Tarsal Tunnel Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 182: | Line 182: | ||
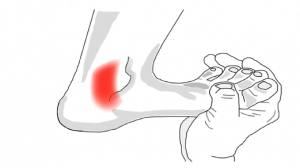
Tarsal tunnel syndrome may lead to a broad range of symptoms affecting the posteromedial ankle and plantar aspects of the foot.<ref name="1" /> This is due to the proximal TTS affecting the tibial nerve in the retromalleolar region, whereas distal TTS tends to affect its branches.<ref name="19" /> According to Zheng et al (2016), paresthesia and/or pain in the sole of the foot is the widely accepted primary symptom of tarsal tunnel syndrome.<ref name="15">Zheng C, Zhu Y, Jiang J, Ma X, Lu F, Jin X, Weber R. The prevalence of tarsal tunnel syndrome in patiens with lumbosacral radiculopathy. European Spine Journal 2016;25:895-905. (Level of Evidence 2b)</ref> Ahmad et al (2012) says that the predominant symptom is indeed pain, directly over the tarsal tunnel behind the medial malleolus with radiation to the longitudinal arch and plantar aspect of the foot including the heel.<ref name="5" /> Tu & Bytomski (2011) talk about medial midfoot heel pain<ref name="17" /> and Kavlak & Uygur (2011) about the symptom triad of pain, paresthesia and numbness. Other (sensory) symptoms may include dysesthesia and, as already stated above, paraesthesia (e.g. burning, tingling and numbness) at all or varied sites of the tarsal tunnel including: the posterior compartment, retromalleolar flexor retinaculum coverage, and both the anterior and posterior fibro-osseus tunnels branching to the plantar margins of the foot.<ref name="1" /><ref name="5" /><ref name="12" /><ref name="17" /> A varied and specific involvement of the differing nerve branches accounts for the diverse presentation and extent level of symptoms observed with the condition of tarsal tunnel syndrome.<ref name="1" /> | Tarsal tunnel syndrome may lead to a broad range of symptoms affecting the posteromedial ankle and plantar aspects of the foot.<ref name="1" /> This is due to the proximal TTS affecting the tibial nerve in the retromalleolar region, whereas distal TTS tends to affect its branches.<ref name="19" /> According to Zheng et al (2016), paresthesia and/or pain in the sole of the foot is the widely accepted primary symptom of tarsal tunnel syndrome.<ref name="15">Zheng C, Zhu Y, Jiang J, Ma X, Lu F, Jin X, Weber R. The prevalence of tarsal tunnel syndrome in patiens with lumbosacral radiculopathy. European Spine Journal 2016;25:895-905. (Level of Evidence 2b)</ref> Ahmad et al (2012) says that the predominant symptom is indeed pain, directly over the tarsal tunnel behind the medial malleolus with radiation to the longitudinal arch and plantar aspect of the foot including the heel.<ref name="5" /> Tu & Bytomski (2011) talk about medial midfoot heel pain<ref name="17" /> and Kavlak & Uygur (2011) about the symptom triad of pain, paresthesia and numbness. Other (sensory) symptoms may include dysesthesia and, as already stated above, paraesthesia (e.g. burning, tingling and numbness) at all or varied sites of the tarsal tunnel including: the posterior compartment, retromalleolar flexor retinaculum coverage, and both the anterior and posterior fibro-osseus tunnels branching to the plantar margins of the foot.<ref name="1" /><ref name="5" /><ref name="12" /><ref name="17" /> A varied and specific involvement of the differing nerve branches accounts for the diverse presentation and extent level of symptoms observed with the condition of tarsal tunnel syndrome.<ref name="1" /> | ||
A very common used clinical test for the diagnosis of tarsal tunnel syndrome is the [[Tinel’s Test|Hoffmann-Tinel Sign]].<ref name="1" /><ref name="17" /> Originally used as a specific test for the carpal tunnel syndrome, it can also be used to examine tibial nerve compression in the ankle.<ref name="13">http://www.physio-pedia.com/Tinel%E2%80%99s_Test</ref> During this test, the nerve is percussed or tapped at the suspected site of compression, the area below the medial malleolus.<ref name="1" /> A positive diagnosis will cause paresthesia either locally or radiating along the course of the nerve.<ref name="1" /> This positive result may be due to the entrapment of the nerve by surrounding tissues.<ref name="7">Harries M, Williams C, Stanish WD, Micheli LJ. Oxford textbook of sports medicine. Great Britain: Butler &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Tanner ltd., frame, 2000, pp. 699 – 700. (Level of evidence 2B)</ref><ref name="9">Nagaoka M, Satou K. Tarsal tunnel syndrome caused by ganglia. The journal of bone &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; joins surgery 1998:607-10. (Level of Evidence 2b)</ref> When the test delivers a negative result, the patient feels no pain.<ref name="13" /> It is furthermore postulated that greater than 50% of patients with compressive neuropathy of the tarsal tunnel will portray a positive Tinel’s sign of the posterior tibial nerve.<ref name="8">Division of Physiotherapy, School of Health and Rehabilitation Sciences, The University of Queensland, QLD 4072 St. Lucia, Australia. Strain and excursion of the sciatic, tibial, and plantar nerves during a modified straight leg raising test. Pubmed. [Online] [Citaat van: 16 november 2010.] http://www.ncbi.nlm.nih.gov/pubmed/16838375 (Level of Evidence 1a)</ref> Alongside Tinel’s sign, the physiotherapist could also use the SLR (Straight Leg Raise) test to provoke symptoms similar to a nerve problem.<ref name="8" /> | A very common used clinical test for the diagnosis of tarsal tunnel syndrome is the [[Tinel’s Test|Hoffmann-Tinel Sign]].<ref name="1" /><ref name="17" /> Originally used as a specific test for the carpal tunnel syndrome, it can also be used to examine tibial nerve compression in the ankle.<ref name="13">http://www.physio-pedia.com/Tinel%E2%80%99s_Test</ref> During this test, the nerve is percussed or tapped at the suspected site of compression, the area below the medial malleolus.<ref name="1" /> A positive diagnosis will cause paresthesia either locally or radiating along the course of the nerve.<ref name="1" /> This positive result may be due to the entrapment of the nerve by surrounding tissues.<ref name="7">Harries M, Williams C, Stanish WD, Micheli LJ. Oxford textbook of sports medicine. Great Britain: Butler &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Tanner ltd., frame, 2000, pp. 699 – 700. (Level of evidence 2B)</ref><ref name="9">Nagaoka M, Satou K. Tarsal tunnel syndrome caused by ganglia. The journal of bone &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; joins surgery 1998:607-10. (Level of Evidence 2b)</ref> When the test delivers a negative result, the patient feels no pain.<ref name="13" /> It is furthermore postulated that greater than 50% of patients with compressive neuropathy of the tarsal tunnel will portray a positive Tinel’s sign of the posterior tibial nerve.<ref name="8">Division of Physiotherapy, School of Health and Rehabilitation Sciences, The University of Queensland, QLD 4072 St. Lucia, Australia. Strain and excursion of the sciatic, tibial, and plantar nerves during a modified straight leg raising test. Pubmed. [Online] [Citaat van: 16 november 2010.] http://www.ncbi.nlm.nih.gov/pubmed/16838375 (Level of Evidence 1a)</ref> Alongside Tinel’s sign, the physiotherapist could also use the SLR (Straight Leg Raise) test to provoke symptoms similar to a nerve problem.<ref name="8" /> | ||
A second test that could be used (in addition to the Tinel’s sign) for making the symptoms become diagnostically apparent is the dorsiflexion-eversion test.<ref name="1" /><ref name="14" /><ref name="17" /><ref name="18">Kinoshita M, Okuda R, Morikawa J, Jotoku T, Abe M. The dorsiflexion-eversion test for diagnosis of tarsal tunnel syndrome. The Journal of Joint &amp;amp;amp;amp;amp;amp;amp;amp; Bone Surgery 2001;83(12):1835-39. (Level of Evidence 2b)</ref> To perform this test the clinician both passively maximally everts and dorsiflexes the ankle whilst maximally dorsiflexing the metatarsophalangeal joints.<ref name="1" /> This position is held for 5 – 10 s and will display further intensification of the symptoms if positive.<ref name="1" /> On occasions pain may also ascend to the thigh following this means of testing (1; LOE: 5), although this would happen rather rarely.<ref name="15" /> Kinoshita et al (2006) have reported that the dorsiflexion-eversion test reproduced or aggravated symptoms for 82% in symptomatic feet, with no replication evident in the healthy control group.<ref name="14" /> In brief, what happens during the dorsiflexion-eversion test is that the distal posterior tibial nerve is stretched and compressed.<ref name="14" /> | A second test that could be used (in addition to the Tinel’s sign) for making the symptoms become diagnostically apparent is the dorsiflexion-eversion test.<ref name="1" /><ref name="14" /><ref name="17" /><ref name="18">Kinoshita M, Okuda R, Morikawa J, Jotoku T, Abe M. The dorsiflexion-eversion test for diagnosis of tarsal tunnel syndrome. The Journal of Joint &amp;amp;amp;amp;amp;amp;amp;amp;amp; Bone Surgery 2001;83(12):1835-39. (Level of Evidence 2b)</ref> To perform this test the clinician both passively maximally everts and dorsiflexes the ankle whilst maximally dorsiflexing the metatarsophalangeal joints.<ref name="1" /> This position is held for 5 – 10 s and will display further intensification of the symptoms if positive.<ref name="1" /> On occasions pain may also ascend to the thigh following this means of testing (1; LOE: 5), although this would happen rather rarely.<ref name="15" /> Kinoshita et al (2006) have reported that the dorsiflexion-eversion test reproduced or aggravated symptoms for 82% in symptomatic feet, with no replication evident in the healthy control group.<ref name="14" /> In brief, what happens during the dorsiflexion-eversion test is that the distal posterior tibial nerve is stretched and compressed.<ref name="14" /> | ||
[[Image:Figuur_DE5.png|thumb|left|Fig. 5 McSweeney & Cichero (2015). The dorsiflexion-eversion test – the testing clinician passively maximally everts and dorsiflexes the ankle whilst maximally dorsiflexing the metatarsophalangeal joints.]] | |||
Abouelala & Zohiery (2012) investigated a fourth clinical test, called the triple compression stress test (TCST). This provocative test was supposed to be more specific and therefore sensitivity and specificity for diagnosing TTS was investigated. The TCST showed 85,9% sensitivity and 100% specificity. The TCST combines the Tinel’s sign test with the Trepman test<ref name="1" /> by bringing the foot passively in full plantar flexion, inversion and applying an even and constant digital pressure over the posterior tibial nerve for 30s.<ref name="12" /> A double compression on the nerve occurs from the plantar flexion and inversion, and along with a simultaneous third compression maneuver by direct digital pressure, the test was hence named triple compression stress test.<ref name="12" /> The study found that clinical signs and symptoms of tarsal tunnel syndrome were apparent within a matter of seconds for 93,8% of symptomatic feet.<ref name="12" /> Pain usually developed within 10 s and numbness within 30 s of the test. All control feet had negative clinical TCST. The researchers also state that the TCST achieves a simple, fast and very reliable provocative maneuver to increase sensitivity of TSS diagnosis, both clinically and electrophysiologically.<br><br> | <br> | ||
Further intensification of symptoms can also be obtained by using the Trepman test or the plantar flexion-inversion test.<ref name="1" /><ref name="17" /> This maneuver also increases pressure on the tibial nerve within the tarsal tunnel confines.<ref name="1" /> Through intra-operative observation, Hendrix et al (reviewed by McSweeney & Cichero, 2015) acknowledged this combined movement not only reduced the overall width of the tarsal tunnel, but also compressed the lateral-planter nerve.<ref name="1" /> So either dorsiflexion-eversion or plantar flexion-inversion can reproduce pain or increase the symptoms of tarsal tunnel syndrome.<ref name="14" /> | |||
Abouelala & Zohiery (2012) investigated a fourth clinical test, called the triple compression stress test (TCST). This provocative test was supposed to be more specific and therefore sensitivity and specificity for diagnosing TTS was investigated. The TCST showed 85,9% sensitivity and 100% specificity. The TCST combines the Tinel’s sign test with the Trepman test<ref name="1" /> by bringing the foot passively in full plantar flexion, inversion and applying an even and constant digital pressure over the posterior tibial nerve for 30s.<ref name="12" /> A double compression on the nerve occurs from the plantar flexion and inversion, and along with a simultaneous third compression maneuver by direct digital pressure, the test was hence named triple compression stress test.<ref name="12" /> The study found that clinical signs and symptoms of tarsal tunnel syndrome were apparent within a matter of seconds for 93,8% of symptomatic feet.<ref name="12" /> Pain usually developed within 10 s and numbness within 30 s of the test. All control feet had negative clinical TCST. The researchers also state that the TCST achieves a simple, fast and very reliable provocative maneuver to increase sensitivity of TSS diagnosis, both clinically and electrophysiologically. | |||
[[Image:Figuur_AB6.png|thumb|left|Fig.6 Abouelela & Zohiery (2012). TCST (A) ankle plantar flexion. (B) Heel and foot inversion. (C) Digital compression of the tibial nerve posterior to the medial malleolus.]]<br><br> | |||
== Outcome Measures == | == Outcome Measures == | ||
Revision as of 00:42, 10 January 2017
Original Editor - Staci Burns, Jonathan Blondeel
Top Contributors - Admin, Blondeel Jonathan, Dieter Schuddinck, Rani Sileghem, Staci Burns, Kim Jackson, Rachael Lowe, Jesse Lemmens, Vidya Acharya, 127.0.0.1, Tarina van der Stockt, Kai A. Sigel, WikiSysop, Jenny Wong and Naomi O'Reilly
Search Strategy[edit | edit source]
We searched the web using different databases: Pubmed, PEDro, ScienceDirect, Web of Science and Google Scholar. We used one of or a combination of the following keywords.
Keywords: tarsal tunnel syndrome, TTS, tibial nerve entrapment, tibial neuropathy, plantar heel pain, diagnosis, physical therapy, conservative management, surgery, medical management, physical management, etc.
Definition/Description[edit | edit source]
Tarsal tunnel syndrome is a compressive neuropathy of the posterior tibial nerve or one of its associated branches individually or collectively.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleThe tunnel lies posterior to the medial malleolus of the ankle, beneath the flexor retinaculum. Symptoms include pain radiating into the foot, usually this pain is worsened by walking (or weight-bearing acitvities). Examination may reveal Tinel’s sign over the tibial nerve at the ankle, weakness and atrophy of the small foot muscles or loss of sensation in the foot.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Clinically Relevant Anatomy[edit | edit source]
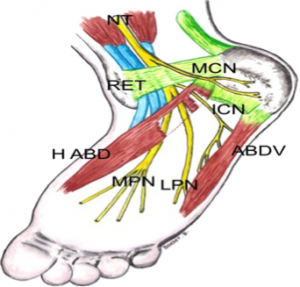
The tarsal tunnel is a fibrous osseus tunnel, it has a proximal floor and a distal floor. The proximal floor is formed by the flexor retinaculum (RET, Fig 1), it contains several flexor tendons (M. Tibialis posterior, M. Flexor digitorum longus, M. Flexor halluces longus), the posterior tibial nerve, the posterior tibial artery and the tibial veins. The distal floor is formed between the abductor hallucis muscle (H ABD, Fig. 1) and the deep quadratus plantae. This contains branches of the plantar vessels and the plantar nerves.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
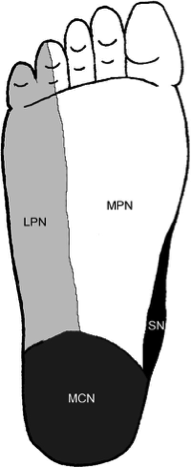
The posterior tibial nerve (NT, Fig. 1) runs along the M. soleus in the posterior compartment. The nerve exits the compartment and passes deep behind the RET between the calcaneus and the medial malleolus. Before passing behind the flexor retinaculum the nerve branches, one part moves on behind the RET, the other part forms the Medial calcaneal nerve (MCN, Fig 1). At the distal floor the tibial nerve divides into two terminal branches: Medial plantar nerve (MPN, Fig. 1) and Lateral plantar nerve (LPN, Fig. 1), sometimes this happens at the proximal tunnel. The inferior calcaneal nerve runs branches off from the lateral plantar nerve and is also referred to as the motor nerve for the abductor muscle for the fifth toe (ABD V, Fig. 1)
Compression of the Tibial nerve at the tarsal tunnel leads to plantar heel pain, this condition is called Tarsal Tunnel Syndrome. Other nerves that run in the foot also have risk of compression due to their anatomical situation.
The LPN supplies most of the muscles of the foot, the lateral part of the skin (Fig. 2) and the fourth and fifth toe. This nerve runs between the abductor hallucis and the quadratus plantae, entrapment between these muscles is possible and also the most common. The first branch of the LPN runs close to the calcaneal tuberosity (ICN, Fig. 1), which is also a possible site of entrapment. The MCN supplies sensory innervation to most of the heel (heel fat pad, superficial tissues) (Fig. 2), this nerve is less likely to be compressed between its anatomical sturctures. But can be traumatised and irritated as a result of atrophy of the heel fat pad. The MPN innervates the abductor hallucis, flexor hallucis brevis, flexor digitorum brevis, first lumbrical and also the medial side of the plantar part (Fig. 2) of the foot.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Epidemiology / Etiology[edit | edit source]
Tarsal Tunnel Syndrome is caused by any kind of entrapment or compression of the tibial nerve or its plantar branches. In many cases the cause is idiopathic or posttraumatic. In a literature review, by John T.C. Lau, M.D. et al., was estimated that 20-40 % of cases were idiopathic.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Up to 10% of all cases are the result of the following diseases: arthrosis, tenosynovitis and Rheumatoid Arthritis. Nearly twice as many cases have convoluted vessels as the origin.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Some other rare causes are Diabetes Mellitus, Hypothyroidism, Gout, mucopolysaccharidoses, and (very rarely) hyperlipidemia.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Some muscles or tendons, medial of the talus bone, can entrap the tibial nerve due to hypertrophy or being accessory. As mentioned in the ‘anatomy’-section the tendon of the flexor hallucis longus muscle passes the tarsal tunnel along with blood vessels, the tibial nerve and other muscles. When enough hypertrophy occurs in one of these muscles the pressure within the tarsal tunnel increases. Sometimes this can even lead up to the muscle belly of the flexor hallucis longus entering the tarsal tunnel. This can cause an overstimulation of the tibial nerve or its branches. Depending on which nerve is being impinged the patient can get different uncomfortable sensations in its foot.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Some persons are born with accessory muscles. These variations from the norm can cause more harm than good. Those muscles are not necessarily helpful, but it is a given that they do occupy space within the foot. Similar to hypertrophy of the muscles in the medial ankle region this can compress the tibial nerve possibly resulting in chronic pain.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Surgery or an overload on the ankle region can cause local inflammation and swelling, yet again causing pressure on the tibial nerve. Sports where sprinting and jumping play a significant role have been proven to be provocative for TTS. People with flat feet, talocalcaneal coalition or bony fragments around the tarsal tunnel are more vulnerable to develop the syndrome.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
People with flat feet, talocalcaneal coalition or bony fragments around the tarsal tunnel are more vulnerable to develop TTS.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
It might be important to mention that because tarsal tunnel syndrome is a relatively uncommon clinical entity, it can often be misdiagnosed in both children and adults due to the clinician’s low index of suspicion.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title McSweeney & Cichero (2015) also state in their review that the incidence of TTS is not known but the prevalence would be greater in females than males, predominately in adults.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title TTS also tends to be more common in athletes and individuals whom are subjected to prolonged weight-baring periods inclusive of standing, walking or intense physical activity.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Pes planus deformity/hyperpronation may compromise the anatomical structures within the tarsal tunnel and thus lead to a physical decrease of space and an increase in tension of the nerve.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title It would be one of the most common extrinsic factors to cause TTS.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Alleviation of pain/complaints could be obtained with restCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title or neutral immobilization of the foot and ankle, and loose-fitting footwear.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title External compression resulting from footwear or tight plaster casts is said to be a most common cause.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Clinical Presentation[edit | edit source]
TTS has the following symptoms: tingling or burning pain (paresthesia), hyperesthesia and sensory impairment (dysesthesia). The symptoms diffuse in the sole and/ or the heel or digits of the forefoot. The Valleix phenomenon, in which the symptoms extend midway to the lower leg due to percussion of the entrapped nerve, may also occur. McSweeney & Cichero (2015) also state in their review that the symptoms are often unilaterally presented and that they may worsen as the day progresses.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This can also be accompanied by nocturnal awakening.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Furthermore, in some cases muscle the patients may also present weakened, atrophied or paralyzed flexor and digital abductor muscles.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Patients may be unable to move the hallux as a result of local tenderness and swelling. These movements include flexion, extension, abduction and adduction.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Pain becomes worse after or during weight-bearing activities and improves with rest.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Pain is the most prominent symptom, which is localized directly over the medial malleolus with radiation to the longitudinal arch and plantar aspect of the foot including the heel.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Pain begins in the plantar part of the forefoot and extends to the toes. It is usually aggravated in the night due to the modification of foot posture that causes the posterior tibial nerve to be restrained or venous congestion. There is rarely motor weakness or atrophy of intrinsic foot muscles.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Common manifestations of tarsal tunnel syndrome is a positive Tinel’s sign and pain felt on provocation using passively maximally dorsiflexion and eversion of the ankle while all the metatarsophalangeal joints are performing dorsiflexion. Most common and objective symptom is a diminished sensation.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Differential Diagnosis
[edit | edit source]
Most persons have once had sensation of so-called sleeping limbs, usually referred to as paresthesia. This feeling can also rise due to a pathogenic condition such as polyneuropathy. That’s when this numb, tingling feeling can no longer be put under control by the patient. It’s a condition often arises at the hands or feet. Considering one has paresthesia at the foot, the symptoms are very similar to those of the TTS.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
A shortage of oxygen supply to tissue is called ischemia. Permanent damage can occur when this supply is put on hold for extensive time. As nerves start to lack oxygen their functionality slowly decreases. The result of extended ischemia can be devastating. However if a lack of blood flow is the cause, and it is normalized in time, damage can be near to none. Concerning nerves, in some cases permanent ischemic paresthesia can arise. This makes the neurons fire at random which gives the same sensation as the symptoms of TTS.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
A compartment syndrome can mostly be found in the upper arm and lower leg. It can show up after a pressure build-up on or within a muscle compartment with an overload of certain muscle groups or fluid build-up being possible origins of this syndrome. The tibial nerve runs along the deep calf muscles with a compartment. Excessive pressure may trigger this nerve to fire uncontrollably. The TTS can be misdiagnosed for this compartment syndrome if the compression of the nerve mostly takes place near the medial malleolus.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The former has also proven to be able to produce a distal tibial nerve lesion. A lesion is any damage or abnormal change in tissue. A lesion in or near a nerve can compromise its function. Therefore it can simulate the same symptoms as the TTS when a nerve near the medial malleolus is involved.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
As a tumour is a group of cells which grow uncontrollably and can be benign, precancerous or malignant. Despite these three distinctions they do have in common that they take up space unnecessarily. Pressure caused by tumours rarely induces trouble to its surround tissues. It can however be a differential diagnosis for TTS if it overexcites a nerve at the medial malleolus.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
A sum-up of possible differential diagnosesCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
|
|
Diagnostic Procedures[edit | edit source]
The diagnosis of TTS is mainly a clinical diagnosis based on detailed medical history and clinical examination. The clinical tests performed by physiotherapists are mostly provocative tests.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title These will be further described in the topic “Examination” (underneath). Adjunctive medical imaging and electrophysiological studies may assist in diagnosingCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title and could provide additional information useful to plan management.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleThis can include electrodiagnostic studies, radiographs, ultrasound, MRI and computed tomography.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title It is, for example, also possible for the digital abductor and flexor muscles of the symptomatic foot to weaken, atrophy or even paralyse in some chronic circumstances.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This is often difficult to detect clinically and may therefore require subsequent referral for medical imaging or nerve conduction studies.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title We should keep in mind though that these kinds of examinations are not substitutes for the clinical examination but they can play a key role in confirming or excluding the physician’s suspicion.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
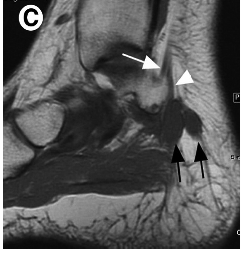
As already mentioned, diagnosing the cause of TTS, and actually a lot of other medial ankle and heel pain, by physical examination alone can be challenging for the clinician.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This is due to the complex anatomy of the medial aspect of the ankle and hindfoot, which makes localizing symptoms to a specific structure difficult.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title For example, plain X-rays of the ankle are useful in demonstrating structural abnormalities such as hind foot varus/valgus. Magnetic resonance imaging (MRI) adds further detail and is highly accurate (83%) when investigating space-occupying lesions.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
MRI is considered the gold standard in identifying suspected compression of the tarsal tunnel caused by the presence of obstructive foreign masses, lesions or tumours.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This type of imaging not only confirms the presence of a suspected lesion but also defines the depth, extent and margins of the lesion for accurate characterization.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title In a study undertaken by Frey (reviewed by McSweeney & Cichero, 2015), MRI was deemed to have shown significant findings in 88% of symptomatic tarsal tunnel candidates, thus assisting with etiological reasoning and surgical planning if required.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title MRI and high-resolution ultrasound have the diagnostic capability to detect and demonstrate the thickness of the flexor retinaculum, overall depth and contents within the tarsal tunnel, including the posterior tibial nerve cross-sectional area and its terminal branch derivatives.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
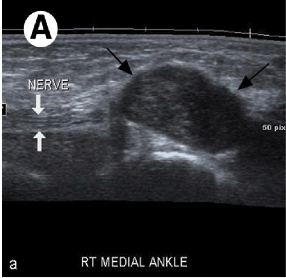
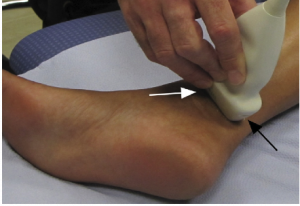
Ultrasound represents an accessible, portable and relatively inexpensive (less expensive than MRI) imaging tool for the assessment of medial ankle and heel pain.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title In addition, it offers the advantage of comparison with the contralateral side.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Although MRI (above) is considered the gold standard, ultrasound is effective in the diagnosis of pathologic conditions affecting the medial ankle and heel and correlates well with MRI.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Ultrasound is able to demonstrate the complex anatomy of the tarsal tunnel and show the entire course of the tibial nerve and its branches at the medial ankle. It is also effective in the identification of space occupying lesions. Even small changes in the cross sectional area of the nerve can be detected on ultrasound in symptomatic patients.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Electrodiagnostic testing can also assist in the diagnosis of tarsal tunnel syndrome.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title These tests include nerve conduction studies that assess sensory conduction velocities of the tibial nerve or one of its branches, as well as the amplitude and duration of motor-evoked potentials.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title There is limited quality evidence based research that demonstrates high sensitivity and specificity of the electrophysiological techniques in TTS. Reduced amplitude and increased duration of the motor response are the more sensitive indicators of the presence of pathology.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Unfortunately these investigations often yield an unacceptable level of false negative results, and should be utilized as an adjunctive assessment to confirm physical examination findings.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Saeed (reviewed by McSweeney & Cichero, 2015) discusses evidence of false positive readings in his study of 70 asymptomatic subjectsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title and Ahmad et al (2012) report that false negative tests are not uncommon and therefore do not rule out the diagnosis.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Thus, Abouelela & Zohiery (2012) state that provocative tests remain important in the diagnosis of TTS due to the unaccepted range of false negative results in electrodiagnostic testing.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Last, plain weight-bearing radiographs and/or computed tomography of the foot and ankle should be acquired if suspecting morphological influences or structural anomalies from bony abnormalities, according to McSweeney & Cichero (2012).Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Omoumi et al (2010) state that in practice, the visualization of articular communication with MRI or ultrasonography can be challenging.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Computed tomography (arthrography) with delayed acquisitions has been shown to be a valuable technique for the detection of articular communication between structures and a joint.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Closing, it is recommended that all tests should ideally be performed bilaterally for adequate observation and comparative study of the contralateral joint.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Examination
[edit | edit source]
Tarsal tunnel syndrome may lead to a broad range of symptoms affecting the posteromedial ankle and plantar aspects of the foot.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This is due to the proximal TTS affecting the tibial nerve in the retromalleolar region, whereas distal TTS tends to affect its branches.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title According to Zheng et al (2016), paresthesia and/or pain in the sole of the foot is the widely accepted primary symptom of tarsal tunnel syndrome.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Ahmad et al (2012) says that the predominant symptom is indeed pain, directly over the tarsal tunnel behind the medial malleolus with radiation to the longitudinal arch and plantar aspect of the foot including the heel.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Tu & Bytomski (2011) talk about medial midfoot heel painCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title and Kavlak & Uygur (2011) about the symptom triad of pain, paresthesia and numbness. Other (sensory) symptoms may include dysesthesia and, as already stated above, paraesthesia (e.g. burning, tingling and numbness) at all or varied sites of the tarsal tunnel including: the posterior compartment, retromalleolar flexor retinaculum coverage, and both the anterior and posterior fibro-osseus tunnels branching to the plantar margins of the foot.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title A varied and specific involvement of the differing nerve branches accounts for the diverse presentation and extent level of symptoms observed with the condition of tarsal tunnel syndrome.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
A very common used clinical test for the diagnosis of tarsal tunnel syndrome is the Hoffmann-Tinel Sign.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Originally used as a specific test for the carpal tunnel syndrome, it can also be used to examine tibial nerve compression in the ankle.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title During this test, the nerve is percussed or tapped at the suspected site of compression, the area below the medial malleolus.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title A positive diagnosis will cause paresthesia either locally or radiating along the course of the nerve.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This positive result may be due to the entrapment of the nerve by surrounding tissues.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title When the test delivers a negative result, the patient feels no pain.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title It is furthermore postulated that greater than 50% of patients with compressive neuropathy of the tarsal tunnel will portray a positive Tinel’s sign of the posterior tibial nerve.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Alongside Tinel’s sign, the physiotherapist could also use the SLR (Straight Leg Raise) test to provoke symptoms similar to a nerve problem.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
A second test that could be used (in addition to the Tinel’s sign) for making the symptoms become diagnostically apparent is the dorsiflexion-eversion test.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title To perform this test the clinician both passively maximally everts and dorsiflexes the ankle whilst maximally dorsiflexing the metatarsophalangeal joints.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This position is held for 5 – 10 s and will display further intensification of the symptoms if positive.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title On occasions pain may also ascend to the thigh following this means of testing (1; LOE: 5), although this would happen rather rarely.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Kinoshita et al (2006) have reported that the dorsiflexion-eversion test reproduced or aggravated symptoms for 82% in symptomatic feet, with no replication evident in the healthy control group.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title In brief, what happens during the dorsiflexion-eversion test is that the distal posterior tibial nerve is stretched and compressed.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Further intensification of symptoms can also be obtained by using the Trepman test or the plantar flexion-inversion test.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This maneuver also increases pressure on the tibial nerve within the tarsal tunnel confines.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Through intra-operative observation, Hendrix et al (reviewed by McSweeney & Cichero, 2015) acknowledged this combined movement not only reduced the overall width of the tarsal tunnel, but also compressed the lateral-planter nerve.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title So either dorsiflexion-eversion or plantar flexion-inversion can reproduce pain or increase the symptoms of tarsal tunnel syndrome.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Abouelala & Zohiery (2012) investigated a fourth clinical test, called the triple compression stress test (TCST). This provocative test was supposed to be more specific and therefore sensitivity and specificity for diagnosing TTS was investigated. The TCST showed 85,9% sensitivity and 100% specificity. The TCST combines the Tinel’s sign test with the Trepman testCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title by bringing the foot passively in full plantar flexion, inversion and applying an even and constant digital pressure over the posterior tibial nerve for 30s.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title A double compression on the nerve occurs from the plantar flexion and inversion, and along with a simultaneous third compression maneuver by direct digital pressure, the test was hence named triple compression stress test.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title The study found that clinical signs and symptoms of tarsal tunnel syndrome were apparent within a matter of seconds for 93,8% of symptomatic feet.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Pain usually developed within 10 s and numbness within 30 s of the test. All control feet had negative clinical TCST. The researchers also state that the TCST achieves a simple, fast and very reliable provocative maneuver to increase sensitivity of TSS diagnosis, both clinically and electrophysiologically.
Outcome Measures[edit | edit source]
There exists a wide variety in clinical outcomes that can be used to evaluate foot conditions. In 2013 Kenneth J. et al. concluded in their 10-year research that most of them were inconsistently used. Out of 139 clinical outcomes the American Orthopaedic Foot & Ankle Society (AOFAS), the visual analog scale (VAS) for pain, the Short Form-36 (SF-36) Health Survey, the Foot Function Index (FFI) and the American Academy of Orthopaedic Surgeons (AAOS) outcomes instruments were the most popular. The study underlined the need for consistent use of a responsive, valid, reliable and clinically meaningful outcome measurement tool.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
One measurement tool that meets the requirements is the Foot and Ankle Abitlity Measure. It was made in 2005 by RobRoy et al. It covers a wide variety of disorders in the lower extremity, namely the lower leg, foot and ankle. Examples are plantar fasciitisCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title, ankle instabilityCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title, etc. Its clinical relevance was researched by Martin et al. and in the table underneath the validity, reliability and responsiveness of the tool is summerised.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
| Instrument | Content validity | Construct validity | Reliability | Responsiveness |
| FAAM | 1-factor structure and high interal consistency (alpha .96 and .98 respectively) |
- No correlation to SF-36 physical function subscale and physical component summary score (r, 0.78 and 0.84, respectively)* - Low correlation to SF-36 mental health subscale and mental component summary score* |
- ADL subscale - Sport subscale ICC, 0.89 (SEM 4,5) - MDC95 of 6 points on the ADL subscale and 12 points on the sport subscale during 9 wk |
- Minimum clinically important differences of 8 and 9 points for the ADL and sports subscales, respectively, distinguishing between those improved versus not improved after 4 wk of physical therapy* - Significantly different change in scores during 4 wk in the group expected to change (P<.001)* |
Medical Management
[edit | edit source]
The management goes into two directions: a conservative or non-operative management and surgery. The former is used prior to the latter approach, unless signs of muscle atrophy or motor involvement are obvious, according to McSweeney & Cichero. The latter is used when patients haven’t benefitted from the former approach.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Conservative approach
In this approach the following can be included: “physical therapy, non-steroidal anti-inflammatory, analgesic, opioid or GABA analog medications, tri-cyclic antidepressants and vitamin B-complex supplements and corticosteroid injections” (1). In the literature there is unfortunately an absence of RCTs, and in existing case series the efficacy of treatment methods can’t be quantified.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Surgical approach
When the non-operative management doesn’t work, surgical management is recommended.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This approach can include: “surgical decompression of the tibial nerve and its branches with division of the medial flexor retinaculum; release of the deep fascia of the abductor hallucis muscle and removal of impinging or pathological lesions”.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title It is stated by McSweeney & Cichero that surgery may improve symptoms of the syndrome but that evidence of the efficacy of the surgery in the literature can conflict itself.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Another surgical approach is cryosurgery. McSweeney & Cichero state that there are different advantages of using cryosurgery for this syndrome, but as there is a lack of clinical trials the guideline for the use of this method is still undergoing change.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Physical Therapy Management
[edit | edit source]
There is a lack of evidence in literature on treatment approaches.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Small RCT’s would help to find succesfull rehabilitation excersices or other treatments for patients with tarsal tunnel syndrome.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Published papers have reported case studies, but empirical evidence of their efficacy is lacking.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
At the time patients who do not respond to physical therapy or other conservative treatment are reffered to a clinician for a surgical approach (e.g. decompression of the tarsal tunnel).
Conservative treatment
There are three stagesCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title in the development of TTS, in every stage there are different aspect that may be adressed in the management of the symptoms.
Orthotics and tapingCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
1. UCBL orthosis
A University of California Berkeley Laboratory orthosis can be used to improve hind foot alignment
2. CAM walker
Controlled ankle motion walker, with this boot the ROM of the patients ankle can be altered.
3. Plantar arch tapingCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
https://www.youtube.com/watch?v=5Z2XlqsuQSY
4. Patient education on footwear
The therapist should educate the patient on wearing appropriate footwear. Thight fitting shoes should be avoided. When dealing with athletes one must pay attention tot heir running mechanics and/or motions in their technique (sport specific) that may cause the symptoms.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Therapeutic excersices
1. StretchingCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
• Calf muscle
There are many ways to stretcht the calf muscle, one of the most frequently used is the calf stretch using a wall. The left picture focusses on stretching the gastrocnemius muscle, the right picture focusses on stretching the soleus muscle
• Achilles tendon:
• Plantar fascia
1) cross you affected leg over your other leg
2) Using the hand on your affected side, take hold of your affected foot and pull your toes back towards shin. This creates tension/stretch in the arch of the foot/plantar fascia.
3) Check for the appropriate stretch position by gently rubbing the thumb of your unaffected side left to right over the arch of the affected foot. The plantar fascia should feel firm, like a guitar string.
4) Hold the stretch for a count of 10. A set is 10 repetitions.
2. Nerve mobilityCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Nerve mobilization exercises have been used to treat carpal tunnel syndrome (nerve entrapment in the wrist) with contradicting results. In the present literature, only a limited number of case studies where nerve mobilization exercises have been used to treat plantar heel pain of neural origin.
Kavlak Y. and Uygur F. conducted a RCT where they used nerve mobilization techniques as an adjunct to conservative treatment. The studie reported a positive outcome for R.OM., muscle strenght and pain in both groups. The study group showed a significant improvement for 2-point discrimination, light touch and tinel’s sign.
Nerve mobilization as described by Meyer et al.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The patient is seated at the egde of the table wit hand is asked to slump forward into a comfortable position with the hands behind the back (see image). The ankle is taken into end-range dorsiflexion and eversion to bring tension on the tibial nerve.
The knee is extended to R1 (= the angle where the PT feels the first resistance) with the ankle in end-range dorsiflexion and eversion and back to the relaxed flexed state.
Each extension-flexion takes about 4 seconds and is repeated 10 times
3. Tibialis posterior strenghteningCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The function of the tibialis posterior muscle is to stabilize the ankle, it is also used for inversion of the ankle. Exercises can be classified into two categories: weight bearing and non-weigth bearing.
Example of a non-weight bearing exercise:
https://www.youtube.com/watch?v=zJ56EjnQ3Ok
Example of a weight bearing exercise:
https://www.youtube.com/watch?v=aDyr2wAOIhM
Other types of conservative treatment may includeCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title:
• Rest
• NSAID’s
• Corticosteroid injections
• Extracorporeal shockwave therapy
• Laser
• Local anaesthetic injections
• Heel pads and heel cups
• Night splints
• Medial longitudinal arch supports
• Strapping
• Soft-soled shoes
• Casting
It is recommended that patients are treated conservatively prior to the surgical treatment. When patients do not respond to the conservative treatment or if there are signs of atrophy or motor involvment they should be reffered to a clinician.
Postoperative rehabilitationCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
| Timeline | Goals | Intervention | |
| Phase I | Week 1 - 3 |
- Protect joint/nerve integrity - Control inflammation - Control pain/edema |
- Immobilization - Passive mobilization - Surgical site protection - Elevation and ice - Educate and monitor non-weight bearing crutch ambulation |
| Phase II | Week 3 - 6 |
- Prevent contraction, scar tissue - Soft tissue and joint mobility |
- Weight-bearing as tolerated - Gentle passive, active-assist, active ankle stretches - Genlte passive dorsiflexion - Tibial nerve gliding with anti-tension - Pain-free, weight-bearing dorsiflexion - Gait training wearing protective splint - Aqua therapy |
| Phase III | Week 6 - 12 |
- Normal gait mechanics - Symmetric ankle mobility - Single leg proprioception - Repeated single leg heel raises (pain free) - Sport/job - specific exercises
|
- Gatin training - Resistive ankle ex. (parin free) - Progress stretching ex. - Progress resistive ex. (to body weight) - Progress proprioceptive and balance ex. - Cardiovascular ex. (pain free) - Low level plyometric ex. |
Key Research and Case Studies[edit | edit source]
KEY RESEARCH
The following source was key research for this page:
Kavlak Y, Uygur F. Effects of nerve mobilization exercise as an adjunct to the conservative treatment for patients with tarsal tunnel syndrome. Journal of manipulative and physiological therapeutics 2011;34(7):441-48. (Level of Evidence 1b)Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
CASE STUDIES
Dr. Karen Hudes published a case studie about a 61 year old who had been diagnosed with tarsal tunnel syndrome. During a period of 6 months the patient complained of plantar and dorsal pain and a burning sensation. The patient rated a 9/10 on a Verbal Rating Scale and had been wearing a pair of custom orthotics prescribed by a podiatrist. These orthotics did not reduce the pain. A treatment plan was started using fascial stripping to the lateral heel ocer the tarsal tunnel, and over the plantar and dorsal surfaces of the forefoot, high velocity low amplitude (HVLA) toggle board adjustments of the talonavicular joint and mobilization of the cuboid. The treatment was given twice per week for two weeks. After a few weeks the patients symptoms started to resolve and later the symptoms dissapeared. The patient reported no pain on a 10 month follow up.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Meyer et al. described a case of a 44 year old patient who complaints of limited standing and walking tolerance, secondary to left subcalcaneal heel pain. Prior to the treatment Meyer et al. prescribed the patient had underwent a 2-week medication presciption, 2 cortisone injections to the insertion of the plantar fascia on the calcaneus, 2 months of wearing orthotics and a 3 week exercise program that consisted of calf stretching and toe curls. Over the course of 4 months these treatments where unsuccesful. An intervention strategy was developed to address weakness, excessive foot pronation, restricted lower extremity mobility, muscular tightness and pain. The PT used soft-tissue mobilization to the gastrocnemius and the soleus, neural mobilization (as discribed above) and a home exercise program. Plantar arch taping was applied and later in the treatment, the patient was instructed in posterior tibialis strength exercises. The patient received 10 PT sesions, after these sessions the symptoms were gone.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template).
Resources
[edit | edit source]
http://sportspodiatry.co.uk
http://www.footlogics.co.za/achilles-tendonitis-pain-treatment.html
http://www.aofas.org/footcaremd/conditions/ailments-of-the-heel/pages/plantar-fasciitis.aspx
https://www.youtube.com/watch?v=5Z2XlqsuQSY
https://www.youtube.com/watch?v=zJ56EjnQ3Ok
https://www.youtube.com/watch?v=aDyr2wAOIhM
Clinical Bottom Line[edit | edit source]
Tarsal tunnel syndrome is a rare condition and often underdiagnosed.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title A variety of symptoms are possible, such as: tingling or burning pain (paresthesia), hyperesthesia and sensory impairment (dysesthesia). These are felt on the plantar face of the ankel and foot.
There are a few test to identify tarsal tunnel syndrome or rule out other possibilities, these tests include: MRI, Ultrasound, Hoffman-tinels test, dorsiflexion-eversion test, trepman test and the triple compression stress test.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Treatment of a tarsal tunnel syndrom should be attemted conservatively at first (see “Physical therapy management”). If conservative treatment fails a surgical aproach can be taken.
Recent Related Research (from Pubmed)[edit | edit source]