Personal Protective Equipment (PPE)
Introduction[edit | edit source]
Protecting ourselves so that we can continue to help others, is a priority for health care providers around the world. This includes being conscious and up to date with infection prevention and control measures and the appropriate implementation of personal protective equipment (PPE), hand hygiene and waste management of potentially harmful materials.
According to the World Health Organization (WHO), personal protective equipment "...consists of garments placed to protect the health care workers or any other persons to get infected"[1]
Medical PPE typically includes face protection, goggles and mask or face shield, gloves, gown or coverall, head cover, and rubber boots.
The following page addresses specifically medical PPE, for the protection against possible external infectious pathogens or substances.
Hierarchy of Safety and Health Controls[edit | edit source]
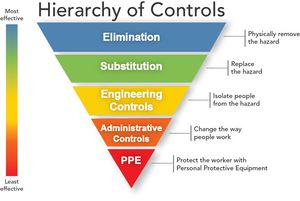
According to the Occupational Safety and Health Administration (OSHA) the protection of healthcare workers from infectious disease exposures in the workplace requires a combination of controls:
- Training and administrative controls: By providing appropriate safety and infection control training to healthcare professionals, and administrative controls such as establishing and applying isolation policies and procedures, also procedures to identify patients with communicable diseases before the exposure to the healthcare worker.
- Engineering controls: such as negative pressure rooms for patients with airborne diseases such as Tuberculosis (TB)
- Work practice control: for example, not recapping needles.
- Personal Protective Equipment (PPE): Although PPE is at the end of the hierarchy of prevention, it is very important for protecting healthcare workers from disease transmission.
Types of PPE[edit | edit source]
- Gloves: Protects your hands from microbes and minimizes the possible spreading of microbes.
- Masks: Cover your mouth and nasal area. Some masks have a see-through plastic piece, which also covers your eyes (shield). A special respiratory mask (respirator) forms a tight seal around your nose and mouth. It can be useful to minimize the inhalation of smaller microbes, such as tuberculosis bacteria. Click here for a comprehensive guide on selecting the appropriate face mask.
- Eye protection: This includes face shields as well as goggles. They can protect the mucous membranes of your eyes from bodily fluids. If the fluids make contact with the eyes, microbes within the fluid can enter the body through the mucous membranes.
- Clothing: Includes gowns, aprons, head covering, and shoe covers.
Where We Should Use PPE[edit | edit source]
PPE is used in all healthcare settings:
- Acute Care
- Long Term Care
- Outpatient Care
- Community Care
PPE is needed where contact occurs with patients, residents, and clients (PRC). The PRCs environment certainly includes physiotherapy departments, clinics and a physiotherapy treatment room in a long term care facility.
General PPE Guidelines (as outlined by OSHA)[edit | edit source]
- Wear gloves, when handling chemicals and/or body fluids.
- Wear safety shoes/boots/covers if hazardous or infectious substances are likely to splash.
- Wear an apron/gown/coveralls- if hazardous or infectious substances are likely to splash.
- Use a respirator: when hazardous or infectious substances are airborne such as tuberculosis.
- Wear hearing protection: for loud noises such as from equipment.
- Remove PPE carefully to avoid contaminating yourself.
- Dispose of PPE in designated containers before leaving the area.
Selection of Appropriate PPE[edit | edit source]
It is important to consider the following factors influencing the selection of PPE:
- Type of anticipated exposure: Such as from touch or surfaces, splashes or sprays, or large volumes of bodily fluids, which may seep through the clothing. PPE selection (and combinations of PPE), is determined by the category of isolation of the patient being treated (see the link below from the CDC).
- Durability and appropriateness of the PPE for the task. This will affect, for example, whether a gown or apron is selected. If a gown is required, the type of gown is also important. Does it need to be fluid resistant, fluid proof, both or neither?
- Fitting. PPE must fit the individual user (form a proper seal). For example; if a glove is too large / too small than the person's hand, it will compromise the level of protection while also affecting the dexterity of the health care provider.
Full list of recommendations for the application of standard precautions for the care of all patients in all healthcare settings, according to the Centre for Disease Control and Prevention (CDC - US).
There are also some limiting factors to consider when wearing PPE in a healthcare environment. It is important to have a full understanding of the different types of PPE when making your selection based on the purpose and goal of the protection.
Using a head or full body ventilated PPE suit equipped with powered-air-purifying-respirators was found to cause reduced dexterity due to multiple glove layering. Back pain related to the respirator of the fully ventilated suit and impaired visibility by a flexible face shield may also be an issue. The temperature of the work environment may also have an impact on healthcare workers; working at a temperature of 28°C wearing a full-body ventilated PPE may cause heat stress and dehydration, whereas a temperature of 22°C had no negative impact on the same physical parameters[2].
The WHO recommends that airborne and contact precautions should be followed when performing aerosol-generating procedures.[3]
This includes the use of N95/respirators, eye protection, gloves and gowns (Aprons should also be used if gowns are not fluid-resistant)[4] However, follow your local guidelines, as there are inconsistencies in the recommendations of organizations and countries.
Different Types of Personal Protective Equipment[edit | edit source]
Medical Gloves[edit | edit source]
Medical gloves are examples of personal protective equipment that are used to protect the wearer and/or the patient from the spread of infection or illness during medical procedures and examinations. Medical gloves are one part of an infection-control strategy.
Gloves should be worn if you anticipate being exposed to the following situations or substances:[6]
- Blood or body substances—fluids and solids
- Mucous membranes—oral, nasal, conjunctival, rectal, genital
- Non-intact skin—wounds, surgical incisions
- Indwelling device insertion site—urinary and intravenous catheters, feeding tube
- Potentially contaminated items in the resident's environment
- Visibly soiled equipment, supplies, or linens that may have been in contact with blood or body fluids.
- Shared equipment moving between residents
Types of Gloves[edit | edit source]
- Polythene: Thin and have a tendency to tear. They are not an appropriate choice for healthcare settings.
- Vinyl: They have been shown to be less effective than latex gloves in providing an impermeable barrier against microorganisms. They are also loose-fitting and unsuitable for procedures that require manual dexterity. The use of vinyl gloves in healthcare is limited.
- Latex including DPNRL (De Proteinised Natural Rubber Latex): Closer fitting than vinyl and provide a more effective barrier against microorganisms. They should be non-powdered and have the lowest level of extractable protein available. If a healthcare worker has a suspected latex allergy, they should not wear latex gloves. Similarly, when caring for a patient who is known to be sensitive to latex, an alternative should also be available for use. Most Healthcare settings are now becoming latex-free due to the allergy risk to patients and staff.
- Nitrile (acrylonitrile): Comparable to natural rubber latex in providing a biological barrier but arguably afford less elasticity. Nitrile gloves are the common choice of gloves for use where a latex-free environment is required. There have however been reports of healthcare workers also developing allergic reactions to nitrile.
- Neoprene: Also have similar properties to natural rubber latex and are often a popular replacement in situations when a latex-free glove is required and manual dexterity is important e.g. surgery. They are a more expensive alternative to natural rubber latex gloves.[7][8]
Do’s and Don’ts of Glove Use[edit | edit source]
The way you use the gloves influences the risk of infections and disease transmission in a healthcare setting. The following are the most important do’s and don’ts of glove use:
- Work from clean to dirty: This refers to touching clean body sites or surfaces before you touch dirty or heavily contaminated areas.
- Limit opportunities for “touch contamination” - protect yourself, others and environmental surfaces. Examples of touch contamination include: adjusting your glasses, rubbing your nose or scratching your face with a glove that has been in contact with a patient. Also, avoid unnecessarily touching environmental surfaces with contaminated gloves. Surfaces such as light switches, door and cabinet knobs can become contaminated if touched by soiled gloves.
- Change gloves as needed. Always change the gloves after use for each patient, and discard them in the nearest appropriate receptacle.
- The CDC does not recommend the use of double gloves when providing care to a suspected or confirmed COVID-19 patient.[10]
Click here for excellent "Dos and Don'ts" educational pamphlets for download, for healthcare workers.
Gowns or Aprons?[edit | edit source]
There are 3 factors influencing the selection of a gown or apron:
- The purpose of use: Isolation gowns are generally the preferred PPE for clothing, but aprons are occasionally used where limited contamination is anticipated. If contamination of the arms can be anticipated, a gown should be selected. Gowns should fully cover the torso, fit comfortably over the body and have long sleeves that fit snuggly at the wrist.
- The material properties of the gown: Isolation gowns are made either of cotton or a spun synthetic material which dictates whether they can be laundered and reused or must be disposed of. Cotton and spun synthetic isolation gowns vary in their degree of fluid resistance, another factor that must be considered in the selection of this type of PPE. If fluid penetration is likely, a fluid-resistant gown should be used.
- Patient risks and whether a clean, rather than a sterile gown, can be used. Clean gowns are generally used for isolation precautions. Sterile gowns are only necessary for performing invasive procedures, such as inserting a central line. In this case, a sterile gown is best for both patient and healthcare worker protection.
For contact precaution, long-sleeved water-resistant gowns and gloves are recommended.[4]
Face Protection[edit | edit source]
Masks should fully cover the nose and mouth and prevent any fluid penetration. Masks should fit snuggly over the nose and mouth. Please note that facial hair can compromise the seal of a face mask. This should be a consideration for the healthcare provider if you are regularly required to wear a face mask in your work environment.
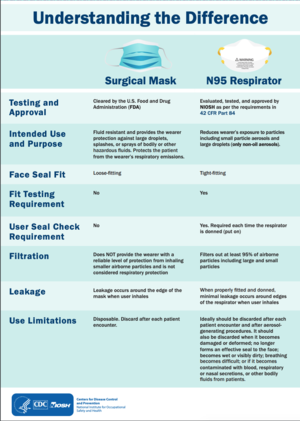
Masks also have a flexible nose piece and can be secured to the head with string ties or elastic. It is important to understand the different types of masks and their recommended usage. Not all masks and filtering facepieces (FFP) offer the same protection and it is important to understand the use and limitations of each one[11]. See the table below:
N95 or FFP2 masks: N95 and surgical masks (face masks) are examples of personal protective equipment that are used to protect the wearer from airborne particles and from liquid contaminating the face. An FFP2 mask is a disposable dust mask, that offers mid-range protection typically used for moderate level fine dust/oil or water-based mists, plastering, sanding and wood dust. Click here for a helpful article from Forbes: Should you Get a Face Mask?
An
An important note: The Centers for Disease Control and Prevention (CDC) does not recommend that the general public wear N95 respirators to protect themselves from respiratory diseases, including coronavirus (COVID-19). The best way to prevent illness is to avoid being exposed to this virus. However, as a reminder, CDC always recommends everyday preventive actions, such as hand washing, to help prevent the spread of respiratory diseases.
CDCs recommendations for the use of N95 Filtering Facepiece Respirators in Healthcare Settings.
Surgical Face Mask: Surgical face masks are to be used for different purposes than the N95 mask. A surgical face mask is a loose-fitting, disposable device that creates a physical barrier between the mouth and nose of the wearer and potential contaminants in the immediate environment. These are often referred to as face masks, although not all face masks are regulated as surgical masks. Note that the edges of the mask are not designed to form a seal around the nose and mouth (Information outlined by the FDA).
Note - use of a mask is generally insufficient to provide complete protection and should be combined with other measures and/or PPEs depending on the context.
COVID19 WHO guidance on the use of medical masks in healthcare-related settings.
Goggles provide barrier protection for the eyes. They should fit snuggly over and around the eyes. Goggles with anti-fog features will help maintain clarity of vision.
When skin protection, in addition to mouth, nose, and eye protection, is required; for example, when irrigating a wound or suctioning copious secretions, a face shield can be used as a substitute to wearing a mask or goggles. The face shield should cover the forehead, extend below the chin, and wrap around the side of the face.
Respiratory Protection[edit | edit source]
Respiratory protection occurs through the use of face masks as well as respirators.
Common types of respirators used in healthcare settings are [13]:
- Filtering facepiece respirators (FFRs) (such as the N95 respirator)
- Powered air-purifying respirators (PAPRs).
Respirators that filter the air before it is inhaled should be used for respiratory protection to protect healthcare workers from hazardous or infectious aerosols, such as Mycobacterium Tuberculosis. The most commonly used respirators in healthcare settings are the N95, N99, or N100 particulate respirators.
N95 Respirator: The N95 device was designed to achieve a very close facial fit and very efficient filtration of airborne particles. The 'N95' designation means that when subjected to careful testing, the respirator blocks at least 95 per cent of very small (0.3 microns) test particles. If properly fitted, the filtration capabilities of N95 respirators exceed those of face masks. However, even a properly fitted N95 respirator does not completely eliminate the risk of illness or death (Information outlined by the FDA).
As outlined by the FDA "All FDA-cleared N95 respirators are labelled as "single-use," disposable devices. If your respirator is damaged or soiled, or if breathing becomes difficult, you should remove the respirator, discard it properly, and replace it with a new one. To safely discard your N95 respirator, place it in a plastic bag and put it in the trash. Wash your hands after handling the used respirator.
N95 respirators are not designed for children or people with facial hair, because a proper fit cannot be achieved and the respirator may not provide full protection.
Like other types of PPE, the selection of a respirator type must consider the nature of the exposure and risk involved. For example, N95 particulate respirators might be worn by personnel entering the room of a patient with infectious Tuberculosis. However, if bronchoscopy is performed on the patient, the healthcare worker might wear a higher level of respiratory protection, such as a PAPR.
PAPR: A PAPR should be worn for high-risk aerosol-generating procedures. It is a more complicated filtration system and is battery powered. It is composed of a full face mask, a breathing tube, a battery-operated blower, and particulate filters (HEPA only). A PAPR uses a blower to pass contaminated air through a HEPA filter, which removes the contaminant and supplies purified air to the facemask.
- A PAPR may be selected for use if: (Retrieved from Minnesota Department of Health)
- The N95 respirator choice(s) does not fit or is unavailable.
- If the employee has facial hair or facial deformity that would interfere with q mask-to-face seal for an N95 respirator.
- It is to be used for a high-risk aerosol-generating procedure.
- PAPRs can be used by persons who are medically certified, but who cannot wear N95 -disposable respirators.
Prior to the use, it is important to undergo a medical evaluation determining the safety of wearing the respirator, fit testing to determine the appropriate size and type, training on how and when to use the respirator and finally fit checking when donning to ensure a proper seal.
Before Donning PPE[edit | edit source]
- Ensure you are hydrated and have used the bathroom as the PPE may need to be worn for an extended period.
- Don your PPE with a colleague who can assist and provide a final check.
- Perform thorough hand hygiene.
The CDCs downloadable checklist for donning and doffing PPE.
Sequence for Donning PPE[edit | edit source]
The order of which you put on (donning) or remove (doffing) your personal protective equipment is essential for protecting yourself and preventing the spread of any possible contaminants or fluids. The following is the correct sequence for donning your PPE:
- Gown or apron;
- Mask or respirator;
- Goggles or face shields;
- Gloves.
Keep in mind that the combination of PPE used, and the sequence for donning, will be determined by the precautions that need to be taken for each patient.
For an excellent guide on donning (putting on) and doffing (removing) PPE, consult the Infection Control Today website.
Sequence for Doffing PPE[edit | edit source]
It is extremely important to take great care when removing and disposing of used PPE to avoid exposure to infection. It is important to practice before using these techniques in a clinical setting, ideally with a colleague to provide guidance and feedback.
- Gloves;
- Face shield or goggles;
- Gown;
- Mask or respirator.
- Hand hygiene.
The sequence for removing PPE is intended to limit opportunities for self-contamination. The gloves are considered the most contaminated pieces of PPE and are therefore removed first[16].
The Location for Doffing PPE[edit | edit source]
This depends on the amount, and type of PPE, being worn as well as the category of isolation of the patient,
- If only gloves are worn as PPE, it is safe to remove and discard them in the patient's room (in the appropriate bin or receptacle).
- When a gown or full PPE is worn, PPE should be removed at the doorway or in an anteroom.
- Respirators should always be removed outside the patient room after the door is closed.
- Hand hygiene should be performed after all PPE is removed.
There is a risk of contamination of skin and clothing during the removal of contaminated gloves or gowns. It is important to pay attention to the method of removing PPE, in order to avoid contamination and disease transmission. Educating healthcare workers in the correct way of removing PPE by practice in the removal of contaminated PPE with providing immediate visual feedback can reduce the risk of contamination of skin and clothes during removal of PPE [18].
Hand Hygiene[edit | edit source]
Hand hygiene is the cornerstone of preventing infection transmission. You should perform hand hygiene immediately after removing PPE. If your hands become visibly contaminated during PPE removal, wash hands before continuing to remove PPE. Wash your hands thoroughly with soap and warm water or, if hands are not visibly contaminated, use an alcohol-based hand rub. Below is a video that demonstrates the steps of hand hygiene.
Hand Washing Versus Hand Sanitizer?[edit | edit source]
Using hand sanitizer is NOT a replacement for hand washing. As a healthcare provider, hand washing needs to be an automatic reflex between patients, after activities which could promote contact with contaminants or bodily fluids, following the use of the washroom, before and after eating as well as any other activity which may compromise the sanitation of your hands. When in doubt, wash your hands.
It is important to understand that alcohol-based hand sanitizers do not kill all types of germs or bacteria. It is a prudent tool in addition to hand washing, but it should never replace the practice of handwashing and good hygiene.
Here is an excellent promotional pamphlet from the CDC, on Hand Washing vs. Sanitization.
PPE During Shortages[edit | edit source]
Read this guideline on PPE usage when facing a shortage - WHO. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages. Updated 23 Dec 2020
Other helpful Physiopedia Pages:[edit | edit source]
Helpful Resources[edit | edit source]
- World Health Organization - PPE
- Health & Safety Executive (UK)
- The University of Western Australia - What is PPE?
- Center for Disease Control and Prevention - Isolation Precautions
- Guidance and Advice for Health Care Workers regarding PPE
- NHS Training Videos for PPE
- Chemical Hazards Emergency Medical Management - CHEMM
- Responsibilities of the Employer / Employee regarding PPE
- Dos and Don'ts of PPE
- FDA Recommendations for PPE and Infection Control
- PPE Sequences
- Advice on the use of masks in the community, during home care and in health care settings in the context of the novel coronavirus (2019-nCoV) outbreak: World Health Organisation, 29 Jan 2020
References[edit | edit source]
- ↑ Protective Personal Equipment. World Health Organization.https://www.who.int/medical_devices/meddev_ppe/en/. Retrieved on: 13 March 2020.
- ↑ Loibner M, Hagauer S, Schwantzer G, Berghold A, Zatloukal K. Limiting factors for wearing personal protective equipment (PPE) in a health care environment evaluated in a randomised study. PloS one. 2019 Jan 22;14(1):e0210775.
- ↑ WHO. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages. Updated 23 Dec 2020
- ↑ 4.0 4.1 Park SH. Personal protective equipment for healthcare workers during the COVID-19 pandemic. Infection & chemotherapy. 2020 Jun;52(2):165
- ↑ Globus Group.The Globus Guide to Putting-on and Removing Non-Sterile Disposable Gloves. Published on 29 August 2014. Available fromhttps://www.youtube.com/watch?time_continue=2&v=3I_kKVNrEMo&feature=emb_logo. [last accessed 17 March 2020]
- ↑ Siegel JD, Rhinehart E, Jackson M, et al. Centers for Disease Control and Prevention. 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Atlanta, GA: US Department of Health and Human Services, CDC; 2007. Accessed March 13 2020.
- ↑ Coia, J.E. Ritchie, L. Adisesh, A. Makison-Booth, C.Bradley, C. Bunyan, D. Carson, G. Fry, C. Hoffman, P. Jenkins, D. Phin, N. Taylor, B. Nguyen-Van-Tam, Zuckerman, M. Guidance on the use of respiratory and facial protection equipment Journal of Hospital Infection (2013)
- ↑ FRAISE, A . and BRADLEY, C. Ayliffe’s Control of Healthcare-Associated Infection: A Practical Handbook Fifth Ed. (2009)
- ↑ Dentalkart. Learn More About Different Types of Disposable Gloves - DENTALKART. Available from: http://www.youtube.com/watch?v=JFi34jW3M_8[last accessed 28/3/2020]
- ↑ CDC. Strategies for Optimizing the Supply of Disposable Medical Gloves. Updated 23 Dec 2020
- ↑ Lazzeri M, Lanza A, Bellini R, Bellofiore A, Cecchetto S, Colombo A et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Archives for Chest Disease. 2020;90(1).
- ↑ World Health Organisation.What is the correct way to wear and dispose of masks? Published on 5 February 2020. Available fromhttps://www.youtube.com/watch?v=lrvFrH_npQI&feature=emb_logo. [last accessed 17 March 2020]
- ↑ Chughtai, A. A. et al. (2020). Selection and Use of Respiratory Protection by Healthcare Workers to Protect from Infectious Diseases in Hospital Settings. Annals of work exposures and health, [s. l.], DOI 10.1093/annweh/wxaa020.
- ↑ US Department of Labor.Respiratory Protection for Healthcare Workers Training Video. Published on 12 January 2o11. Available from https://www.youtube.com/watch?time_continue=7&v=6qkXV4kmp7c&feature=emb_logo. [last accessed 17 March 2020]
- ↑ Public Health England. COVID-19: Donning of Personal Protective Equipment (PPE). Published on 2 March 2020. Available fromhttps://www.youtube.com/watch?v=kKz_vNGsNhc&feature=emb_logo. [last accessed on 17 March 2020]
- ↑ Cdcgov. Cdcgov. [Online]. Available from: https://www.cdc.gov/niosh/ppe/default.html [Accessed 21 April 2019].
- ↑ Public Health England. COVID-19: Removal and disposal of Personal Protective Equipment (PPE) Published on 2 March 2020. Available from https://www.youtube.com/watch?time_continue=2&v=oUo5O1JmLH0&feature=emb_logo, [last accessed 17 March 2020]
- ↑ Tomas ME, Kundrapu S, Thota P, Sunkesula VC, Cadnum JL, Mana TS, Jencson A, O’donnell M, Zabarsky TF, Hecker MT, Ray AJ. Contamination of health care personnel during removal of personal protective equipment. JAMA internal medicine. 2015 Dec 1;175(12):1904-10.
- ↑ Johns Hopkins Medicine.Hand-washing Steps Using the WHO Technique. Published on 26 March 2019. Available fromhttps://www.youtube.com/watch?v=IisgnbMfKvI&feature=emb_logo. [last accessed 17 March 2020]
- ↑ WHO: How to handrub? With alcohol-based formulation, World Health Organisation, Oct 2015, https://www.youtube.com/watch?v=ZnSjFr6J9HI [last accessed 29 May 2020]