Thoracic Disc Syndrome: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Fear‐Avoidance Belief Questionnaire" to "[[Fear Avoidance Belief Questionnaire") |
||
| (44 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- '''Original Editor '''- [[User:Sarah Harnie|Sarah Harnie]] | |||
{ | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | ||
== Definition/Description == | == Definition/Description == | ||
[[File:Sam-burriss-zHSX9o2 B7Y-unsplash.jpg|right|frameless]] | |||
Symptomatic thoracic discogenic pain syndrome (TDPS) is a rare phenomenon making it challenging to diagnose. The rarity of TDPS is attributed to the particular orientation, structure, and function of the thoracic spine in the vertebral column. | |||
* The lordotic nature of the cervical and lumbar spine allows the imaginary line of gravity to run through, allowing them to bear most of the weight of the of the axial skeleton as compared to the thoracic and sacral spine. | |||
* Consequently, they are subject to a higher percentage of degenerated discs and subsequent discogenic pain syndrome. | |||
The majority of the thoracic disc herniation is asymptomatic, or the patient presents with nonspecific symptoms like chest wall pain, epigastric pain, upper extremity pain, and sometimes, a pain in the groin or the lower extremity. | |||
* While the rare nature, coupled with the atypical presentation, may lead to delay in diagnosis. | |||
* Treatment of thoracic discogenic pain syndrome is conservative but sometimes surgical. Surgical interventions, with surgical intervention associated with many complications<ref name=":3" />. | |||
The | == Pathophysiology == | ||
[[Thoracic Anatomy|Thoracic]] discogenic pain syndrome may be a radicular or myelopathic pain. | |||
* The radicular pain is mostly secondary to posterolateral herniations that compress spinal nerves as they exit through the intervertebral foramen. Radicular pain will usually radiate towards the dermatome of the nerve roots innervated by the exiting nerve. | |||
* Myelopathic pain is seen in central herniations. The herniated disc compresses the spinal cord, leading to sensory and/or motor problems in the corresponding compressed area and below. This is particularly more severe in the thoracic spinal cord since the spinal canal in this region is smaller compared to the cervical and lumbar region. Hence, a slight compression will lead to symptoms<ref name=":3" />. | |||
== | == Etiology == | ||
Intervertebral disc degeneration primarily causes thoracic discogenic pain syndrome. | |||
Thoracic disc lesions are primarily degenerative of nature and affect mostly the lower part of the thoracic spine. Three quarters of incidence occurs below T8, with T11-T12 being most common. The exact cause of disc degeneration is believed to be multifactorial, factors that can attribute include: | |||
* Trauma | |||
* Metabolic abnormalities | |||
* Genetic predisposition | |||
* Vascular problems | |||
* Infections | |||
The effects of trauma as previously mentioned is less devasting on the thoracic spine as compared to the cervical and lumbar spine because the thoracic spine participates in less weight-bearing activities and the rib cage and coronal orientation of the facet joints make it more stable, hence less prone to degenerative disc disease. With trauma, chronic overload from the lifting of heavy objects or chronic multi-trauma from individuals participating in sports leads to the repeated rotation of the axial spine, causing vertebral instability with alteration of the of the spinal alignment that accelerates the risk of developing disc degeneration.<ref name=":3">Fogwe DT, Zulfiqar H, Mesfin FB. [https://www.ncbi.nlm.nih.gov/books/NBK470388/ Thoracic Discogenic Syndrome]. InStatPearls [Internet] 2019 Jun 25. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK470388/ (last accessed 2.5.2020)</ref> | |||
== Epidemiology == | |||
Why clinically significant thoracic disc disease is less common, has essentially two causes: | |||
* As opposed to the cervical or lumbar spine, the intervertebral foramina of the thoracic spine are located at the level of the body, as opposed to directly behind the discs. | |||
* There is relatively little movement in the thoracic motion segments, so the anatomical relationship of neural structures to their surroundings remains constant. | |||
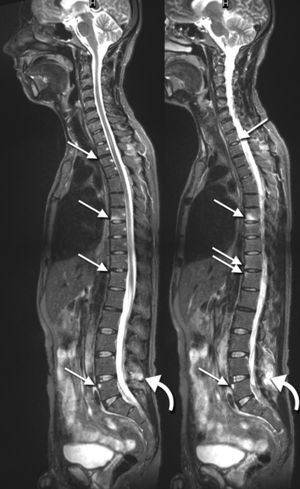
[[File:MRI HTML.jpg|right|frameless]] | |||
Thoracic disc herniation is rare and usually asymptomatic. | |||
Often found incidentally with MRI. | |||
< | Herniation of the intervertebral disc in the thoracic region makes up: | ||
* 0.5% to 4.5% of all disc ruptures | |||
* 0.25-0.75 of all symptomatic disc herniation | |||
* 0.15% and 1.8% of all surgically-treated herniations.<ref name=":3" /> | |||
About 80% of patients usually present with problems in the third or fourth decades of life. | |||
= | About 75% incidence occurs below the T8 with a peak around the T11 to T12 and about 63% are symptomatic and have an incidence of one in one million. | ||
* Note - in acquired deformities of the spine eg [[scoliosis]], [[Scheuermanns Disease|Scheuermann]] disease (which develop gradually) the nerve roots to adapt to the situation not necessarily causing thoracic syndrome.<ref name="p1">Juergen Kraemer, 2009, Intervertebral Disk Diseases: Causes, Diagnosis, Treatment and Prophylaxis , Thieme , Stuttgart, 375p. </ref> | |||
=== Characteristics/Clinical Presentation === | |||
* The majority of the thoracic disc herniation are asymptomatic and are discovered incidentally with an [[MRI Scans|MRI]]. | |||
* Unlike the lumbar and cervical disc herniations, thoracic disc herniations have atypical symptoms and often a diagnosis of exclusion. | |||
* To accurately diagnose thoracic discogenic pain syndrome, a thorough history and physical examination should be done. As part of the patient's pain evaluation, assessment of the quality, intensity, distribution, alleviating, and aggravating factors is essential. | |||
* Degenerative thoracic syndromes can be classified as local, radicular (intercostal neuralgia) or pseudoradicular. | |||
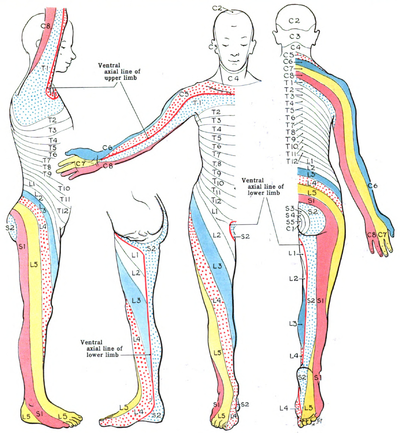
Patients with thoracic disc herniations may either present with a radicular and/or myelopathic pain depending on if the herniated disc compresses the nerve roots or the spinal cord itself, respectively. [[File:Dermatomes Grant.png|right|frameless|433x433px]]With radicular pain, the patients will have pain that follows the dermatomal distribution. | |||
Essential landmarks for thoracic disc herniations to help with assessment include | |||
* T-1 pain that radiates to the medial forearm, | |||
* T-2 pain that radiates to the axilla, | |||
* T-4 pain that radiates to the nipple area, | |||
* T-10 pain that radiates to the umbilicus | |||
* T-12 pain that is just above the inguinal ligaments. | |||
The most common initial pain is usually thoracic pain occurring in the midline area. | |||
The pain may be: | |||
* unilateral or bilateral depending on the location and how significant the herniation is. | |||
* intermittent and aggravated by coughing and straining. | |||
* In rare cases, radiation to the groin, flank, and even the lower extremities<ref name=":3" />. | |||
In upper thoracic and lateral disc herniations | |||
* Radicular pain is more common and often reported in combination with some amount of axial pain. | |||
* Sensory changes (e.g. parenthesias, dysesthesia) below the level of the lesion. | |||
* Other symptoms include bladder and bowel dysfunction (15-20% of patients), hyperreflexia and gait impairment.<ref name="p1" /><ref name=":0">Vanichkachorn JS, Vaccaro AR. [https://journals.lww.com/jaaos/Fulltext/2000/05000/Thoracic_Disk_Disease__Diagnosis_and_Treatment.3.aspx Thoracic disk disease: diagnosis and treatment]. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2000 May 1;8(3):159-69.</ref> | |||
[[Red Flags in Spinal Conditions|Red flags]] one should be aware of are: | |||
* Myelopathy (injury to the spinal cord due to severe compression) | |||
* Gait disturbance | |||
* Paralysis | |||
* Cardiovascular disturbances | |||
* History of:Cancer; Trauma; Tumor; Infection; Constitutional symptoms (feeling ill); Weight loss; Laboratory abnormalities | |||
<ref name=" | |||
<ref name=" | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Thoracic disc | Thoracic disc syndrome are relatively rare | ||
* Symptoms in this area will more likely arouse suspicion of disease of the internal organs/ primary disorder of the nervous system. | |||
* Important that the patient is examined thoroughly to rule out all other causes for symptoms.<ref name="p1" /><ref name=":0" /><ref name=":3" /> | |||
Rule out conditions such as | |||
* [[Diabetes]] and shingles | |||
* Other mechanical issues such as oblique muscle pain, [[Rib stress fracture in rowers|rib fracture]], [[fracture]] of the [[Facet Joint Syndrome|facet joints]] and clavicle | |||
* Malignancies, like neurofibroma | |||
* Herpes zoster (can cause segmentally radiating pain with postherpetic [[Neuropathic Pain|neuralgia]]) | |||
* Costotransverse joint syndrome due to inflammatory changes or arthrosis | |||
* Infections, tumors and dilated arteries of the chest wall | |||
* [[Referred Pain|Referred pain]] from the organs (zones of Head) | |||
* [[Tietzes|Tietze syndrome]] | |||
* [[Scheuermann's Kyphosis|Scheuermann kyphosis]] | |||
Pain referred around the chest wall tends to be costovertebral in origin.<ref name=":4">Magee, D. J. (2008). Orthopedic physical assessment. St. Louis, Mo: Saunders Elsevier. Print</ref> | |||
== Physical examination == | |||
Start your examination with: | |||
* History eg Chronic or acute, Specific inciting incident, Location of the pain and its radiation, The character of the pain and aggravating activities including static and dynamic load. | |||
* Observation (standing) Examination | |||
* Assessment of sensation with pinprick and touch in the upper extremity, thorax, and abdomen in the dermatomal regions mentioned above to check for radiculopathy and also in the lower extremity to check for myelopathy. | |||
* Active movements (standing or sitting) - Forward flexion - Extension - Side flexion (left and right) - Rotation (left and right) - Combined movements (if necessary) - Repetitive movements (if necessary) - Sustained postures (if necessary) | |||
* Passive movements (sitting) - Forward flexion - Extension - Side flexion (left and right) - Rotation (left and right) - Resisted isometric movements (sitting) - Forward flexion - Extension - Side flexion (left and right) - Rotation (left and right) | |||
* Functional assessment | |||
* Special tests (sitting) - [[Adsons Test|Adson’s test]] - [[Costoclavicular (Military) Brace Test|Costoclavicular maneuver]] - Hyperabduction (EAST) test - [[Roos Stress Test|Roos test]] - [[Slump Test|Slump test]] | |||
* Reflexes and cutaneous distribution (sitting) - [[Reflexes|Reflex testing]] - Sensation scan | |||
* Special tests (prone lying) - Joint play movements (prone lying) - Posteroanterior central vertebral pressure (PACVP) - Posteroanterior unilateral vertebral pressure (PAUVP) - Transverse vertebral pressure (TVP) - Rib springing - Palpation (prone lying) | |||
* Special tests (supine lying) - First rib mobility - Rib springing - [[Upper Limb Tension Tests (ULTTs)|Upper limb neurodynamic (tension) test 4]] (ULNT4) - Palpation (supine lying) - Federung test (segmental translation of the thoracic vertebrea) | |||
* Sensitivity of the thorax and stomach | |||
After any assessment, the patient should be warned of the possibility of exacerbation of symptoms as a result of assessment.<ref name=":4" /> | |||
'''Elaboration on some testing''' | |||
Assess passive movements of the thoracic spine and the end feel:<ref name=":4" /> | |||
• Forward flexion (tissue stretch) | |||
• Extension (tissue stretch) | |||
• Side flexion, left and right (tissue stretch) | |||
• Rotation, left and right (tissue stretch) | |||
Pain provocation by performing passive movements, in particular rotation, forward flexion, backward flexion and lateral flexion can indicate a spinal aetiology. | |||
Sensory symptoms can be present if the patient has a thoracic disc herniation. It can cause altered sensation to light touch or pinprick along a dermatomal pattern. Cord compression and myelopathy should be strongly considered if a sensory level is established such that sensation is consistently altered below a specific dermatome. | |||
== | Provocative manoeuvres such as the Spurling manoeuvre (cervical radiculopathy) and the Straight-Leg Raise test or the Slump Test (lumbosacral radiculopathy) may exclude a thoracic disc syndrome.<ref name="p1" /><ref name="p9">Shirzadi A, Drazin D, Jeswani S, Lovely L, Liu J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3638501/ Atypical presentation of thoracic disc herniation: case series and review of the literature]. Case reports in orthopedics. 2013;2013.</ref><ref name="p0">Deitch K, Chudnofsky C, Young M. [https://www.ncbi.nlm.nih.gov/pubmed/17976778 T2–3 Thoracic Disc Herniation with Myelopathy]. The Journal of emergency medicine. 2009 Feb 1;36(2):138-40. </ref> /> | ||
Thoracic | You can also take a look at [[Thoracic Examination]] on Physiopedia. | ||
=== Evaluation === | |||
In addition to a detailed neurological examination, an MRI of the thoracic spine is very sensitive and specific for diagnosing thoracic disc herniation[10]. In some situations, thoracic discography can be performed to confirm the pain being of discogenic origin being that most thoracic discogenic syndrome can be asymptomatic<ref name=":3" /> | |||
== Outcome measures == | |||
* [[Occiput to Wall Distance OWD|Occiput to Wall]] Distance | |||
* [[Visual Analogue Scale|VAS-pain scale]] | |||
* [[Pain Catastrophizing Scale]] | |||
* [[Fear Avoidance Belief Questionnaire|Fear-avoidance Beliefs Questionnaire]] | |||
* [[Patient Specific Functional Scale]] | |||
* [[Fingertips to Floor Distance - Special Test|Fingertips to Floor]] | |||
=== Medical Management === | |||
The initial treatment of thoracic discogenic syndrome is usually conservative (nonoperational) since some disc herniations have been reported to stabilize/regress with time, especially in younger patients. | |||
== Medical Management | * Conservative management includes rest, [[Pain Medications|anti-inflammatory drugs]], and physical therapy. | ||
* Drugs like Pregabalin have been reported to be useful for the numbness and radicular pain. | |||
* Selective spinal root or intercostal nerve blockade and [[Therapeutic Corticosteroid Injection|epidural steroids injections]] can also be used to treat radicular pain. | |||
* Surgical intervention is considered as a last resort for the treatment of symptomatic thoracic disc herniations with patients unresponsive to conservative treatment.<ref name=":3" /> | |||
Surgical | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
[[File:Massage image.jpg|right|frameless]] | |||
Several guidelines recommend physical exercise to alleviate pain. The goal of physiotherapy should be to increase the range of motion and pain relief, using a multiple-exercise based approach to strengthen supporting muscles and postural support.<ref name="p0" /><ref name=":7">Manchikanti L, Hirsch JA. [https://www.ncbi.nlm.nih.gov/pubmed/25982996 Clinical management of radicular pain.] Expert review of neurotherapeutics. 2015 Jun 3;15(6):681-93.</ref> Animal model studies show that physical exercise helps in intravertebral disk proliferation, particularly in moderate to high volume low repetition and frequency exercises.<ref>Luan S, Wan Q, Luo H, Li X, Ke S, Lin C, Wu Y, Wu S, Ma C. [https://www.ncbi.nlm.nih.gov/pubmed/25607736 Running exercise alleviates pain and promotes cell proliferation in a rat model of intervertebral disc degeneration.] International journal of molecular sciences. 2015 Jan;16(1):2130-44.</ref><ref>Steele J, Bruce-Low S, Smith D, Osborne N, Thorkeldsen A. [https://www.ncbi.nlm.nih.gov/pubmed/26409630 Can specific loading through exercise impart healing or regeneration of the intervertebral disc?.] The Spine Journal. 2015 Oct 1;15(10):2117-21.</ref> Most patients (80%) with a prolapsed intervertebral disc respond in 4-6 weeks to conservative therapy.<ref>Hofstee DJ, Gijtenbeek JM, Hoogland PH, van Houwelingen HC, Kloet A, Lötters F, Tans JT. [https://www.ncbi.nlm.nih.gov/pubmed/11797655 Westeinde sciatica trial: randomized controlled study of bed rest and physiotherapy for acute sciatica.] Journal of Neurosurgery: Spine. 2002 Jan 1;96(1):45-9.</ref><ref>Weber H, Holme I, Amlie E. [https://www.ncbi.nlm.nih.gov/pubmed/8235813 The natural course of acute sciatica with nerve root symptoms in a double-blind placebo-controlled trial evaluating the effect of piroxicam]. Spine. 1993 Sep;18(11):1433-8..</ref> | |||
Mechanical strain on the disc can be reduced by horizontal positioning, although bedrest is usually not indicated. The application of heat can bring relief by relaxing the reflexive tension of the thoracic musculature, particularly the paravertebral extensors of the trunk and by promoting circulation.<ref name="p1" /> | |||
Some ideas from Physiopedia for physical therapy treatment: | |||
* [[Exercise in Pain Management|Exercise in pain management]] | |||
* [https://www.physiospot.com/opinion/my-top-3-thoracic-spine-mobility-exercises/ Top 3 thoracic spine mobility exercises] (Physiospot) | |||
* [[Thoracic Manual Techniques and Exercises]] | |||
== Case Studies == | == Case Studies == | ||
# [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5131583/ Unusual chest wall pain caused by thoracic disc herniation in a professional baseball pitcher] | |||
# [https://www.ncbi.nlm.nih.gov/pubmed/26156777?log$=activity Histologically proven acute paediatric thoracic disc herniation causing paraparesis] | |||
# [https://www.ncbi.nlm.nih.gov/pubmed/19404165 Acute chest pain in a top soccer player due to thoracic disc herniation] | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
* [[File:Thoracic manip.JPG|right|frameless]]Thoracic discogenic pain syndrome (TDPS) is rare making it challenging for the healthcare team to diagnose and treat the condition. | |||
* The rarity of TDPS is attributed to the particular orientation, structure, and function of the thoracic spine in the vertebral column. | |||
* Despite this rarity, physiotherapists, physician assistants, and physicians should be familiar with its diagnosis and treatment and work as an interprofessional team to provide treatment<ref name=":3" /> | |||
* Physical therapy should be focussed on increasing the range of motion and pain relief, using a multiple-exercise based approach to strengthen muscles and postural support.<ref name="p0" /> <ref name=":7" /><br> | |||
Thoracic | == References == | ||
<references /> | |||
[[Category:Thoracic Spine]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Primary Contact]] | |||
[[Category:Syndromes]] | |||
[[Category:Conditions]] | |||
[[Category:Thoracic Spine - Conditions]] | |||
Latest revision as of 12:30, 17 October 2023
Definition/Description[edit | edit source]
Symptomatic thoracic discogenic pain syndrome (TDPS) is a rare phenomenon making it challenging to diagnose. The rarity of TDPS is attributed to the particular orientation, structure, and function of the thoracic spine in the vertebral column.
- The lordotic nature of the cervical and lumbar spine allows the imaginary line of gravity to run through, allowing them to bear most of the weight of the of the axial skeleton as compared to the thoracic and sacral spine.
- Consequently, they are subject to a higher percentage of degenerated discs and subsequent discogenic pain syndrome.
The majority of the thoracic disc herniation is asymptomatic, or the patient presents with nonspecific symptoms like chest wall pain, epigastric pain, upper extremity pain, and sometimes, a pain in the groin or the lower extremity.
- While the rare nature, coupled with the atypical presentation, may lead to delay in diagnosis.
- Treatment of thoracic discogenic pain syndrome is conservative but sometimes surgical. Surgical interventions, with surgical intervention associated with many complications[1].
Pathophysiology[edit | edit source]
Thoracic discogenic pain syndrome may be a radicular or myelopathic pain.
- The radicular pain is mostly secondary to posterolateral herniations that compress spinal nerves as they exit through the intervertebral foramen. Radicular pain will usually radiate towards the dermatome of the nerve roots innervated by the exiting nerve.
- Myelopathic pain is seen in central herniations. The herniated disc compresses the spinal cord, leading to sensory and/or motor problems in the corresponding compressed area and below. This is particularly more severe in the thoracic spinal cord since the spinal canal in this region is smaller compared to the cervical and lumbar region. Hence, a slight compression will lead to symptoms[1].
Etiology[edit | edit source]
Intervertebral disc degeneration primarily causes thoracic discogenic pain syndrome.
Thoracic disc lesions are primarily degenerative of nature and affect mostly the lower part of the thoracic spine. Three quarters of incidence occurs below T8, with T11-T12 being most common. The exact cause of disc degeneration is believed to be multifactorial, factors that can attribute include:
- Trauma
- Metabolic abnormalities
- Genetic predisposition
- Vascular problems
- Infections
The effects of trauma as previously mentioned is less devasting on the thoracic spine as compared to the cervical and lumbar spine because the thoracic spine participates in less weight-bearing activities and the rib cage and coronal orientation of the facet joints make it more stable, hence less prone to degenerative disc disease. With trauma, chronic overload from the lifting of heavy objects or chronic multi-trauma from individuals participating in sports leads to the repeated rotation of the axial spine, causing vertebral instability with alteration of the of the spinal alignment that accelerates the risk of developing disc degeneration.[1]
Epidemiology[edit | edit source]
Why clinically significant thoracic disc disease is less common, has essentially two causes:
- As opposed to the cervical or lumbar spine, the intervertebral foramina of the thoracic spine are located at the level of the body, as opposed to directly behind the discs.
- There is relatively little movement in the thoracic motion segments, so the anatomical relationship of neural structures to their surroundings remains constant.
Thoracic disc herniation is rare and usually asymptomatic.
Often found incidentally with MRI.
Herniation of the intervertebral disc in the thoracic region makes up:
- 0.5% to 4.5% of all disc ruptures
- 0.25-0.75 of all symptomatic disc herniation
- 0.15% and 1.8% of all surgically-treated herniations.[1]
About 80% of patients usually present with problems in the third or fourth decades of life.
About 75% incidence occurs below the T8 with a peak around the T11 to T12 and about 63% are symptomatic and have an incidence of one in one million.
- Note - in acquired deformities of the spine eg scoliosis, Scheuermann disease (which develop gradually) the nerve roots to adapt to the situation not necessarily causing thoracic syndrome.[2]
Characteristics/Clinical Presentation[edit | edit source]
- The majority of the thoracic disc herniation are asymptomatic and are discovered incidentally with an MRI.
- Unlike the lumbar and cervical disc herniations, thoracic disc herniations have atypical symptoms and often a diagnosis of exclusion.
- To accurately diagnose thoracic discogenic pain syndrome, a thorough history and physical examination should be done. As part of the patient's pain evaluation, assessment of the quality, intensity, distribution, alleviating, and aggravating factors is essential.
- Degenerative thoracic syndromes can be classified as local, radicular (intercostal neuralgia) or pseudoradicular.
Patients with thoracic disc herniations may either present with a radicular and/or myelopathic pain depending on if the herniated disc compresses the nerve roots or the spinal cord itself, respectively.
With radicular pain, the patients will have pain that follows the dermatomal distribution.
Essential landmarks for thoracic disc herniations to help with assessment include
- T-1 pain that radiates to the medial forearm,
- T-2 pain that radiates to the axilla,
- T-4 pain that radiates to the nipple area,
- T-10 pain that radiates to the umbilicus
- T-12 pain that is just above the inguinal ligaments.
The most common initial pain is usually thoracic pain occurring in the midline area.
The pain may be:
- unilateral or bilateral depending on the location and how significant the herniation is.
- intermittent and aggravated by coughing and straining.
- In rare cases, radiation to the groin, flank, and even the lower extremities[1].
In upper thoracic and lateral disc herniations
- Radicular pain is more common and often reported in combination with some amount of axial pain.
- Sensory changes (e.g. parenthesias, dysesthesia) below the level of the lesion.
- Other symptoms include bladder and bowel dysfunction (15-20% of patients), hyperreflexia and gait impairment.[2][3]
Red flags one should be aware of are:
- Myelopathy (injury to the spinal cord due to severe compression)
- Gait disturbance
- Paralysis
- Cardiovascular disturbances
- History of:Cancer; Trauma; Tumor; Infection; Constitutional symptoms (feeling ill); Weight loss; Laboratory abnormalities
Differential Diagnosis[edit | edit source]
Thoracic disc syndrome are relatively rare
- Symptoms in this area will more likely arouse suspicion of disease of the internal organs/ primary disorder of the nervous system.
- Important that the patient is examined thoroughly to rule out all other causes for symptoms.[2][3][1]
Rule out conditions such as
- Diabetes and shingles
- Other mechanical issues such as oblique muscle pain, rib fracture, fracture of the facet joints and clavicle
- Malignancies, like neurofibroma
- Herpes zoster (can cause segmentally radiating pain with postherpetic neuralgia)
- Costotransverse joint syndrome due to inflammatory changes or arthrosis
- Infections, tumors and dilated arteries of the chest wall
- Referred pain from the organs (zones of Head)
- Tietze syndrome
- Scheuermann kyphosis
Pain referred around the chest wall tends to be costovertebral in origin.[4]
Physical examination[edit | edit source]
Start your examination with:
- History eg Chronic or acute, Specific inciting incident, Location of the pain and its radiation, The character of the pain and aggravating activities including static and dynamic load.
- Observation (standing) Examination
- Assessment of sensation with pinprick and touch in the upper extremity, thorax, and abdomen in the dermatomal regions mentioned above to check for radiculopathy and also in the lower extremity to check for myelopathy.
- Active movements (standing or sitting) - Forward flexion - Extension - Side flexion (left and right) - Rotation (left and right) - Combined movements (if necessary) - Repetitive movements (if necessary) - Sustained postures (if necessary)
- Passive movements (sitting) - Forward flexion - Extension - Side flexion (left and right) - Rotation (left and right) - Resisted isometric movements (sitting) - Forward flexion - Extension - Side flexion (left and right) - Rotation (left and right)
- Functional assessment
- Special tests (sitting) - Adson’s test - Costoclavicular maneuver - Hyperabduction (EAST) test - Roos test - Slump test
- Reflexes and cutaneous distribution (sitting) - Reflex testing - Sensation scan
- Special tests (prone lying) - Joint play movements (prone lying) - Posteroanterior central vertebral pressure (PACVP) - Posteroanterior unilateral vertebral pressure (PAUVP) - Transverse vertebral pressure (TVP) - Rib springing - Palpation (prone lying)
- Special tests (supine lying) - First rib mobility - Rib springing - Upper limb neurodynamic (tension) test 4 (ULNT4) - Palpation (supine lying) - Federung test (segmental translation of the thoracic vertebrea)
- Sensitivity of the thorax and stomach
After any assessment, the patient should be warned of the possibility of exacerbation of symptoms as a result of assessment.[4]
Elaboration on some testing
Assess passive movements of the thoracic spine and the end feel:[4]
• Forward flexion (tissue stretch)
• Extension (tissue stretch)
• Side flexion, left and right (tissue stretch)
• Rotation, left and right (tissue stretch)
Pain provocation by performing passive movements, in particular rotation, forward flexion, backward flexion and lateral flexion can indicate a spinal aetiology.
Sensory symptoms can be present if the patient has a thoracic disc herniation. It can cause altered sensation to light touch or pinprick along a dermatomal pattern. Cord compression and myelopathy should be strongly considered if a sensory level is established such that sensation is consistently altered below a specific dermatome.
Provocative manoeuvres such as the Spurling manoeuvre (cervical radiculopathy) and the Straight-Leg Raise test or the Slump Test (lumbosacral radiculopathy) may exclude a thoracic disc syndrome.[2][5][6] />
You can also take a look at Thoracic Examination on Physiopedia.
Evaluation[edit | edit source]
In addition to a detailed neurological examination, an MRI of the thoracic spine is very sensitive and specific for diagnosing thoracic disc herniation[10]. In some situations, thoracic discography can be performed to confirm the pain being of discogenic origin being that most thoracic discogenic syndrome can be asymptomatic[1]
Outcome measures[edit | edit source]
- Occiput to Wall Distance
- VAS-pain scale
- Pain Catastrophizing Scale
- Fear-avoidance Beliefs Questionnaire
- Patient Specific Functional Scale
- Fingertips to Floor
Medical Management[edit | edit source]
The initial treatment of thoracic discogenic syndrome is usually conservative (nonoperational) since some disc herniations have been reported to stabilize/regress with time, especially in younger patients.
- Conservative management includes rest, anti-inflammatory drugs, and physical therapy.
- Drugs like Pregabalin have been reported to be useful for the numbness and radicular pain.
- Selective spinal root or intercostal nerve blockade and epidural steroids injections can also be used to treat radicular pain.
- Surgical intervention is considered as a last resort for the treatment of symptomatic thoracic disc herniations with patients unresponsive to conservative treatment.[1]
Physical Therapy Management[edit | edit source]
Several guidelines recommend physical exercise to alleviate pain. The goal of physiotherapy should be to increase the range of motion and pain relief, using a multiple-exercise based approach to strengthen supporting muscles and postural support.[6][7] Animal model studies show that physical exercise helps in intravertebral disk proliferation, particularly in moderate to high volume low repetition and frequency exercises.[8][9] Most patients (80%) with a prolapsed intervertebral disc respond in 4-6 weeks to conservative therapy.[10][11]
Mechanical strain on the disc can be reduced by horizontal positioning, although bedrest is usually not indicated. The application of heat can bring relief by relaxing the reflexive tension of the thoracic musculature, particularly the paravertebral extensors of the trunk and by promoting circulation.[2]
Some ideas from Physiopedia for physical therapy treatment:
- Exercise in pain management
- Top 3 thoracic spine mobility exercises (Physiospot)
- Thoracic Manual Techniques and Exercises
Case Studies[edit | edit source]
- Unusual chest wall pain caused by thoracic disc herniation in a professional baseball pitcher
- Histologically proven acute paediatric thoracic disc herniation causing paraparesis
- Acute chest pain in a top soccer player due to thoracic disc herniation
Clinical Bottom Line[edit | edit source]
- Thoracic discogenic pain syndrome (TDPS) is rare making it challenging for the healthcare team to diagnose and treat the condition.
- The rarity of TDPS is attributed to the particular orientation, structure, and function of the thoracic spine in the vertebral column.
- Despite this rarity, physiotherapists, physician assistants, and physicians should be familiar with its diagnosis and treatment and work as an interprofessional team to provide treatment[1]
- Physical therapy should be focussed on increasing the range of motion and pain relief, using a multiple-exercise based approach to strengthen muscles and postural support.[6] [7]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Fogwe DT, Zulfiqar H, Mesfin FB. Thoracic Discogenic Syndrome. InStatPearls [Internet] 2019 Jun 25. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK470388/ (last accessed 2.5.2020)
- ↑ 2.0 2.1 2.2 2.3 2.4 Juergen Kraemer, 2009, Intervertebral Disk Diseases: Causes, Diagnosis, Treatment and Prophylaxis , Thieme , Stuttgart, 375p.
- ↑ 3.0 3.1 Vanichkachorn JS, Vaccaro AR. Thoracic disk disease: diagnosis and treatment. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2000 May 1;8(3):159-69.
- ↑ 4.0 4.1 4.2 Magee, D. J. (2008). Orthopedic physical assessment. St. Louis, Mo: Saunders Elsevier. Print
- ↑ Shirzadi A, Drazin D, Jeswani S, Lovely L, Liu J. Atypical presentation of thoracic disc herniation: case series and review of the literature. Case reports in orthopedics. 2013;2013.
- ↑ 6.0 6.1 6.2 Deitch K, Chudnofsky C, Young M. T2–3 Thoracic Disc Herniation with Myelopathy. The Journal of emergency medicine. 2009 Feb 1;36(2):138-40.
- ↑ 7.0 7.1 Manchikanti L, Hirsch JA. Clinical management of radicular pain. Expert review of neurotherapeutics. 2015 Jun 3;15(6):681-93.
- ↑ Luan S, Wan Q, Luo H, Li X, Ke S, Lin C, Wu Y, Wu S, Ma C. Running exercise alleviates pain and promotes cell proliferation in a rat model of intervertebral disc degeneration. International journal of molecular sciences. 2015 Jan;16(1):2130-44.
- ↑ Steele J, Bruce-Low S, Smith D, Osborne N, Thorkeldsen A. Can specific loading through exercise impart healing or regeneration of the intervertebral disc?. The Spine Journal. 2015 Oct 1;15(10):2117-21.
- ↑ Hofstee DJ, Gijtenbeek JM, Hoogland PH, van Houwelingen HC, Kloet A, Lötters F, Tans JT. Westeinde sciatica trial: randomized controlled study of bed rest and physiotherapy for acute sciatica. Journal of Neurosurgery: Spine. 2002 Jan 1;96(1):45-9.
- ↑ Weber H, Holme I, Amlie E. The natural course of acute sciatica with nerve root symptoms in a double-blind placebo-controlled trial evaluating the effect of piroxicam. Spine. 1993 Sep;18(11):1433-8..