Calcaneal Spurs
Original Editors - Caro De Koninck
Top Contributors - Mahyar Firouzi, Lionel Geernaert, Julie Lhost, Ivakhnov Sergei, Caro De Koninck, Sheik Abdul Khadir, Scott Cornish, Admin, Kim Jackson, Simisola Ajeyalemi, Rachael Lowe, Joao Costa, Wanda van Niekerk, 127.0.0.1, Evan Thomas, Naomi O'Reilly and Priyanka Chugh
Definition/Description[edit | edit source]
A calcaneal spur, or commonly known as a heel spur, occurs when a bony outgrowth forms on the heel bone. Calcaneal spurs can be located at the back of the heel (dorsal heel spur) or under the sole (plantar heel spur). The dorsal spurs are often associated with achilles Tendinopathy, while spurs under the sole are associated with Plantar fasciitis.
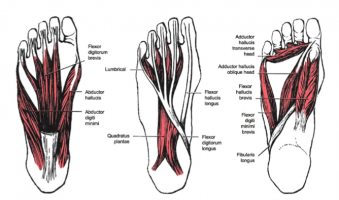
The apex of the spur lies either within the origin of the planter fascia (on the medial tubercle of the calcaneus) or superior to it (in the origin of the flexor digitorum brevis muscle). The relationship between spur formation, the medial tubercle of the calcaneus and intrinsic heel musculature results in a constant pulling effect on the plantar fascia resulting in an inflammatory response.[1]
Clinically Relevant Anatomy[edit | edit source]
There are numerous muscles (Soleus, gastrocnemius, plantaris, abductor digiti minimi, flexor digitorum brevis, extensor digitorum brevis, abductor hallucis, extensor hallucis brevis, quadratus plantae) and the plantar fascia which exert a traction force on the tuberosity and adjacent regions of the calcaneus, especially when excessive or abnormal pronation occurs. The origin of the spurs appears to be caused by repetitive trauma which produces micro tears in the plantar fascia near its attachment and the attempted repair leads to inflammation which is responsible for the production and the maintenance of the symptoms.[2][3][4][5]
Epidemiology /Etiology[edit | edit source]
The etiology of spurs has been debated. Heredity, metabolic disorders, tuberculosis, systemic inflammatory diseases and many other disorders have also been implicated. Current reasoning is that abnormal biomechanics (excessive or abnormal pronation) is the prime etiological factor for a painful plantar heel and inferior calcaneal spur. The spur is thought to be a result of the biomechanical fault and an incidental finding when associated with a painful plantar heel. The most common etiology is thought to be abnormal pronation which results in increased tension forces within the structures that attach in the region of the calcaneal tuberosity.
Asymptomatic heel spurs are relatively common in the normal, adult population. One epidemiologic study found that 11% of the adult U.S. population had developed a calcaneal spur which showed up on incidental radiographic finding.[6]
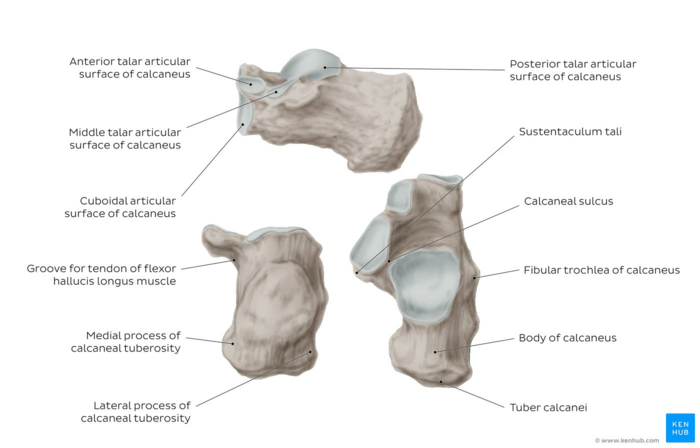
Image: Overview of the calcaneus bone[7]
Characteristics/Clinical Presentation[edit | edit source]
The painful heel is a relatively common foot problem, but calcaneal spurs are not considered as a primary cause of heel pain. A calcaneal spur is caused by long-term stress on the plantar fascia and foot muscles and may develop as a reaction to plantar fasciitis.[8]
The pain, mostly localised in the area of the medial process of the calcaneal tuberosity, is caused by pressure in the region of the plantar aponeurosis attachment to the calcaneal bone. The condition may exist without producing symptoms, or it may become very painful, even disabling.[9]
Most heel pain patients are middle-aged adults. Obesity may be considered a risk factor. Not all heel spurs cause symptoms and are often painless, but when they do cause symptoms people often experience more pain during weight-bearing activities, in the morning or after a period of rest. The pain, however, is not as a result of mechanical pressure on the spur, but from the inflammatory response.
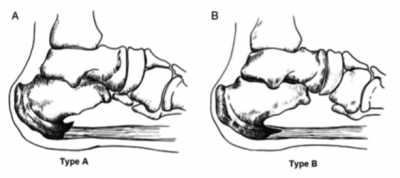
There are 2 types of calcaneal spurs;
- Type A spurs are superior to the plantar fascia insertion
- Type B spurs extend forward from the plantar fascia insertion distally within the plantar fascia.
The mean spur length for type A is significantly longer statistically than the mean spur length for type B, although patients with type B spurs reported more severe clinical pain.[10]
Spurs can be classified into 3 distinct types:
- There are those which are large in size, but which are asymptomatic, because the angle of growth is such that the spur aggravated through weight-bearing and/or the inflammatory changes have halted.[11]
- The 2nd type are large, but painful on weight-bearing, because the pitch of the calcaneus has been changed by a depression of the longitudinal arch and, as a result, the spur may become a weight-bearing point, sometimes causing intractable refractory pain.[11]
- This 3rd type has only a tiny amount of proliferation and its outline is irregular and jagged, usually accompanied by an area of decreased density around the origin of the plantar fascia, indicating a subacute inflammatory process. All calcaneal spurs undoubtedly begin in this manner, but only a few become symptomatic at this stage, because the etiologic factors are acute.[11]
Differential Diagnosis[edit | edit source]
As chronic heel pain is a common manifestation of many conditions, these must be excluded before planning treatment. Diagnostic imaging as well as medical signs are often used to differentiate some of the conditions that are mentioned below from calcaneal spurs.
Musculoskeletal Causes[edit | edit source]
- Peroneal tendonitis: (inflammation of one or both peroneal tendons)
- MRI scan or ultrasound investigation
- Haglund's deformity (with or without bursitis): symptomatic osseous posterior-superior prominence of the calcaneus
- Radiographs or Sonography of foot in maximal dorsiflexion [12]
- Sever's disease (calcaneal apophysitis): inflammation of the calcaneal apophysis due to overloading
Traumatic Influences[edit | edit source]
- Calcaneal fractures (and stress fractures): fractures as a consequence of repetitive load to the heel
- Ottawa Ankle Rules, Radiography, MRI (isotopic bone scan) and ultrasound.[15]
Neurological Causes[edit | edit source]
- Baxter nerve entrapment: (chronic compression of the first branch of the lateral plantar nerve)
- Clinical (Tinel’s sign)
- Tarsal tunnel syndrome (sinus tarsi): Impingement of the posterior tibial nerve
- Clinical (Tinel’s sign, dorsiflexion-eversion test)
Other[edit | edit source]
- Heel fat pad syndrome: Atrophy or inflammation of the shock-absorbing fatty pad or corpus adiposum
- Clinical, ultrasound scan
- Chronic lateral ankle pain with other cause:
- MRI
- MRI
Diagnostic Procedures[edit | edit source]
A diagnosis is based on the patient's history and on the results of the physical examination. Diagnosis is usually confirmed by X-ray, but other diagnostic adjuncts are also used.[16] Radiology may show calcaneal spur formation or calcification at either the insertion of the Achilles tendon or the origin of the plantar fascia.[17] Rarely is an MRI required.
Outcome Measures[edit | edit source]
Examination[edit | edit source]
There are different aspects that need to be taken into consideration when performing the clinical examination.
- Is range of motion limited in the ankle and foot, especially passive dorsiflexion of the toes?
- Palpation of the proximal plantar fascia attachment at the heel. The presence of a calcaneal spur, any tenderness (site/severity) or deformities can be felt (in combination with the dorsiflexion)
- Is there any atrophy of the heel pad in comparison with the other foot in combination with reduced muscle strength?
- Is there any swelling?
- Sensation
- Presence of hypesthesias/dysthesias of the tibial nerve? Tinel’s sign
- Are there any skin tears on the foot?
- Any difference in foot alignment in comparison with the other foot?
- Aggravation on weight-bearing?
- Evaluation of gait
Management[edit | edit source]
‘The clinical practice guideline revision 2010 outlines different phases, divided in tiers. If a certain tier reduces symptoms, treatment should continue. If no improvement is reported, then treatment moves to a higher tier.
Recommended treatment timeline before moving up a tier if no improvement in symptoms:
Tier 1: 6 weeks
Tier 2: 6 months
Tier 3: 6 months
Medical Management[edit | edit source]
Tier I
● Non steroidal anti inflammatory drugs (NSAID)[18]
Grade I recommendation
● Cortisone injections[19]
Grade B recommendation
Tier II
● Repeat cortisone injections[20][21][22]
Grade B recommendation
● Botulinum toxin[23][24][25]
Grade I recommendation
Tier III
● Endoscopic plantar fasciotomy[26]
● In-step fasciotomy[27][28]
● Minimal invasive surgical technique
All grade B recommendations
Conservative Management[edit | edit source]
Tier I
● Padding and strapping of the foot [29][30]
● Therapeutic orthodic insoles for short-term pain relief [31][32]
● Achilles and plantar fascia stretching [33][34]
● Prefabricated and custom orthotic device. Prefabricated shows better results compared to the custom device in the improvement of symptoms [35]
Grade B recommendation
● Night splints[36]
Grade B recommendation
●Physiotherapy[37]
Grade I recommendation
● Cast or boot immobilisation[38]
Grade C recommendation
Tier III
● ESWT (Extracorporal Shock Wave Therapy)[39][40][41][42]
Grade B recommendation
● Bipolar radiofrequency (microtenotomy) [43]
Grade C recommendation
Missing Evidence in the Guidelines[edit | edit source]
Some treatments are proven effective in treating plantar fasciitis, but not in the presence of calcaneal spurs. Those recommendations can, therefore, only be used when the calcaneal spur is associated with plantar fasciitis.
Bipolar radiofrequency (microtenotomy) :
In the guidelines, this treatment received a grade C recommendation. This grade may change in the future pending new research.
- March 2015: “Bipolar radiofrequency microtenotomy appears to be a safe procedure that can provide outcomes equivalent to those with open surgery, with less morbidity, for recalcitrant plantar fasciitis.” [44]
- December 2015: “RM is as effective as PF in the treatment of plantar fasciitis. Patients who underwent both procedures experienced no benefit and a higher rate of complications.” [45] For long-term efficacy a larger research cohort is needed.
Physical Therapy Management[edit | edit source]
Calcaneal spurs, both upper and lower spurs, are treated with conventional physiotherapy.
- Low Dose Radiotherapy (radiation side effects and syndromes)
Using this method, there is evidence that the re-irritation of the painful heel spur is a safe and effective treatment. There was a significant response for at least 2 years in reduction of pain [46], although a placebo effect can occur [47]. There is, however, still no clear decision on what dose is the most effective, either 1.0 Gy or 0.5 Gy.
- Cryoultrasound therapy and cryotherapy are both effective for treating chronic plantar fasciitis with heel spurs. Cryoultrasound therapy appears to offer better outcomes. [48]
- Thermotherapy
Cold therapy may be used to relieve inflammation and reduce pain.
Heat therapy to loosen tense muscles and promote oxygen and blood flow to the affected area.[49] Thermotherapy might be useful for the reduction of pain during exercises. - Low level laser therapy is found to be an effective method for treating heel spurs. Although, more research with larger groups is needed for more evidence. [50]
- Conventional therapy includes ultrasound, laser treatment, passive and active stretching and strengthening of the muscles of the legs, cold and hot applications (Contrast Bath). The aim is to eliminate inflammation surrounding the spur. This treatment programme may take 6 to 12 months for symptom resolution.
- Conservative treatment: While conservative treatments can help reduce the symptoms of bone spurs, they do not always treat the source of your pain.
- Radial shockwave therapy consists of very high energy mechanical waves, directed at the plantar fasciitis, to help reduce inflammation.
- Extracorporeal Shock Wave Therapy (ESWT): Various studies do suggest that ESWT is not an effective treatment for plantar fasciitis. (Buchanan et al. 2002, Haake et al. 2003) This discrepancy between studies means that further support for an effective treatment with ESWT is needed, because there was a remarkable positive effect of ESWT pointed at the calcaneal spur, but the difference between the presence and absence of a calcaneal spur was not significant enough.[51] According to De Vera Barredo et al.(2007) night splints, massage, taping, acupuncture, walking casts, laser therapy and cryotherapy are more effective. Shafshak reported that ESWT appeared effective in relieving heel pain among patients with calcaneal spur especially when given within the first 4 months after the start of a patient's symptoms. ECSWT is recommended to be the first choice in treating calcaneal spur and is most effective when treatment is at least 3x500 impulses. [52] Yalcin however suggested that ESWT is perhaps not the most effective therapy for heel spurs. After five ESWT treatments, no patient had significant spur reductions, but 19 patients (17.6%) had a decrease in the angle of the spur, 23 patients (21.3%) had a decrease in the dimensions of the spur, and one patient had a broken spur. The therapy did however produce significant effects in reducing patients’ symptoms. Further studies are required about the effectiveness of ESWT. [53]
Orthotics[edit | edit source]
The effect of orthotics is only relevant when the calcaneal spur is related to plantar fasciitis.
Night Splints[edit | edit source]
A conservative treatment in combination with the use of a night splint that keeps the ankle in 5-degree of dorsiflexion for eight weeks; Patients without previous treatments for plantar fasciitisobtain significant relief of heel pain in the short term with the use of a nightsplint incorporated into conservative methods; however, this application does not have a significant effect on prevention of recurrences after a two-year follow-up.
Heel Inserts[edit | edit source]
Heel inserts or Heel spur pads should relieve heel spur pressure and inflammation and catch shock forces and distribute them evenly throughout the heel reducing stress. However, Chia suggested that Heel spur pads were ineffective in reducing rearfoot pressure and increased rearfoot peak forces while orthotics and customised orthotics reduced rearfoot peak forces on both sides. Pre-fabricated and customised orthotics are therefore useful in distributing pressure uniformly over the rearfoot region. [54]
Footwear Modification [edit | edit source]
- Footlogics: provide relief from Plantar Fasciitis (heel pain and heel spurs), achilles Tendinopathy and also forefoot pain. Aims to correct over-pronation, fallen arches and flat feet.
- Insoles: Patients with heel pain, diagnosed as Sever's injury, wore insoles with no other treatments added and all patients maintained their high level of physical activity throughout the study period. Significant pain reduction during physical activity when using insoles was found. [55]
Clinical Bottom Line[edit | edit source]
Calcaneal spurs are bony growths at the back of the heel (dorsal) or under the sole of the foot (plantar). Dorsal spurs are associated with Achilles tendinopathy and plantar with plantar fascitis. Their aetiology appears to be linked with repetitive trauma to the associated muscles and tendons with the attempted repair of micro-tears causing inflammation and pain. Abnormal biomechanics is thought to the reason for this reaction. Pain is commonly felt at the heel, affected gait and weight bearing, but differential diagnosis has to be excluded to the number of possible conditions for an appropriate treatment protocol. X-ray is an effective diagnostic tool. Management can either be medical or non-medical depending on an individual's response.
References[edit | edit source]
- ↑ Johal KS .,‘Plantar fasciitis and the calcaneal spur: Fact or fiction?’., Foot Ankle Surg.,18 March 2012 (level of evidence 3B)
- ↑ Gill LH. Plantar fasciitis: diagnosis and conservative management. J Am Acad Orthop Surg, 1997
- ↑ McCarthy DJ, Gorecki GE: The anatomical basis of inferior calcaneal lesions. J Am Podiatry Assoc 69527-536,1979 (level of evidence: 2C)
- ↑ Young CC, Rutherford DS, Niedfeldt MW. Treatment of plantar fasciitis. AmfckLRFam Physician 2001 (level of evidence: 5)
- ↑ Heyd, Reinhard, et al. "Radiation therapy for painful heel spurs." Strahlentherapie und Onkologie 183.1 (2007): 3-9. (level of evidence: 1B)
- ↑ McCarthy DJ, Gorecki GE: The anatomical basis of inferior calcaneal lesions. J Am Podiatry Assoc 69527-536,1979 (level of evidence: 2C)
- ↑ Overview of the calcaneus bone image - © Kenhub [https://www.kenhub.com/en/library/anatomy/calcaneus
- ↑ E.K. Agyekum., “Heel pain: A systematic review”., Chinese Journal of Traumatology., 2015 (level of evidence 1A)
- ↑ B. Jasiak-Tyrkalska., ‘Efficacy of two different physiotherapeutic preocedures in comprehensive therapy of plantar calcaneal spur’., Fizjoterapia Polska., January 2007 (level of evidence: 1B)
- ↑ Zhou, Binghua, et al. "Classification of Calcaneal Spurs and Their Relationship With Plantar Fasciitis." The Journal of Foot and Ankle Surgery 54.4 (2015): 594-600. (level of evidence: 3A)
- ↑ 11.0 11.1 11.2 Henri L. Duvries., “Heel Spur (Calcaneal Spur)”., AMA Arch Surg., (level of evidence: 3A)
- ↑ Chauveaux, D., et al. "A new radiologic measurement for the diagnosis of Haglund's deformity." Surgical and Radiologic Anatomy 13.1 (1991): 39-44. (level of evidence: I)
- ↑ Perhamre, Stefan, et al. "Sever’s injury: a clinical diagnosis." Journal of the American Podiatric Medical Association 103.5 (2013): 361-368. (level of evidence: 3A)
- ↑ Hosgoren, B., A. Koktener, and Gülçin Dilmen. "Ultrasonography of the calcaneus in Sever's disease." Indian pediatrics 42.8 (2005): 801. (level of evidence: 4)
- ↑ Yu, Sarah M., and Joseph S. Yu. "Calcaneal avulsion fractures: an often forgotten diagnosis." American Journal of Roentgenology 205.5 (2015): 1061-1067. (level of evidence: 2A)
- ↑ Rosenbaum, Andrew J., John A. DiPreta, and David Misener. "Plantar heel pain." Medical Clinics of North America 98.2 (2014): 339-352. (level of evidence: 2A)
- ↑ Aldridge, Tracy. "Diagnosing heel pain in adults." American family physician 70 (2004): 332-342. (Level of evidence: 2A)
- ↑ Donley BG, Moore T, Sferra J, Gozdanovic J, Smith R. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int 28:20–23, 2007.(level of evidence: 1B)
- ↑ Kalaci A, Cakici H, Hapa O, Yanat AN, Dogramaci Y, Sevinç TT. Treatment of plantar fasciitis using four different local injection modalities: a randomized prospective clinical trial. J Am Podiatr Med Assoc 99:108–113, 2009.(level of evidence: 1B)
- ↑ Kiter E, Celikbas E, Akkaya S, Demirkan F, Kilic BA. Comparison of injection modalities in the treatment of plantar heel pain: a randomized controlled trial. J Am Podiatr Med Assoc 96:293–296, 2006. (level of evidence: 1B)
- ↑ Buccilli TA Jr, Hall HR, Solmen JD. Sterile abscess formation following a cortico- steroid injection for the treatment of plantar fasciitis. J Foot Ankle Surg 44:466– 468, 2005. (level of evidence: 3A)
- ↑ Porter MD, Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport Med 15:119–124, 2005. (level of evidence: 1B)
- ↑ Placzek R, Holscher A, Deuretzbacher G, Meiss L, Perka C. [Treatment of chronic plantar fasciitis with botulinum toxin Adan open pilot study on 25 patients with a 14-week-follow-up.]. Z Orthop Ihre Grenzgeb 144:405–409, 2006. German. (level of evidence: 1B)
- ↑ Placzek R, Deuretzbacher G, Meiss AL. Treatment of chronic plantar fasciitis with Botulinum toxin A: preliminary clinical results. Clin J Pain 22:190–192, 2006. (level of evidence: 1B)
- ↑ Babcock MS, Foster L, Pasquina P, Jabbari B. Treatment of pain attributed to plantar fasciitis with botulinum toxin a: a short-term, randomized, placebo- controlled, double-blind study. Am J Phys Med Rehabil 84:649–654, 2005. (level of evidence: 1B)
- ↑ Urovitz EP, Birk-Urovitz A, Birk-Urovitz E. Endoscopic plantar fasciotomy in the treatment of chronic heel pain. Can J Surg 51:281–283, 2008. (level of evidence: 2A)
- ↑ Fishco WD, Goecker RM, Schwartz RI. The instep plantar fasciotomy for chronic plantar fasciitis. A retrospective review. J Am Podiatr Med Assoc 90:66–69, 2000.(level of evidence: 2B)
- ↑ Woelffer KE, Figura MA, Sandberg NS, Snyder NS. Five-year follow-up results of instep plantar fasciotomy for chronic heel pain. J Foot Ankle Surg 39:218–223, 2000. (level of evidence: 2B)
- ↑ Shikoff MD, Figura MA, Postar SE. A retrospective study of 195 patients with heel pain. J Am Podiatr Med Assoc 76:71–75, 1986. (level of evidence: 2B)
- ↑ Williams PL. The painful heel. Br J Hosp Med 38:562–563, 1987. (level of evidence: 4)
- ↑ Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med 166:1305–1310, 2006.(level of evidence: 1B)
- ↑ Roos E, Engstrom M, Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int 27:606–611, 2006.(level of evidence: 1B)
- ↑ DiGiovanni BF, Nawoczenski DA, Lintal ME, Moore EA, Murray JC, Wilding GE, Baumhauer JF. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am 85-A:1270–1277, 2003.(level of evidence: 1B)
- ↑ Digiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, Baumhauer JF. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg Am 88:1775–1781, 2006.(level of evidence: 2B)
- ↑ Pfeffer, Glenn, et al. "Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis." Foot & Ankle International 20.4 (1999): 214-221.(level of evidence: 1B)
- ↑ Lee, Sae Yong, Patrick McKeon, and Jay Hertel. "Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis." Physical Therapy in Sport 10.1 (2009): 12-18.(level of evidence: 1A)
- ↑ Cleland JA, Abbott JH, Kidd MO, Stockwell S, Cheney S, Gerrard DF, Flynn TW. Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial.(level of evidence: 1B)
- ↑ Cole C, Seto C, Gazewood J. Plantar fasciitis: evidence-based review of diagnosis and therapy. Am Fam Physician 72:2237–2242, 2005. (level of evidence: 1A)
- ↑ Lee, Gregory P., John A. Ogden, and G. Lee Cross. "Effect of extracorporeal shock waves on calcaneal bone spurs." Foot & ankle international 24.12 (2003): 927-930. (level of evidence: 1A)
- ↑ Marks W, Jackiewicz A, Witkowski Z, Kot J, Deja W, Lasek J. Extracorporeal shock- wave therapy (ESWT) with a new-generation pneumatic device in the treatment of heel pain. A double blind randomised controlled trial. Acta Orthop Belg 74:98– 101, 2008. (level of evidence: 1B)
- ↑ Chuckpaiwong B, Berkson EM, Theodore GH. Extracorporeal shock wave for chronic proximal plantar fasciitis: 225 patients with results and outcome predictors. J Foot Ankle Surg 48:148–155, 2009. (level of evidence: 2B)
- ↑ Pribut SM. Current approaches to the management of plantar heel pain syndrome, including the role of injectable corticosteroids. J Am Podiatr Med Assoc 97:68–74, 2007. (Level of Evidence: 5)
- ↑ Weil L Jr, Glover JP, Sr Weil LS. A new minimally invasive technique for treating plantar fasciosis using bipolar radiofrequency: a prospective analysis. Foot Ankle Spec 1:13–18, 2008. (Level of Evidence: 4)
- ↑ Lucas, Douglas E., Scott R. Ekroth, and Christopher F. Hyer. "Intermediate-Term Results of Partial Plantar Fascia Release With Microtenotomy Using Bipolar Radiofrequency Microtenotomy." The Journal of Foot and Ankle Surgery54.2 (2015): 179-182.(level of evidence: 3B)
- ↑ Chou, Andrew Chia Chen, et al. "Radiofrequency microtenotomy is as effective as plantar fasciotomy in the treatment of recalcitrant plantar fasciitis." Foot and Ankle Surgery (2015). (Level of Evidence: 4)
- ↑ Hautmann, M. G., U. Neumaier, and O. Kölbl. "Re-irradiation for painful heel spur syndrome." Strahlentherapie und Onkologie 190.3 (2014): 298-303. (level of evidence: 2B)
- ↑ Holtmann, Henrik et al. “Randomized Multicenter Follow-up Trial on the Effect of Radiotherapy for Plantar Fasciitis (painful Heels Spur) Depending on Dose and Fractionation – a Study Protocol.” Radiation Oncology (London, England) 10 (2015): 23. PMC. Web. 8 Jan. 2016. (level of evidence: 1B)
- ↑ Costantino, C., et al. "Cryoultrasound therapy in the treatment of chronic plantar fasciitis with heel spurs. A randomized controlled clinical study." European journal of physical and rehabilitation medicine 50.1 (2014): 39-47. (level of evidence: 1B)
- ↑ E.K. Agyekum., “Heel pain: A systematic review”., Chinese Journal of Traumatology., 2015 (level of evidence: 1A)
- ↑ Cinar, E., F. Uygur, and S. Toprak Celenay. "AB1447-HPR The efficacy of low level laser therapy in the treatment of calcaneal spur." Annals of the Rheumatic Diseases 71.Suppl 3 (2013): 757-757. (Level of Evidence: 4)
- ↑ Lee, Gregory P, John A. Ogden, and G. Lee Cross. "Effect of extracorporeal shock waves on calcaneal bone spurs." Foot & ankle international 24.12 (2003): 927-930.
- ↑ Krischek O., “Symptomatic low-energy shockwave therapy in heel pain and radiologically detected plantar heel spur”., Z Orthop Ihre Grenzgeb., April 1998 (level of evidence: 1B)
- ↑ Yalcin E, “Effects of extracorporal shock wave therapy on symptomatic heel spurs: a correlation between clinical outcome and radiologic changes”, Rheumatol Int.; February 2012
- ↑ Chia KK., “Comparative trial of the foot pressure patterns between corrective orthotics, formthotics, bone spur pads and flat insoles in patients with chronic plantar fasciitis”., Ann Acad Med Singapore., October 2009 (level of evidence: 3A)
- ↑ Perhamre S1., “Sever's injury: treatment with insoles provides effective pain relief”., Scand J Med Sci Sports., December 2011 (level of evidence: 1B)