T4 Syndrome: Difference between revisions
No edit summary |
m (adding an interest to a topic) |
||
| (20 intermediate revisions by 5 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | |||
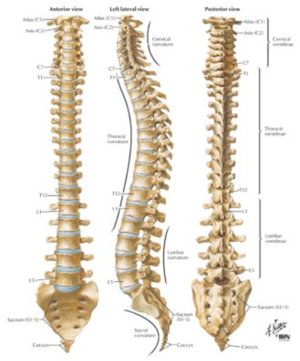
[[File:Thoracic Spine.png|thumb]]T4 syndrome is a diagnosis of exclusion when all other diagnoses do not fit the clinical pattern.<ref name=":12">Karas S, Pannone A, [https://www.sciencedirect.com/science/article/abs/pii/S0161475416303244 The T4 Syndrome: A Scoping Review of the Literature,] Journal of Manipulative and Physiological Therapeutics, 2017,Volume 40, Issue 2, Pages 118-125,</ref> It is a rare occurrence of symptoms involving upper limb parathaesia, weakness with reduced [[Thoracic Examination|thoracic movement]] and tenderness on palpation of the T4 vertebra.<ref>Miyuki Hirai P, Thomson O P, 2016 [https://www.sciencedirect.com/science/article/abs/pii/S1360859216301000 T4 syndrome – A distinct theoretical concept or elusive clinical entity? A case report], Journal of Bodywork and Movement Therapies, Volume 20, Issue 4, P:722-727,</ref> | |||
It was originally theorized these symptoms exist due to sympathetic nerve fibers converging at T4<ref>Brukner, P. and Khan, K., 2012. ''Brukner's & Khan's Clinical Sports Medicine''. 4th ed. Sydney: McGraw-Hill, pp.455-456.</ref>. It is thought that the head and neck are provided with sympathetic outflow from T1 to T4. The upper trunk and extremities are thought to be supplied by T2 to T5. This could account for the symptoms in the neck, head, and upper extremities.<ref name=":1">Evans P, [https://www.sciencedirect.com/science/article/abs/pii/S0031940605660774 The T4 Syndrome: Some Basic Science Aspects], Physiotherapy, 1997, Volume 83, Issue 4, P:186-189,</ref> | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
A typical thoracic vertebra has a total of six joints with neighboring vertebrae: four synovial joints and two symphyses | A typical [[Thoracic Anatomy|thoracic]] vertebra has a total of six joints with neighboring vertebrae: four [[Joint Classification|synovial joints]] and two symphyses.<ref name=":0">Richard L. Drake et al.; Gray’s Anatomy for students, second edition; churchill livingstone elsevier; 2010; p 70-80 | ||
</ref> | </ref> | ||
There are two major types of joints between the vertebrae <ref name=":0" /><br>- Symphyses between vertebral bodies <br>- Synovial joints between articular processes | There are two major types of joints between the vertebrae <ref name=":0" /><br>- Symphyses between vertebral bodies <br>- Synovial joints between articular processes | ||
In thoracic regions, the joints are oriented vertically and limit flexion and extension, but facilitate rotation <ref name=":0" /> | |||
The [https://www.physio-pedia.com/Thoracic_Spinal_Nerves#:~:text=The%20thoracic%20spine%20has%2012,for%20the%20vertebra%20above%20it. thoracic spinal nerves] mostly innervate respiratory, visceral and lower back areas however, T1 and 2 do also provide some of the upper limb. | |||
== Epidemiology == | |||
= | T4 syndrome is a rare occurrence with little high quality evidence to prove it as a diagnosis so caution should be used when diagnosing this as the primary pain driver<ref name=":12" />. | ||
Given the anatomical complexity of the thoracic and shoulder areas, the potential sources of pain in this region are numerous | Given the anatomical complexity of the thoracic and shoulder areas, the potential sources of pain in this region are numerous<ref name=":2">Fruth SJ. 2006, [https://pubmed.ncbi.nlm.nih.gov/16445339/ Differential diagnosis and treatment in a patient with posterior upper thoracic pain]. Phys Ther. Feb;86(2):254-68. PMID: 16445339.</ref><ref>Gummesson C, Ward MM, Atroshi I. 2006, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1513569/ The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH.] BMC Musculoskelet Disord. May 18;7:44.</ref>. | ||
In the worse case scenarios red flag questions to rule out long-standing visceral issues should be asked specifically regarding: | |||
* Cardiac | |||
* [[Respiratory System|Respiratory]] | |||
* Renal | |||
* Gastroesophageal conditions | |||
* [[Cancer Pain|Cancer]] <ref name=":1" /><ref>Edmondston SJ, Singer KP. 1997. [https://pubmed.ncbi.nlm.nih.gov/11440526/ Thoracic spine: anatomical and biomechanical considerations for manual therapy.] Man Ther. 1 Aug;2(3):132-143.</ref>. | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
[[File:Spinal assessment 3.png|right|frameless]] | |||
T4 syndrome is an exclusion diagnosis: once other issues have been excluded then it may be indicative of T4 syndrome. | |||
* Symptoms may arise following a change in normal routine i.e. new job or hobby. These signs and symptoms could be the result of thoracic dysfunction and its influence on the sympathetic nervous system. | |||
Typical presentation includes: | |||
*Paresthesia to the upper limbs and hands in a "glove" presentation<ref name=":1" /><ref name=":4">Mellick GA et al,.Mellick LB, 2006. [https://www.sciencedirect.com/science/article/abs/pii/S0161475406000820 Clinical presentation, quantitative sensory testing, and therapy of 2 patients with fourth thoracic syndrome.] J Manipulative Physiol Ther ;29:403-408.</ref><ref name=":5">DeFranca GG, Levine LJ. [https://pubmed.ncbi.nlm.nih.gov/7706958/ The T4 syndrome]. J Manipulative Physiol Ther. 1995 Jan;18(1):34-7. PMID: 7706958.</ref> | |||
*[[Neck Pain: Clinical Practice Guidelines|Neck pain]] | |||
*[[Headaches and Dizziness|Headaches]] | |||
*Upper limb pain (bilateral or unilateral) | |||
*[[Thoracic Back Pain|Pain around the T4 area]] | |||
*[[Scapula|Scapular]] pain<ref name=":1" /> | |||
*Reduced hand dexterity<ref name=":4" /> | |||
*"Heaviness" in upper extremities | |||
*Hands swollen<ref name=":1" /> | |||
*Thoracic spine stiffness<ref name=":5" /> | |||
*Tenderness on palpation of T4 vertebra<br> | |||
Less common symptoms:<ref name=":1" /> | |||
* | *Pain around chest wall | ||
* | *Worse pain at night | ||
* | *Pain on deep breathing | ||
* | *Pain on coughing or sneezing<ref>Vernon H, Mior S. [https://pubmed.ncbi.nlm.nih.gov/1834753/ The Neck Disability Index: a study of reliability and validity.] J Manipulative Physiol Ther. 1991 Sep;14(7):409-15. Erratum in: J Manipulative Physiol Ther 1992 Jan;15(1):</ref> | ||
Symptoms are often diffuse and located in the neck, head, and upper extremities (unilateral or bilateral) <ref name=":1" /><ref name=":3">Conroy JL, Schneiders AG. The T4 syndrome. Manual Therapy 2005;10:292-296.(LOE 5)</ref><ref name=":4" /><ref name=":5" /> | |||
* | == Diagnostic Procedures == | ||
* | * T4 syndrome is an exclusion diagnosis with '''no''' validated clinical criteria to assist the diagnosis.<ref name=":7">Philip Librone et al.2014. [https://www.vertebralsubluxationresearch.com/2017/09/04/resolution-of-t4-syndrome-following-chiropractic-care-a-case-study/ Resolution of T4 Syndrome Following Chiropractic Care: A Case Report; A. Vertebral Subluxation Res.] Annals of Vertebral Subluxation Research, Volume 2014 Pages 161-168</ref> | ||
* | * Radiographs are no aid in the diagnosis, but can help with ruling out other conditions.<ref name=":5" /> | ||
* Subjective and objective assessments may also help to aid in excluding other diagnoses. | |||
== Examination == | |||
= | There is no evidence about examinations that include T4 syndrome. Unfortunately, a great deal of literature exists on shoulder pain, yet little exists in the area of periscapular or rib pain.<ref name=":7" /> | ||
T4 | It can be concluded that the intervertebral joint around T4 is hypomobile in patients with T4 syndrome. | ||
== | During objective examination it may be useful to assess: | ||
# Overall observation of patient posture in sitting, standing and provocative movements<ref name=":7" /> | |||
# [[Thoracic Examination|Thoracic AROM]]<ref name=":7" /><ref name=":1" /> | |||
# [[Cervical Examination|Cervical AROM]] | |||
# [[Shoulder Examination|Shoulder AROM]] | |||
# Passive thoracic and cervical ROM | |||
# Shoulder and cervical strength | |||
# Neurological assessment - ([[dermatomes]], [[myotomes]], [[reflexes]]) to determine whether nerve root or peripheral nerve lesions were present | |||
== Differential Diagnosis == | |||
[[Red Flags in Spinal Conditions|Red flag]] questions should be asked extensively to rule out any cardiac, respiratory or visceral issues.<ref name=":10">Robert D. Gerwin. [https://www.tandfonline.com/doi/abs/10.1300/J094v10n01_13 Myofascial and Visceral Pain Syndromes: Visceral-Somatic Pain Representations], Journal of Musculoskeletal Pain, 2002. 10:1-2, 165-175</ref> | |||
Thoracic pain is also common with [[Cancer Pain|cancer]] metastases so prior to any manual therapy be sure to rule out cancer as a cause of pain.<ref>Greenhalgh, S. and Selfe, J. Red Flags: A guide to identifying serious pathology of the spine. Churchill Livingstone: Elsevier. 2006.</ref> | |||
After red flags are cleared it is then important to rule out other differential diagnosis especially in potential T4 syndrome as this is a rare condition therefore other diagnoses are more likely. | |||
[[User:Yahya Al-Razi|Dr.Yahya Al-RAzi]] Yemeni Physiotherapist is studying this Syndome and its muskeloskeletal-related pain | |||
These can include: | |||
*[[Thoracic Outlet Syndrome (TOS)|Thoracic Outlet Syndrome]] | |||
*[[Carpal Tunnel Syndrome|Carpal tunnel syndrome]] <ref name=":7" /> | |||
*[[Ulnar Nerve|Ulnar nerve]] entrapment <ref name=":7" /> | |||
*[[Cervical Osteoarthritis|Cervical disc disease or degeneration]] <ref name=":7" /> | |||
*Visceral disease <ref name=":1" /><ref name=":3" /><ref name=":7" /><ref name=":4" /><ref name=":5" /> | |||
*[[Neurological Disorders|Neurological]] disease | |||
*[[Fibromyalgia]] | |||
*[[Myelopathy]] | |||
*[[Complex Regional Pain Syndrome (CRPS)|Complex Regional Pain Syndrome]] | |||
*[[Coronary Artery Disease (CAD)|Cardiac disease]] | |||
== Medical Management == | == Medical Management == | ||
After excluding other conditions including ruling out [[The Flag System|red flags]] and differential diagnosis, pain management should begin. | |||
This should follow the [[Pharmacology in Pain Management|standard ladder of analgesia]] however, if neurological symptoms are present it may be helpful to prescribe gabapentinoids or if pain is ongoing consider intramuscular injections of 1 to 2 mL of 0.5% bupivacaine at the fourth thoracic paraspinal level.<ref name=":4" /> | |||
Physiotherapy and conservative management are the primary treatment options. | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
[[File:Thoracic grade 2 T6 PA mobilisations.png|right|frameless]] | |||
After analgesia has been optimized and if pain is still an issue with functional deficits, physiotherapy is the primary treatment option for T4 syndrome. | |||
Thoracic joint mobilisation techniques are the basics | Various manual therapy techniques have been shown to have some affect on symptom relief. | ||
</ | * Thoracic joint mobilisation techniques are the basics in treating T4 syndrome.<ref>Hirai P M, Thomson O P, 2016,[https://www.sciencedirect.com/science/article/abs/pii/S1360859216301000 T4 syndrome – A distinct theoretical concept or elusive clinical entity? A case report,] Journal of Bodywork and Movement Therapies, Volume 20, Issue 4,Pages 722-727,</ref> <ref>Pete Jowsey, Jo Perry, [https://www.sciencedirect.com/science/article/abs/pii/S1356689X09002185 Sympathetic nervous system effects in the hands following a grade III postero-anterior rotatory mobilisation technique applied to T4: A randomised, placebo-controlled trial,] Manual Therapy, Volume 15, Issue 3, 2010, Pages 248-253,</ref><ref name=":9">Chu J, Allen DD, Pawlowsky S, Smoot B. [https://pubmed.ncbi.nlm.nih.gov/25395830/ Peripheral response to cervical or thoracic spinal manual therapy: an evidence-based review with meta analysis.] J Man Manip Ther. 2014 Nov;22(4):220-9. </ref><ref name=":12" /> | ||
** These mobilisations have been shown to have analgesic mechanisms due to their affect on the sympathetic nervous system.<ref name=":0" /><ref name=":4" /><ref name=":12" /><ref>Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2775050/ The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model]. Man Ther. 2009 Oct;14(5):531-8. </ref> | |||
Soft tissue | * Soft tissue mobilisation | ||
** Light pressure or gentle skin rolling technique have been shown to have analgesic affects in the short term <ref>Diego MA, Field T. [https://pubmed.ncbi.nlm.nih.gov/19283590/ Moderate pressure massage elicits a parasympathetic nervous system response]. Int J Neurosci. 2009;119(5):630-8. </ref><ref name=":12" /><ref>Tozzi P, Bongiorno D, Vitturini C. [https://pubmed.ncbi.nlm.nih.gov/21943614/ Fascial release effects on patients with non-specific cervical or lumbar pain.] J Bodyw Mov Ther. 2011 Oct;15(4):405-16. </ref><ref>Castro-Sánchez AM, Matarán-Peñarrocha GA, Granero-Molina J, Aguilera-Manrique G, Quesada-Rubio JM, Moreno-Lorenzo C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3018656/# Benefits of massage-myofascial release therapy on pain, anxiety, quality of sleep, depression, and quality of life in patients with fibromyalgia.] Evid Based Complement Alternat Med. 2011;2011:561753. </ref><ref>Fernández-Pérez AM, Peralta-Ramírez MI, Pilat A, Villaverde C. [https://pubmed.ncbi.nlm.nih.gov/18724827/ Effects of myofascial induction techniques on physiologic and psychologic parameters: a randomized controlled trial.] J Altern Complement Med. 2008 Sep;14(7):807-11. </ref> | |||
* Address [[Psychological Approaches to Pain Management|psycho-social factors]] and management of these anxieties/stresses <ref name=":9" /> | |||
* Graded exercise program to include<ref name=":12" />:<ref name=":9" /> | |||
** Thoracic and upper limb active and passive ROM<ref name=":2" /> | |||
** Trapezius and rhomboid stretches (as required)<ref name=":2" /> | |||
** Gradual strengthening exercises | |||
** Functional movements | |||
** [[Posture|Postural]] correction (as required) | |||
* [[Neurodynamics|Neurodynamic]] mobilisations | |||
* | |||
* | |||
* | |||
* | |||
* | |||
== | {{#ev:youtube|v=0CrX59ulj9U}}<ref>Physiotutors. Top 5 Thoracic Spine Mobility Drills. Available from: https://www.youtube.com/watch?v=0CrX59ulj9U [last accessed 16/09/2019]</ref> | ||
*<br> | |||
== Outcome Measures == | |||
*No self-report outcome measure has been validated for this specific condition. Any number of outcome measures would be appropriate for this patient population. This includes: | |||
* | ** [[Patient Specific Functional Scale]] (PSFS) <ref name=":8">P. Stratford C. Gill M. Westaway J. Binkley 1995. [https://www.utpjournals.press/doi/abs/10.3138/ptc.47.4.258 Assessing disability and change on individual patients: a report of a patient specific measure]. Physiotherapy Canada. 1995;47(4):258-263 </ref> This scale can determine the functional status of the individual patient. There is asked to report the most important activities that are unable to perform and score them on a 11-points scale (0 = not possible to carry out activity, 10 = possible to carry out activity). A higher score means a better function | ||
* | ** [[Neck Disability Index]] (NDI)<ref name=":8" />: This questionnaire is a self-reported measurement that reports pain and limitations in performing daily work activities. This index can indicate how much the neck problems affect the daily activities. | ||
* | ** [[DASH Outcome Measure|DASH]] <ref name=":2" />: This questionnaire uses a 5-point Likert scale from which the patient can select an appropriate number corresponding to his/her severity in functioning. | ||
* | |||
* | |||
== Key Evidence == | == Key Evidence == | ||
Several case studies have been reported in the literature <ref name=":3" /><ref name=":4" /><ref name=":5" /> | Several case studies have been reported in the literature that conclude there is no validated diagnostic criteria established for T4 Syndrome <ref name=":3" /><ref name=":4" /><ref name=":5" />. | ||
== | No randomized controlled trials have examined the most efficacious intervention strategies. | ||
== Clinical Bottom Line == | |||
T4 syndrome is described as “a pattern that involves upper extremity paresthesia”. It can be caused by thoracic hypomobility but can also have a sympathetic origin. <br>Typical signs and symptoms include headaches, neck and arm pain and ‘bilateral stocking glove’ paresthesia. | |||
It is more likely to be a differential diagnosis and T4 symptom should only be concluded once other conditions are excluded. | |||
Physiotherapy is the primary treatment option along with pharmacology management. Joint mobilisation of the thoracic spine, soft tissue work, mobility exercises and neurodynamic movements are all viable treatments and are best managed with a focus on reducing any potential psychosocial issues at the same time. | |||
== References | == References == | ||
< | <references /> | ||
[[Category:Thoracic Spine]] | [[Category:Thoracic Spine]] | ||
[[Category:Pain]] | [[Category:Pain]] | ||
[[Category:Musculoskeletal/Orthopaedics]] | [[Category:Musculoskeletal/Orthopaedics]] | ||
[[Category:Conditions]] | |||
[[Category:Thoracic Spine - Conditions]] | |||
[[Category:Thoracic Spine - Conditions]] | |||
Latest revision as of 01:09, 21 November 2023
Original Editor - Ernest Gamble
Top Contributors - Abbey Wright, Ernest Gamble, Admin, Rachael Lowe, Liena Lamonte, Stijn Van de Vondel, Evan Thomas, Oyemi Sillo, Kim Jackson, Yahya Al-Razi, Ilona Malkauskaite and Lucinda hampton
Introduction[edit | edit source]
T4 syndrome is a diagnosis of exclusion when all other diagnoses do not fit the clinical pattern.[1] It is a rare occurrence of symptoms involving upper limb parathaesia, weakness with reduced thoracic movement and tenderness on palpation of the T4 vertebra.[2]
It was originally theorized these symptoms exist due to sympathetic nerve fibers converging at T4[3]. It is thought that the head and neck are provided with sympathetic outflow from T1 to T4. The upper trunk and extremities are thought to be supplied by T2 to T5. This could account for the symptoms in the neck, head, and upper extremities.[4]
Clinically Relevant Anatomy[edit | edit source]
A typical thoracic vertebra has a total of six joints with neighboring vertebrae: four synovial joints and two symphyses.[5]
There are two major types of joints between the vertebrae [5]
- Symphyses between vertebral bodies
- Synovial joints between articular processes
In thoracic regions, the joints are oriented vertically and limit flexion and extension, but facilitate rotation [5]
The thoracic spinal nerves mostly innervate respiratory, visceral and lower back areas however, T1 and 2 do also provide some of the upper limb.
Epidemiology[edit | edit source]
T4 syndrome is a rare occurrence with little high quality evidence to prove it as a diagnosis so caution should be used when diagnosing this as the primary pain driver[1].
Given the anatomical complexity of the thoracic and shoulder areas, the potential sources of pain in this region are numerous[6][7].
In the worse case scenarios red flag questions to rule out long-standing visceral issues should be asked specifically regarding:
- Cardiac
- Respiratory
- Renal
- Gastroesophageal conditions
- Cancer [4][8].
Characteristics/Clinical Presentation[edit | edit source]
T4 syndrome is an exclusion diagnosis: once other issues have been excluded then it may be indicative of T4 syndrome.
- Symptoms may arise following a change in normal routine i.e. new job or hobby. These signs and symptoms could be the result of thoracic dysfunction and its influence on the sympathetic nervous system.
Typical presentation includes:
- Paresthesia to the upper limbs and hands in a "glove" presentation[4][9][10]
- Neck pain
- Headaches
- Upper limb pain (bilateral or unilateral)
- Pain around the T4 area
- Scapular pain[4]
- Reduced hand dexterity[9]
- "Heaviness" in upper extremities
- Hands swollen[4]
- Thoracic spine stiffness[10]
- Tenderness on palpation of T4 vertebra
Less common symptoms:[4]
- Pain around chest wall
- Worse pain at night
- Pain on deep breathing
- Pain on coughing or sneezing[11]
Symptoms are often diffuse and located in the neck, head, and upper extremities (unilateral or bilateral) [4][12][9][10]
Diagnostic Procedures[edit | edit source]
- T4 syndrome is an exclusion diagnosis with no validated clinical criteria to assist the diagnosis.[13]
- Radiographs are no aid in the diagnosis, but can help with ruling out other conditions.[10]
- Subjective and objective assessments may also help to aid in excluding other diagnoses.
Examination[edit | edit source]
There is no evidence about examinations that include T4 syndrome. Unfortunately, a great deal of literature exists on shoulder pain, yet little exists in the area of periscapular or rib pain.[13]
It can be concluded that the intervertebral joint around T4 is hypomobile in patients with T4 syndrome.
During objective examination it may be useful to assess:
- Overall observation of patient posture in sitting, standing and provocative movements[13]
- Thoracic AROM[13][4]
- Cervical AROM
- Shoulder AROM
- Passive thoracic and cervical ROM
- Shoulder and cervical strength
- Neurological assessment - (dermatomes, myotomes, reflexes) to determine whether nerve root or peripheral nerve lesions were present
Differential Diagnosis[edit | edit source]
Red flag questions should be asked extensively to rule out any cardiac, respiratory or visceral issues.[14]
Thoracic pain is also common with cancer metastases so prior to any manual therapy be sure to rule out cancer as a cause of pain.[15]
After red flags are cleared it is then important to rule out other differential diagnosis especially in potential T4 syndrome as this is a rare condition therefore other diagnoses are more likely.
Dr.Yahya Al-RAzi Yemeni Physiotherapist is studying this Syndome and its muskeloskeletal-related pain
These can include:
- Thoracic Outlet Syndrome
- Carpal tunnel syndrome [13]
- Ulnar nerve entrapment [13]
- Cervical disc disease or degeneration [13]
- Visceral disease [4][12][13][9][10]
- Neurological disease
- Fibromyalgia
- Myelopathy
- Complex Regional Pain Syndrome
- Cardiac disease
Medical Management [edit | edit source]
After excluding other conditions including ruling out red flags and differential diagnosis, pain management should begin.
This should follow the standard ladder of analgesia however, if neurological symptoms are present it may be helpful to prescribe gabapentinoids or if pain is ongoing consider intramuscular injections of 1 to 2 mL of 0.5% bupivacaine at the fourth thoracic paraspinal level.[9]
Physiotherapy and conservative management are the primary treatment options.
Physical Therapy Management[edit | edit source]
After analgesia has been optimized and if pain is still an issue with functional deficits, physiotherapy is the primary treatment option for T4 syndrome.
Various manual therapy techniques have been shown to have some affect on symptom relief.
- Thoracic joint mobilisation techniques are the basics in treating T4 syndrome.[16] [17][18][1]
- Soft tissue mobilisation
- Address psycho-social factors and management of these anxieties/stresses [18]
- Graded exercise program to include[1]:[18]
- Neurodynamic mobilisations
Outcome Measures[edit | edit source]
- No self-report outcome measure has been validated for this specific condition. Any number of outcome measures would be appropriate for this patient population. This includes:
- Patient Specific Functional Scale (PSFS) [25] This scale can determine the functional status of the individual patient. There is asked to report the most important activities that are unable to perform and score them on a 11-points scale (0 = not possible to carry out activity, 10 = possible to carry out activity). A higher score means a better function
- Neck Disability Index (NDI)[25]: This questionnaire is a self-reported measurement that reports pain and limitations in performing daily work activities. This index can indicate how much the neck problems affect the daily activities.
- DASH [6]: This questionnaire uses a 5-point Likert scale from which the patient can select an appropriate number corresponding to his/her severity in functioning.
Key Evidence[edit | edit source]
Several case studies have been reported in the literature that conclude there is no validated diagnostic criteria established for T4 Syndrome [12][9][10].
No randomized controlled trials have examined the most efficacious intervention strategies.
Clinical Bottom Line[edit | edit source]
T4 syndrome is described as “a pattern that involves upper extremity paresthesia”. It can be caused by thoracic hypomobility but can also have a sympathetic origin.
Typical signs and symptoms include headaches, neck and arm pain and ‘bilateral stocking glove’ paresthesia.
It is more likely to be a differential diagnosis and T4 symptom should only be concluded once other conditions are excluded.
Physiotherapy is the primary treatment option along with pharmacology management. Joint mobilisation of the thoracic spine, soft tissue work, mobility exercises and neurodynamic movements are all viable treatments and are best managed with a focus on reducing any potential psychosocial issues at the same time.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Karas S, Pannone A, The T4 Syndrome: A Scoping Review of the Literature, Journal of Manipulative and Physiological Therapeutics, 2017,Volume 40, Issue 2, Pages 118-125,
- ↑ Miyuki Hirai P, Thomson O P, 2016 T4 syndrome – A distinct theoretical concept or elusive clinical entity? A case report, Journal of Bodywork and Movement Therapies, Volume 20, Issue 4, P:722-727,
- ↑ Brukner, P. and Khan, K., 2012. Brukner's & Khan's Clinical Sports Medicine. 4th ed. Sydney: McGraw-Hill, pp.455-456.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Evans P, The T4 Syndrome: Some Basic Science Aspects, Physiotherapy, 1997, Volume 83, Issue 4, P:186-189,
- ↑ 5.0 5.1 5.2 5.3 Richard L. Drake et al.; Gray’s Anatomy for students, second edition; churchill livingstone elsevier; 2010; p 70-80
- ↑ 6.0 6.1 6.2 6.3 Fruth SJ. 2006, Differential diagnosis and treatment in a patient with posterior upper thoracic pain. Phys Ther. Feb;86(2):254-68. PMID: 16445339.
- ↑ Gummesson C, Ward MM, Atroshi I. 2006, The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. May 18;7:44.
- ↑ Edmondston SJ, Singer KP. 1997. Thoracic spine: anatomical and biomechanical considerations for manual therapy. Man Ther. 1 Aug;2(3):132-143.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Mellick GA et al,.Mellick LB, 2006. Clinical presentation, quantitative sensory testing, and therapy of 2 patients with fourth thoracic syndrome. J Manipulative Physiol Ther ;29:403-408.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 DeFranca GG, Levine LJ. The T4 syndrome. J Manipulative Physiol Ther. 1995 Jan;18(1):34-7. PMID: 7706958.
- ↑ Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991 Sep;14(7):409-15. Erratum in: J Manipulative Physiol Ther 1992 Jan;15(1):
- ↑ 12.0 12.1 12.2 Conroy JL, Schneiders AG. The T4 syndrome. Manual Therapy 2005;10:292-296.(LOE 5)
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 Philip Librone et al.2014. Resolution of T4 Syndrome Following Chiropractic Care: A Case Report; A. Vertebral Subluxation Res. Annals of Vertebral Subluxation Research, Volume 2014 Pages 161-168
- ↑ Robert D. Gerwin. Myofascial and Visceral Pain Syndromes: Visceral-Somatic Pain Representations, Journal of Musculoskeletal Pain, 2002. 10:1-2, 165-175
- ↑ Greenhalgh, S. and Selfe, J. Red Flags: A guide to identifying serious pathology of the spine. Churchill Livingstone: Elsevier. 2006.
- ↑ Hirai P M, Thomson O P, 2016,T4 syndrome – A distinct theoretical concept or elusive clinical entity? A case report, Journal of Bodywork and Movement Therapies, Volume 20, Issue 4,Pages 722-727,
- ↑ Pete Jowsey, Jo Perry, Sympathetic nervous system effects in the hands following a grade III postero-anterior rotatory mobilisation technique applied to T4: A randomised, placebo-controlled trial, Manual Therapy, Volume 15, Issue 3, 2010, Pages 248-253,
- ↑ 18.0 18.1 18.2 Chu J, Allen DD, Pawlowsky S, Smoot B. Peripheral response to cervical or thoracic spinal manual therapy: an evidence-based review with meta analysis. J Man Manip Ther. 2014 Nov;22(4):220-9.
- ↑ Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009 Oct;14(5):531-8.
- ↑ Diego MA, Field T. Moderate pressure massage elicits a parasympathetic nervous system response. Int J Neurosci. 2009;119(5):630-8.
- ↑ Tozzi P, Bongiorno D, Vitturini C. Fascial release effects on patients with non-specific cervical or lumbar pain. J Bodyw Mov Ther. 2011 Oct;15(4):405-16.
- ↑ Castro-Sánchez AM, Matarán-Peñarrocha GA, Granero-Molina J, Aguilera-Manrique G, Quesada-Rubio JM, Moreno-Lorenzo C. Benefits of massage-myofascial release therapy on pain, anxiety, quality of sleep, depression, and quality of life in patients with fibromyalgia. Evid Based Complement Alternat Med. 2011;2011:561753.
- ↑ Fernández-Pérez AM, Peralta-Ramírez MI, Pilat A, Villaverde C. Effects of myofascial induction techniques on physiologic and psychologic parameters: a randomized controlled trial. J Altern Complement Med. 2008 Sep;14(7):807-11.
- ↑ Physiotutors. Top 5 Thoracic Spine Mobility Drills. Available from: https://www.youtube.com/watch?v=0CrX59ulj9U [last accessed 16/09/2019]
- ↑ 25.0 25.1 P. Stratford C. Gill M. Westaway J. Binkley 1995. Assessing disability and change on individual patients: a report of a patient specific measure. Physiotherapy Canada. 1995;47(4):258-263