-642 (B)</ref><span style="line-height: 1.5em;">, with peak prominence between the ages of 40-50</span><ref name="Eubanks,JD" /><ref>Radhakrishnan K, Litchy WJ, O'Fallon M, et al. Epidemiology of cervical radiculopathy: A population-based study from Rochester, Minnesota, 1976 through 1990. Brain 1994; 117:325-335.</ref><ref name="Bogduk">Bogduk N. Twomey CT. Clinically Relevant Anatomy for the Lumbar Spine. 2ed. Edinburgh UK: Churchill Livingston. 1991</ref> with a reported prevelance of 83 people per 100,000 people<ref name="Bogduk" /><br> | ||
The systematic review by Barrett et al. (2015) reported about the most impactful population based study performed in Rochester Minnesota from 1976 – 1990. The study estimated the anual incidence to be 107,3 per 100.000 for men and 63,5 per 100.000 for women. <ref name="Barrett">Barrett I. et al. Cervical Radiculopathy Epidemiology, Etiology, Diagnosis, and Treatment. Journal of Spinal Disorders &amp;amp;amp;amp;Techniques. April 2015; 28:5. LoE: 2A</ref> These figures corresponds to the study of Radhakrishnan et al. <ref name="Rad">Radhaknshnank et al. Epidemiology of Cervical Radiculopathy. A Population Based Study. Brain. 1994: 117; 325-335 LoE: 2C</ref> | The systematic review by Barrett et al. (2015) reported about the most impactful population based study performed in Rochester Minnesota from 1976 – 1990. The study estimated the anual incidence to be 107,3 per 100.000 for men and 63,5 per 100.000 for women. <ref name="Barrett">Barrett I. et al. Cervical Radiculopathy Epidemiology, Etiology, Diagnosis, and Treatment. Journal of Spinal Disorders &amp;amp;amp;amp;amp;Techniques. April 2015; 28:5. LoE: 2A</ref> These figures corresponds to the study of Radhakrishnan et al. <ref name="Rad">Radhaknshnank et al. Epidemiology of Cervical Radiculopathy. A Population Based Study. Brain. 1994: 117; 325-335 LoE: 2C</ref> | ||
The two main mechanisms of the nerve root irritation or impingement are: | The two main mechanisms of the nerve root irritation or impingement are: | ||
| Line 54: | Line 54: | ||
This rule is not correct 100% of the time but it is a good basis to go on for a logical reason: As you age, disc height decreases and there is less material within the intervertebral disc itself making a prolapse less likely and making it harder for a prolapse to impinge a nerve root. | This rule is not correct 100% of the time but it is a good basis to go on for a logical reason: As you age, disc height decreases and there is less material within the intervertebral disc itself making a prolapse less likely and making it harder for a prolapse to impinge a nerve root. | ||
<blockquote>Just think: '''There is more material to prolapse from a disc of a younger person!''' </blockquote> | <blockquote>Just think: '''There is more material to prolapse from a disc of a younger person!''' </blockquote> | ||
Cervical radiculopathy (Barrett et al. 2015) is a neurological disorder from nerve root dysfunction often due to mechanical compression (because of disc hernation, stenosis, spondylosis, …). Spondylosis can affect the neuroforamen from all directions, wich limits nerve root excursion. Also cytokines released from damaged intervertebral discs can cause this disorder. <ref name="Barrett">Barrett I. et al. Cervical Radiculopathy Epidemiology, Etiology, Diagnosis, and Treatment. Journal of Spinal Disorders &amp;amp;amp;amp;Techniques. April 2015; 28:5. LoE: 2A</ref> <br> | Cervical radiculopathy (Barrett et al. 2015) is a neurological disorder from nerve root dysfunction often due to mechanical compression (because of disc hernation, stenosis, spondylosis, …). Spondylosis can affect the neuroforamen from all directions, wich limits nerve root excursion. Also cytokines released from damaged intervertebral discs can cause this disorder. <ref name="Barrett">Barrett I. et al. Cervical Radiculopathy Epidemiology, Etiology, Diagnosis, and Treatment. Journal of Spinal Disorders &amp;amp;amp;amp;amp;Techniques. April 2015; 28:5. LoE: 2A</ref> <br> | ||
These inflammatory cytokines like interleukin-6, interleukin-8, nitric oxide, tumor necrosis factor alfa and prostaglandin E2 are involved in the development of pain associated with cervical radiculopathy and provide the rational for treatment with anti-inflammatory medications. <ref name="Barrett">Barrett I. et al. Cervical Radiculopathy Epidemiology, Etiology, Diagnosis, and Treatment. Journal of Spinal Disorders &amp;amp;amp;amp;Techniques. April 2015; 28:5. LoE: 2A</ref> | These inflammatory cytokines like interleukin-6, interleukin-8, nitric oxide, tumor necrosis factor alfa and prostaglandin E2 are involved in the development of pain associated with cervical radiculopathy and provide the rational for treatment with anti-inflammatory medications. <ref name="Barrett">Barrett I. et al. Cervical Radiculopathy Epidemiology, Etiology, Diagnosis, and Treatment. Journal of Spinal Disorders &amp;amp;amp;amp;amp;Techniques. April 2015; 28:5. LoE: 2A</ref> | ||
There is increasing evidence that inflammation (Kuijper et al. 2009) in itself and/or in association with root compression is the main cause of symptoms and signs. This is proved by the presence of interleukins and prostaglandin in herniated discs and the spontaneous recovery within weeks or months in the majority of patients. <ref name="Kuijper">Kuijper B. et al. Degenerative cervical radiculopathy: diagnosis and conservative treatment: A review. European journal of neurology. 2009; 16(1): 15-20fckLRLoE: 2A</ref> | There is increasing evidence that inflammation (Kuijper et al. 2009) in itself and/or in association with root compression is the main cause of symptoms and signs. This is proved by the presence of interleukins and prostaglandin in herniated discs and the spontaneous recovery within weeks or months in the majority of patients. <ref name="Kuijper">Kuijper B. et al. Degenerative cervical radiculopathy: diagnosis and conservative treatment: A review. European journal of neurology. 2009; 16(1): 15-20fckLRLoE: 2A</ref> | ||
| Line 89: | Line 89: | ||
Symptoms are generally amplified with side flexion towards the side of pain and when an extension or rotation of the neck takes place because these movements reduce the space available for the nerve root to exit the foramen causing impingement<ref name="Eubanks,JD" />. This often causes the patient to present with a stiff neck and a decrease in cervical spine range of motion (ROM) as movement may activate their symptoms. This in turn results in secondary musculoskeletal problems which can manifest as a decrease in muscle length of the cervical spine musculature (upper fibres of trapezius, scaleni, levator scapulae), weakness, joint stiffness, capsule tightness and postural defects which can go on to affect movement mechanisms of the rest of the body.<br> | Symptoms are generally amplified with side flexion towards the side of pain and when an extension or rotation of the neck takes place because these movements reduce the space available for the nerve root to exit the foramen causing impingement<ref name="Eubanks,JD" />. This often causes the patient to present with a stiff neck and a decrease in cervical spine range of motion (ROM) as movement may activate their symptoms. This in turn results in secondary musculoskeletal problems which can manifest as a decrease in muscle length of the cervical spine musculature (upper fibres of trapezius, scaleni, levator scapulae), weakness, joint stiffness, capsule tightness and postural defects which can go on to affect movement mechanisms of the rest of the body.<br> | ||
It is possible that when you are assessing a patient it may not be easy to 'bring on' the radiating arm pain, if this is the case try not to rule out radiculopathy, just try and get more information about the movements, positions or functional tasks which bring on the pain and replicate them. Reproducing the S+S (Signs and Symptoms) is a very useful tool in aiding diagnosis. Equally do not be alarmed if you cannot replicate the S+S in the assessment, give the patient exercises to do at home along with postural advice and continue to perform the activities which usually bring on the radiating arm symptoms and see if there is a change.<br> | It is possible that when you are assessing a patient it may not be easy to 'bring on' the radiating arm pain, if this is the case try not to rule out radiculopathy, just try and get more information about the movements, positions or functional tasks which bring on the pain and replicate them. Reproducing the S+S (Signs and Symptoms) is a very useful tool in aiding diagnosis. Equally do not be alarmed if you cannot replicate the S+S in the assessment, give the patient exercises to do at home along with postural advice and continue to perform the activities which usually bring on the radiating arm symptoms and see if there is a change.<br> | ||
== Differential Diagnosis == | |||
Due to the close proximity of the cervical spine vertebrae and nerve roots to the vertebral arteries it is crucial that during the initial assessment of a patient any conditions which can cause severe damage to the patients blood supply, especially during any manual therapy. It is also important to be aware of other pathologies which mimic the S+S of radiculopathy.<ref name="Erhard">C: R. Erhard et al. Cervical Radiculopathy or Parsonage-Turner Syndrome: Differential Diagnosis of a Patient With Neck and Upper Extremity Symptoms. JOSPT. OCTOBER 2005fckLRVolume 35, No. 10 LoE: 3B</ref> | |||
*Spinal Tumor | |||
*Systemic diseases known to cause peripheral neuropathies | |||
*Cervical myelopathy | |||
*Ligamentous Instability | |||
*Vertebral Artery Insufficiency (VBI) | |||
*Herniated nucleous pulposos (HNP) | |||
*Shoulder Pathology | |||
*Peripheral nerve disorders | |||
*Thoracic outlet syndrome | |||
*Brachial plexus pathology | |||
*Systemic disease | |||
*Parsonage-Turner syndrome | |||
*[[Pancoast_Tumor|Superior pulmonary sulcus tumor]]: | |||
When we combine the aspects of patiënts history, physical examination and radiological findings we should be able to differentiate this from cervical radiculopathy. A negative Spurling’s test, normale range of motion of the neck and the lack of pulmonary air at the top of the lung in anteroposterior cervical radiographs could indicate a Superior pulmonary sulcus tumor. In this case such a diagnose can be confirmed with CT or MRI imaging. <ref name="Gu">Gu R., et al. Differential diagnosis of cervical radiculopathy and superior pulmonary sulcus tumor. Chinese medical journal. 2012 August; 125(15): 2755-2757 | |||
LoE: 3B</ref> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 95: | Line 119: | ||
In a non-Physiotherapy sense, the most common diagnostic methods used to assess the presence of possible compression are imaging studies (radiograph and MRI) and electrophysiologic studies ([http://emedicine.medscape.com/article/1846028-overview EMG] + [http://jnnp.bmj.com/content/76/suppl_2/ii23.full Nerve Conduction Studies]) to examine the nerve root and nerve conduction velocity<ref>Partanen J, Partanen K, Oikarinen H, et al. Preoperative electroneuromyography and myelography in cervical root compression. Electromyogr Clin Neurophysiol. 1991; 31:21-26.</ref><ref name="Eubanks,JD" /><ref name="Young IA" />. If either of these options have been performed on your patient then it is possible to assess and see if radiculopathy is present through commonly used Physiotherapy assessment and treatment starting with the [http://www.physio-pedia.com/Subjective_Assessment Subjective Assessment].<br> | In a non-Physiotherapy sense, the most common diagnostic methods used to assess the presence of possible compression are imaging studies (radiograph and MRI) and electrophysiologic studies ([http://emedicine.medscape.com/article/1846028-overview EMG] + [http://jnnp.bmj.com/content/76/suppl_2/ii23.full Nerve Conduction Studies]) to examine the nerve root and nerve conduction velocity<ref>Partanen J, Partanen K, Oikarinen H, et al. Preoperative electroneuromyography and myelography in cervical root compression. Electromyogr Clin Neurophysiol. 1991; 31:21-26.</ref><ref name="Eubanks,JD" /><ref name="Young IA" />. If either of these options have been performed on your patient then it is possible to assess and see if radiculopathy is present through commonly used Physiotherapy assessment and treatment starting with the [http://www.physio-pedia.com/Subjective_Assessment Subjective Assessment].<br> | ||
= | Cervical radiculopathy could be confirmed when root compression is seen on MRI, which is the method of choice to detect disc protrusions. To detect foraminal stenosis which gives bony compression on the nerve, thin slices spiral CT is described as the best way to detect this.<ref name="Kuijper">Kuijper B. et al. Degenerative cervical radiculopathy: diagnosis and conservative treatment: A review. European journal of neurology. 2009; 16(1): 15-20 | ||
LoE: 2A</ref> | |||
There still is no consensus on wether conventional needle [[Biofeedback|myography (EMG]]) has a strong diagnostic value for cervical radiculopathy. Several unblinded studies reported sensitivities ranging from 30-95%.<ref name="Kuijper">Kuijper B. et al. Degenerative cervical radiculopathy: diagnosis and conservative treatment: A review. European journal of neurology. 2009; 16(1): 15-20 | |||
LoE: 2A</ref> | |||
== | Dillingham TR et al (2001) performed a study to determine the optimal electromyography screening examination of the upper limb that ensures the detection of a cervical radiculopathy. They found that six muscle screens including paraspinal muscles yielded consistently high identification rates. The results of this study indicates that if six muscles, representing all cervical root levels, are studied, then the examiner can be confident of detecting a cervical radiculopathy.<ref name="Kuijper">Kuijper B. et al. Degenerative cervical radiculopathy: diagnosis and conservative treatment: A review. European journal of neurology. 2009; 16(1): 15-20 | ||
LoE: 2A</ref><ref name="Dillingham">Dillingham TR et al. Identification of cervical radiculopathies.American journal of physical medicine and rehabilitation. Feb 2001. 80(2): 84-91. LoE: 2B</ref> | |||
Kuijper B. et al (2009) nuanced this by pointing out that most C6 muscles are also innervated by C5 or C7. So according to their information, a Cervical radiculopathy at the C6 level alone will be difficult to find by the use of EMG. The use of paraspinal muscle examination seems to be more sensitive to them, but this technique is harder to perform without giving false-positive results, especially in older patiënts.<ref name="Kuijper">Kuijper B. et al. Degenerative cervical radiculopathy: diagnosis and conservative treatment: A review. European journal of neurology. 2009; 16(1): 15-20 | |||
LoE: 2A</ref><br> | |||
'''Subjective Assessment''' | |||
The HPC and Mechanism of Injury ([http://www.physio-pedia.com/Section_3:_Patient_history Patient History]) sections of a subjective assessment can be integral to diagnosis and the cause of the radiating arm pain. More frequently acute radiating arm pain is caused by a disk herniation, while chronic bilateral axial neck and radiating arm pain is usually caused by cervical spondylosis<ref name="Eubanks,JD" />.<br> | |||
== Outcome Measures == | == Outcome Measures == | ||
| Line 125: | Line 140: | ||
[[Fear‐Avoidance Belief Questionnaire|FABQ]] [[Neck Disability Index|NDI]] [[Neck Pain and Disability Scale|Neck Pain and Disability Scale]] | [[Fear‐Avoidance Belief Questionnaire|FABQ]] [[Neck Disability Index|NDI]] [[Neck Pain and Disability Scale|Neck Pain and Disability Scale]] | ||
== Examination == | |||
In 2003, Dr. Robert Wainner and colleagues examined the accuracy of the clinical examination and developed a clinical prediction rule to aid in the diagnosis of cervical radiculopathy. Their research demonstrated that these 4 clinical tests, when combined, hold high diagnostic accuracy compared to EMG studies: Positive tests for [http://www.physio-pedia.com/Spurlings_Test Spurlings Test], [http://www.physio-pedia.com/Neurodynamic_Assessment#Upper_limb_tension_test_1_.28median_nerve_bias.29 Upper limb tension-1] [[Cervical distraction test|Distraction test]] and [http://www.physio-pedia.com/Cervical_Flexion-Rotation_Test Cervical Flexion Rotation Test]. When all 4 of these clinical features are present, the post-test probablity of cervical radiculopathy is '''<u>90%</u>''', if only three of the four <span style="line-height: 1.5em;">test are positive the probability decrease to </span>'''<u>65%</u>'''<ref>Wainner RS, Fritz JM, Irrgang JJ, et al. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28(1):52-62.</ref><span style="line-height: 1.5em;"> </span><ref name="Kenneth" /><ref name="Young IA" /><ref>C: Wainner et al. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine 2003 Jan 1. 28(1):52-62.</ref>. Another combination of tests, with good reliability are the combination of the [http://www.physio-pedia.com/Spurlings_Test Spurlings Test], Neck Distraction, Valsalva and [http://www.physio-pedia.com/Neurodynamic_Assessment#Upper_limb_tension_test_1_.28median_nerve_bias.29 Upper Limb Tension Tests 1], [http://www.physio-pedia.com/Neurodynamic_Assessment#Upper_limb_tension_test_2a_.28median_nerve_bias.29 2a] <span style="line-height: 1.5em;">and [http://www.physio-pedia.com/Neurodynamic_Assessment#Upper_limb_tension_test_2b_.28radial_nerve_bias.29 2b]</span><ref>A1: Sidney M. Rubinstein et al. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. European Spine Journal. Volume 16, Number 3, 307-319</ref><span style="line-height: 1.5em;">.</span> | |||
== Management and Treatment Approaches == | == Management and Treatment Approaches == | ||
| Line 176: | Line 195: | ||
==== Exercise Therapy ==== | ==== Exercise Therapy ==== | ||
Exercises targeted at opening the intervertebral foramen are the best choice for reducing the impact of radiculopathy. Exercises such as contralateral rotation and sideflexion are amongst the simplest forms of exercises which are effective against signs and symptons, given in the form of active ROM<ref name="Langevin">Langevin P. Rou JS. Desmeules F. Cervical radiculopathy: Study protocol of a randomised clinical trial evaluating the effect of mobilisations and exercises targeting the opening of intervertebral foramen. BMC Msk Disorders.13:10 2012.</ref>. Due to the intricate and close relationship of muscles on the intervertebral foramen and the likely presentation of reduced ROM, stretching is also an effective form of treatment to regain ROM<ref name="Mal">Malanga G. Sherwin SW.Cervical Radiculopathy Treatment &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Management 2013 [ONLINE]fckLRAvailable from http://emedicine.medscape.com/article/94118-treatment#aw2aab6b6b2</ref>.<br> | Exercises targeted at opening the intervertebral foramen are the best choice for reducing the impact of radiculopathy. Exercises such as contralateral rotation and sideflexion are amongst the simplest forms of exercises which are effective against signs and symptons, given in the form of active ROM<ref name="Langevin">Langevin P. Rou JS. Desmeules F. Cervical radiculopathy: Study protocol of a randomised clinical trial evaluating the effect of mobilisations and exercises targeting the opening of intervertebral foramen. BMC Msk Disorders.13:10 2012.</ref>. Due to the intricate and close relationship of muscles on the intervertebral foramen and the likely presentation of reduced ROM, stretching is also an effective form of treatment to regain ROM<ref name="Mal">Malanga G. Sherwin SW.Cervical Radiculopathy Treatment &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Management 2013 [ONLINE]fckLRAvailable from http://emedicine.medscape.com/article/94118-treatment#aw2aab6b6b2</ref>.<br> | ||
Once ROM increases strengthening can also be utilised to create new stability and reduce the risk of developing nerve root irritation in the future, as long as it is not caused by a structure which cannot be influenece by physiotherapy. During the initial stages of treatment, strengthening should be limited to isometric exercises in the involved upper limb. Once the radicular symptoms have been resolved, progressive isotonic strengthening can begin. This should initially stress low weight and high repetitions (15-20 repetitions). Closed kinetic chain activities can be very helpful in rehabilitating weak shoulder girdle muscles. However, a multicenter randomized controlled trial found no significant difference with the addition of specific neck stabilization exercises to a program of general neck advice and exercise<ref name="Mal" /><ref name="Griff">Griffiths C, Dziedzic K, Waterfield J, Sim J. Effectiveness of specific neck stabilization exercises or a general neck exercise program for chronic neck disorders: a randomized controlled trial. J Rheumatol. Feb 2009;36(2):390-7</ref><br> | Once ROM increases strengthening can also be utilised to create new stability and reduce the risk of developing nerve root irritation in the future, as long as it is not caused by a structure which cannot be influenece by physiotherapy. During the initial stages of treatment, strengthening should be limited to isometric exercises in the involved upper limb. Once the radicular symptoms have been resolved, progressive isotonic strengthening can begin. This should initially stress low weight and high repetitions (15-20 repetitions). Closed kinetic chain activities can be very helpful in rehabilitating weak shoulder girdle muscles. However, a multicenter randomized controlled trial found no significant difference with the addition of specific neck stabilization exercises to a program of general neck advice and exercise<ref name="Mal" /><ref name="Griff">Griffiths C, Dziedzic K, Waterfield J, Sim J. Effectiveness of specific neck stabilization exercises or a general neck exercise program for chronic neck disorders: a randomized controlled trial. J Rheumatol. Feb 2009;36(2):390-7</ref><br> | ||
Revision as of 11:35, 26 April 2016
Original Editor - Stéphanie Dartevelle
Top Contributors - Scott Buxton, Admin, Jasper Vermeersch, Stéphanie Dartevelle, Rachael Lowe, Garima Gedamkar, Kim Jackson, Scott Cornish, Simisola Ajeyalemi, Thomas Rodeghero, Jesse Demeester, Laura Ritchie, 127.0.0.1, WikiSysop, Evan Thomas, Olajumoke Ogunleye, Jelle Van Hemelryck, Stijn De Coninck, Venugopal Pawar, Fasuba Ayobami, Maxime Tuerlinckx, Candace Goh, Rucha Gadgil, Wendy Walker, Lucinda hampton, Jess Bell, Johnathan Fahrner and Khloud Shreif
Search Strategy[edit | edit source]
Databases: Pubmed, Web of Science, Pedro
As subject headings varied between the databases, various combinations of the key words were used:
Cervical radiculopathy, Root compression, Epidemiology of Cervical radiculopathy, prognose for cervical radiculopathy, Cervical radiculopathy anatomy, physcial/medical management cervical radiculopathy, outcome measures for cervical radiculopathy
Definition/Description[edit | edit source]
"Cervical radiculopathy is a disease process marked by nerve compression from herniated disk material or arthritic bone spurs. This impingement typically produces neck and radiating arm pain or numbness, sensory deficits, or motor dysfunction in the neck and upper extremities."[1]
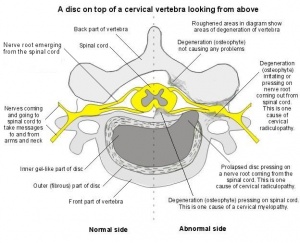
Cervical radiculopathy occurs with pathologies that causes symptoms on the nerve roots. [2] Those can be compression, irritation, traction, and a lesion on the nerve root caused by either a herniated disc, foraminal narrowing or degenerative spondylitic change (Osteoarthritic changed or degeneration) leading to stenosis of the intervertebral foramen[2] [3].
Most of the time cervical radiculopathy appears unilaterally, however it is possible for bilateral symptoms to be present if severe bony spurs are present at one level, impinging/irritating the nerve root on both sides. If peripheral radiation of pain, weakness or pins and needle are present, the location of the pain will follow back to the concerned afected nerve root [2].
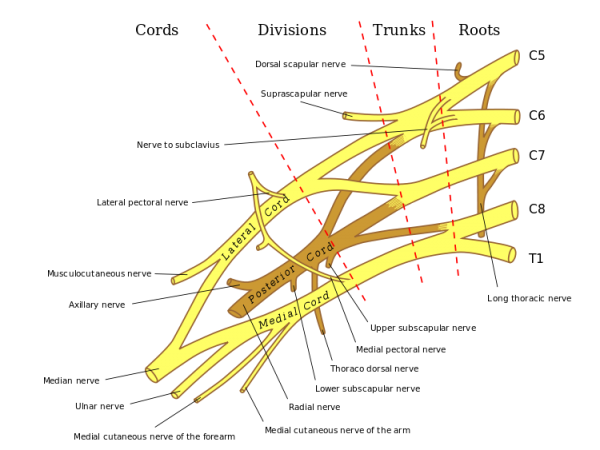
Clinically Relevant Anatomy[edit | edit source]
Cervical radiculopathy is defined as a disorder affecting a spinal nerve root in the Cervical Spine, therefore a knowledge of the brachial plexus is crucial to understanding the impact of nerve root impingement or damge has on the body.
| [4][5] |
Having an understanding of anatomy is key to effective physiotherapy practice, putting this anatomy into a functional sense is even more crucial for treatment considerations and movement analysis. In the cervical spine 50% of cervical rotation occurs at the C1-2 joints (AtlantoAxial Joint) and 50% of flexion and extension occurs at the Occipitoatlanto joint. Another important consideration is that the cervical facet joints are at a 45° meaning that below C2 sideflexion is coupled with rotation to the same side[6].
We have 8 cervical nerve roots, for 7 cervical vertebrae and this may seem confusing at first. However a nerve root comes out of the spinal column between C7 and T1, hence the name C8 as T1 already exists [2].
Nerve roots and the local vessels lack a perineurium and have a poorly developed epineurium, making them vulnerable to mechanical injury when compared to the periphery. The blood supply is also less secured and vulnerable to ischemic damage[7]. These anatomical difference to peripheral nerves may explain why low pressures on the nerve root elicit large changes and S+S. The nerve roots are vulnerable to pressure damage which is why small impingements can cause S+S (Signs + Symptoms). At 5-10mmHg (0.1psi) capilliary stasis and ischemia has been observed with partial blockage of axonal transport. At 50mmhg tissue permeability increases with an influx of oedema, higher to 75mmhg, there is nerve conduction failure if sustained for 2 hours. At 70+mmhg neural ischemia is complete and conduction is not possible[7]. It is rare to get pressures that high but 5-10mmhg is a large small amount of pressure and S+S occur[7]. These pressures can occur with a less severe clinical picture in unique circumstances, if the pressure is acute then the symptoms are severe however if chronic the nervous tissue is given time to adapt and evolve to the surrounding structure and have less severe symptoms.
Tanaka N. et al (2000) used a surgical microscope to do a anatomic study of the of the cervical intervertebral foramina, nerve roots and intradural rootlets. Their goal was to investigate the anatomy of cervical root compression. Therefor they used 18 cadavers. All soft tissue was removed and so intervertebral discs and foramina, were exposed.
The intervertrebral foramina were shaped like a funnel with the entrance zone being the most narrow part. Therefore this is the place where the compression of the nerve roots in the intervertebral foramina occures. Compression of the roots at the anterior side was ascribed to protruding discs and osteophytes of the uncovertebral region. Compression on the posterior side was caused by the superior articular process, the ligamentum flavum and the periradicular fibrous tissues. [8]
Epidemiology / Etiology
[edit | edit source]
Simply defined cervical radiculopathy is a dysfunction of a nerve root in the cervical spine, as this is such a broad disorder with several mechanisms of pathology people of any age can be affected[9], with peak prominence between the ages of 40-50[2][10][11] with a reported prevelance of 83 people per 100,000 people[11]
The systematic review by Barrett et al. (2015) reported about the most impactful population based study performed in Rochester Minnesota from 1976 – 1990. The study estimated the anual incidence to be 107,3 per 100.000 for men and 63,5 per 100.000 for women. [12] These figures corresponds to the study of Radhakrishnan et al. [6]
The two main mechanisms of the nerve root irritation or impingement are:
- Spondylosis leading to stenosis or bony spurs - More common in older patients
- Disc Herniation - More common in younger patients
This rule is not correct 100% of the time but it is a good basis to go on for a logical reason: As you age, disc height decreases and there is less material within the intervertebral disc itself making a prolapse less likely and making it harder for a prolapse to impinge a nerve root.
Just think: There is more material to prolapse from a disc of a younger person!
Cervical radiculopathy (Barrett et al. 2015) is a neurological disorder from nerve root dysfunction often due to mechanical compression (because of disc hernation, stenosis, spondylosis, …). Spondylosis can affect the neuroforamen from all directions, wich limits nerve root excursion. Also cytokines released from damaged intervertebral discs can cause this disorder. [12]
These inflammatory cytokines like interleukin-6, interleukin-8, nitric oxide, tumor necrosis factor alfa and prostaglandin E2 are involved in the development of pain associated with cervical radiculopathy and provide the rational for treatment with anti-inflammatory medications. [12]
There is increasing evidence that inflammation (Kuijper et al. 2009) in itself and/or in association with root compression is the main cause of symptoms and signs. This is proved by the presence of interleukins and prostaglandin in herniated discs and the spontaneous recovery within weeks or months in the majority of patients. [13]
The most common level of root compression is C7 (reported percentages 46.3–69%), followed by C6 (19–17.6%); compression of roots C5 (2–6.6%) and C8 (10– 6.2%) are less frequent. One possible explanation is that intervertebral foramina are largest in the upper cervical region and progressively decrease in size in the middle and lower cervical areas, with an exception of the C7-Th1 foramen (C8). [13][5]
Characteristics/Clinical Presentation[edit | edit source]
To understand the clinical presentation of cervical radiculopathy you must have a functional understanding of the clinically relevant anatomy section.
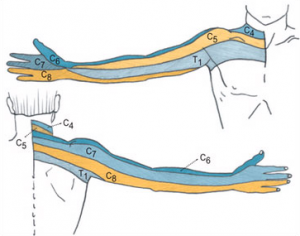
Typical symptoms of cervical radiculopathy are: irradiating arm pain corresponding a dermatomal pattern, neck pain, parasthesia, muscle weakness in a myotomal pattern, reflex impairment/loss, headaches, scapular pain, sensory and motor dysfunction in upper extremities and neck[2][9][3][14][15].
At the most basic level these are the upper limb movements that are affected in the myotomal pattern.
- C1/C2- Neck flexion/extension
- C3- Neck lateral flexion
- C4- Shoulder elevation
- C5- Shoulder abduction
- C6- Elbow flexion/wrist extension
- C7- Elbow extension/wrist flexion
- C8- Thumb extension
- T1- Finger abduction
For more detailed information on the exact muscles or dermatomes that will clinically present themselves go here:
Nerve roots and the muscles affected
Dermatomal Pattern
If a nerve root is compressed it can cause a combination of factors: inflammatory mediators, changes in vascular response and intraneural oedema which causes radicular pain. Absence of radiating pain does not exclude nerve root compression. The same appears with sensory and motor dysfunction that might be present without significant pain[2].
Symptoms are generally amplified with side flexion towards the side of pain and when an extension or rotation of the neck takes place because these movements reduce the space available for the nerve root to exit the foramen causing impingement[2]. This often causes the patient to present with a stiff neck and a decrease in cervical spine range of motion (ROM) as movement may activate their symptoms. This in turn results in secondary musculoskeletal problems which can manifest as a decrease in muscle length of the cervical spine musculature (upper fibres of trapezius, scaleni, levator scapulae), weakness, joint stiffness, capsule tightness and postural defects which can go on to affect movement mechanisms of the rest of the body.
It is possible that when you are assessing a patient it may not be easy to 'bring on' the radiating arm pain, if this is the case try not to rule out radiculopathy, just try and get more information about the movements, positions or functional tasks which bring on the pain and replicate them. Reproducing the S+S (Signs and Symptoms) is a very useful tool in aiding diagnosis. Equally do not be alarmed if you cannot replicate the S+S in the assessment, give the patient exercises to do at home along with postural advice and continue to perform the activities which usually bring on the radiating arm symptoms and see if there is a change.
Differential Diagnosis[edit | edit source]
Due to the close proximity of the cervical spine vertebrae and nerve roots to the vertebral arteries it is crucial that during the initial assessment of a patient any conditions which can cause severe damage to the patients blood supply, especially during any manual therapy. It is also important to be aware of other pathologies which mimic the S+S of radiculopathy.[16]
- Spinal Tumor
- Systemic diseases known to cause peripheral neuropathies
- Cervical myelopathy
- Ligamentous Instability
- Vertebral Artery Insufficiency (VBI)
- Herniated nucleous pulposos (HNP)
- Shoulder Pathology
- Peripheral nerve disorders
- Thoracic outlet syndrome
- Brachial plexus pathology
- Systemic disease
- Parsonage-Turner syndrome
When we combine the aspects of patiënts history, physical examination and radiological findings we should be able to differentiate this from cervical radiculopathy. A negative Spurling’s test, normale range of motion of the neck and the lack of pulmonary air at the top of the lung in anteroposterior cervical radiographs could indicate a Superior pulmonary sulcus tumor. In this case such a diagnose can be confirmed with CT or MRI imaging. [17]
Diagnostic Procedures[edit | edit source]
In a non-Physiotherapy sense, the most common diagnostic methods used to assess the presence of possible compression are imaging studies (radiograph and MRI) and electrophysiologic studies (EMG + Nerve Conduction Studies) to examine the nerve root and nerve conduction velocity[18][2][9]. If either of these options have been performed on your patient then it is possible to assess and see if radiculopathy is present through commonly used Physiotherapy assessment and treatment starting with the Subjective Assessment.
Cervical radiculopathy could be confirmed when root compression is seen on MRI, which is the method of choice to detect disc protrusions. To detect foraminal stenosis which gives bony compression on the nerve, thin slices spiral CT is described as the best way to detect this.[13]
There still is no consensus on wether conventional needle myography (EMG) has a strong diagnostic value for cervical radiculopathy. Several unblinded studies reported sensitivities ranging from 30-95%.[13]
Dillingham TR et al (2001) performed a study to determine the optimal electromyography screening examination of the upper limb that ensures the detection of a cervical radiculopathy. They found that six muscle screens including paraspinal muscles yielded consistently high identification rates. The results of this study indicates that if six muscles, representing all cervical root levels, are studied, then the examiner can be confident of detecting a cervical radiculopathy.[13][19]
Kuijper B. et al (2009) nuanced this by pointing out that most C6 muscles are also innervated by C5 or C7. So according to their information, a Cervical radiculopathy at the C6 level alone will be difficult to find by the use of EMG. The use of paraspinal muscle examination seems to be more sensitive to them, but this technique is harder to perform without giving false-positive results, especially in older patiënts.[13]
Subjective Assessment
The HPC and Mechanism of Injury (Patient History) sections of a subjective assessment can be integral to diagnosis and the cause of the radiating arm pain. More frequently acute radiating arm pain is caused by a disk herniation, while chronic bilateral axial neck and radiating arm pain is usually caused by cervical spondylosis[2].
Outcome Measures[edit | edit source]
Outcome measures are an essential tool to assess whether or not you are having a positive. negative or static effect on a patients' condition. Cervical Radiculopathy is no different. There are a lot of outcome measures in existance and it is important to know if the tool you are using is measuring what you want to measure (Specificity) and how good it is correctly identifying a pattern (Sensitivity)[20].
FABQ NDI Neck Pain and Disability Scale
Examination[edit | edit source]
In 2003, Dr. Robert Wainner and colleagues examined the accuracy of the clinical examination and developed a clinical prediction rule to aid in the diagnosis of cervical radiculopathy. Their research demonstrated that these 4 clinical tests, when combined, hold high diagnostic accuracy compared to EMG studies: Positive tests for Spurlings Test, Upper limb tension-1 Distraction test and Cervical Flexion Rotation Test. When all 4 of these clinical features are present, the post-test probablity of cervical radiculopathy is 90%, if only three of the four test are positive the probability decrease to 65%[21] [3][9][22]. Another combination of tests, with good reliability are the combination of the Spurlings Test, Neck Distraction, Valsalva and Upper Limb Tension Tests 1, 2a and 2b[23].
Management and Treatment Approaches[edit | edit source]
Medical Management
[edit | edit source]
There are several intervention strategies for managing cervical radiculopathy with physical therapy and surgical interventions being the most common. Long-term benefits of surgical interventions are questionable with reported numbers of 25% of people continuing to experience pain and disability at 12 month follow-ups[24]. There is a significant amount of evidence available to support the use of physical therapy interventions for patients with cervical radiculopathy, and the benefit of physical therapy and manual techniques in general for patients with neck pain with or without radicular symptoms (see key evidence for a list of references).
The nonoperative treatment includes a period (+/- one week, not more) of immobilisation with a cervical collar to decrease the compression on the nerve root; cervical traction; medication to reduce the pain; physical therapy and manipulation including massage, stretching, exercices to improve range of motion and eventually ice, heat and electrical stimulation. They must be used together and not separately to show improvement. But all these elements of the treatment need further studies to prove more effectiveness. [2]
Physiotherapy Management
[edit | edit source]
Although a definitive treatment progression for treating cervical radiculopathy has not been developed, a general consensus exists within the literature that using manual therapy techniques in conjunction with therapeutic exercise is effective in regard to increasing function, as well as active range of movement (AROM), focusing on decreasing levels of pain and disability will most likely be the main focus of the patient[25].
If the patient has had long-term pain, an element of pain sensitisation may have developed and chronic pain behaves differently to acute pain. Therefore education about pain and reconceptualisation may be necessary.
Treatment Options:
- Education and Advice
- Manual Therapy - PAIVMS/PIVMS/NAGS/SNAGS
- Exercise Therapy - AROM, Stretches and Strengthening
- Postural Re-Education
Education and advice[edit | edit source]
Education is key to getting the patient on your side and to work co-operatively with Physiotherapy. If a patient understands why they are having the neck pain which is causing them to have arm pain then they will more likely want to take part in rehabilitation. If they do not understand what the point in this 'exercise' or this 'pressing' then they will likely think it to be a waste of time. This is a generalisation of course but it is often accurate.
An important piece of advice to rehabilitation from a prolapsed disc, is that smoking can increase the pressure on the disc causing further damage and impingement, therefore this should not be overlooked[7]. Additionally it is always good to bring up the topic of smoking cessation with patients for their all round health, tying in with Holistic Management.
Manual Therapy[edit | edit source]
In a recent systematic review by Boyles et al in 2011[26], manual therapy was shown to be effective at reducing pain levels, improving function and increasing joint ROM. When combined with exercise therapy it was more effective than the control group of manual therapy or exercise therapy however both control groups were effective at reducing signs and symptoms[27].
The manual therapy techniques proven to be effective by the systematic review were:
- Thrust mobilisations of the cervical or thoracic spine
- Cervical mobilisations - A-P/P-A/Lateral Glides/Rotations/Retractions
The parameters were recorded in a study by Ragonese et al[27]; performing one set of 30 seconds or 15-20 repetitions at each desired level of the cervical spine at grade 3 or 4[28](Maitland Mobilisations). Others stated that it was down to the practitioners discgression.
- Muscle Energy Techniques
Cleland et al[29] utilised muscle energy techniques in 28 patients, 46% recieving positive outcomes, however details of the techniques used were insufficient and a variety of techniques were used as it was down to the practitioner to decide which technique would be used.
- Neurodynamics - Gliding and Sliding/Tensioning
Another study[27] performed the neurodynamics sliding and tensioning techniques, outlined by Butler[30], whilst having the patient in an upper limb tension positions described by Magee[31], again having positive outcomes in regards to pain and function.
Overall a study by Persson et al[32] highlighted that there was no significant difference between outcome measures of patients who had had surgery, physiotherapy or cervical collar explaining that physiotherapy is at least as effective as surgery.
When performing manual therapy on the neck it is important to to be aware of any potential risk factors such as arterial insufficiency, Hypertension, Craniovertbral ligament insufficiency and upper motor neurone disorders[33].
Exercise Therapy[edit | edit source]
Exercises targeted at opening the intervertebral foramen are the best choice for reducing the impact of radiculopathy. Exercises such as contralateral rotation and sideflexion are amongst the simplest forms of exercises which are effective against signs and symptons, given in the form of active ROM[34]. Due to the intricate and close relationship of muscles on the intervertebral foramen and the likely presentation of reduced ROM, stretching is also an effective form of treatment to regain ROM[35].
Once ROM increases strengthening can also be utilised to create new stability and reduce the risk of developing nerve root irritation in the future, as long as it is not caused by a structure which cannot be influenece by physiotherapy. During the initial stages of treatment, strengthening should be limited to isometric exercises in the involved upper limb. Once the radicular symptoms have been resolved, progressive isotonic strengthening can begin. This should initially stress low weight and high repetitions (15-20 repetitions). Closed kinetic chain activities can be very helpful in rehabilitating weak shoulder girdle muscles. However, a multicenter randomized controlled trial found no significant difference with the addition of specific neck stabilization exercises to a program of general neck advice and exercise[35][36]
Prognosis[edit | edit source]
Regarding physical therapy interventions, in 2007 Joshua Cleland and colleagues examined the predictors of positive short-term outcomes in people with a clinical diagnosis of cervical radiculopathy. The following clinical features were found to be most predictive of a positive short-term outcome:
- Age <54
- Dominant arm not affected
- Looking down does not worsen symptoms
- Treatment involves manual therapy, cervical traction, and deep neck flexor strengthening for at least 50% of visits
If 3 of these features are present, the probability of success is 85%, and increases to 90% if all 4 are present[37]
Key Evidence[edit | edit source]
The following are key evidence pieces for physical therapy interventions as they relate to both cervical radiculopathy and neck pain in general:
- Manual therapy compared to 'usual' physical therapy and general practitioner care[38]
- Clinical Practice Guidelines[39]
- Classification System for Neck Pain[40]
- Proposal of Treatment-Based Classification System[41]
- Prognostic factors for neck pain in the general population[42]
- Immediate effects of thoracic manipulation for patients with neck pain[43]
- Clinical prediction rule for thoracic manipulation in patients with neck pain[44]
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1te-EkLj_9jpgNC-jko6UJ7YMs5JbVD6Kxvy9L0i-rZQe-cEFb|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1HAC9OLsDE6IY3VNDEJiQ1T1PtAgZ6HIPXZmWdr5m3EUp_o916|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1FQ_Hz0ueKYrijP-RUp8OTCPcXeD93_TZpxk5OeUNUM1us1YW4|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=10WuL-PqA2AcCL2SCvSTAgK0mBQ5-9KHWon5221dBAkDerqQkC|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1bmzyevNxeknWLiS61IY6m9VzycnTYBRZFG7O7P6VrA5OO29Tj|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1XKgVAYRUbsND-tSO9HWh5F8wKS92vNzcfI7DhtcgM0QEweIoG|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1PUPW_FOWnJATlJ-BvmJiDMobqfTqr5Ry-qTKPFzLPcnSnTsUC|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=12cYCaYYmd3KKH2ZbY--PFg5cz0WbUCrZ_jjoHrLPdJMOa0Y5B|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1NosRw4HLZNUZT0tNPU8mh6HsSTM99PnO7ZN8qWNgoH25DKMdw|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1zoXkRH9ZTQV9qqKu9gm7THn_aoG_u64kcd2bYWy2oSw7r9EN2|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=16YUOEaK6JjMWOKsO3g3O4OsfM61TPApcKUi4j-1fidkhgeI6T|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=18Cx71VHHP30UEkmjQMlwtsQfseQofyKVLswMuJ0_7l1GGsIt5|charset=UTF-8|short|max=10: Error parsing XML for RSS Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1XqGRY609FjiTKhFvt58h2Wou8inCBZcoZ5xkTdrA-ObZQ9wQb|charset=UTF-8|short|max=10: Error parsing XML for RSS
Read 4 Credit[edit | edit source]
|
Would you like to earn certification to prove your knowledge on this topic? All you need to do is pass the quiz relating to this page in the Physiopedia member area. |
References[edit | edit source]
- ↑ Eubanks J. Cervical Radiculopathy: Nonoperative Management of Neck Pain and Radicular Symptoms. Am Fam Physician. 2010 Jan 1;81(1):33-40.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Eubanks, JD.Cervical Radiculopathy:Nonoperative Management of Neck Pain and Radicular Symptoms.American Family Physician 2010;81,33-40
- ↑ 3.0 3.1 3.2 Kenneth A. Olson. Manual physical therapy of the spine.Saunders Elsevier 2009.p 253, 257, 258
- ↑ Marc J. Levine, Todd J. Albert, Michael D. Smith.Cervical Radiculopathy: Diagnosis and Nonoperative Management.Journal of the American Academy of Orthopaedic Surgeons 1996;4:305-316
- ↑ 5.0 5.1 Ellenberg M, Honet J, Treanor W. Cervical Radiculopathy. Arch Phys Med Rehabil. 1994; 75:342-352. LoE: 2A
- ↑ 6.0 6.1 Radhaknshnank et al. Epidemiology of Cervical Radiculopathy. A Population Based Study. Brain. 1994: 117; 325-335 LoE: 2C
- ↑ 7.0 7.1 7.2 7.3 Lipetz JS. Pathophysiology of Inflammatory, Degenerative, and Compressive Radiculopathies. Phys Med Rehabil Clin N Am. 2002;13:439-449
- ↑ Tanaka N. et al, The anatomic relation among the nerve roots, intervertebral foramina, and intervertebral discs ofthe cervical spine. Spine. 2000 February; 25(3): 286-291fckLRLoE: 2B
- ↑ 9.0 9.1 9.2 9.3 Young IA,Michener LA,Cleland JA,Aguilera AJ,Snyder AR.Manual therapy, exercise, and traction for patients with cervical radiculopathy: a randomize clinical trial.Physical Therapy 2009;89:632-642 (B)
- ↑ Radhakrishnan K, Litchy WJ, O'Fallon M, et al. Epidemiology of cervical radiculopathy: A population-based study from Rochester, Minnesota, 1976 through 1990. Brain 1994; 117:325-335.
- ↑ 11.0 11.1 Bogduk N. Twomey CT. Clinically Relevant Anatomy for the Lumbar Spine. 2ed. Edinburgh UK: Churchill Livingston. 1991
- ↑ 12.0 12.1 12.2 Barrett I. et al. Cervical Radiculopathy Epidemiology, Etiology, Diagnosis, and Treatment. Journal of Spinal Disorders &amp;amp;amp;amp;Techniques. April 2015; 28:5. LoE: 2A
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 Kuijper B. et al. Degenerative cervical radiculopathy: diagnosis and conservative treatment: A review. European journal of neurology. 2009; 16(1): 15-20fckLRLoE: 2A Cite error: Invalid
<ref>tag; name "Kuijper" defined multiple times with different content Cite error: Invalid<ref>tag; name "Kuijper" defined multiple times with different content Cite error: Invalid<ref>tag; name "Kuijper" defined multiple times with different content Cite error: Invalid<ref>tag; name "Kuijper" defined multiple times with different content - ↑ Kenneth W. Lindsay, Ian Bone.Neurology and neurosurgery illustrated.4th ed. Churchill Livingstone.p408
- ↑ Kuijper B, Tans JT, Beelen A, Nollet F, de Visser M.Cervical collar or physiotherapy versus wait and see policy for recent onset cervical radiculopathy : randomised trial.BMJ 2009;p1-7
- ↑ C: R. Erhard et al. Cervical Radiculopathy or Parsonage-Turner Syndrome: Differential Diagnosis of a Patient With Neck and Upper Extremity Symptoms. JOSPT. OCTOBER 2005fckLRVolume 35, No. 10 LoE: 3B
- ↑ Gu R., et al. Differential diagnosis of cervical radiculopathy and superior pulmonary sulcus tumor. Chinese medical journal. 2012 August; 125(15): 2755-2757 LoE: 3B
- ↑ Partanen J, Partanen K, Oikarinen H, et al. Preoperative electroneuromyography and myelography in cervical root compression. Electromyogr Clin Neurophysiol. 1991; 31:21-26.
- ↑ Dillingham TR et al. Identification of cervical radiculopathies.American journal of physical medicine and rehabilitation. Feb 2001. 80(2): 84-91. LoE: 2B
- ↑ Lalkhen A. McCluskey A. Clinical tests: sensitivity and specificity. Contin Educ Anaesth Crit Care Pain (2008) 8 (6): 221-223.
- ↑ Wainner RS, Fritz JM, Irrgang JJ, et al. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28(1):52-62.
- ↑ C: Wainner et al. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine 2003 Jan 1. 28(1):52-62.
- ↑ A1: Sidney M. Rubinstein et al. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. European Spine Journal. Volume 16, Number 3, 307-319
- ↑ Heckmann J, Lang J, Zobelein I, et al. Herniated cervical intervertebral discs with radiculopathy: an outcome study of conservatively or surgically treated patients. J Spinal Disord. 1999;12:396-401.
- ↑ Boyles, Robert; Toy, Patrick; Mellon, James; Hayes, Margaret; Hammer, Bradley.Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review Journal of Manual and Manipulative Therapy 19 (2011) 135-142.
- ↑ Boyles R. Toy P. Mellon J. Hayes M.Hammer B. Effectiveness of manual physical therapy in the treatment of cervical radiculopathy a systematic review. Journal of Manipulative therapy. 19 (3) 2011
- ↑ 27.0 27.1 27.2 Ragonese J. A randomized trial comparing manual physical therapy to therapeutic exercises, to a combination of therapies,for the treatment of cervical radiculopathy. Orthop Prac 2009;21(3):71–7.
- ↑ Maitland G. Vertebral manipulation. Oxford: Butterworths;fckLR1986
- ↑ Cleland JA, Whitman JM, Fritz JM, Palmer JA. Manual physical therapy, cervical traction, and strengthening exercises in patients with cervical radiculopathy: a case series. J Ortho Sports Phys Ther 2005;35:802–11.
- ↑ Butler, 0 (1991). Mobilisation of the Nervous System, Churchill Livingstone, Edinburgh
- ↑ Magee DJ. Orthopedic physical assessment. 5th ed. St. Louis,MO: Saunders Elsevier; 2008.
- ↑ Persson LC, Carlsson CA, Carlsson JY. Long lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar. A prospective, randomized study. Spine 1997;22(7):751–8
- ↑ Rushton A, Rivett D, Carlesso L, Flynn T, Hing W, Kerry R. International Framework for Examination of the Cervical Region http://www.physio-pedia.com/Section_5:_Physical_examination
- ↑ Langevin P. Rou JS. Desmeules F. Cervical radiculopathy: Study protocol of a randomised clinical trial evaluating the effect of mobilisations and exercises targeting the opening of intervertebral foramen. BMC Msk Disorders.13:10 2012.
- ↑ 35.0 35.1 Malanga G. Sherwin SW.Cervical Radiculopathy Treatment &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Management 2013 [ONLINE]fckLRAvailable from http://emedicine.medscape.com/article/94118-treatment#aw2aab6b6b2
- ↑ Griffiths C, Dziedzic K, Waterfield J, Sim J. Effectiveness of specific neck stabilization exercises or a general neck exercise program for chronic neck disorders: a randomized controlled trial. J Rheumatol. Feb 2009;36(2):390-7
- ↑ Cleland JA, Fritz JM, Whitman JM, et al. Predictors of short-term outcomes in people with a clinical diagnosis of cervical radiculopathy. Phys Ther. 2007;87(12):1619-1632.
- ↑ Hoving JL, Koes BW, de Vet HC, et al. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. Ann Intern Med. 2002;136(10):713-722.
- ↑ Childs JD, Cleland JA, Elliott JM, et al. Neck Pain: Clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Assoction. J Orthop Sports Phys Ther. 2008;38(9):A1-A34.
- ↑ Childs JD, Fritz JM, Piva SR, et al. Proposal of a Classification System for Patients with Neck Pain. J Orthop Sports Phys Ther. 2004;34(11):686-700.
- ↑ Fritz JM and Brennan GP. Preliminary Examination of a Proposed Treatment-Based Classification System for Patients Receiving Physical Therapy Interventions for Neck Pain. Phys Ther. 2007;87(5):513-524.
- ↑ Carroll LJ, Hogg-Johnson S, van der Velde G, et al. Course and Prognostic Factors for Neck Pain in the General Population. Spine. 2008;33(4S):S75-S82.
- ↑ Cleland JA, Childs JD, McRae M, et al. Immediate effects of thoracic manipulation in patients with neck pain: a randomized clinical trial. Man Ther. 2005;10:127-135.
- ↑ Cleland JA, Childs JD, Fritz JM, et al. Development of a Clinical Prediction Rule for Guiding Treatment of a Subgroup of Patients with Neck Pain: Use of Thoracic Spine Manipulation, Exercise, and Patient Education. Phys Ther. 2007;87(1):9-23.