Total Ankle Arthroplasty
Original Editor - Sharon Schumacher, Carlos De Coster
Top Contributors - Jeremy Brady, Jorge Solorzano, Admin, Scott Buxton, Kim Jackson, Dana Williams, Shaimaa Eldib, Carlos De Coster, Neha Palsule, 127.0.0.1, Mariam Hashem, Tony Lowe, Simisola Ajeyalemi, Uchechukwu Chukwuemeka, Rachael Lowe, Rucha Gadgil, Sharon Schumacher, Lucinda hampton, Jess Bell, Michael Kauffmann, George Prudden and Ryan De Laet
Search Strategy[edit | edit source]
PubMed (http://www.ncbi.nlm.nih.gov/pubmed)
MeSH terms:
- Complications
- Diagnosis
- Drug therapy
- Epidemiology
- Etiology
- Pathology
- Rehabilitation
- Surgery
- Therapy
Medline Plus
Used keyword:
- Ankle replacement
Definition/Description[edit | edit source]
Ankle replacement surgery has been available for over two decades however it is a far less common procedure than hip or knee arthroplasty owing to the less frequent incidence of osteoarthritis ankle pathology. The majority of ankle osteoarthritis is secondary to trauma.[1]
Until relatively recently, ankle joint arthrodesis (fusion) was the gold standard of treatment, but this was not without its complications, e.g. non-union,Osteoarthritis in the other mid/hind foot joints and stiffness and loss of proprioception[2]
Total ankle replacement was developed in the 1970's but initially was plagued with high long term failure rates. The older prosthesis loosened or malfunctioned and frequently needed to be removed[3]. In the late 70's Dr. Frank G. Alvine an orthopedic surgeon from Sioux Falls, SD developed the Agility Ankle which was the first FDA approved total ankle implant in use in the United States[4]. Since its introduction the Agility Ankle System has gone through several modifications. Currently the Agility Ankle System is the most widely used ankle prosthesis. With more than 20 years of experience it has the longest followup of any fixed bearing device[5].
On May 29, 2009 the medical news today announced the FDA approved the first mobile bearing device called the Scandinavian Total Ankle Replacement System (STAR). As a condition of FDA approval the company (Small Bone Innovations Inc.) must evaluate the safety and effectiveness of the device during the next eight years[6].
In a systematic review of the literature published in the Journal of Bone and Joint Surgery in 2007, the intermediate outcome of total ankle arthroplasty appears to be similiar to that of ankle arthrodesis however data was sparse[7]. In a study comparing reoperation rates following ankle arthrodesis and total ankle arthroplasty SooHoo, Zingmond and Ko confirmed that ankle replacement is associated with a higher risk of complications as compared with ankle fusion, but also has potential advantages in terms of a decreased risk of the patient requiring subtalar joint fusion[8]. In a seven to sixteen year follow up on the Agility Total Ankle Arthroplasty, Knecht, Estin, Callagham et al concluded that the relatively low rates of radiographic hindfoot arthritis and revision procedures at an average of nine years after the arthroplasty are encouraging[9].
Although interest in total ankle replacements is increasing, midterm clinical results to date are few and often have not been validated by independent pratitioners. In addition no level I or II studies have been published[10].
Clinically Relevant Anatomy[edit | edit source]
For detailed anatomy see here
Talocrural Joint[edit | edit source]
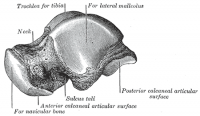
The ankle joint is a synovial hinge joint comprised of hyaline covered articular surfaces of the talus, the tibia as well as the fibula, allowing up to 20 degrees dorsiflexion and 50 degress plantarflexion. The distal ends of the tibia and fibula are held together firmly by ligaments of the medial (Deltoid) and lateral ligament complexes of the ankle which can be damaged and contribute to ankle arthritis (Ankle Sprain). The ligaments hold the tibia and fibula into a deep bracket-like shape in which the talus sits[11].
- TheROOF of the joint is the distal inferior surface of the tibia
- The MEDIAL SIDE of the joint is formed of the medial malleolus of the tibia
- The LATERAL SIDE of the joint is formed of the lateral malleolus of the fibula
The articular part of the talus looks like a cylinder and fits snugly into the bracket provided by the syndemosis of the tibia and fibula, when looking down upon the talus the articular surface is wider anteriorly than posteriorly. Subsequently this increases the congruent, stable nature of this joint when it is in dorsiflexion. As this is a synovial joint, a membrane is present as well as a fibrous membrane providing the same functions as any other synovial jointSynovial Membrane[11].
The Arthroplasty[edit | edit source]
Indication for Procedure
[edit | edit source]
There is no well-defined indication for a Total Ankle Arthroplasty. Surgery is considered only when conservative treatment has been attempted with no improvement. The operation is mainly being executed in patients who suffer from different types of arthrides. This cause advanced arthritic changes of disabling pain and loss of ankle motion. The ankle is most frequently affected by post-traumatic arthritis.[12] Total ankle joint replacement is also indicated following unsuccessful ankle arthrodesis [13] the ‘ideal’ patient for ankle joint replacement is an elderly person with the low physical demands who has good bone stock, normal vascular status, no immune-suppression, and excellent hind foot-ankle alignment.[14]
Pre-operative Procedure and Definitive Diagnosis[edit | edit source]
Weight bearing A-P and lateral mortise views of bilateral ankles is required to make effective preparation and anticipation of that will be required in the surgery. The rearfoot alignment (Cobey/Saltzman) view is essential to evaluate the ankle joint and identify any calcaneal-totibial deformities. This is performed by getting the patient to stand, elevated with a cassette positioned at 15 degres anteriorly inclined with the x-ray bemed perpendicular to the film. This position is altered if deformities are present, after this has been taken anterior distal tibial angle (ADTA) is measured. The ADTA is formed by the mechanical axis of the tibia and the joint orientation line of the ankle in the sagittal plane and measures 80° ± 3° in the normal lower extremity. In the coronal plane, the lateral distal tibial angle (LDTA), the tibial-talar angle and the calcaneal tibial alignment should be measured. The LDTA is formed by the distal tibial articular surface and the anatomical axis of the tibia and measures 89° ± 3°.29, if this is decreased this represents a varus deformity. The tibial-talar angle (Figure 3C) is defined by the tibial and talar articular surfaces in the ankle joint. When the tibialtalar angle is >10° the joint is defined as incongruent (unstable)[15].
"If an abnormal ADTA or LDTA is present (sagittal or coronal deformity), the center of rotation of angulation (CORA) is measured. The CORA is the intersection of the mid-diaphyseal line and the line starting from the middle of the joint and perpendicular to the abnormal ADTA or LDTA (Figure 4). The CORA can be located at the joint line level (usually due to anatomical joint line malalignment or to ankle degeneration) or proximally (usually due to tibial deformities/fractures)"[15]. So as you can see there are many consideration to be taken, and multiple angles to be analysed and this is important and any instability and malalignment of the new prosthesis can be excessively worn or may even fail[15].
Surgical Procedure[edit | edit source]
To perfrom the procedure the patient is positined supine with the hip slightly elevated and a tourniquet on the proxinal thight to restrict blood flow during the procedure. Next a 10 cm incision is made over the centre of the joint line to expose the relevent anatomical structures. Once the structures have been exposed the crucial nerves and tendons are identified as to protect and ensure their intergrity to minimise operative complications, these include; peroneal nerves, tibialis anterior and extensor hallucis longus. This is also to achieve correct talocrural alignment and soft tissue balance to ensure the prosthesis can achieve plantar grade in standing. It is also important to debride and correct any osteophytes or any other structures that can contribute to malalignment. Depending on the natural angle of the talocrural joint (varus or valgus) more bone medially or laterally may have ot be removed, this also may occur if the joint is deep or shallow as it may need to be reduced or elevated[15].
Once the joints have been corrected and bones properly aligned the new components are trialled making sure rull ROM and stability is achieved. If dorsiflexion is limited and not due to malalignment then achilled tendon lengthening is required, the same goes for if there is instability in inversion or eversion the ligaments are reconstructed. Persistent malalignment can occure and may need seperate procedures to correct such as subtalar fusion depending on severity and correctability[15].
Physical Therapy Management
[edit | edit source]
As it will be explained in the pre-operation and post-operation phaes the multi-disciplinary team in volved with the patient have a big role in making the arrangements before and after the surgery, this may involve physiotherapists, occupational therapists, discharge nurses, staff nurses, healthcare assistants as well as doctors. Both pre and post operative phases are integral to the progress of the patient and the pre-op should not be overlooked as important as it can be easy to focus on post-op.
Pre-Operative Phase[edit | edit source]
Before the surgery one of the main job for the team is to educate the patient about what will happen before, during and after the surgery as this will give the patient the opportunity to prepare, mentally rehearse, ensure smooth transition through short-term to long-term goals but also help control and reduce post-operative pain[16]
ROM, muscle strength, gait and deviations will all be recorded as to compared before and after arthroplasty and ensure the patinet is as optimal strength prior to operation if possible. For safety and ease of transition is can be important that the patient learns how to walk with crutches so they can perform ADL’s as soon as possible post arthroplasty but also understand that they will be non-weight bearing after the arthroplasty[17].
As will all procedures under general anaesthetic there are common pulmonary postoperative complications (PPC's) which need to be controlled and risk reduced and htis can be explained at this stage as well.
Post-Operative Phase[edit | edit source]
It is important to ensure the risk of PPC's are reduced and respiratory physiotherapy may be used at this early stage, cough, deep breathing exercises and early mobility are essential here to reduce atelectasis and reinstate the muscocilliary elevatory as soon as possible.
IT IS IMPORTANT TO KNOW YOUR OWN HOSPITALS/SURGEONS GUILDLINES FOLLOWING ARTHROPLASTY OR ANY OPERATION AND THE FOLLOWING SHOULD ONLY BE USED TO EDUCATE AND CONSIDER SOME BASIC/COMMON PROTOCOLS
THIS SHOULD NOT BE USED IN REPLACEMENT OF THE SURGEONS PROTOCOL
THIS IS A PROTOCOL BY THE ROYAL NATIONAL ORTHOPAEDIC HOSPITAL NHS TRUST[18]
Initial Rehab 0-4 Weeks[edit | edit source]
Restrictions:
- Non-weight bearing 2/52 with a back slab
- Below knee POP at 2/52 and begin full weight bearing in this POP
- POP removed at 4/52 and aircast boot is considered
- Elevation
- If sedentary employment, return to work at 4/52 as long as elevated and protected
Goals:
- Safe and independent mobility with walking aid
- Independent with exercise programme
- Know monitoring and protection
Treatment:
- POP
- Pain-relief
- POLICE
- Basic circulatory exercises
- Mobility
Progress when:
Out of POP, fully weight bearing, no complications and then refer to physiotherapy out patients
Recovery Rehab 4 weeks - 3 months[edit | edit source]
Restrictions:
- No strengthening against resistance until 3 months if any tendon transfers
- No stretching tendons if transferred
Goals:
- Independent from aircast boot
- Achieve full ROM
Treatment:
- Pain relief, swlling management
- Advice, education, postural advice, monitoring complications, pacing
- Gait re-education
- Exercises --> PROM,AAROM, AROM, light strengthening, corse stability, balance/proprioception, stretching
- Hydrotherapy
- Orthotics
- Manual therapy --> SSTM's, mobilisations
Progress when:
Full ROM, independently mobile, neutral foot position in standing
Intermediate Rehab 12 weeks - 6 months[edit | edit source]
Restrictions:
- None
Goals:
- Independent with no aids
- Normal footwear
- Grade 5 strength
- Grade 4 strength in tendons transferred
Treatment:
- Pain relief, swlling management
- Advice, education, postural advice, monitoring complications, pacing
- Gait re-education
- Exercises --> PROM,AAROM, AROM, light strengthening, corse stability, balance/proprioception, stretching
- Hydrotherapy
- Orthotics
- Manual therapy --> SSTM's, mobilisations
Progress when:
Normal footwear, independent with no aids, pain controlled, strength 5/5 (4/5 if tendon transferred)
Final Rehab 6 months - 1 year[edit | edit source]
Goals:
- Return to gentle no-impact/low impact sports
- Grade 5 strength in transferred tendons
Treatment:
- Maximise function
- End stage exercises, balance and proprioception and sport specific
- Manual therapy
After the surgery it is important that the patient keeps moving and performing his daily activities. However there is still discussion between physicians about when the patient should start again with exercising. There are some that allow exercise immediately after surgery. But some say it is considered best to wait until there is a satisfactory bony in growth as shown radio graphically. However it’s the job of the physician to try to improve: the patient’s ROM of the ankle, maintain the ROM in the hip and knee, increase the muscle strength with exercise for the Gluteus Maximus, Quadriceps femoris muscles and the muscles that are responsible for dorsal flexion and the plantar flexion of the ankle. Postoperative mobilization begins early, with rapid progression to resumption of normal activities.[19] The goal is to obtain 10° of dorsal flexion and 30° of plantar flexion. For patients who have almost no motion in their ankle is any motion an improvement.[20]
In early postoperative period it is important that the incision heals and the implant becomes solidly fixed to the bony bed to do this they will use a below knee non-weight bearing immobilization. This is maintained until there is satisfactory bony in growth. [21]. The first 2 weeks the physician’s most important job is to help the patient maintain doing ADL activities, with crutches on a safe way. The second goal is to control the swelling and pain. It’s important that the patient rests and keeps his affected limb elevated above the heart.
After 2 weeks the cast will be replaced by a short leg boot. At this moment the patient goes back to the hospital for a first post-operative visit to the doctor.
The main goal for the physician is to increase the ROM of the ankle and maintain the hip and the knee ROM.
However there is still discussion between physicians about when the patient should start again with exercising. There are some that allow exercise immediately after surgery. But some say it is considered best to wait until there is a satisfactory bony in growth as shown radio graphically.
From here on it is important that the patient maintain his ROM from his ankle, knee and hip. He will be giving exercise to improve the strength of the Gluteus Maximus, Quadriceps and the muscles that are responsible for dorsal flexion and plantar flexion of the ankle.[22]
After a few months the patient needs to make an appointment with the doctor. Here they will take X-ray scans to see if there are no complications like: joint debridement for osseous impingement; the next most common procedures were extra-articular procedures for axial misalignments and component replacements.[23]
Resources
[edit | edit source]
| [24] | [25] |
| [26] | [27] |
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1lg0RU4SkRVBqMFj5d-bSyy2dkWVinKpajNeDAG9Bmj8Xqj5o|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Ankle Replacement Surgery. Annals of the Royal College of Surgeons of England. 2006 July;88(4):417-418
- ↑ Ankle Replacement Surgery. Annals of the Royal College of Surgeons of England. 2006 July;88(4):417-418
- ↑ http://www.medicalnewstoday.com/articles/11222.php
- ↑ http://www.medicalnewstoday.com/articles/11222.php
- ↑ Cerrato R, Myerson MS. Total Ankle Replacement:the Agility LP prosthesis. Foot and Ankle Clin. 2008 Sept; 13(3): 485-94.
- ↑ http://medicalnewstoday.com/printerfriendlynews.php?newsid=151776
- ↑ Haddad SL, Coetzee JC, Estok R. et al. Intermediate and Long-Term Outcomes of Total Ankle Arthroplasy and Ankle Arthrodesis. The Journal of Bone and Joint Surgery (American). 2007;89:1899-1905.
- ↑ SooHoo NF, Zingmond DS, Ko CY. Comparison of Reoperation Rates Following Ankle Arthrodesis and Total Ankle Arthroplasty. The Journal of Bone and Joint Surgery (American). 2007;89:2143-2149.
- ↑ Knecht SI, Estin M, Callaghan JJ et al. The Agility Total Ankle Arthroplasty: Seven to Sixteen-Year Follow-up. The Journal of Bone and Joint Surgery (American). 2004;86:1161-1171.
- ↑ Cracchiolo A 3rd, Deorio JK. Design features of current total ankle replacements: implants and instrumentation. Journal of the American Academy of Orthopedic Surgeons. 2008 Sept:16(9):530-40.
- ↑ 11.0 11.1 Drake, R. Vogl, A. Mitchell, A. Gray's Anatomy for Students. 2nd ed. 2010: 609. Churchill Livingstone: Elsevier: Philadelphia.
- ↑ MURNAGHAN J.M., WARNOCK D.S., HENDERSON S.A.., ‘Total Ankle Replacement: Early experience with STAR prothesis’, The Ulster Medical Journal, 2005, May, vol. 74, nr. 1, p. 9-13
- ↑ SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306
- ↑ SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic & Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67
- ↑ 15.0 15.1 15.2 15.3 15.4 Bonasia DE. Dettoni F. Femino JE. Phisitkul P. Germano M. Amendola A. Total Ankle Replacement: When, Why and How? The Iowa Orthopaedic Journal 2010(30)119-130
- ↑ Grawe JS. Mirow L. Bouchard R. Lindig M. Huppe M. Impact of preoperative patient education on postoperative pain in consideration of individual coping style. Schmerz 2010;24(6):575-86
- ↑ SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306
- ↑ Royal National Orthopaedic Hospital NHS Trust. Physiotherapy Rehabilitation Guidelines - Total Ankle Replacement Surgery. [ONLINE] available from: http://www.rnoh.nhs.uk/sites/default/files/downloads/physiotherapy_rehabilitation_guidelines_-_total_ankle_replacement_surgery.doc accessed [26/05/2014]
- ↑ SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306.
- ↑ SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic & Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67
- ↑ SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic & Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67
- ↑ SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306.
- ↑ ADRIENNE A. SPIRT, MATHIEU ASSAL, SIGVARD T. HANSEN Jr., ‘Complications and Failure After Total Ankle Arthroplasty’, The Journal of Bone and Joint Surgery, 2004, June, vol. 86-A, nr. 6, p.1172-1178
- ↑ Dr Selene Parekh Ankle Replacement Surgery https://www.youtube.com/channel/UCxqRUzmxviIRrz3MBt6Xxew [Accessed 24/05/2014]
- ↑ Dr Selene Parekh Ankle Replacement Surgery https://www.youtube.com/channel/UCxqRUzmxviIRrz3MBt6Xxew [Accessed 24/05/2014]
- ↑ Dr Selene Parekh Ankle Replacement Surgery https://www.youtube.com/channel/UCxqRUzmxviIRrz3MBt6Xxew {Accessed 24/05/2014]
- ↑ Total Ankle Replacement Surgery educational video. Available from https://www.youtube.com/watch?v=JGjyRJNWAbA [Accessed 24/05/2014]fckLR|}