Nocebo Effect
Original Editor - Melissa Coetsee
Top Contributors - Melissa Coetsee, Kim Jackson and Vidya Acharya
Introduction[edit | edit source]
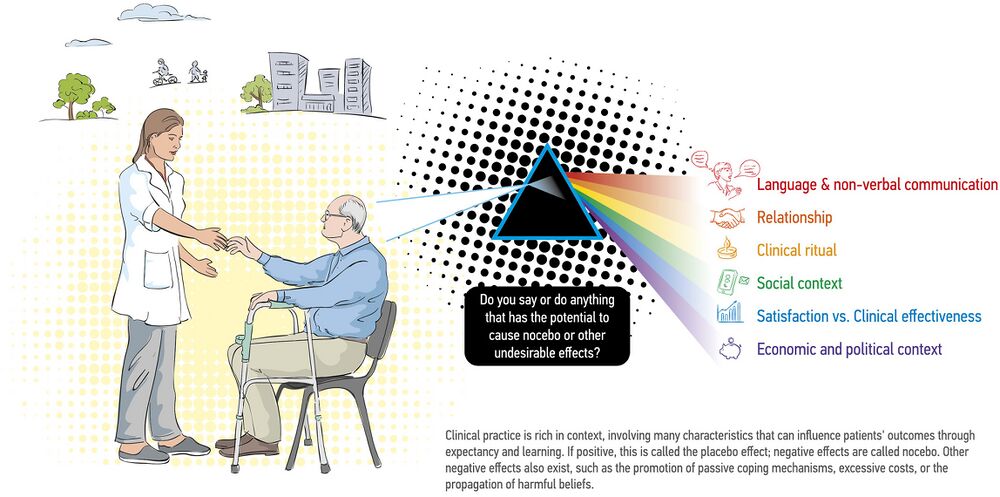
The nocebo effect, the opposite of the placebo effect, is the psychobiological phenomenon of adverse treatment effects that cannot be ascribed to specific treatment mechanism, but rather is shaped by expectations and learning.[1]In contrast to the placebo effect of positive expectation which results in health benefits, the nocebo effect worsens the health status due to negative beliefs and expectations. It refers to the adverse outcomes that occur as a result of patient expectations and subconscious learning [2].
Increasing research suggests that the clinicians' communication style could be a substantial source of nocebo effects, resulting in adverse symptoms that are much more significant than previously thought. [1]
Contributing Factors[edit | edit source]
The following factors can contribute to a nocebo effect[2]:
- The healthcare setting
- Patient-practitioner interaction (verbal and non-verbal communication)
- Patient-practitioner characteristics (reputation, previous negative experiences)
- Actions that convey meaning
- Words/language that have negative meaning attached to them
- Social media/pamphlets focusing on disease and biomedical models
Manifestation of Nocebo Effect[edit | edit source]
- Aggravation of pain, not related to disease/treatment factors
- Treatment 'side-effects'
- Learnt helplessness; loss of self-efficacy and self-esteem
- Fear avoidance
- Pain catastrophising
- Over-reliance on medical care
- Increased psychological and physical distress
- Increase in perceived and actual disability
Physiology[edit | edit source]
For a long time, the placebo and nocebo effects were largely explained by psychological mechanisms, but research has revealed that biological factors are involved. Some of the physiological mechanisms which are activated by negative expectancy include[2][3]:
- Activation of the pro-nociceptive system (cholecystokinin pathway)
- Activation of various cortical and spinal cord mechanisms - Increased anxiety which activates the hypothalamic-pituitary-adrenal axis
- Effect on neural pathways that mediate pain experience
For more on pain modulation follow the links to these pages: Pain facilitation and inhibition; Pain-modulation; Pain descending pathways
Evidence of the Nocebo Effect[edit | edit source]
A meta-analysis has demonstrated that the effect sizes related to verbally induced nocebo can be significant - negative verbal information can even convert non-nociceptive stimulation into an experience of pain.[2][4]
Below are some specific conditions/settings that have been researched:
- ICU: Negative 'warnings' prior to procedures (such as inserting lines) can result in hyperalgesia and distress. Family meetings also require a careful consideration of language used. [1]
- Performance: The nocebo effect can negatively influence muscle force production, endurance and response accuracy.[5]
- Postural Stability: Negative performance expectations (evoked by instructions) can negatively impact objective (increased postural sway) and subjective postural stability. [5]
- Low back pain (LBP): Routine imaging leads to worse outcomes compared to a clinical report (reassurance of incidental findings). Early MRI's for LBP results in longer duration of disability, higher medical cost and worse outcomes regardless of radiculopathy (after controlling for severity and demographics).[6]
- Hyperalgesia: Higher levels of fear of pain significantly increases stress levels and is associated with increased nocebo hyperalgesia.[6]
- Medical Imaging: The use of negative words to describe a non-threatening situation, for example, diagnostic descriptions of imaging reports - can be perceived by patients as implying an increased severity of their condition, which can lead to poor outcomes.[2]Healthcare advice that emphasises structural/anatomical vulnerability of the spine from radiographic imaging, resulted in patients having greater reported disability.[7] See also: Medical imaging
- A study found that when patients with low back pain are told that a leg flexion test could lead to pain, reported an increase in pain and performed fewer repetitions, than those who were told the test is painless[8].
- Various studies have reported that chronic back pain can in part be iatrogenic due to misconceptions and negative beliefs instilled by practitioners.[7]
Language Matters[edit | edit source]
Healthcare is infiltrated with meaning and words, from the jargon of medical terms to the waiting room, interview, relaying of information and clinical mannerisms - which can all influence outcomes.[3] Both the way we communicate and the words we use can be harmful.
Communication[edit | edit source]
Research has shown that good communication forms an integral part of efficient and quality health care. The way medical information is delivered (non-verbal and verbal factors) by clinicians can have a significant impact on patient outcomes.[9]Clinicians should mindful of tone, affect, facial expressions and word choice.[9]
For more detail, visit the following pages:
Words[edit | edit source]
Like medication, words can change the way a person thinks and feels:[9][10]
- Words have emotive power and can generate good or bad emotions
- Words can prompt actions that can lead to negative or positive behaviour change
- The meaning attached to words are influenced by one's background and culture - for example, the word degenerative discs may sound non-threatening to a clinician, but scary to a patient
- Words affect patients' response to medical interventions
"Words are, of course, the most powerful drug used by mankind" - Rudyard Kipling
Pathoanatomical language still dominates the health care sector, with less acknowledgement of the well researched psychological factors involved in pain and disability[10]. An improved understanding of pain as a phenomenon that is mediated by the mind may help to increase awareness of the meaning behind the words we choose.
Watch this video on the power of words:
Clinical Implications[edit | edit source]
It is important to be aware of the impact that words (when we educate, interview, assess) can have on patient expectations, and subsequently on health outcomes.
“Pain is an ideal habitat for worry to flourish”[11]; Without awareness of the potential harm that words can do, clinicians may continue to unknowingly fertilize pain's vulnerable ground.[10]
Clinicians who have short interactions with patients, need to carefully consider what to say and convey in the limited time, and those who have prolonged contact with patients (such as allied health practitioners) should continually focus on positive reframing and challenge negative beliefs.[3]
Reframing Words[edit | edit source]
There is no one formula for how we might use language within clinical practice. Not all medicalized language is harmful to all individuals. Below are some guiding principles that can help to minimise nocebo effects:[10]
- Positive framing: Rephrasing medical information and descriptions to focus on the positive elements, without being dishonest. Realistic but not fatalistic. This usually includes words of encouragement and positive words. Minimise the attention placed on negative aspects.
- Patient engagement: Involve the patient in the knowledge process to determine what they want to know and explore patient expectations and beliefs
- Positivity: Focus on factors that eliminate worry and fear and focus on language towards hopes, and not hurts, on what one can do rather than what can't be done
Here are some examples of word reframing[6][10]:
| Potentially harmful words | Reframed wording |
|---|---|
| Instability | Needs more strength and control |
| Chronic | It may persist, but you can overcome it |
| Bone out of place | Normal individual variation |
| Lumbar dysfunction/ disc bulge | Episode of back pain; lumbar sprain |
| If we do not work on your balance you will definitely fall again | Balance training can be highly effective in reducing the risk of falls |
| Tear | Pull; defect |
| Trapped nerve | Tight, but can be stretches/mobilised |
| Frozen/ locked | Tight; stiff |
| Wear and tear (may imply the need for a technical fix); Degenerative changes | Normal age changes; A lot of people without pain also have this |
You have to do X before "..."
|
If you do X, you can "..."
|
| Your joint is bone on bone | Narrowing/tightness |
| That is the worst joint I have ever seen | The good news is, we can help |
| No wonder you are in pain | This doesn't have to be a life sentence to pain |
| You are going to have to live with this | You may need to make some adjustments |
| Bulge/herniation | Bump, swelling |
| This is going to "sting/burn" | I am about to inject an anaesthetic that numbs the skin |
| You will probably need a joint replacement in 10 years | There is a lot we can do make sure your joint remains as strong as possible for the future |
Role of the Multi-disciplinary Team[edit | edit source]
| Rehabilitation Professionals | Medical Doctors/ Specialists |
|---|---|
| Rehab professionals are well-placed to provide primary health care that reduces requests for imaging, and to mitigate the commonly-held belief that where there is pain there must be an injury. It is important to provide patient-focused communication and build supportive relationships.[2] | Doctors plan an important role in conveying image findings and information regarding treatment options and prognosis. Single and at times offhand statements can heavily influence recovery expectations. The inappropriate use of routine medical imaging can also be harmful, especially when the results are not conveyed in context and with sensitivity. |
Rehabilitation professionals need to be aware of the following actions and their possible negative effects on patient outcomes[2]:
- Using unhelpful diagnostic labels: Can promote fear of movement and catastrophising, and can create negative expectancy
- Failure to focus on positive aspects of structures in the human body: Can lead to false perceptions of vulnerability and lead to fear-avoidance
- Excessive attention to tissue modification induced through treatment: Reinforces dependence, discourages self-management and promotes beliefs in purely biological causes of pain
- Over-emphasis on teaching 'proper' postures: Triggers fear and limits contextual adaptation
- Overuse of low-value-based therapies (such as electrotherapy) instead of therapies with more robust evidence: Delayed recovery and dependence which could result in lack of self-efficacy and negative expectations
- Advocating maintenance therapy: including any suggestions or practices that could promote the belief that deterioration is inevitable without continuous intervention/'maintenance' therapy
Ethical Considerations[edit | edit source]
- Informed Consent: Evidence has shown that information disclosure about potential side effects of treatment, may create expectancies which contribute to adverse effects and may hinder the positive effects of the treatment.[5]The very process of describing potential adverse events can therefore lead to nocebo responses (i.e. harm).[1] It is therefore necessary to reframe the risks of interventions in a wat that reassures (eg. "as X can occur, we always do Y to make sure it is as safe as possible"). The risk of harm through a nocebo effect needs to be balanced with the obligation of full disclosure.
- First do no harm: This ethical principle emphasises why it is important for all clinicians to be aware of the possible harm that can be done through their words. If a patient's expectation/request could cause harm (eg. an early MRI that is not indicated or insisting on only passive treatment modalities), it is necessary to reshape the patient's beliefs to be consistent with best practice.[3]
- Truth-telling: It is not ethical to use positive words, which are in fact false (eg. telling a patient they will definitely recover fully, when this is not the case). One can however leverage the positive effects of words and combine evidence based interventions with a positive therapeutic experience.[3]At the same time, the effect of evidence-based interventions are at risk of being minimised when combined with a negative therapeutic experience. It is important to balance communicating important clinical information and ensuring that every attempt is made to minimize negative expectancies.[4]
Summary[edit | edit source]
As with the placebo effect, the nocebo response highlights the powerful interaction between the therapeutic context and the patient's mind-brain interaction.[4]All healthcare professionals need to be aware of the potential harm that can be done through verbal and non-verbal communication and should seek to improve their communication skills through word reframing, patient-centred care and a supportive therapeutic relationship.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Huynh KN, Rouse-Watson S, Chu J, Lane AS, Cyna AM. Unheard and unseen: The hidden impact of nocebo communication in the Intensive Care Unit. Journal of the Intensive Care Society. 2023 Nov 29:17511437231214148.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Hohenschurz-Schmidt D, Thomson OP, Rossettini G, Miciak M, Newell D, Roberts L, Vase L, Draper-Rodi J. Avoiding nocebo and other undesirable effects in chiropractic, osteopathy and physiotherapy: An invitation to reflect. Musculoskeletal Science and Practice. 2022 Oct 21:102677.
- ↑ 3.0 3.1 3.2 3.3 3.4 Benz LN, Flynn TW. Placebo, nocebo, and expectations: leveraging positive outcomes. journal of orthopaedic & sports physical therapy. 2013 Jul;43(7):439-41.
- ↑ 4.0 4.1 4.2 Colloca L, Finniss D. Nocebo effects, patient-clinician communication, and therapeutic outcomes. Jama. 2012 Feb 8;307(6):567-8.
- ↑ 5.0 5.1 5.2 Russell K, Duncan M, Price M, Mosewich A, Ellmers T, Hill M. A comparison of placebo and nocebo effects on objective and subjective postural stability: a double-edged sword?. Frontiers in Human Neuroscience. 2022 Aug 18;16:967722.
- ↑ 6.0 6.1 6.2 Dorow B. Words that Hurt, Words that Heal. [PowerPoint presentation]. Kaiser Permanente Persistent Pain Fellowship.
- ↑ 7.0 7.1 Lin IB, O'Sullivan PB, Coffin JA, Mak DB, Toussaint S, Straker LM. Disabling chronic low back pain as an iatrogenic disorder: a qualitative study in Aboriginal Australians. BMJ open. 2013;3(4).
- ↑ Pfingsten M, Leibing E, Harter W, Kröner-Herwig B, Hempel D, Kronshage U, Hildebrandt J. Fear-avoidance behavior and anticipation of pain in patients with chronic low back pain: a randomized controlled study. Pain medicine. 2001 Dec 1;2(4):259-66.
- ↑ 9.0 9.1 9.2 Vranceanu AM, Elbon M, Ring D. The emotive impact of orthopedic words. Journal of Hand Therapy. 2011 Apr 1;24(2):112-7.
- ↑ 10.0 10.1 10.2 10.3 10.4 Stewart M, Loftus S. Sticks and stones: the impact of language in musculoskeletal rehabilitation. journal of orthopaedic & sports physical therapy. 2018 Jul;48(7):519-22.
- ↑ Eccleston C, Crombez G. Worry and chronic pain: a misdirected problem solving model. Pain. 2007 Dec 5;132(3):233-6.







