Imperforate Anus
Introduction[edit | edit source]
Imperforate anus is a congenital malformation within the anus, in which the anal opening doesn't exist. This anorectal malformation (ARM) includes a spectrum of defects within the anus and rectum during the development of the fetus. And varies in its severity from minor ones, which look like a thin membrane covering the anal opening, to more complex conditions that also involve abnormalities in the urinary and genital tracts (cloacal malformations). This defect may be associated with malformation of pelvic floor muscles[1]. Infants with ARM may also have anomalies with other organ systems, these anomalies were found in about half of the patients[2] such as:[3]
- Vertebral defects – reduced bone volume or absence of one-half of a vertebral structure.
- Anal defects – blocked anus/ absence of the opening
- Cardiac defects – abnormalities in ventricular septa, atrial septa, or tetralogy of Fallot
- Tracheoesophageal - inability to separate the esophagus and windpipe
- Renal defects — lack of a full renal system or partial renal system (this could be either unilateral or bilateral), other urinary-genital system irregularities
- Limbs defects – no digits, displaced digits, many digits, or fused digits.
These defects presentations are named as VACTERL Syndrome and can be diagnosed by the presence of 3 or more of these defects.
Mechanism of Injury / Pathological Process[edit | edit source]
In 1.4% of instances, ARM may be associated with hereditary genetic factors, an increased risk within the family when some members were previously affected by the same disease[4].
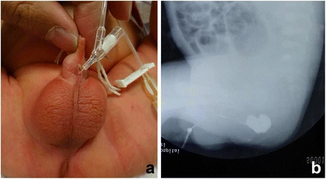
Types of imperforate anus[edit | edit source]
Low type, in which the anal opening exists but it may be curved by a membrane or is in an abnormal position and the rectum terminates beneath the muscles located at the base of the pelvis.
Intermediate type, child with this type may have fistulas, and the ends of the rectum and anal canal extend through the muscles of the pelvic floor
High Type, there is no anal opening exist and the end of the rectum and anal canal ends above the muscles of the pelvic floor and they also may have a fistula.
Diagnostic Procedures[edit | edit source]
Radiologic evaluations for newborns with the imperforate anus are different[5]:
- Abdominal ultrasound to check Urologic anomalies,
- A spinal ultrasound done within 3 months from birth to look for a tethered spinal cord (spinal cord is attached abnormally within the lower spine among other spinal anomalies.
- Plain X-rays of the spine can show spinal anomalies such as spina bifida also, X-rays of the sacrum reveal sacral irregularities and aid in determining the degree of sacral underdevelopment.
- In cases of colostomy, colonography can be used after to identify the site of the lower rectum and any communication between the urinary tract and bowel to help in planning the final surgical correction.
Management / Interventions[edit | edit source]
Surgical interventions[edit | edit source]
The surgical intervention depends on the type of the imperforate anus, in high type it will need surgical intervention over a period of time. The baby may need to undergo colostomy for a temporary period of time and later on a surgical anal reconstruction will be carried in addition to correction to any defect exits like fistula[6].
For low and Moderate type surgical removal of the membrane, repeated stretching of the anal opening can be done through endoscopy in a procedure named perineal anoplasty this may need to be followed by an enema daily after surgery to avoid constipation and is combined with dilatation[7].
Physical therapy rehabilitation[edit | edit source]
Physical therapy and pelvic rehabilitation are important procedures to restore muscle strength and postoperative fecal incontinence after surgery. You may have long-term fecal incontinence (FI) problems. If left untreated, it can easily persist into adulthood.
Transcutaneous functional electrical nerve stimulation TFES with a frequency of 40 Hz, duration of 250 μs, hold and rest time of 3 s with adjustable amplitude (range 0–100 mA) was generated. It was used to enhance the power and/or stamina of striated muscle contractions and will help them to be aware of pelvic floor muscles and identify the feelings when these muscles and the sphincter tighten[9].
Biofeedback Therapy is another intervention to help retrain the child postoperative, pelvic floor muscle training, in addition to, bowel training[10].
Dealing with constipation is important with those patients and a healthy balanced diet is important and may be till the age of school. You can find more about physical therapy intervention for constipation on the following pages, Functional constipation, Detrusor Sphincter Dyssynergia
Differential Diagnosis[edit | edit source]
Most infants with anorectal malformation are discovered and treated early nowadays. However, in the past. it was sometimes misdiagnosed especially in mild cases so it is important to examine and check for anal opening, its position to external anal, and the presence of the fistula or not[11].
References[edit | edit source]
- ↑ Watanabe Y, Ando H, Seo T, Kaneko K, Katsuno S, Shinohara T, Mori K, Toriwaki J. Three-dimensional image reconstruction of an anorectal malformation with multidetector-row helical computed tomography technology. Pediatric surgery is international. 2003 May;19:167-71.
- ↑ Cho S, Moore SP, Fangman T. One hundred three consecutive patients with anorectal malformations and their associated anomalies. Archives of pediatrics & adolescent medicine. 2001 May 1;155(5):587-91.
- ↑ Solomon BD. Vacterl/vater association. Orphanet journal of rare diseases. 2011 Dec;6:1-2.
- ↑ Falcone Jr RA, Levitt MA, Peña A, Bates M. Increased heritability of certain types of anorectal malformations. Journal of pediatric surgery. 2007 Jan 1;42(1):124-8.
- ↑ Levitt MA, Peña A. Anorectal malformations. Orphanet journal of rare diseases. 2007 Jul 26;2(1):33.
- ↑ Wood RJ, Levitt MA. Anorectal malformations. Clinics in colon and rectal surgery. 2018 Mar;31(02):061-70.
- ↑ Ueno S. Imperforate Anus: Low Type. Operative General Surgery in Neonates and Infants. 2016:247-53.
- ↑ Children's Hospital Colorado. Anorectal Malformation Surgery. Available from: http://www.youtube.com/watch?v=RpLNaARmO5U[last accessed 5/4/2024]
- ↑ Sharifi‐Rad L, Ladi‐Seyedian SS, Ashjaei B. Management of post‐surgical fecal incontinence due to anorectal malformations by pelvic floor rehabilitation. Journal of Paediatrics and Child Health. 2022 Aug;58(8):1379-83
- ↑ Scott KM. Pelvic floor rehabilitation in the treatment of fecal incontinence. Clinics in colon and rectal surgery. 2014 Sep;27(03):99-105.
- ↑ Amerstorfer EE, Schmiedeke E, Samuk I, Sloots CE, van Rooij IA, Jenetzky E, Midrio P, ARM-Net Consortium. Clinical differentiation between a normal anus, anterior anus, congenital anal stenosis, and perineal fistula: definitions and consequences—the ARM-Net Consortium Consensus. Children. 2022 Jun 3;9(6):831.