Total Ankle Arthroplasty: Difference between revisions
No edit summary |
Rachael Lowe (talk | contribs) No edit summary |
||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
= What is an Ankle Arthroplasty? = | == What is an Ankle Arthroplasty? == | ||
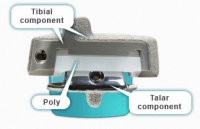
Ankle arthroplasty is when the ankle joint (Talocrural Joint) is replace with prosthetic components comprised of polyethylene and metal and is preferred to ankle arthrodesis (fusion) as range of movement and function an not compromised. Main objectives of the arthroplasty are to | Ankle arthroplasty is when the ankle joint (Talocrural Joint) is replace with prosthetic components comprised of polyethylene and metal and is preferred to ankle arthrodesis (fusion) as range of movement and function an not compromised. Main objectives of the arthroplasty are to | ||
| Line 13: | Line 13: | ||
#Maintain alignment and stability | #Maintain alignment and stability | ||
= History of Total Ankle Arthroplasty = | == History of Total Ankle Arthroplasty == | ||
Ankle replacement surgery has been available for over two decades however it is a far less common procedure than hip or knee arthroplasty owing to the less frequent incidence of osteoarthritis ankle pathology. The majority of ankle osteoarthritis is secondary to trauma.<ref>Ankle Replacement Surgery. Annals of the Royal College of Surgeons of England. 2006 July;88(4):417-418</ref><sup></sup> | Ankle replacement surgery has been available for over two decades however it is a far less common procedure than hip or knee arthroplasty owing to the less frequent incidence of [[Ankle_Osteoarthritis|osteoarthritis ankle pathology]]. The majority of ankle osteoarthritis is secondary to trauma.<ref>Ankle Replacement Surgery. Annals of the Royal College of Surgeons of England. 2006 July;88(4):417-418</ref><sup></sup> | ||
Until relatively recently, ankle joint arthrodesis (fusion) was the gold standard of treatment, but this was not without its complications, e.g. non-union, | Until relatively recently, ankle joint arthrodesis (fusion) was the gold standard of treatment, but this was not without its complications, e.g. non-union, osteoarthritis in the other mid/hind foot joints and stiffness and loss of proprioception<sup><ref>Ankle Replacement Surgery. Annals of the Royal College of Surgeons of England. 2006 July;88(4):417-418</ref></sup> | ||
Total ankle replacement was developed in the 1970's but initially was plagued with high long term failure rates. The older prosthesis loosened or malfunctioned and frequently needed to be removed<sup></sup><ref>[http://www.medicalnewstoday.com/articles/11222.php http://www.medicalnewstoday.com/articles/11222.php]</ref>. In the late 70's Dr. Frank G. Alvine an orthopedic surgeon from Sioux Falls, SD developed the Agility Ankle which was the first FDA approved total ankle implant in use in the United States<ref>[http://www.medicalnewstoday.com/articles/11222.php http://www.medicalnewstoday.com/articles/11222.php]</ref>. Since its introduction the Agility Ankle System has gone through several modifications. Currently the Agility Ankle System is the most widely used ankle prosthesis. With more than 20 years of experience it has the longest followup of any fixed bearing device<sup></sup><ref>Cerrato R, Myerson MS. Total Ankle Replacement:the Agility LP prosthesis. Foot and Ankle Clin. 2008 Sept; 13(3): 485-94.</ref>. | Total ankle replacement was developed in the 1970's but initially was plagued with high long term failure rates. The older prosthesis loosened or malfunctioned and frequently needed to be removed<sup></sup><ref>[http://www.medicalnewstoday.com/articles/11222.php http://www.medicalnewstoday.com/articles/11222.php]</ref>. In the late 70's Dr. Frank G. Alvine an orthopedic surgeon from Sioux Falls, SD developed the Agility Ankle which was the first FDA approved total ankle implant in use in the United States<ref>[http://www.medicalnewstoday.com/articles/11222.php http://www.medicalnewstoday.com/articles/11222.php]</ref>. Since its introduction the Agility Ankle System has gone through several modifications. Currently the Agility Ankle System is the most widely used ankle prosthesis. With more than 20 years of experience it has the longest followup of any fixed bearing device<sup></sup><ref>Cerrato R, Myerson MS. Total Ankle Replacement:the Agility LP prosthesis. Foot and Ankle Clin. 2008 Sept; 13(3): 485-94.</ref>. | ||
| Line 29: | Line 29: | ||
Poor patient satisfaction, high rates of revision due to loosening, and high wound complications rates were all very problematic when total ankle arthroplasty (TAA) surgeries were first introduced in the 1970’s.<ref name="Cook" /> In 1990, noncemented prostheses were shown to allow for bony ingrowth and less bone removal as compared to cemented.<ref name="Cook" /> Beyond the transition to cementless, further advances in technology over the years has led to new surgical arthroplasty techniques, primarily moving from a two-component design to a 3-component model. | Poor patient satisfaction, high rates of revision due to loosening, and high wound complications rates were all very problematic when total ankle arthroplasty (TAA) surgeries were first introduced in the 1970’s.<ref name="Cook" /> In 1990, noncemented prostheses were shown to allow for bony ingrowth and less bone removal as compared to cemented.<ref name="Cook" /> Beyond the transition to cementless, further advances in technology over the years has led to new surgical arthroplasty techniques, primarily moving from a two-component design to a 3-component model. | ||
An observational study analyzed advantages of arthroplasty over arthrodesis stating individuals with monoarticular or polyarticular disease who undergo arthroplasty have less gait abnormalities and fewer adverse effects to other joints in the lower extremity.<ref name="Doets">Doets, C., Brand, R., Nelissen, R. Total Ankle Arthroplasty in Inflammatory Joint Disease with Use of Two Mobile-Bearing Designs. The Journal of Bone and Joint Surgery. 2006;88:1274-1284.</ref> A systematic review provided that in 852 individuals undergoing TAA's, there was a 78% implant survival 5 years post-op and 77% at 10 years post-op and overall only had a 7% revision rate. This provides evidence that the procedure yields satisfactory results and should be considered for potential candidates that are appropriate for surgical corrections.<ref name="Haddad">Haddad, S. et all. Arthroplasty vs Arthrodesis: Intermediate and Long-Term Outcomes of Total Ankle Arthroplasty and Ankle Arthrodesis A Systematic Review of the Literature. The Journal of Bone and Joint Surgery. 2007;89:1899-1905.</ref><br> | An observational study analyzed advantages of arthroplasty over arthrodesis stating individuals with monoarticular or polyarticular disease who undergo arthroplasty have less gait abnormalities and fewer adverse effects to other joints in the lower extremity.<ref name="Doets">Doets, C., Brand, R., Nelissen, R. Total Ankle Arthroplasty in Inflammatory Joint Disease with Use of Two Mobile-Bearing Designs. The Journal of Bone and Joint Surgery. 2006;88:1274-1284.</ref> A systematic review provided that in 852 individuals undergoing TAA's, there was a 78% implant survival 5 years post-op and 77% at 10 years post-op and overall only had a 7% revision rate. This provides evidence that the procedure yields satisfactory results and should be considered for potential candidates that are appropriate for surgical corrections.<ref name="Haddad">Haddad, S. et all. Arthroplasty vs Arthrodesis: Intermediate and Long-Term Outcomes of Total Ankle Arthroplasty and Ankle Arthrodesis A Systematic Review of the Literature. The Journal of Bone and Joint Surgery. 2007;89:1899-1905.</ref><br> | ||
== The Arthroplasty == | |||
= | |||
The | |||
== Indication for Procedure<br> == | === Indication for Procedure<br> === | ||
There is no well-defined indication for a Total Ankle Arthroplasty. Surgery is considered only when conservative treatment has been attempted with no improvement. The operation is mainly being executed in patients who suffer from different types of arthrides. This cause advanced arthritic changes of disabling pain and loss of ankle motion. The ankle is most frequently affected by post-traumatic arthritis.<sup><ref>MURNAGHAN J.M., WARNOCK D.S., HENDERSON S.A.., ‘Total Ankle Replacement: Early experience with STAR prothesis’, The Ulster Medical Journal, 2005, May, vol. 74, nr. 1, p. 9-13</ref></sup> Total ankle joint replacement is also indicated following unsuccessful ankle arthrodesis <ref>SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306</ref> the ‘ideal’ patient for ankle joint replacement is an elderly person with the low physical demands who has good bone stock, normal vascular status, no immune-suppression, and excellent hind foot-ankle alignment.<ref>SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67</ref> Generally here are common indications for arthroplasty:<br> | There is no well-defined indication for a Total Ankle Arthroplasty. Surgery is considered only when conservative treatment has been attempted with no improvement. The operation is mainly being executed in patients who suffer from different types of arthrides. This cause advanced arthritic changes of disabling pain and loss of ankle motion. The ankle is most frequently affected by post-traumatic arthritis.<sup><ref>MURNAGHAN J.M., WARNOCK D.S., HENDERSON S.A.., ‘Total Ankle Replacement: Early experience with STAR prothesis’, The Ulster Medical Journal, 2005, May, vol. 74, nr. 1, p. 9-13</ref></sup> Total ankle joint replacement is also indicated following unsuccessful ankle arthrodesis <ref>SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306</ref> the ‘ideal’ patient for ankle joint replacement is an elderly person with the low physical demands who has good bone stock, normal vascular status, no immune-suppression, and excellent hind foot-ankle alignment.<ref>SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67</ref> Generally here are common indications for arthroplasty:<br> | ||
#Primary or post-traumatic [http://www.physio-pedia.com/Ankle_Osteoarthritis osteoarthritis] | #Primary or post-traumatic [http://www.physio-pedia.com/Ankle_Osteoarthritis osteoarthritis] | ||
| Line 77: | Line 41: | ||
#Rejected arthrodesis | #Rejected arthrodesis | ||
<br> '''Indications:''' | <br> '''Indications:''' | ||
According to Saltzman, there are no exact indications for receiving a total ankle arthroplasty.<ref name="Saltzman, CL" /> The “ideal” patient who would typically undergo this intervention is one who is elderly with a healthy immunity, normal vascular status, good bone density, and a proper hindfoot-ankle alignment who has not had success with conservative treatment measures. Individuals with debilitating ankle arthritis, unresponsive to nonoperative approaches, or have failures with the outcome of their ankle arthroplasty are typically treated with an arthrodesis procedure to fuse the joint. | |||
'''Contraindications:''' | '''Contraindications:''' | ||
Arthroplasty is contraindicated for those with neuroarthropathic degenerative joint disease, infection, avascular necrosis of the talus, osteochondritis dessicans, malalignment of the hindfoot-ankle, severe benign joint hypermobility syndromes or soft tissue problems, or decreased sensation or motion in the lower extremities.<ref name="Cook" /> In individuals with rheumatoid arthritis (RA), inflammatory processes may occur before signs of swelling, tissue reaction, and joint destruction are seen. In the first and second year of this disease process, structural damage (ie. joint erosion) can be seen with X-ray imaging.<ref name="Goodman & Snyder">Goodman, C., Snyder, T. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th ed. St. Louis: Saunders Elsevier, 2009.</ref> Diabetic patients may develop gouty arthritis in their ankle joint. This is caused by uric acid changing into urate crystals, which is deposited into the joint.<ref name="Goodman & Snyder" /> | |||
Thus, RA and diabetic individuals may or may not be candidates for ankle arthroplasty depending on the severity of joint degeneration found with radiographic imaging.<br> | Thus, RA and diabetic individuals may or may not be candidates for ankle arthroplasty depending on the severity of joint degeneration found with radiographic imaging.<br> | ||
| Line 89: | Line 55: | ||
#Neurological disorders or recurrent infection | #Neurological disorders or recurrent infection | ||
== Pre-operative Procedure and Definitive Diagnosis == | === Pre-operative Procedure and Definitive Diagnosis === | ||
Weight bearing A-P and lateral mortise views of bilateral ankles is required to make effective preparation and anticipation of that will be required in the surgery. The rearfoot alignment (Cobey/Saltzman) view is essential to evaluate the ankle joint and identify any calcaneal-totibial deformities. This is performed by getting the patient to stand, elevated with a cassette positioned at 15 degres anteriorly inclined with the x-ray bemed perpendicular to the film. This position is altered if deformities are present, after this has been taken anterior distal tibial angle (ADTA) is measured. The ADTA is formed by the mechanical axis of the tibia and the joint orientation line of the ankle in the sagittal plane and measures 80° ± 3° in the normal lower extremity. In the coronal plane, the lateral distal tibial angle (LDTA), the tibial-talar angle and the calcaneal tibial alignment should be measured. The LDTA is formed by the distal tibial articular surface and the anatomical axis of the tibia and measures 89° ± 3°.29, if this is decreased this represents a varus deformity. The tibial-talar angle (Figure 3C) is defined by the tibial and talar articular surfaces in the ankle joint. When the tibialtalar angle is >10° the joint is defined as incongruent (unstable)<ref name="Bon" />.<br><br>"If an abnormal ADTA or LDTA is present (sagittal or coronal deformity), the center of rotation of angulation (CORA) is measured. The CORA is the intersection of the mid-diaphyseal line and the line starting from the middle of the joint and perpendicular to the abnormal ADTA or LDTA (Figure 4). The CORA can be located at the joint line level (usually due to anatomical joint line malalignment or to ankle degeneration) or proximally (usually due to tibial deformities/fractures)"<ref name="Bon" />. So as you can see there are many consideration to be taken, and multiple angles to be analysed and this is important and any instability and malalignment of the new prosthesis can be excessively worn or may even fail<ref name="Bon" />. | Weight bearing A-P and lateral mortise views of bilateral ankles is required to make effective preparation and anticipation of that will be required in the surgery. The rearfoot alignment (Cobey/Saltzman) view is essential to evaluate the ankle joint and identify any calcaneal-totibial deformities. This is performed by getting the patient to stand, elevated with a cassette positioned at 15 degres anteriorly inclined with the x-ray bemed perpendicular to the film. This position is altered if deformities are present, after this has been taken anterior distal tibial angle (ADTA) is measured. The ADTA is formed by the mechanical axis of the tibia and the joint orientation line of the ankle in the sagittal plane and measures 80° ± 3° in the normal lower extremity. In the coronal plane, the lateral distal tibial angle (LDTA), the tibial-talar angle and the calcaneal tibial alignment should be measured. The LDTA is formed by the distal tibial articular surface and the anatomical axis of the tibia and measures 89° ± 3°.29, if this is decreased this represents a varus deformity. The tibial-talar angle (Figure 3C) is defined by the tibial and talar articular surfaces in the ankle joint. When the tibialtalar angle is >10° the joint is defined as incongruent (unstable)<ref name="Bon" />.<br><br>"If an abnormal ADTA or LDTA is present (sagittal or coronal deformity), the center of rotation of angulation (CORA) is measured. The CORA is the intersection of the mid-diaphyseal line and the line starting from the middle of the joint and perpendicular to the abnormal ADTA or LDTA (Figure 4). The CORA can be located at the joint line level (usually due to anatomical joint line malalignment or to ankle degeneration) or proximally (usually due to tibial deformities/fractures)"<ref name="Bon" />. So as you can see there are many consideration to be taken, and multiple angles to be analysed and this is important and any instability and malalignment of the new prosthesis can be excessively worn or may even fail<ref name="Bon" />. | ||
| Line 148: | Line 114: | ||
<br> Both component designs permit semiconstrained motion, specifically allowing some inversion and eversion during sagittal plane ankle movement. The four 2 component designs have been approved by the U.S. Food and Drug Administration (FDA). The STAR was recommended for approval by the FDA in 2008.<ref name="Cracchiolo">Cracchiolo A. III, Deorio, J.K. Design features of current total ankle replacements: implants and instrumentation. J Am Acad Orthop Surg. 2008;16(9):530-540.</ref><ref name="Guyer" /> There is insufficient evidence determining the life expectancy of current prosthesis designs.<ref name="Guyer" /> | <br> Both component designs permit semiconstrained motion, specifically allowing some inversion and eversion during sagittal plane ankle movement. The four 2 component designs have been approved by the U.S. Food and Drug Administration (FDA). The STAR was recommended for approval by the FDA in 2008.<ref name="Cracchiolo">Cracchiolo A. III, Deorio, J.K. Design features of current total ankle replacements: implants and instrumentation. J Am Acad Orthop Surg. 2008;16(9):530-540.</ref><ref name="Guyer" /> There is insufficient evidence determining the life expectancy of current prosthesis designs.<ref name="Guyer" /> | ||
== Surgical Procedure == | == Surgical Procedure == | ||
| Line 155: | Line 119: | ||
To perfrom the procedure the patient is positioned supine with the hip slightly elevated and a tourniquet on the proximal thigh to restrict blood flow during the procedure. Next a 10 cm incision is made over the centre of the joint line to expose the relevent anatomical structures. Once the structures have been exposed the crucial nerves and tendons are identified as to protect and ensure their integrity to minimise operative complications, these include; peroneal nerves, tibialis anterior and extensor hallucis longus. This is also to achieve correct talocrural alignment and soft tissue balance to ensure the prosthesis can achieve plantar grade in standing. It is also important to debride and correct any osteophytes or any other structures that can contribute to malalignment. Depending on the natural angle of the talocrural joint (varus or valgus) more bone medially or laterally may have ot be removed, this also may occur if the joint is deep or shallow as it may need to be reduced or elevated<ref name="Bon">Bonasia DE. Dettoni F. Femino JE. Phisitkul P. Germano M. Amendola A. Total Ankle Replacement: When, Why and How? The Iowa Orthopaedic Journal 2010(30)119-130</ref>. | To perfrom the procedure the patient is positioned supine with the hip slightly elevated and a tourniquet on the proximal thigh to restrict blood flow during the procedure. Next a 10 cm incision is made over the centre of the joint line to expose the relevent anatomical structures. Once the structures have been exposed the crucial nerves and tendons are identified as to protect and ensure their integrity to minimise operative complications, these include; peroneal nerves, tibialis anterior and extensor hallucis longus. This is also to achieve correct talocrural alignment and soft tissue balance to ensure the prosthesis can achieve plantar grade in standing. It is also important to debride and correct any osteophytes or any other structures that can contribute to malalignment. Depending on the natural angle of the talocrural joint (varus or valgus) more bone medially or laterally may have ot be removed, this also may occur if the joint is deep or shallow as it may need to be reduced or elevated<ref name="Bon">Bonasia DE. Dettoni F. Femino JE. Phisitkul P. Germano M. Amendola A. Total Ankle Replacement: When, Why and How? The Iowa Orthopaedic Journal 2010(30)119-130</ref>. | ||
Once the joints have been corrected and bones properly aligned the new components are trialed making sure rull ROM and stability is achieved. If dorsiflexion is limited and not due to malalignment then achilles tendon lengthening is required, the same goes for if there is instability in inversion or eversion the ligaments are reconstructed. Persistent malalignment can occure and may need separate procedures to correct such as subtalar fusion depending on severity and correctability<ref name="Bon" />. | |||
Once the joints have been corrected and bones properly aligned the new components are trialed making sure rull ROM and stability is achieved. If dorsiflexion is limited and not due to malalignment then achilles tendon lengthening is required, the same goes for if there is instability in inversion or eversion the ligaments are reconstructed. Persistent malalignment can occure and may need separate procedures to correct such as subtalar fusion depending on severity and correctability<ref name="Bon" />. | |||
=== Alternate Option: === | === Alternate Option: === | ||
| Line 163: | Line 125: | ||
'''Ankle Arthrodesis''' | '''Ankle Arthrodesis''' | ||
Ankle arthrodesis or fusion was the recommended surgical option after the failure of the first generation ankle arthroplasty. The procedure includes resecting the articular surfaces of the joint, realignment the talus and tibia and fusing the bones together. As a result, the ankle joint doesn’t allow any motion. The goal of ankle arthrodesis is pain relief.<ref name="Pfeiff">Pfeiff C. The Scandinavian Total Ankle Replacement (STAR). Orthop Nurs. 2006; 25(1): 30-33.</ref><ref name="Gill">Gill. LH. Challenges in Total Ankle Arthroplasty. Foot Ankle Int. 2004;25(4):195-207.</ref> Unfortunately, the lack of ankle motion can cause elevated stress on the knee and hindfoot and in addition, increases motion at the hindfoot that may become arthritic.<ref name="Cook" /> Other complications of fusion include accelerated degeneration of adjacent joint and limitations in activity.<ref name="Guyer">Guyer, A.J., Richardson, E.G. Current Concepts Review: Total Ankle Arthroplasty. Foot Ankle Int. 2008;29(2): 256-264.</ref><br> | [[Ankle_arthrodesis|Ankle arthrodesis]] or fusion was the recommended surgical option after the failure of the first generation ankle arthroplasty. The procedure includes resecting the articular surfaces of the joint, realignment the talus and tibia and fusing the bones together. As a result, the ankle joint doesn’t allow any motion. The goal of ankle arthrodesis is pain relief.<ref name="Pfeiff">Pfeiff C. The Scandinavian Total Ankle Replacement (STAR). Orthop Nurs. 2006; 25(1): 30-33.</ref><ref name="Gill">Gill. LH. Challenges in Total Ankle Arthroplasty. Foot Ankle Int. 2004;25(4):195-207.</ref> Unfortunately, the lack of ankle motion can cause elevated stress on the knee and hindfoot and in addition, increases motion at the hindfoot that may become arthritic.<ref name="Cook" /> Other complications of fusion include accelerated degeneration of adjacent joint and limitations in activity.<ref name="Guyer">Guyer, A.J., Richardson, E.G. Current Concepts Review: Total Ankle Arthroplasty. Foot Ankle Int. 2008;29(2): 256-264.</ref><br> | ||
{| width="300" cellspacing="1" cellpadding="1" border="0" align="center" | {| width="300" cellspacing="1" cellpadding="1" border="0" align="center" | ||
| Line 174: | Line 136: | ||
<br> | <br> | ||
== Outcome Measures == | == Outcome Measures == | ||
*[[Foot and Ankle Disability Index|Foot and Ankle Disability Index]] | *[[Foot and Ankle Disability Index|Foot and Ankle Disability Index]] | ||
| Line 182: | Line 144: | ||
== Physical Therapy Management <br> == | == Physical Therapy Management <br> == | ||
As it will be explained in the pre-operation and post-operation phase the multi-disciplinary team involved with the patient have a big role in making the arrangements before and after the surgery, this may involve physiotherapists, occupational therapists, discharge nurses, staff nurses, healthcare assistants as well as doctors. Both pre and post operative phases are integral to the progress of the patient and the pre-op should not be overlooked as important as it can be easy to focus on post-op. | As it will be explained in the pre-operation and post-operation phase the multi-disciplinary team involved with the patient have a big role in making the arrangements before and after the surgery, this may involve physiotherapists, occupational therapists, discharge nurses, staff nurses, healthcare assistants as well as doctors. Both pre and post operative phases are integral to the progress of the patient and the pre-op should not be overlooked as important as it can be easy to focus on post-op.<br> | ||
<br> | |||
== Pre-Operative Phase == | === Pre-Operative Phase === | ||
Before the surgery one of the main job for the team is to educate the patient about what will happen before, during and after the surgery as this will give the patient the opportunity to prepare, mentally rehearse, ensure smooth transition through short-term to long-term goals but also help control and reduce post-operative pain<ref name="Grawe">Grawe JS. Mirow L. Bouchard R. Lindig M. Huppe M. Impact of preoperative patient education on postoperative pain in consideration of individual coping style. Schmerz 2010;24(6):575-86</ref> | Before the surgery one of the main job for the team is to educate the patient about what will happen before, during and after the surgery as this will give the patient the opportunity to prepare, mentally rehearse, ensure smooth transition through short-term to long-term goals but also help control and reduce post-operative pain<ref name="Grawe">Grawe JS. Mirow L. Bouchard R. Lindig M. Huppe M. Impact of preoperative patient education on postoperative pain in consideration of individual coping style. Schmerz 2010;24(6):575-86</ref> | ||
| Line 192: | Line 152: | ||
ROM, muscle strength, gait and deviations will all be recorded as to compared before and after arthroplasty and ensure the patient is as optimal strength prior to operation if possible. For safety and ease of transition is can be important that the patient learns how to walk with crutches so they can perform ADL’s as soon as possible post arthroplasty but also understand that they will be non-weight bearing after the arthroplasty<ref>SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306</ref><span style="line-height: 1.5em;">.</span> | ROM, muscle strength, gait and deviations will all be recorded as to compared before and after arthroplasty and ensure the patient is as optimal strength prior to operation if possible. For safety and ease of transition is can be important that the patient learns how to walk with crutches so they can perform ADL’s as soon as possible post arthroplasty but also understand that they will be non-weight bearing after the arthroplasty<ref>SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306</ref><span style="line-height: 1.5em;">.</span> | ||
As will all procedures under general anesthetic there are common pulmonary postoperative complications (PPC's) which need to be controlled and risk reduced and this can be explained at this stage as well. | As will all procedures under general anesthetic there are common pulmonary postoperative complications (PPC's) which need to be controlled and risk reduced and this can be explained at this stage as well. <br> | ||
=== Post-Operative Phase === | |||
== Post-Operative Phase == | |||
It is important to ensure the risk of PPC's are reduced and respiratory physiotherapy may be used at this early stage, cough, deep breathing exercises and early mobility are essential here to reduce atelectasis and reinstate the muscoscilliary elevator as soon as possible. | It is important to ensure the risk of PPC's are reduced and respiratory physiotherapy may be used at this early stage, cough, deep breathing exercises and early mobility are essential here to reduce atelectasis and reinstate the muscoscilliary elevator as soon as possible. | ||
Atelecatsis occurs in 90% of anesthetized patients which leads to a 16-20% reduction in functional residual capacity which is why the alveoli tend collapse resulting in increased work of breathing, hypoxia, reduced compliance, V/Q mismatch and risk of pneumonia<ref>Neligan, Patrick. Anesthesiology Clin. 2013:30; 495-511</ref><ref>Neligan, Patrick. Anesthesiology Clin. 2013:30; 495-511</ref>. There is a 9% chance of developing pneumonia and this is where physiotherapy intervention is crucial at reducing the rate of all of these complications<ref>Tusman, Gerardo, et al. Curr Opin Anesthesiol 2012:25;1-10</ref>. | Atelecatsis occurs in 90% of anesthetized patients which leads to a 16-20% reduction in functional residual capacity which is why the alveoli tend collapse resulting in increased work of breathing, hypoxia, reduced compliance, V/Q mismatch and risk of pneumonia<ref>Neligan, Patrick. Anesthesiology Clin. 2013:30; 495-511</ref><ref>Neligan, Patrick. Anesthesiology Clin. 2013:30; 495-511</ref>. There is a 9% chance of developing pneumonia and this is where physiotherapy intervention is crucial at reducing the rate of all of these complications<ref>Tusman, Gerardo, et al. Curr Opin Anesthesiol 2012:25;1-10</ref>. | ||
<u>'''IT IS IMPORTANT TO KNOW YOUR OWN HOSPITALS/SURGEONS GUIDELINES FOLLOWING ARTHROPLASTY OR ANY OPERATION AND THE FOLLOWING SHOULD ONLY BE USED TO EDUCATE AND CONSIDER SOME BASIC/COMMON PROTOCOLS<br>'''</u> | <u>'''IT IS IMPORTANT TO KNOW YOUR OWN HOSPITALS/SURGEONS GUIDELINES FOLLOWING ARTHROPLASTY OR ANY OPERATION AND THE FOLLOWING SHOULD ONLY BE USED TO EDUCATE AND CONSIDER SOME BASIC/COMMON PROTOCOLS<br>'''</u> | ||
| Line 212: | Line 166: | ||
<u>'''THIS IS A PROTOCOL BY THE ROYAL NATIONAL ORTHOPAEDIC HOSPITAL NHS TRUST'''</u><ref name="Royal">Royal National Orthopaedic Hospital NHS Trust. Physiotherapy Rehabilitation Guidelines - Total Ankle Replacement Surgery. [ONLINE] available from: http://www.rnoh.nhs.uk/sites/default/files/downloads/physiotherapy_rehabilitation_guidelines_-_total_ankle_replacement_surgery.doc accessed [26/05/2014]</ref>, utilising the best available evidence<ref>Ali et al. Intermediate results of Buechel Pappas unconstrained total ankle replacement for osteoarthritis. The journal of foot and ankle surgery. 2007;46(1):16-20</ref><ref>Buechel at al. Twenty-year evaluation of cementless mobile-bearing total ankle replacements. clinical othopaedics and related research. 2004;424:19-26</ref><ref>Coetzee J. Caatro M. Accurate measurement of ankle range of motion after total ankle arthroplasty. Clinical orthopaedics and related research. 2004 27-31</ref><ref>Conti S. Wong YS. Complications of total ankle replacements. Clinical orthopaedics and related research. 2001;391:105-114</ref><ref>Knecht et al. The agility of total ankle arthroplasty. The journal of bone and joint surgery. 2004 1161-1171</ref><ref>Kontis et al. The management of failed ankle replacement. The jounrla of bone and joint surgery. 2006 1039-1047</ref> | <u>'''THIS IS A PROTOCOL BY THE ROYAL NATIONAL ORTHOPAEDIC HOSPITAL NHS TRUST'''</u><ref name="Royal">Royal National Orthopaedic Hospital NHS Trust. Physiotherapy Rehabilitation Guidelines - Total Ankle Replacement Surgery. [ONLINE] available from: http://www.rnoh.nhs.uk/sites/default/files/downloads/physiotherapy_rehabilitation_guidelines_-_total_ankle_replacement_surgery.doc accessed [26/05/2014]</ref>, utilising the best available evidence<ref>Ali et al. Intermediate results of Buechel Pappas unconstrained total ankle replacement for osteoarthritis. The journal of foot and ankle surgery. 2007;46(1):16-20</ref><ref>Buechel at al. Twenty-year evaluation of cementless mobile-bearing total ankle replacements. clinical othopaedics and related research. 2004;424:19-26</ref><ref>Coetzee J. Caatro M. Accurate measurement of ankle range of motion after total ankle arthroplasty. Clinical orthopaedics and related research. 2004 27-31</ref><ref>Conti S. Wong YS. Complications of total ankle replacements. Clinical orthopaedics and related research. 2001;391:105-114</ref><ref>Knecht et al. The agility of total ankle arthroplasty. The journal of bone and joint surgery. 2004 1161-1171</ref><ref>Kontis et al. The management of failed ankle replacement. The jounrla of bone and joint surgery. 2006 1039-1047</ref> | ||
As can be expected after any type of surgery, pain and inflammation must be controlled. This is the case especially after ankle replacement because pain and inflammation can last up to 12 months after surgery.<ref name="Lagaay">Lagaay PM, Schuberth JM. Analysis of Ankle Range of Motion and Functional Outcome Following Total Ankle Arthoplasty. The Journal of Foot and Ankle Surgery. 2010: Iss. 49, 147-151.</ref><span style="font-size: 13.28px;"> Surrounding muscles can be damaged during surgery and can result in decreased range of motion and strength.</span><ref name="Gougoulias">Gougoulias N, Khanna A, Maffulli N. How Successful are Current Ankle Replacements?: A Systematic Review of the Literature. Clinical Orthopaedics and Related Research. Clin Orthop Relat Res. Jan 2010: 199-208.</ref><ref name="Buechel">Buechel FF Sr, Buechel FF Jr, Pappas MJ. Twenty- year evaluation of cementless mobile-bearing total ankle replacements. Department of Orthopaedic Surgery New Jersey Medical School. Jul 2004: 19-26.</ref><ref name="Bonnin">Bonnin M, Judet T, Colombier JA, Buscayret JA, Graveleau N, Piriou P. Midterm results of the Salto Total Ankle Prosthesis. Clin Orthop Relat Res. Jul 2004: 6-18.</ref><span style="font-size: 13.28px;"> Damage to joint proprioceptors during excision of the capsule may cause deficits in both static and dynamic balance.</span><ref name="Lee">Lee KB, Park YH, Song EK, Yoon TR, Jung KI. Static and dynamic postural balance after successful mobile-bearing total ankle arthroplasty. Arch Phys Med Rehabil. Apr 2010: 519-522.</ref><ref name="Culham">Culham EG, Westlake KP, Wu Y. Sensory-specific balance training in older adults: effect on position, movement, and velocity sense at the ankle. Phys Ther. May 2007: 560-568.</ref><span style="font-size: 13.28px;"> These components can lead to gait disability and decreased efficiency of locomotion.</span><ref name="Detrembleur">Detrembleur C. Leemrijse T. The effects of total ankle replacement on gait disability: analysis of energetic and mechanical variables. Gait Posture. Feb 2009. 270-274.</ref><span style="font-size: 13.28px;"> Correction of gait posture and ambulation deficiencies will be a target of therapy once the patient is ambulating independently.</span> | |||
As can be expected after any type of surgery, pain and inflammation must be controlled. This is the case especially after ankle replacement because pain and inflammation can last up to 12 months after surgery.<ref name="Lagaay">Lagaay PM, Schuberth JM. Analysis of Ankle Range of Motion and Functional Outcome Following Total Ankle Arthoplasty. The Journal of Foot and Ankle Surgery. 2010: Iss. 49, 147-151.</ref> Surrounding muscles can be damaged during surgery and can result in decreased range of motion and strength.<ref name="Gougoulias">Gougoulias N, Khanna A, Maffulli N. How Successful are Current Ankle Replacements?: A Systematic Review of the Literature. Clinical Orthopaedics and Related Research. Clin Orthop Relat Res. Jan 2010: 199-208.</ref><ref name="Buechel">Buechel FF Sr, Buechel FF Jr, Pappas MJ. Twenty- year evaluation of cementless mobile-bearing total ankle replacements. Department of Orthopaedic Surgery New Jersey Medical School. Jul 2004: 19-26.</ref><ref name="Bonnin">Bonnin M, Judet T, Colombier JA, Buscayret JA, Graveleau N, Piriou P. Midterm results of the Salto Total Ankle Prosthesis. Clin Orthop Relat Res. Jul 2004: 6-18.</ref> Damage to joint proprioceptors during excision of the capsule may cause deficits in both static and dynamic balance.<ref name="Lee">Lee KB, Park YH, Song EK, Yoon TR, Jung KI. Static and dynamic postural balance after successful mobile-bearing total ankle arthroplasty. Arch Phys Med Rehabil. Apr 2010: 519-522.</ref><ref name="Culham">Culham EG, Westlake KP, Wu Y. Sensory-specific balance training in older adults: effect on position, movement, and velocity sense at the ankle. Phys Ther. May 2007: 560-568.</ref> These components can lead to gait disability and decreased efficiency of locomotion.<ref name="Detrembleur">Detrembleur C. Leemrijse T. The effects of total ankle replacement on gait disability: analysis of energetic and mechanical variables. Gait Posture. Feb 2009. 270-274.</ref> Correction of gait posture and ambulation deficiencies will be a target of therapy once the patient is ambulating independently.< | |||
===== Physical Therapy Goals: ===== | ===== Physical Therapy Goals: ===== | ||
| Line 225: | Line 177: | ||
*Improve proprioception | *Improve proprioception | ||
*Proper independent ambulation<br> | *Proper independent ambulation<br> | ||
===== Assessment ===== | ===== Assessment ===== | ||
| Line 261: | Line 211: | ||
**Assess safety in mobility | **Assess safety in mobility | ||
*Gait Assessment<ref name="Huber" /><br> | *Gait Assessment<ref name="Huber" /><br> | ||
=== '''Initial Rehab 0-4 Weeks''' === | === '''Initial Rehab 0-4 Weeks''' === | ||
| Line 290: | Line 238: | ||
'''Progress when:''' | '''Progress when:''' | ||
Out of POP, fully weight bearing, no complications and then refer to physiotherapy out patients | Out of POP, fully weight bearing, no complications and then refer to physiotherapy out patients<br> | ||
<br> | |||
=== Recovery Rehab 4 weeks - 3 months === | === Recovery Rehab 4 weeks - 3 months === | ||
| Line 318: | Line 264: | ||
'''Progress when:''' | '''Progress when:''' | ||
Full ROM, independently mobile, neutral foot position in standing | Full ROM, independently mobile, neutral foot position in standing<br> | ||
<br> | |||
=== Intermediate Rehab 12 weeks - 6 months === | === Intermediate Rehab 12 weeks - 6 months === | ||
| Line 347: | Line 291: | ||
'''Progress when:''' | '''Progress when:''' | ||
Normal footwear, independent with no aids, pain controlled, strength 5/5 (4/5 if tendon transferred) | Normal footwear, independent with no aids, pain controlled, strength 5/5 (4/5 if tendon transferred)<br> | ||
<br> | |||
=== Final Rehab 6 months - 1 year === | === Final Rehab 6 months - 1 year === | ||
| Line 362: | Line 304: | ||
*Maximise function | *Maximise function | ||
*End stage exercises, balance and proprioception and sport specific | *End stage exercises, balance and proprioception and sport specific | ||
*Manual therapy | *Manual therapy<br> | ||
<br> | |||
=== Muscles to Consider === | === Muscles to Consider === | ||
| Line 426: | Line 366: | ||
| <sup>Ankle PF</sup> | | <sup>Ankle PF</sup> | ||
|} | |} | ||
<br> | <br> | ||
| Line 433: | Line 371: | ||
=== Additional Information === | === Additional Information === | ||
After the surgery it is important that the patient keeps moving and performing his daily activities. However there is still discussion between physicians about when the patient should start again with exercising. There are some that allow exercise immediately after surgery. But some say it is considered best to wait until there is a satisfactory bony in growth as shown radio graphically. However it’s the job of the physician to try to improve:<span style="mso-spacerun:yes"> </span>the patient’s ROM of the ankle, maintain the ROM in the hip and knee, increase the muscle strength with exercise for the Gluteus Maximus, Quadriceps femoris muscles and the muscles that are responsible for dorsal flexion and the plantar flexion of the ankle<ref>SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306.</ref><span style="line-height: 1.5em;">. Postoperative mobilization begins early, with rapid progression to resumption of normal activities.</span><ref>SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306.</ref><sup style="line-height: 1.5em;"> </sup><span style="line-height: 1.5em;">The goal is to obtain 10° of dorsal flexion and 30° of plantar flexion. For patients who have almost no motion in their ankle is any motion an improvement.</span><ref>SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67</ref><span style="line-height: 1.5em;"> </span> | After the surgery it is important that the patient keeps moving and performing his daily activities. However there is still discussion between physicians about when the patient should start again with exercising. There are some that allow exercise immediately after surgery. But some say it is considered best to wait until there is a satisfactory bony in growth as shown radio graphically. However it’s the job of the physician to try to improve:<span style="mso-spacerun:yes"> </span>the patient’s ROM of the ankle, maintain the ROM in the hip and knee, increase the muscle strength with exercise for the Gluteus Maximus, Quadriceps femoris muscles and the muscles that are responsible for dorsal flexion and the plantar flexion of the ankle<ref>SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306.</ref><span style="line-height: 1.5em;">. Postoperative mobilization begins early, with rapid progression to resumption of normal activities.</span><ref>SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306.</ref><sup style="line-height: 1.5em;"> </sup><span style="line-height: 1.5em;">The goal is to obtain 10° of dorsal flexion and 30° of plantar flexion. For patients who have almost no motion in their ankle is any motion an improvement.</span><ref>SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67</ref><span style="line-height: 1.5em;"> </span> | ||
In early postoperative period it is important that the incision heals and the implant becomes solidly fixed to the bony bed to do this they will use a below knee non-weight bearing immobilization. This is maintained until there is satisfactory bony in growth.<sup> </sup><ref>SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67</ref><sup>. </sup>Another goal is to i<span lang="EN-US">ncrease the ROM of the ankle and maintain the hip and the knee ROM.</span><br> | In early postoperative period it is important that the incision heals and the implant becomes solidly fixed to the bony bed to do this they will use a below knee non-weight bearing immobilization. This is maintained until there is satisfactory bony in growth.<sup> </sup><ref>SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67</ref><sup>. </sup>Another goal is to i<span lang="EN-US">ncrease the ROM of the ankle and maintain the hip and the knee ROM.</span><br> | ||
After a few months the patient needs to make an appointment with the doctor. Here they will take X-ray scans to see if there are no complications like: joint debridement for osseous impingement; the next most common procedures were extra-articular procedures for axial misalignments and component replacements.<ref>ADRIENNE A. SPIRT, MATHIEU ASSAL, SIGVARD T. HANSEN Jr., ‘Complications and Failure After Total Ankle Arthroplasty’, The Journal of Bone and Joint Surgery, 2004, June, vol. 86-A, nr. 6, p.1172-1178</ref> <br> | After a few months the patient needs to make an appointment with the doctor. Here they will take X-ray scans to see if there are no complications like: joint debridement for osseous impingement; the next most common procedures were extra-articular procedures for axial misalignments and component replacements.<ref>ADRIENNE A. SPIRT, MATHIEU ASSAL, SIGVARD T. HANSEN Jr., ‘Complications and Failure After Total Ankle Arthroplasty’, The Journal of Bone and Joint Surgery, 2004, June, vol. 86-A, nr. 6, p.1172-1178</ref> <br> | ||
= Prognosis & Outcome = | == Prognosis & Outcome == | ||
Outcome of ankle arthroplasty includes pain, function implant survival and complications. There are numerous studies looking at survival rate of implants and rates are reported around 67-94% at 5 years<ref name="Had">Haddad, S.L.; Coetzee, J.C.; Estok, R.; Fahrbach, K.; Banel, D.; Nalysnyk, L. (2007). "Intermediate and Long-Term Outcomes of Total Ankle Arthroplasty and Ankle Arthrodesis. A Systematic Review of the Literature". Journal of Bone and Joint Surgery 89A (9): 1899–905</ref><ref name="Ste">Stengel, Dirk; Bauwens, Kai; Ekkernkamp, Axel; Cramer, Jörg (2005). "Efficacy of total ankle replacement with meniscal-bearing devices: a systematic review and meta-analysis". Archives of Orthopaedic and Trauma Surgery 125 (2): 109–19</ref><ref>Gougoulias, Nikolaos; Khanna, Anil; Maffulli, Nicola (2009). "How Successful are Current Ankle Replacements? All though most total ankle replacement are successful by reducing pain and improving mobility there is a very high possibility that the pain may be ten times worse. There have been several cases where the doctors have recommended amputation to resolve the issue of pain that was not there prior to the total ankle replacement. : A Systematic Review of the Literature". Clinical Orthopaedics and Related Research 468: 199–208.</ref> and 75% at ten years<ref name="Had" /> which is reasonably reliable. | Outcome of ankle arthroplasty includes pain, function implant survival and complications. There are numerous studies looking at survival rate of implants and rates are reported around 67-94% at 5 years<ref name="Had">Haddad, S.L.; Coetzee, J.C.; Estok, R.; Fahrbach, K.; Banel, D.; Nalysnyk, L. (2007). "Intermediate and Long-Term Outcomes of Total Ankle Arthroplasty and Ankle Arthrodesis. A Systematic Review of the Literature". Journal of Bone and Joint Surgery 89A (9): 1899–905</ref><ref name="Ste">Stengel, Dirk; Bauwens, Kai; Ekkernkamp, Axel; Cramer, Jörg (2005). "Efficacy of total ankle replacement with meniscal-bearing devices: a systematic review and meta-analysis". Archives of Orthopaedic and Trauma Surgery 125 (2): 109–19</ref><ref>Gougoulias, Nikolaos; Khanna, Anil; Maffulli, Nicola (2009). "How Successful are Current Ankle Replacements? All though most total ankle replacement are successful by reducing pain and improving mobility there is a very high possibility that the pain may be ten times worse. There have been several cases where the doctors have recommended amputation to resolve the issue of pain that was not there prior to the total ankle replacement. : A Systematic Review of the Literature". Clinical Orthopaedics and Related Research 468: 199–208.</ref> and 75% at ten years<ref name="Had" /> which is reasonably reliable. | ||
| Line 461: | Line 399: | ||
|} | |} | ||
<br> | |||
<br | |||
= References = | = References = | ||
Revision as of 14:38, 22 March 2017
Original Editor - Carlos De Coster
Top Contributors - Jeremy Brady, Jorge Solorzano, Admin, Scott Buxton, Kim Jackson, Dana Williams, Shaimaa Eldib, Carlos De Coster, Neha Palsule, 127.0.0.1, Mariam Hashem, Simisola Ajeyalemi, Uchechukwu Chukwuemeka, Tony Lowe, Sharon Schumacher, Lucinda hampton, Jess Bell, Michael Kauffmann, George Prudden, Ryan De Laet, Rachael Lowe and Rucha Gadgil
What is an Ankle Arthroplasty?[edit | edit source]
Ankle arthroplasty is when the ankle joint (Talocrural Joint) is replace with prosthetic components comprised of polyethylene and metal and is preferred to ankle arthrodesis (fusion) as range of movement and function an not compromised. Main objectives of the arthroplasty are to
- Replicate ROM of the talocrural joint
- Function well under weight bearing
- Be wear resistent
- Maintain alignment and stability
History of Total Ankle Arthroplasty [edit | edit source]
Ankle replacement surgery has been available for over two decades however it is a far less common procedure than hip or knee arthroplasty owing to the less frequent incidence of osteoarthritis ankle pathology. The majority of ankle osteoarthritis is secondary to trauma.[1]
Until relatively recently, ankle joint arthrodesis (fusion) was the gold standard of treatment, but this was not without its complications, e.g. non-union, osteoarthritis in the other mid/hind foot joints and stiffness and loss of proprioception[2]
Total ankle replacement was developed in the 1970's but initially was plagued with high long term failure rates. The older prosthesis loosened or malfunctioned and frequently needed to be removed[3]. In the late 70's Dr. Frank G. Alvine an orthopedic surgeon from Sioux Falls, SD developed the Agility Ankle which was the first FDA approved total ankle implant in use in the United States[4]. Since its introduction the Agility Ankle System has gone through several modifications. Currently the Agility Ankle System is the most widely used ankle prosthesis. With more than 20 years of experience it has the longest followup of any fixed bearing device[5].
On May 29, 2009 the medical news today announced the FDA approved the first mobile bearing device called the Scandinavian Total Ankle Replacement System (STAR). As a condition of FDA approval the company (Small Bone Innovations Inc.) must evaluate the safety and effectiveness of the device during the next eight years[6].
In a systematic review of the literature published in the Journal of Bone and Joint Surgery in 2007, the intermediate outcome of total ankle arthroplasty appears to be similiar to that of ankle arthrodesis however data was sparse[7]. In a study comparing reoperation rates following ankle arthrodesis and total ankle arthroplasty SooHoo, Zingmond and Ko confirmed that ankle replacement is associated with a higher risk of complications as compared with ankle fusion, but also has potential advantages in terms of a decreased risk of the patient requiring subtalar joint fusion[8]. In a seven to sixteen year follow up on the Agility Total Ankle Arthroplasty, Knecht, Estin, Callagham et al concluded that the relatively low rates of radiographic hindfoot arthritis and revision procedures at an average of nine years after the arthroplasty are encouraging[9].
Although interest in total ankle replacements is increasing, midterm clinical results to date are few and often have not been validated by independent pratitioners. In addition no level I or II studies have been published[10].
Poor patient satisfaction, high rates of revision due to loosening, and high wound complications rates were all very problematic when total ankle arthroplasty (TAA) surgeries were first introduced in the 1970’s.[11] In 1990, noncemented prostheses were shown to allow for bony ingrowth and less bone removal as compared to cemented.[11] Beyond the transition to cementless, further advances in technology over the years has led to new surgical arthroplasty techniques, primarily moving from a two-component design to a 3-component model.
An observational study analyzed advantages of arthroplasty over arthrodesis stating individuals with monoarticular or polyarticular disease who undergo arthroplasty have less gait abnormalities and fewer adverse effects to other joints in the lower extremity.[12] A systematic review provided that in 852 individuals undergoing TAA's, there was a 78% implant survival 5 years post-op and 77% at 10 years post-op and overall only had a 7% revision rate. This provides evidence that the procedure yields satisfactory results and should be considered for potential candidates that are appropriate for surgical corrections.[13]
The Arthroplasty[edit | edit source]
Indication for Procedure
[edit | edit source]
There is no well-defined indication for a Total Ankle Arthroplasty. Surgery is considered only when conservative treatment has been attempted with no improvement. The operation is mainly being executed in patients who suffer from different types of arthrides. This cause advanced arthritic changes of disabling pain and loss of ankle motion. The ankle is most frequently affected by post-traumatic arthritis.[14] Total ankle joint replacement is also indicated following unsuccessful ankle arthrodesis [15] the ‘ideal’ patient for ankle joint replacement is an elderly person with the low physical demands who has good bone stock, normal vascular status, no immune-suppression, and excellent hind foot-ankle alignment.[16] Generally here are common indications for arthroplasty:
- Primary or post-traumatic osteoarthritis
- Severe rheumatoid arthritis
- Rejected arthrodesis
Indications:
According to Saltzman, there are no exact indications for receiving a total ankle arthroplasty.[17] The “ideal” patient who would typically undergo this intervention is one who is elderly with a healthy immunity, normal vascular status, good bone density, and a proper hindfoot-ankle alignment who has not had success with conservative treatment measures. Individuals with debilitating ankle arthritis, unresponsive to nonoperative approaches, or have failures with the outcome of their ankle arthroplasty are typically treated with an arthrodesis procedure to fuse the joint.
Contraindications: Arthroplasty is contraindicated for those with neuroarthropathic degenerative joint disease, infection, avascular necrosis of the talus, osteochondritis dessicans, malalignment of the hindfoot-ankle, severe benign joint hypermobility syndromes or soft tissue problems, or decreased sensation or motion in the lower extremities.[11] In individuals with rheumatoid arthritis (RA), inflammatory processes may occur before signs of swelling, tissue reaction, and joint destruction are seen. In the first and second year of this disease process, structural damage (ie. joint erosion) can be seen with X-ray imaging.[18] Diabetic patients may develop gouty arthritis in their ankle joint. This is caused by uric acid changing into urate crystals, which is deposited into the joint.[18]
Thus, RA and diabetic individuals may or may not be candidates for ankle arthroplasty depending on the severity of joint degeneration found with radiographic imaging.
Common contraindications are:
- Severe talus subluxation, severe valgus or varus deformity
- Substantial osteoporosis
- Neurological disorders or recurrent infection
Pre-operative Procedure and Definitive Diagnosis[edit | edit source]
Weight bearing A-P and lateral mortise views of bilateral ankles is required to make effective preparation and anticipation of that will be required in the surgery. The rearfoot alignment (Cobey/Saltzman) view is essential to evaluate the ankle joint and identify any calcaneal-totibial deformities. This is performed by getting the patient to stand, elevated with a cassette positioned at 15 degres anteriorly inclined with the x-ray bemed perpendicular to the film. This position is altered if deformities are present, after this has been taken anterior distal tibial angle (ADTA) is measured. The ADTA is formed by the mechanical axis of the tibia and the joint orientation line of the ankle in the sagittal plane and measures 80° ± 3° in the normal lower extremity. In the coronal plane, the lateral distal tibial angle (LDTA), the tibial-talar angle and the calcaneal tibial alignment should be measured. The LDTA is formed by the distal tibial articular surface and the anatomical axis of the tibia and measures 89° ± 3°.29, if this is decreased this represents a varus deformity. The tibial-talar angle (Figure 3C) is defined by the tibial and talar articular surfaces in the ankle joint. When the tibialtalar angle is >10° the joint is defined as incongruent (unstable)[19].
"If an abnormal ADTA or LDTA is present (sagittal or coronal deformity), the center of rotation of angulation (CORA) is measured. The CORA is the intersection of the mid-diaphyseal line and the line starting from the middle of the joint and perpendicular to the abnormal ADTA or LDTA (Figure 4). The CORA can be located at the joint line level (usually due to anatomical joint line malalignment or to ankle degeneration) or proximally (usually due to tibial deformities/fractures)"[19]. So as you can see there are many consideration to be taken, and multiple angles to be analysed and this is important and any instability and malalignment of the new prosthesis can be excessively worn or may even fail[19].
Medical Management
[edit | edit source]
First generation:[edit | edit source]
Early ankle prosthesis attempts involved cementing a stemmed metal ball into the tibia and a polyethylene cup cemented into the talus. Throughout the 1970’s, prosthesis evolved into using a vitallium component cemented into the talus. All designs used methylmethacrylate cement, which became the defining element of first generation prosthesis.[11]
Types:[edit | edit source]
- Constrained - Increased stability due to only allowing dorsiflexion and plantarflexion. Loosening of the prosthesis was common from increased torque at the joint.[11]
- Nonconstrained - Allows full ROM, resulting in decreased stability that commonly caused impingement against the medial and/or lateral malleoli.
- Semiconstrained - A combination of contrained and nonconstrained models, allowing greater ROM and medial-lateral stability. The Imperial College, London Hospital prosthesis uses a concave polyethylene in the tibia and a stainless steel component on the talus.[11]
Unfortunately, by the early 1980’s, first generation ankle arthroplasties were not recommended by the majority of orthaepedic surgeons. Numerous studies showed loosening of the cement fixation, wound issues, and low patient satisfaction [17][11]. As a result of the poor outcomes and high complication rate, surgeons began to recommended ankle arthrodesis.
Second generation:[edit | edit source]
Second generation arthroplasties are cementless, using bony ingrowth to stabilize the implant. Compared to cement, bony ingrowth prosthesis have less bone resection, damage to soft tissue and complications of the cement such as cement displacement[17].
Surgical Factors:[edit | edit source]
- Fixation: Ingrowth implants tend to have either a beaded surface along the bony interface, hydroxyapatite layer or a combination of both. Current surgical designs tend to use the combination fixation technique.[11][17] Between types of prosthesis the number of articulating surfaces and components both need to be considered.[17][11][20].
- Components:
- Articulating surfaces: Current designs vary on the articulations that need to be resurfaced. Resurfacing may occur at the superior tibiotalar joint, superior and medial articulations, or medial, lateral, and superior joints.[11] Determining which patients would benefit the most from each type of surgery is ongoing.[17]
Design components:[edit | edit source]
- 2 component implants include a tibial and talar articulating component. Implants may also incorporate syndesmosis fusion to resurface the medial and lateral recesses of ankle and converting the ankle from a 3-bone joint to a 2-bone joint. Known designs: Agility, Salto Talaris, Eclipse, INBONE
- Advantages: decreased shear and torsion on prosthesis[21], syndesmosis decreases shear force and increase the bony support for the tibial component[17]
- Disadvantages: increased bony resection, likelihood of soft tissue compromise, accelerated polyethylene wear, and possibility of syndesmosis fusion failure.[17]

|
|
| Salto Talaris | Agility |
- 3 component implants include a “mobile bearing” of polyethylene between the tibial plate and talar component. Known designs: Buechel-Pappas, Scandinavian Total Ankle Replacement (STAR), Mobility, HINTEGRA

|
|
| STAR | Buechel Pappas |
Both component designs permit semiconstrained motion, specifically allowing some inversion and eversion during sagittal plane ankle movement. The four 2 component designs have been approved by the U.S. Food and Drug Administration (FDA). The STAR was recommended for approval by the FDA in 2008.[22][21] There is insufficient evidence determining the life expectancy of current prosthesis designs.[21]
Surgical Procedure[edit | edit source]
To perfrom the procedure the patient is positioned supine with the hip slightly elevated and a tourniquet on the proximal thigh to restrict blood flow during the procedure. Next a 10 cm incision is made over the centre of the joint line to expose the relevent anatomical structures. Once the structures have been exposed the crucial nerves and tendons are identified as to protect and ensure their integrity to minimise operative complications, these include; peroneal nerves, tibialis anterior and extensor hallucis longus. This is also to achieve correct talocrural alignment and soft tissue balance to ensure the prosthesis can achieve plantar grade in standing. It is also important to debride and correct any osteophytes or any other structures that can contribute to malalignment. Depending on the natural angle of the talocrural joint (varus or valgus) more bone medially or laterally may have ot be removed, this also may occur if the joint is deep or shallow as it may need to be reduced or elevated[19].
Once the joints have been corrected and bones properly aligned the new components are trialed making sure rull ROM and stability is achieved. If dorsiflexion is limited and not due to malalignment then achilles tendon lengthening is required, the same goes for if there is instability in inversion or eversion the ligaments are reconstructed. Persistent malalignment can occure and may need separate procedures to correct such as subtalar fusion depending on severity and correctability[19].
Alternate Option:[edit | edit source]
Ankle Arthrodesis
Ankle arthrodesis or fusion was the recommended surgical option after the failure of the first generation ankle arthroplasty. The procedure includes resecting the articular surfaces of the joint, realignment the talus and tibia and fusing the bones together. As a result, the ankle joint doesn’t allow any motion. The goal of ankle arthrodesis is pain relief.[23][20] Unfortunately, the lack of ankle motion can cause elevated stress on the knee and hindfoot and in addition, increases motion at the hindfoot that may become arthritic.[11] Other complications of fusion include accelerated degeneration of adjacent joint and limitations in activity.[21]
| Used with permission by Susan Barber Lindquist, Media Relations Coordinator, Mayo Clinic Health System[24] |
Outcome Measures[edit | edit source]
Physical Therapy Management
[edit | edit source]
As it will be explained in the pre-operation and post-operation phase the multi-disciplinary team involved with the patient have a big role in making the arrangements before and after the surgery, this may involve physiotherapists, occupational therapists, discharge nurses, staff nurses, healthcare assistants as well as doctors. Both pre and post operative phases are integral to the progress of the patient and the pre-op should not be overlooked as important as it can be easy to focus on post-op.
Pre-Operative Phase[edit | edit source]
Before the surgery one of the main job for the team is to educate the patient about what will happen before, during and after the surgery as this will give the patient the opportunity to prepare, mentally rehearse, ensure smooth transition through short-term to long-term goals but also help control and reduce post-operative pain[25]
ROM, muscle strength, gait and deviations will all be recorded as to compared before and after arthroplasty and ensure the patient is as optimal strength prior to operation if possible. For safety and ease of transition is can be important that the patient learns how to walk with crutches so they can perform ADL’s as soon as possible post arthroplasty but also understand that they will be non-weight bearing after the arthroplasty[26].
As will all procedures under general anesthetic there are common pulmonary postoperative complications (PPC's) which need to be controlled and risk reduced and this can be explained at this stage as well.
Post-Operative Phase[edit | edit source]
It is important to ensure the risk of PPC's are reduced and respiratory physiotherapy may be used at this early stage, cough, deep breathing exercises and early mobility are essential here to reduce atelectasis and reinstate the muscoscilliary elevator as soon as possible.
Atelecatsis occurs in 90% of anesthetized patients which leads to a 16-20% reduction in functional residual capacity which is why the alveoli tend collapse resulting in increased work of breathing, hypoxia, reduced compliance, V/Q mismatch and risk of pneumonia[27][28]. There is a 9% chance of developing pneumonia and this is where physiotherapy intervention is crucial at reducing the rate of all of these complications[29].
IT IS IMPORTANT TO KNOW YOUR OWN HOSPITALS/SURGEONS GUIDELINES FOLLOWING ARTHROPLASTY OR ANY OPERATION AND THE FOLLOWING SHOULD ONLY BE USED TO EDUCATE AND CONSIDER SOME BASIC/COMMON PROTOCOLS
THIS SHOULD NOT BE USED IN REPLACEMENT OF THE SURGEONS PROTOCOL
THIS IS A PROTOCOL BY THE ROYAL NATIONAL ORTHOPAEDIC HOSPITAL NHS TRUST[30], utilising the best available evidence[31][32][33][34][35][36]
As can be expected after any type of surgery, pain and inflammation must be controlled. This is the case especially after ankle replacement because pain and inflammation can last up to 12 months after surgery.[37] Surrounding muscles can be damaged during surgery and can result in decreased range of motion and strength.[38][39][40] Damage to joint proprioceptors during excision of the capsule may cause deficits in both static and dynamic balance.[41][42] These components can lead to gait disability and decreased efficiency of locomotion.[43] Correction of gait posture and ambulation deficiencies will be a target of therapy once the patient is ambulating independently.
Physical Therapy Goals:[edit | edit source]
- Decrease pain
- Decrease inflammation
- Increase strength
- Increase range of motion
- Improve dynamic and static balance
- Improve proprioception
- Proper independent ambulation
Assessment[edit | edit source]
- Mechanism of injury or etiology of illness
- Date of surgery and type of implant
- Use of assistive device with weight bearing status
- Use of controlled ankle motion (CAM) walker/walking boot
- Functional deficits/assistance with ADLs/adaptive equipment
- Pain/ Symptom history: Location, duration, type, intensity (VAS), aggravating and relieving factors, 24 hour symptom behavior
- Relevant Current/Past Medical history: Other lower extremity arthritis or injuries,upper extremity issues that may limit ability to ambulate with an AD and comorbid diagnoses
- Medications for current/previous diagnoses
- Diagnostic tests
- Sleep disturbance
- Barriers to learning
- Social/occupational history
- Patient’s goals
- Vocation/avocation and associated repetitive behaviors
- Living environment
Relevant Tests & Measures:[edit | edit source]
- Observation/inspection/palpation: Skin and incision assessment, edema, muscle atrophy
- Circulation: Dorsal pedal pulse
- Sensory and proprioception testing
- Range of motion and Muscle length: Average postoperative arc of motion (dorsifexion and plantarfexion) is 23°[44][45]
- Muscle strength
- Posture: Increased pronation/supination in standing, ability to maintain wait bearing status
- Assess assistive and adaptive devices for need and proper fit
- Balance: Static and dynamic standing balance, unilateral balance of the unaffected extremity (especially if patient is still non-weight bearing).[44] Patient may demonstrate dynamic postural imbalance, less reliance on ankle strategy and deficit of motor control ability[41]
- Functional mobility
- Gait Assessment[44]
Initial Rehab 0-4 Weeks[edit | edit source]
Restrictions:
- Non-weight bearing 2/52 with a back slab
- Below knee POP at 2/52 and begin full weight bearing in this POP
- POP removed at 4/52 and aircast boot is considered
- Elevation
- If sedentary employment, return to work at 4/52 as long as elevated and protected
Goals:
- Safe and independent mobility with walking aid
- Independent with exercise programme
- Know monitoring and protection
Treatment:
- POP
- Pain-relief
- POLICE
- Basic circulatory exercises
- Mobility
Progress when:
Out of POP, fully weight bearing, no complications and then refer to physiotherapy out patients
Recovery Rehab 4 weeks - 3 months[edit | edit source]
Restrictions:
- No strengthening against resistance until 3 months if any tendon transfers
- No stretching tendons if transferred
Goals:
- Independent from aircast boot
- Achieve full ROM
Treatment:
- Pain relief, swelling management
- Advice, education, postural advice, monitoring complications, pacing
- Gait re-education
- Exercises --> PROM,AAROM, AROM, light strengthening, core stability, balance/proprioception, stretching
- Hydrotherapy
- Orthotics
- Manual therapy --> SSTM's, mobilisations
Progress when:
Full ROM, independently mobile, neutral foot position in standing
Intermediate Rehab 12 weeks - 6 months[edit | edit source]
Restrictions:
- None
Goals:
- Independent with no aids
- Normal footwear
- Grade 5 strength
- Grade 4 strength in tendons transferred
Treatment:
- Pain relief, swelling management
- Advice, education, postural advice, monitoring complications, pacing
- Gait re-education
- Exercises --> PROM,AAROM, AROM, light strengthening, core stability, balance/proprioception, stretching
- Hydrotherapy
- Orthotics
- Manual therapy --> SSTM's, mobilisations
Progress when:
Normal footwear, independent with no aids, pain controlled, strength 5/5 (4/5 if tendon transferred)
Final Rehab 6 months - 1 year[edit | edit source]
Goals:
- Return to gentle no-impact/low impact sports
- Grade 5 strength in transferred tendons
Treatment:
- Maximise function
- End stage exercises, balance and proprioception and sport specific
- Manual therapy
Muscles to Consider[edit | edit source]
Here is a unfinished list of some of the major muscles of the lower leg and foot, consider these in your rehabilitation and mechanism of pathology. Some may have had tendons moved or stretched and now need to be specifically rehabilitated as the proprioceptive function may now have changed.
Posterior Compartment - Superficial[edit | edit source]
- Gastrocnemius
- Plantaris
- Soleus
Posterior Compartment - Deep[edit | edit source]
- Popliteus
- Flexor Hallucis Longus
- Flexor Digitorum Longus
- Tibialis Posterior
Lateral Compartment[edit | edit source]
- Peroneus Longus
- Peroneus Brevis
Anterior Compartment[edit | edit source]
- Tibialis Anterior
- Extensor Hallucis Longus
- Extensor Digitorum Longus
- Peroneus Tertius
Sample Exercises[edit | edit source]

|

|

|
| Balance c perturbation | Ball toss | Standing reach |

|

|

|
| Standing reach | Seated rocker board | DF theraband |

|

|

|
| Ankle eversion | DF stretch | Ankle PF |
Additional Information[edit | edit source]
After the surgery it is important that the patient keeps moving and performing his daily activities. However there is still discussion between physicians about when the patient should start again with exercising. There are some that allow exercise immediately after surgery. But some say it is considered best to wait until there is a satisfactory bony in growth as shown radio graphically. However it’s the job of the physician to try to improve: the patient’s ROM of the ankle, maintain the ROM in the hip and knee, increase the muscle strength with exercise for the Gluteus Maximus, Quadriceps femoris muscles and the muscles that are responsible for dorsal flexion and the plantar flexion of the ankle[48]. Postoperative mobilization begins early, with rapid progression to resumption of normal activities.[49] The goal is to obtain 10° of dorsal flexion and 30° of plantar flexion. For patients who have almost no motion in their ankle is any motion an improvement.[50]
In early postoperative period it is important that the incision heals and the implant becomes solidly fixed to the bony bed to do this they will use a below knee non-weight bearing immobilization. This is maintained until there is satisfactory bony in growth. [51]. Another goal is to increase the ROM of the ankle and maintain the hip and the knee ROM.
After a few months the patient needs to make an appointment with the doctor. Here they will take X-ray scans to see if there are no complications like: joint debridement for osseous impingement; the next most common procedures were extra-articular procedures for axial misalignments and component replacements.[52]
Prognosis & Outcome[edit | edit source]
Outcome of ankle arthroplasty includes pain, function implant survival and complications. There are numerous studies looking at survival rate of implants and rates are reported around 67-94% at 5 years[53][54][55] and 75% at ten years[53] which is reasonably reliable.
A systematic review of intermediate and long term outcomes of arthrolplasty and arthrodesis performed by Haddal et al[56] had interesting results. It reviewed 49 primary studies of 1262 patients and utilised the AOFAS score (Americal Orthopaedic Foot and Ankle Society). This score is out of 100 (0=worst outcome, 100=best outcome) broken into 8 sections of pain, function walking distance, walking surface, gait abnormality, sagittal mobility, hindfoot mobility, ankle hindfoot mobility and alignment. The score has mixed reviews and the objective aspect of the score is hard to make reliable between therapists[57].
The mean AOFAS score was 78.2 points for the patients treated with total ankle arthroplasty and 75.6 points for those treated with arthrodesis. Meta-analytic mean results showed 38% of the patients treated with total ankle arthroplasty had an excellent result, 30.5% had a good result, 5.5% had a fair result, and 24% had a poor result. In the arthrodesis group, the corresponding values were 31%, 37%, 13%, and 13%. The five-year implant survival rate was 78% and the ten-year survival rate was 77%. The revision rate following total ankle arthroplasty was 7% with the primary reason for the revisions being loosening and/or subsidence (28%). The revision rate following ankle arthrodesis was 9% , with the main reason for the revisions being nonunion (65%). One percent of the patients who had undergone total ankle arthroplasty required a below-the-knee amputation compared with 5% in the ankle arthrodesis group. Their conclusion was that on the basis of these findings,
"the intermediate outcome of total ankle arthroplasty appears to be similar to that of ankle arthrodesis; however, data were sparse. Comparative studies are needed to strengthen this conclusion"[56].
Resources
[edit | edit source]
| [58] | [59] |
| [60] | [61] |
References[edit | edit source]
- ↑ Ankle Replacement Surgery. Annals of the Royal College of Surgeons of England. 2006 July;88(4):417-418
- ↑ Ankle Replacement Surgery. Annals of the Royal College of Surgeons of England. 2006 July;88(4):417-418
- ↑ http://www.medicalnewstoday.com/articles/11222.php
- ↑ http://www.medicalnewstoday.com/articles/11222.php
- ↑ Cerrato R, Myerson MS. Total Ankle Replacement:the Agility LP prosthesis. Foot and Ankle Clin. 2008 Sept; 13(3): 485-94.
- ↑ http://medicalnewstoday.com/printerfriendlynews.php?newsid=151776
- ↑ Haddad SL, Coetzee JC, Estok R. et al. Intermediate and Long-Term Outcomes of Total Ankle Arthroplasy and Ankle Arthrodesis. The Journal of Bone and Joint Surgery (American). 2007;89:1899-1905.
- ↑ SooHoo NF, Zingmond DS, Ko CY. Comparison of Reoperation Rates Following Ankle Arthrodesis and Total Ankle Arthroplasty. The Journal of Bone and Joint Surgery (American). 2007;89:2143-2149.
- ↑ Knecht SI, Estin M, Callaghan JJ et al. The Agility Total Ankle Arthroplasty: Seven to Sixteen-Year Follow-up. The Journal of Bone and Joint Surgery (American). 2004;86:1161-1171.
- ↑ Cracchiolo A 3rd, Deorio JK. Design features of current total ankle replacements: implants and instrumentation. Journal of the American Academy of Orthopedic Surgeons. 2008 Sept:16(9):530-40.
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 11.12 Cook R.A., O’Malley M.J. Total Ankle Arthroplasty. Orthop Nurs. 2001;20(4): 30-37.
- ↑ Doets, C., Brand, R., Nelissen, R. Total Ankle Arthroplasty in Inflammatory Joint Disease with Use of Two Mobile-Bearing Designs. The Journal of Bone and Joint Surgery. 2006;88:1274-1284.
- ↑ Haddad, S. et all. Arthroplasty vs Arthrodesis: Intermediate and Long-Term Outcomes of Total Ankle Arthroplasty and Ankle Arthrodesis A Systematic Review of the Literature. The Journal of Bone and Joint Surgery. 2007;89:1899-1905.
- ↑ MURNAGHAN J.M., WARNOCK D.S., HENDERSON S.A.., ‘Total Ankle Replacement: Early experience with STAR prothesis’, The Ulster Medical Journal, 2005, May, vol. 74, nr. 1, p. 9-13
- ↑ SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306
- ↑ SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 17.8 17.9 Saltzman, C.L., McIff, T.E., Buckwalter, J.A., Brown, T.D. Total Ankle Replacement Revisited. JOSPT. 2000;30: 56-67. Cite error: Invalid
<ref>tag; name "Saltzman, CL" defined multiple times with different content - ↑ 18.0 18.1 Goodman, C., Snyder, T. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th ed. St. Louis: Saunders Elsevier, 2009.
- ↑ 19.0 19.1 19.2 19.3 19.4 Bonasia DE. Dettoni F. Femino JE. Phisitkul P. Germano M. Amendola A. Total Ankle Replacement: When, Why and How? The Iowa Orthopaedic Journal 2010(30)119-130
- ↑ 20.0 20.1 Gill. LH. Challenges in Total Ankle Arthroplasty. Foot Ankle Int. 2004;25(4):195-207.
- ↑ 21.0 21.1 21.2 21.3 21.4 Guyer, A.J., Richardson, E.G. Current Concepts Review: Total Ankle Arthroplasty. Foot Ankle Int. 2008;29(2): 256-264.
- ↑ Cracchiolo A. III, Deorio, J.K. Design features of current total ankle replacements: implants and instrumentation. J Am Acad Orthop Surg. 2008;16(9):530-540.
- ↑ Pfeiff C. The Scandinavian Total Ankle Replacement (STAR). Orthop Nurs. 2006; 25(1): 30-33.
- ↑ Herr, Mark. otal Ankle Replacement with Dr. Mark Herr [Video]. YouTube. http://www.youtube.com/watch?v=8GJl4BD-xzM. Published Jan 19, 2010. Accessed July 11, 2011.
- ↑ Grawe JS. Mirow L. Bouchard R. Lindig M. Huppe M. Impact of preoperative patient education on postoperative pain in consideration of individual coping style. Schmerz 2010;24(6):575-86
- ↑ SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306
- ↑ Neligan, Patrick. Anesthesiology Clin. 2013:30; 495-511
- ↑ Neligan, Patrick. Anesthesiology Clin. 2013:30; 495-511
- ↑ Tusman, Gerardo, et al. Curr Opin Anesthesiol 2012:25;1-10
- ↑ Royal National Orthopaedic Hospital NHS Trust. Physiotherapy Rehabilitation Guidelines - Total Ankle Replacement Surgery. [ONLINE] available from: http://www.rnoh.nhs.uk/sites/default/files/downloads/physiotherapy_rehabilitation_guidelines_-_total_ankle_replacement_surgery.doc accessed [26/05/2014]
- ↑ Ali et al. Intermediate results of Buechel Pappas unconstrained total ankle replacement for osteoarthritis. The journal of foot and ankle surgery. 2007;46(1):16-20
- ↑ Buechel at al. Twenty-year evaluation of cementless mobile-bearing total ankle replacements. clinical othopaedics and related research. 2004;424:19-26
- ↑ Coetzee J. Caatro M. Accurate measurement of ankle range of motion after total ankle arthroplasty. Clinical orthopaedics and related research. 2004 27-31
- ↑ Conti S. Wong YS. Complications of total ankle replacements. Clinical orthopaedics and related research. 2001;391:105-114
- ↑ Knecht et al. The agility of total ankle arthroplasty. The journal of bone and joint surgery. 2004 1161-1171
- ↑ Kontis et al. The management of failed ankle replacement. The jounrla of bone and joint surgery. 2006 1039-1047
- ↑ Lagaay PM, Schuberth JM. Analysis of Ankle Range of Motion and Functional Outcome Following Total Ankle Arthoplasty. The Journal of Foot and Ankle Surgery. 2010: Iss. 49, 147-151.
- ↑ Gougoulias N, Khanna A, Maffulli N. How Successful are Current Ankle Replacements?: A Systematic Review of the Literature. Clinical Orthopaedics and Related Research. Clin Orthop Relat Res. Jan 2010: 199-208.
- ↑ Buechel FF Sr, Buechel FF Jr, Pappas MJ. Twenty- year evaluation of cementless mobile-bearing total ankle replacements. Department of Orthopaedic Surgery New Jersey Medical School. Jul 2004: 19-26.
- ↑ Bonnin M, Judet T, Colombier JA, Buscayret JA, Graveleau N, Piriou P. Midterm results of the Salto Total Ankle Prosthesis. Clin Orthop Relat Res. Jul 2004: 6-18.
- ↑ 41.0 41.1 Lee KB, Park YH, Song EK, Yoon TR, Jung KI. Static and dynamic postural balance after successful mobile-bearing total ankle arthroplasty. Arch Phys Med Rehabil. Apr 2010: 519-522.
- ↑ Culham EG, Westlake KP, Wu Y. Sensory-specific balance training in older adults: effect on position, movement, and velocity sense at the ankle. Phys Ther. May 2007: 560-568.
- ↑ Detrembleur C. Leemrijse T. The effects of total ankle replacement on gait disability: analysis of energetic and mechanical variables. Gait Posture. Feb 2009. 270-274.
- ↑ 44.0 44.1 44.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedHuber - ↑ San Giovanni T.P., Keblish D.J., Thomas W.H., Wilson M.G. Eight-year results of a minimally constrained total ankle arthroplasty. Foot Ankle Int. 2006;27(6):418-426
- ↑ Valderrabano V., Nigg B.M., von Tscharner V., Frank C.B., Hintermann B. Total ankle replacement in ankle osteoarthritis: an analysis of muscle rehabilitation. Foot Ankle Int. 2007;28(2):281-291.
- ↑ Dyrby C., Chou L.B., Andriacchi T.P., Mann R.A. Functional evaluation of the Scandinavian Total Ankle Replacement. Foot Ankle Int.2004;25(6):377-381.
- ↑ SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306.
- ↑ SMITH C.L., L.T., M.S.C., U.S.N., ‘Physical therapy management of patients with total ankle replacement’, Physical Therapy, 1980, March, vol. 60, nr. 8, p. 303-306.
- ↑ SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67
- ↑ SALTZMAN C.L., MCLFF T.E., BUCKWALTER J.A., BROWN T.D., ‘Total Ankle Replacement revisited’, Journal of Orthopaedic &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Sports Physical Therapy, 2000, February, vol.nr. 30(2), p. 56-67
- ↑ ADRIENNE A. SPIRT, MATHIEU ASSAL, SIGVARD T. HANSEN Jr., ‘Complications and Failure After Total Ankle Arthroplasty’, The Journal of Bone and Joint Surgery, 2004, June, vol. 86-A, nr. 6, p.1172-1178
- ↑ 53.0 53.1 Haddad, S.L.; Coetzee, J.C.; Estok, R.; Fahrbach, K.; Banel, D.; Nalysnyk, L. (2007). "Intermediate and Long-Term Outcomes of Total Ankle Arthroplasty and Ankle Arthrodesis. A Systematic Review of the Literature". Journal of Bone and Joint Surgery 89A (9): 1899–905
- ↑ Stengel, Dirk; Bauwens, Kai; Ekkernkamp, Axel; Cramer, Jörg (2005). "Efficacy of total ankle replacement with meniscal-bearing devices: a systematic review and meta-analysis". Archives of Orthopaedic and Trauma Surgery 125 (2): 109–19
- ↑ Gougoulias, Nikolaos; Khanna, Anil; Maffulli, Nicola (2009). "How Successful are Current Ankle Replacements? All though most total ankle replacement are successful by reducing pain and improving mobility there is a very high possibility that the pain may be ten times worse. There have been several cases where the doctors have recommended amputation to resolve the issue of pain that was not there prior to the total ankle replacement. : A Systematic Review of the Literature". Clinical Orthopaedics and Related Research 468: 199–208.
- ↑ 56.0 56.1 Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007 Sep;89(9):1899-905.
- ↑ Madeley NJ1, Wing KJ, Topliss C, Penner MJ, Glazebrook MA, Younger AS.Responsiveness and validity of the SF-36, Ankle Osteoarthritis Scale, AOFAS Ankle Hindfoot Score, and Foot Function Index in end stage ankle arthritis. Foot Ankle Int. 2012 Jan;33(1):57-63
- ↑ Dr Selene Parekh Ankle Replacement Surgery https://www.youtube.com/channel/UCxqRUzmxviIRrz3MBt6Xxew [Accessed 24/05/2014]
- ↑ Dr Selene Parekh Ankle Replacement Surgery https://www.youtube.com/channel/UCxqRUzmxviIRrz3MBt6Xxew [Accessed 24/05/2014]
- ↑ Dr Selene Parekh Ankle Replacement Surgery https://www.youtube.com/channel/UCxqRUzmxviIRrz3MBt6Xxew {Accessed 24/05/2014]
- ↑ Total Ankle Replacement Surgery educational video. Available from https://www.youtube.com/watch?v=JGjyRJNWAbA [Accessed 24/05/2014]fckLR|}






