Trigeminal Neuralgia
Original Editor - Wendy Walker
Top Contributors - Kirenga Bamurange Liliane, Wendy Walker, Abbey Wright, Admin, Kim Jackson, Scott Buxton, Evan Thomas, Joao Costa, Claire Knott, Laura Ritchie, Naomi O'Reilly, Vanessa Rhule, WikiSysop and Uchechukwu Chukwuemeka
Introduction[edit | edit source]
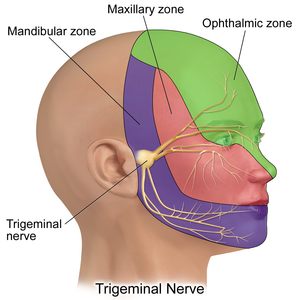
Trigeminal Neuralgia (TN) is a facial pain syndrome. It is typically characterised by short term, unilateral facial pain following the sensory distribution of cranial nerve V, the Trigeminal Nerve. Most commonly the pain radiates to the mandibular or maxillary regions. In some cases, it is accompanied by a brief facial spasm or tic.[1] Trigeminal neuralgia also called tic douloureux; transports sensation from the face to the brain.[2] It's an intermittent pain of high intensity that is raised by light touch.[3]
The Trigeminal nerve, the fifth cranial nerve, is the nerve responsible for sensation in the face, and control of motor functions such as biting and chewing.
"Trigeminal" = tri, and "-geminus" or twin, or thrice twinned derives from the fact that it has three major branches:
- Ophthalmic nerve (V1) 1st branch - sensory
- Maxillary nerve (V2) 2nd branch - sensory
- Mandibular nerve (V3) 3rd branch - sensory and motor. Controlling the muscles of mastication: Temporalis and Masseter.
Aetiology/ Pathological Process[edit | edit source]
The exact aetiology of TN has not been clearly explained.[4] The compression of the trigeminal nerve root, either at the dorsal root entry or by a blood vessel is one of the biggest causes or contributing factors.[5] Symptoms of pain are usually caused by compression of the Trigeminal nerve route in 80-90% of cases.[1] Which is located within the Central Nervous System.
Causes[edit | edit source]
Trigeminal Neuralgia is first of all due to the demyelinating disorder.[6][7] Common causes of compression can be tumours or their associated blood vessels however in many cases the cause can be unknown.[1]
Other causes may include:
- Multiple Sclerosis (MS): approximately 1-2% of patients with MS develop TN.[8][9]
- A tumor
- Physical damage to the nerve
- Family history of blood vessel formation[10]
- craniovertebral junction abnormalities such as Chiari Malformations
- bony disorders like Paget's disease
- osteogenesis imperfecta[11]
Symptoms[edit | edit source]
The pain in TN is usually localized in one side of the face and is felt in conntact of a light touch or a sound. It's usually triggered by the following activities:[12]
- brushing teeth
- shaving
- rubbing
- touching the painful area of the face
- putting on makeup
- eating or drinking
- speaking
- being exposed to the wind
- pain in the cheek, jaw, teeth, gums, and lips
- pain in one side of the face
- tingling or numbness in the face before starting to feel pain[10]
Studies suggest that trigger zones, or areas of increased sensitivity, are present in one half of patients and often lie near the nose or mouth
Epidemiology[edit | edit source]
Recent estimates suggest the prevalence is approximately 4.5 cases per 100,000 population, with an incidence of approximately 15,000 cases per year.[13]
The worldwide prevalence ranges between 10 and 300/100 000. [4] In 90% of patients, the disease begins after age 40 years, generally between 60-70 years. Women are more affected than men.[14]
Clinical Presentation[edit | edit source]
TN presents as a sharp, stabbing unilateral facial pain that is normally episodic in nature. [15]
Area of pain[edit | edit source]
60% of patients with TN present with lancinating pain shooting from the corner of the mouth to the angle of the jaw
30% experience jolts of pain from the upper lip or canine teeth to the eye and eyebrow, sparing the orbit itself—this distribution falls between the division of the first and second portions of the nerve.
According to Patten[16], fewer than 5% of patients experience ophthalmic branch involvement. <figcaption></figcaption>
Characteristic Descriptors of pain[edit | edit source]
The pain quality is severe, paroxysmal, and lancinating.
It usually starts with a sensation of electrical shocks, then quickly increases in less than 20 seconds to an excruciating pain felt deep in the face, often contorting the patient's expression. The pain then begins to fade within seconds, only to give way to a burning ache lasting seconds to minutes. During attacks, patients may grimace, wince, or make an aversive head movement, as if trying to escape the pain, thus producing an obvious movement, or tic; hence the term "tic douloureux."
Frequency of pain[edit | edit source]
The number of attacks may vary from less than 1 per day, to hundreds per day.
Outbursts fully abate between attacks, even when they are severe and frequent.
Diagnosis and Classification[edit | edit source]
The International Headache Society (IHS) have published strict criteria[17] for TN:
A - Paroxysmal attacks of pain lasting from a fraction of a second to 2 minutes, affecting 1 or more divisions of the trigeminal nerve and fulfilling criteria B and C
B - Pain has at least 1 of the following characteristics: (1) intense, sharp, superficial or stabbing; or (2) precipitated from trigger areas or by trigger factors
C - Attacks stereotyped in the individual patient
D - No clinically evident neurologic deficit
E - Not attributed to another disorder
No laboratory, electrophysiologic, or radiologic testing is routinely indicated for the diagnosis of trigeminal neuralgia (TN), as patients with characteristic history and normal neurologic examination may be treated without further investigation.
The diagnosis of TN is almost entirely based on the patient's history and in most cases no specific laboratory tests are needed.
MRI scanning is often indicated simply to exclude other causes of the pain, such as pressure on the trigeminal nerve from Acoustic Neuroma.
Outcome Measures[edit | edit source]
- Visual Analog Scale (VAS)
- McGill Pain Questionnaire (MPQ)
- Brief Pain Inventory (BPI)
- Brief Pain Inventory - Facial (BPI-F)
Management / Interventions[edit | edit source]
Medical Management[edit | edit source]
A range of anti-epileptic drugs have proved to be useful in the management of TN, with carbamazepine in particular having a large number of studies demonstrating efficacy[18]. Non anti-epileptic drugs can also be prescribed, often in conjunction with carbamazepine[19].[20]
Other medications include muscle relaxants and tricyclic antidepressants.[12]
Surgical Management[edit | edit source]
Studies suggest that approximately 25% of TN patients go on to require surgery as their condition worsens over years, and the drug management becomes less effective[21]. Microvascular decompression and radiofrequency thermorhizotomy are the most common surgical procedures employed in these cases.
The other common surgical procedures include:
- Stereotactic Radiosurgery
- Gamma-knife Radiosurgery
- Glycerol injections
- Radiofrequency Thermal Lesioning[12]
Differential Diagnosis[edit | edit source]
The main differential diagnoses for TN are:
- Atypical facial pain - this common facial pain is less intense than TN, described as a dull or throbbing ache which lasts for minutes to hours
TN should also be differentiated from other causes oforofacial pain and heacheds such as:[4]
- Headahe disorders such as Migraine and Cluster headaches
- Dental pain
- Temporo-mandibular Joint disorders
- Other neuralgias
- Tumor
- Sinusitis
- Postherpetic neuralgia
Risks Factors[edit | edit source]
Important risk factors for TN havebeen identified as the following:
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Zakrzewska JM, Linskey ME. Trigeminal neuralgia. Bmj. 2014 Feb 17;348:g474
- ↑ What is Trigeminal Neuralgia? Available from:https://fpa-support.org/learn/ (accessed 29 September, 2020)
- ↑ Zakrzewska JM, Linskey ME. Trigeminal neuralgia. Bmj. 2014 Feb 17;348:g474
- ↑ 4.0 4.1 4.2 Vasappa CK, Kapur S, Krovvidi H. Trigeminal neuralgia. Bja Education. 2016 Oct 1;16(10):353-6.
- ↑ Zhang J, Yang M, Zhou M, He L, Chen N, Zakrzewska JM. Non‐antiepileptic drugs for trigeminal neuralgia. Cochrane Database of Systematic Reviews. 2013(12).
- ↑ Burchiel KJ. Abnormal impulse generation in focally demyelinated trigeminal roots. Journal of neurosurgery. 1980;53(5):674-83.
- ↑ Love S, Coakham HB. Trigeminal neuralgia: pathology and pathogenesis. Brain. 2001 Dec 1;124(12):2347-60.
- ↑ Rushton JG, Olafson RA. Trigeminal neuralgia associated with multiple sclerosis: report of 35 cases. Archives of neurology. 1965;13(4):383-6.
- ↑ Jensen TS, Rasmussen P, Reske‐Nielsen E. Association of trigeminal neuralgia with multiple sclerosis: clinical and pathological features. Acta Neurologica Scandinavica. 1982;65(3):182-9.
- ↑ 10.0 10.1 What to know about Trigeminal neuralgia? Available from: https://www.medicalnewstoday.com/articles/160252#causes ( Accessed 30 September 2020)
- ↑ Duransoy YK, Mete M, Akçay E, Selçuki M. Differences in individual susceptibility affect the development of trigeminal neuralgia. Neural regeneration research. 2013 May 15;8(14):1337
- ↑ 12.0 12.1 12.2 Trigeminal Neuralgia. Available from: https://www.healthline.com/health/trigeminal-neuralgia#symptoms (Accessed 29 September 2020)
- ↑ Katusic S, Williams DB, Beard M, Bergstralh EJ, Kurland LT. Epidemiology and clinical features of idiopathic trigeminal neuralgia and glossopharyngeal neuralgia: similarities and differences, Rochester, Minnesota, 1945-1984. Neuroepidemiology. 1991;10(5-6):276-81.
- ↑ Manzoni GC, Torelli P. Epidemiology of typical and atypical craniofacial neuralgias. Neurological Sciences. 2005 May 1;26(2):s65-7.
- ↑ Eller JL, Raslan AM, Burchiel KJ. Trigeminal neuralgia: definition and classification. Neurosurgical focus. 2005 May 1;18(5):1-3.
- ↑ Patten J. Trigeminal neuralgia. In: Neurological Differential Diagnosis. 2nd ed. London: Springer;1996:373-5.
- ↑ The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24 Suppl 1:9-160
- ↑ Rockliff BW, Davis EH. Controlled sequential trials of carbamazepine in trigeminal neuralgia. Arch Neurol.1966;15(2):129-36
- ↑ He L, Wu B, Zhou M. Non-antiepileptic drugs for trigeminal neuralgia. Cochrane Database Syst Rev. 2006;3:CD004029
- ↑ Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K, et al. AAN‐EFNS guidelines on trigeminal neuralgia management. European journal of neurology. 2008;15(10):1013-28.
- ↑ Dalessio DJ. Trigeminal neuralgia. A practical approach to treatment. Drugs.1982;24(3):248-55