Derby Shoulder Instability Programme
Introduction[edit | edit source]
The Derby Instability Programme is a rehabilitation protocol designed to provide a structured progression for the management of shoulder instability. It is structured and reproducible with target-led milestones for progression. It incorporates strength, proprioception, plyometric training and kinetic control [1]. The programme aims to improve pain, stability and function at the shoulder[2]. It was designed by the by Derby Shoulder Unit’s specialist shoulder physiotherapist Marcus Bateman [3].
Relevance of the Programme[edit | edit source]
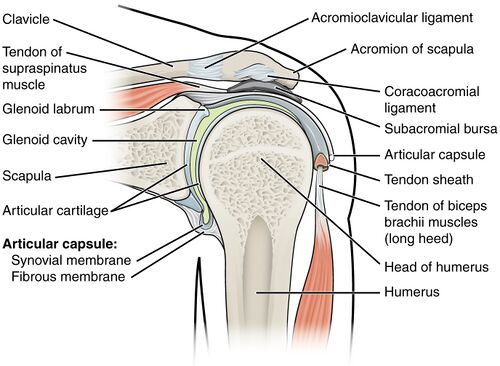
The shoulder is a complex joint which includes the glenohumeral joint. This is a shallow ball and socket joint which allows a large range of movement but is therefore inherently more vulnerable to subluxation and dislocation[4]. Shoulder dislocations can be divided into traumatic and atraumatic with most being an anterior dislocation. A common complication is recurrent dislocation, suggestive of instability[5].
Traumatic shoulder instability is where a traumatic event causes a dislocation of the shoulder which results in instability from a structural defect[6].
Atraumatic shoulder instability is where shoulder subluxations and dislocations occur without prior injury. This can be a result of underlying laxity with associated loss of muscular control or repetitive micro-trauma[6].
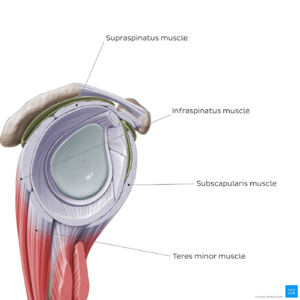
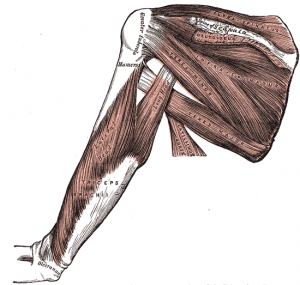
Shoulder instability can present with pain, loss of function, altered movement patterns, sensorimotor deficit and central sensitisation. As such, rehabilitation of the rotator cuff and periscapular muscles are recommended with proprioception, functional and sport-specific training also recommended[7][5].
Programme Outline[1][edit | edit source]
The programme is split into 2 sections. One exercise from each section is provided to the patient, starting at the top of the list. When the patient can achieve the target, they progress to the next exercise in the section.
Section 1: works on speed of muscle activation, plyometrics and deceleration of fast movement.
Section 2: works on proprioception, muscle balance and trunk stability.
The Exercises[1][edit | edit source]
Section 1[edit | edit source]
Prescribe maximum repetitions until fatigue or the specified target. Two sessions per day.
Drop & catch 1kg weight at 90° scaption Target 100 reps
Drop & catch 1kg weight at 90° scaption on 1 leg (opposite side) Target 100 reps
Drop & catch 1kg weight at 90° scaption with eyes closed Target 100 reps
Drop & catch 1kg weight in AER/AIR Target 100 reps
Falling press up in standing Target 50 reps
Falling press up to waist level Target 50 reps
Plyometric push up with hand clap Target 20 reps
Doorway fall Target 20 reps
Section 2[edit | edit source]
Prescribe 5 repetitions of the patient’s maximum ability or specified target time. Two sessions per day.
Single handed ball roll on wall Target 60s
Single handed kneeling crosses Target 60s
Kneeling single handed ball roll Target 60s
Single handed crosses in push up position Target 60s
Double handed ball roll in push up position Target 60s
Double ball roll in push up positions Target 60s
For patients with significant posterior instability modify the position for the single hand exercises to do with the shoulder in an abducted rather than flexed position.
Videos of the exercises can be found here.
Cautions and contraindications for use[1][edit | edit source]
· No true winging of the scapula
· No evidence of true neurological weakness
· Normal gym ball sitting balance
· Able to achieve 90’ scaption
Alternative Programmes[edit | edit source]
· Rockwood Instability Programme.[8] This programme focuses on strengthening the deltoid and the glenohumeral
rotators with the arm at low degrees of shoulder elevation.[8]
· Watson Multidirectional Instability Programme.[9] This programme focuses on re-establishing scapular control prior to any rotator cuff or deltoid strengthening.[8]
- ↑ 1.0 1.1 1.2 1.3 Bateman M, Smith BE, Osborne SE, Wilkes SR. Physiotherapy treatment for atraumatic recurrent shoulder instability: early results of a specific exercise protocol using pathology-specific outcome measures. Shoulder & Elbow. 2015; 7(4):282–288
- ↑ Bateman M, Osborne S, Smith BE. Management of atraumatic shoulder instability - updated results of the Derby Shoulder Instability Rehabilitation Programme. Physiotherapy. 2019; 105:e69
- ↑ Derby Shoulder Unit. Results of Derby Instability Rehab Programme published [Internet]. 2015 [cited 2023 July 06]. Available from: https://derbyshoulderunit.co.uk/results-of-derby-instability-rehab-programme-published/
- ↑ Dumont GD, Russell RD, Robertson WJ. Anterior shoulder instability: a review of pathoanatomy, diagnosis and treatment. Curr Rev Musculoskelet Med. 2011; 4:200–207
- ↑ 5.0 5.1 Hayes K, Callanan M, Walton J, Paxinos A, Murrell GAC. Shoulder Instability: Management and Rehabilitation. J Orthop Sports Phys Ther. 2002; 32:497–509.
- ↑ 6.0 6.1 Noorani A, Goldring M, Jaggi A, Gibson J, Rees J, Bateman M, Falworth M, Brownson P. BESS/BOA patient care pathways: Atraumatic shoulder instability. Shoulder & Elbow. 2019; 11(1):60–70
- ↑ Coulthard C, Cairns MC, Williams D, Hughes B, Jaggi A. Management of atraumatic shoulder instability in physiotherapy (MASIP): a survey of physiotherapy practice. BMC Musculoskelet. Disord. 2021; 22:840
- ↑ 8.0 8.1 8.2 Warby SA, Ford JJ, Hahne AJ, Watson L, Balster S, Lenssen R, Pizzari T. Comparison of 2 Exercise RehabilitatioN Programs for Multidirectional Instability of the Glenohumeral Joint. Am J Sports Med. 2018; 46(1):87–97
- ↑ Watson L, Warby S, Balster S, Lenssen R, Pizzari T. The treatment of multidirectional instability of the shoulder with a rehabilitation programme: Part 2. Shoulder & Elbow. 2017; 9(1):46–53