Normal Pressure Hydrocephalus
Original Editor - David Olukayode
Top Contributors - David Olukayode
Introduction[edit | edit source]
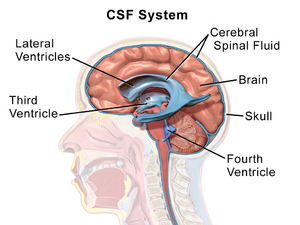
Normal Pressure Hydrocephalus (NPH) occurs when cerebrospinal fluid (CSF) accumulates due to obstructed flow or excess production, resulting in gait and memory problems as well as urinary incontinence.[1] These classic triad of symptoms: gait disturbance (wobbly), urinary incontinence (wet), and dementia (wacky) were first described by Hakim and Adams.[2] To consider the diagnosis, gait disturbance plus one other characteristic is usually required.[3]
Etiology[edit | edit source]
NPH is of two types:
- Idiopathic or primary NPH (without any identifiable cause)
- Symptomatic or secondary NPH (caused by risk factors like traumatic brain injury, brain infection, subarachnoid haemorrhage, tumor, or radiation contributing to hydrocephalus) [4][1]
Both idiopathic NPH and secondary NPH share the fact that they are communicating types of hydrocephalus with similar prognoses. The key distinction between them is that secondary NPH affects people of all ages, whereas idiopathic NPH is mostly a disease of the elderly.[4]Since the causes of secondary NPH has been made clear, this article will focus of idiopathic NPH.
Epidemiology[edit | edit source]
The most extensive population-based investigation on the prevalence of idiopathic NPH in Western Sweden reported that 0.2% of people aged 70 to 79 years and 5.9% of those aged 80 and older met guideline criteria for probable idiopathic NPH. The majority of idiopathic NPH patients were over the age of 80.[5]Men and women are equally afflicted, and the average age of onset is around 70 years. It is estimated that idiopathic NPH accounts for 6% of all dementia cases. The estimated prevalence of normal pressure hydrocephalus is reported to be 0.003% in people under the age of 65 and 0.2% to 2.9% in people 65 and older. The estimated incidence of normal pressure hydrocephalus is 0.2 to 5.5 per 100000 person-years.[6][7][8]
Pathogenesis[edit | edit source]
The actual pathogenesis process of idiopathic NPH remains cloudy.[9]However some studies have identified some mechanisms leading to the condition.[10][11][12][13][14][15]Some of these mechanisms are:
- High dynamic flow of CSF in the ventricular aqueduct
- Increase in the pulse pressure of CSF
- Reduced CSF reabsorption in the venous system due to increased resistance
- Reduction in cerebral blood flow
- CSF absorption via aberrant processes such as transependymal flow rather than through Pacchionian granulations
- Failure of drainage vasoactive metabolites to drain
- Altering of the expression of CSF tumor necrosis factor-alpha (which has been shown to control CSF synthesis) and transforming growth factor-beta
Causes of gait disturbance:
- Interstitial edema causes the corticospinal tract fibers that supply the legs and pass close to the lateral ventricles in the corona radiata to stretch and compress when the intracranial pressure rises
- Compression of the pedunculopontine nucleus and other brainstem structures
- Poor blood flow to the prefrontal and periventricular white matter
Causes of dementia:
- Radial shearing pressures cause dementia when the ventricles continue to grow and the cortex pushes up against the calvarium's inner table.
Causes of bladder incontinence:
- Early in the disease, stretching of the corticospinal tract's periventricular sacral fibers results in a loss of voluntary (supraspinal) control over bladder contractions; later on, dementia may increase the risk of incontinence.[16][17]
Signs and symptoms[edit | edit source]
Although there could be other symptoms asides the classical "wet, wobbly and wacky", hemiparesis or paraparesis should not be present since these suggest a myelopathy.[18]The three classical triad of presentation of NPH are:
- Gait abnormality: The gait impairment in idiopathic NPH is best described as a higher-level gait disorder, which involves difficulty integrating sensory information about the position of the body in its environment, including the effect of gravity, and properly choosing and carrying out motor plans for gait or postural reflexes in the absence of primary sensorimotor deficits, cerebellar dysfunction, or involuntary movements.[19][20]Unless concurrent musculoskeletal diseases (such as those of the knees, hips, or spine) result in asymmetry, the impairment should be symmetric. Inconclusive gait initiation, shuffling, and inadequate foot clearance, tripping, falling, or festination, unstable multistep turns, and retropulsion or anteropulsion are among the findings. Transitional movements (from sitting to standing or from standing to sitting) are also challenging.[20][21]
- Dementia: The signs of dementia in idiopathic NPH are similar to those of other dementias, such as having trouble driving, managing finances, taking prescriptions as prescribed, and remembering appointments. Instead of dementia, some idiopathic NPH patients first have moderate cognitive impairment. It is encouraged to take screening tests like the Mini-Mental State Examination (MMSE) or the Montreal Cognitive Assessment (MoCA).[22]
- Urinary urgency and incontinence: The most typical urinary symptoms are urgency and frequency, which can happen with or without incontinence.[23]
Imaging[edit | edit source]
For the diagnosis of idiopathic NPH, neuroimaging with either computed tomography (CT) or magnetic resonance imaging (MRI) is necessary, though MRI is recommended. The third and lateral ventricles are enlarged in idiopathic NPH, and CSF flow ought to be unhindered. An MRI should be performed to look for obstruction sites if obstructive hydrocephalus, which affects a tiny number of people, is suspected. The Evans ratio or index, which is the ratio of the largest frontal horn span to the largest diameter of the brain on the same axial imaging, is a screening test for ventricular enlargement. Although it is not specific for idiopathic NPH, an Evans ratio of more than 0.3 and more than 0.33 both imply large ventricles and extremely large ventricles, respectively.[18]
Note: Check out the cited article for an image of the Evans ratio.
Treatment and management[edit | edit source]
- Surgery: In about 60% of patients of idiopathic NPH, CSF shunt procedures like, ventriculoperitoneal, ventriculopleural, or ventriculoatrial shunting, can lead to substantial improvement.[24][25]
- Acupuncture: There is early evidence that patients with dementia can improve to varying degrees with Chinese medicine. A three-month course of treatment with acupuncture dramatically lessens cognitive impairment in those with dementia and predementia.[26][27]
- Physiotherapy: In order to increase the frequency and endurance of lower limb active movement, the ideal physiotherapy for both nonoperative and postoperative patients is to motivate them to engage in off-bed activities.[28] Core strengthening, balance training, coordination training, gait training, strength training for the upper and lower limbs is highly beneficial as well. Lastly, exercise at home, as prescribed by the Physiotherapist is crucial for people with idiopathic NPH because it dramatically improves their performance in everyday activities, static balance, functional capacity, dynamic balance, and gait.[29]
References[edit | edit source]
- ↑ 1.0 1.1 Patel S, Ditamo M, Mangal R, Gould M, Ganti L. Normal Pressure Hydrocephalus. Cureus. 2023 Feb 18;15(2):e35131. doi: 10.7759/cureus.35131. PMID: 36949988; PMCID: PMC10026533.
- ↑ Hakim S, Adams RD. The special clinical problem of symptomatic hydrocephalus with normal cerebrospinal fluid pressure. Observations on cerebrospinal fluid hydrodynamics. J Neurol Sci. 1965;2:307–327.
- ↑ Shprecher D, Schwalb J, Kurlan R. Normal pressure hydrocephalus: diagnosis and treatment. Curr Neurol Neurosci Rep. 2008 Sep;8(5):371-6. doi: 10.1007/s11910-008-0058-2. PMID: 18713572; PMCID: PMC2674287.
- ↑ 4.0 4.1 M Das J, Biagioni MC. Normal Pressure Hydrocephalus. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
- ↑ Jaraj D, Rabiei K, Marlow T, Jensen C, Skoog I, Wikkelsø C. Prevalence of idiopathic normal-pressure hydrocephalus. Neurology. 2014 Apr 22;82(16):1449-54.
- ↑ Brean A, Fredø HL, Sollid S, Müller T, Sundstrøm T, Eide PK. Five-year incidence of surgery for idiopathic normal pressure hydrocephalus in Norway. Acta Neurol Scand. 2009 Nov;120(5):314-6.
- ↑ Tanaka N, Yamaguchi S, Ishikawa H, Ishii H, Meguro K. Prevalence of possible idiopathic normal-pressure hydrocephalus in Japan: the Osaki-Tajiri project. Neuroepidemiology. 2009;32(3):171-5.
- ↑ Krauss JK, Halve B. Normal pressure hydrocephalus: survey on contemporary diagnostic algorithms and therapeutic decision-making in clinical practice. Acta Neurochir (Wien). 2004 Apr;146(4):379-88; discussion 388.
- ↑ Edwards RJ, Dombrowski SM, Luciano MG, Pople IK. Chronic hydrocephalus in adults. Brain Pathol. 2004 Jul;14(3):325-36.
- ↑ Owler BK, Pickard JD. Normal pressure hydrocephalus and cerebral blood flow: a review. Acta Neurol Scand. 2001 Dec;104(6):325-42.
- ↑ Tarkowski E, Tullberg M, Fredman P, Wikkelsö C. Normal pressure hydrocephalus triggers intrathecal production of TNF-alpha. Neurobiol Aging. 2003 Sep;24(5):707-14
- ↑ Li X, Miyajima M, Jiang C, Arai H. Expression of TGF-betas and TGF-beta type II receptor in cerebrospinal fluid of patients with idiopathic normal pressure hydrocephalus. Neurosci Lett. 2007 Feb 14;413(2):141-4.
- ↑ Silverberg GD. Normal pressure hydrocephalus (NPH): ischaemia, CSF stagnation or both. Brain. 2004 May;127(Pt 5):947-8.
- ↑ Bateman GA. Vascular compliance in normal pressure hydrocephalus. AJNR Am J Neuroradiol. 2000 Oct;21(9):1574-85.
- ↑ Greitz D. Radiological assessment of hydrocephalus: new theories and implications for therapy. Neurosurg Rev. 2004 Jul;27(3):145-65; discussion 166-7.
- ↑ Gleason PL, Black PM, Matsumae M. The neurobiology of normal pressure hydrocephalus. Neurosurg Clin N Am. 1993 Oct;4(4):667-75.
- ↑ Corkill RG, Cadoux-Hudson TA. Normal pressure hydrocephalus: developments in determining surgical prognosis. Curr Opin Neurol. 1999 Dec;12(6):671-7.
- ↑ 18.0 18.1 Williams MA, Malm J. Diagnosis and Treatment of Idiopathic Normal Pressure Hydrocephalus. Continuum (Minneap Minn). 2016 Apr;22(2 Dementia):579-99. doi: 10.1212/CON.0000000000000305. PMID: 27042909; PMCID: PMC5390935.
- ↑ Nutt JG, Lang AE. Balance and gait disorders. Presented at: 63rd Annual Meeting of the American Academy of Neurology; 2011; Honolulu, Hawaii.
- ↑ 20.0 20.1 Stolze H, Kuhtz-Buschbeck JP, Drücke H, et al. Gait analysis in idiopathic normal pressure hydrocephalus—which parameters respond to the CSF tap test? Clin Neurophysiol 2000; 111(9): 1678– 1686. doi:10.1016/S1388-2457(00)00362-X.
- ↑ Nutt JG, Marsden CD, Thompson PD. Human walking and higher-level gait disorders, particularly in the elderly. Neurology 1993; 43(2): 268– 279. doi:10.1212/WNL.43.2.268.
- ↑ Behrens A, Eklund A, Elgh E, et al. A computerized neuropsychological test battery designed for idiopathic normal pressure hydrocephalus. Fluids Barriers CNS 2014; 11: 22 doi:10.1186/2045-8118-11-22.
- ↑ Sakakibara R, Kanda T, Sekido T, et al. Mechanism of bladder dysfunction in idiopathic normal pressure hydrocephalus. Neurourol Urodyn 2008; 27(6): 507– 510. doi:10.1002/nau.20547.
- ↑ Hebb AO, Cusimano MD. Idiopathic normal pressure hydrocephalus: a systematic review of diagnosis and outcome. Neurosurgery. 2001;49:1166–1184. discussion 1184–1186.
- ↑ Nakajima M, Yamada S, Miyajima M, Ishii K, Kuriyama N, Kazui H, Kanemoto H, Suehiro T, Yoshiyama K, Kameda M, Kajimoto Y, Mase M, Murai H, Kita D, Kimura T, Samejima N, Tokuda T, Kaijima M, Akiba C, Kawamura K, Atsuchi M, Hirata Y, Matsumae M, Sasaki M, Yamashita F, Aoki S, Irie R, Miyake H, Kato T, Mori E, Ishikawa M, Date I, Arai H; research committee of idiopathic normal pressure hydrocephalus. Guidelines for Management of Idiopathic Normal Pressure Hydrocephalus (Third Edition): Endorsed by the Japanese Society of Normal Pressure Hydrocephalus. Neurol Med Chir (Tokyo). 2021 Feb 15;61(2):63-97. doi: 10.2176/nmc.st.2020-0292. Epub 2021 Jan 15. PMID: 33455998; PMCID: PMC7905302.
- ↑ Zhou S, Dong L, He Y, Xiao H. Acupuncture plus herbal medicine for Alzheimer's disease: A Systematic review and meta-analysis. Am J Chin Med. 2017;45:1327–44.
- ↑ Yang JW, Shi GX, Zhang S, Tu JF, Wang LQ, Yan CQ, et al. Effectiveness of acupuncture for vascular cognitive impairment no dementia: A randomized controlled trial. Clin Rehabil. 2019;33:642–52.
- ↑ Isaacs AM, Williams MA, Hamilton MG. Current update on treatment strategies for idiopathic normal pressure hydrocephalus. Curr Treat Options Neurol. 2019;21:65.
- ↑ Modesto PC, Pinto FCG. Home physical exercise program: Analysis of the impact on the clinical evolution of patients with normal pressure hydrocephalus. Arq Neuropsiquiatr. 2019;77:860–70.
- ↑ McGovern Medical School. Normal Pressure Hydrocephalus. Available from: http://www.youtube.com/watch?v=po351hZeS7k [last accessed 15/09/2020]