Sciatica: Difference between revisions
No edit summary |
No edit summary |
||
| Line 10: | Line 10: | ||
* The sciatic nerve provides direct motor function to the [[hamstrings]], lower extremity [[Hip Anatomy|adductors]], and indirect motor function to the [[Gastrocnemius|calf muscles]], anterior lower leg muscles, and some intrinsic [[Foot Anatomy|foot]] muscles. | * The sciatic nerve provides direct motor function to the [[hamstrings]], lower extremity [[Hip Anatomy|adductors]], and indirect motor function to the [[Gastrocnemius|calf muscles]], anterior lower leg muscles, and some intrinsic [[Foot Anatomy|foot]] muscles. | ||
* Indirectly through its terminal branches, the sciatic nerve provides sensation to the posterior and lateral lower leg as well as the plantar foot. | * Indirectly through its terminal branches, the sciatic nerve provides sensation to the posterior and lateral lower leg as well as the plantar foot. | ||
Most cases of sciatica result from an [[Inflammatory Myopathies|inflammatory condition]] leading to an irritation of the sciatic nerve. <ref>Davis DH, Wilkinson JT, Teaford AK, Smigiel MR. Sciatica produced by a sacral perineurial cyst. Texas Medicine. 1987 Mar 1;83(3):55-6.Available from:https://www.statpearls.com/kb/viewarticle/28772/ (last accessed 12.9.2020)</ref> | Most cases of sciatica result from an [[Inflammatory Myopathies|inflammatory condition]] leading to an irritation of the sciatic nerve. <ref name=":0">Davis DH, Wilkinson JT, Teaford AK, Smigiel MR. Sciatica produced by a sacral perineurial cyst. Texas Medicine. 1987 Mar 1;83(3):55-6.Available from:https://www.statpearls.com/kb/viewarticle/28772/ (last accessed 12.9.2020)</ref> | ||
== Etiology == | == Etiology == | ||
Any condition that may structurally impact or compress the sciatic nerve may cause sciatica symptoms. | |||
* The most common cause of sciatica is a [[Lumbar Discogenic Pain|herniated or bulging lumbar intervertebral disc.]] | |||
* In the [[Older People Introduction|older persons]], [[Lumbar Spinal Stenosis|lumbar spinal stenosis]] may cause these symptoms as well. | |||
* [[Spondylolisthesis]] or a relative misalignment of one vertebra relative to another may also result in sciatic symptoms. | |||
* [[Lumbar Anatomy|Lumba]]<nowiki/>r or [[Pelvic Floor Anatomy|pelvic]] muscular spasm and/or inflammation may impinge a lumbar or sacral nerve root causing sciatic symptoms. | |||
* A spinal or paraspinal mass including [[Oncology|malignancy]], [[Overview of Traumatic Brain Injury|epidural hematoma]], or epidural abscess may also cause a mass-like effect and sciatica symptoms<ref name=":0" /> | |||
== Epidemiology == | |||
* No gender predominance | |||
* Peak incidence occurs in patients in their fourth decade | |||
* Lifetime incidence reported between 10% to 40% | |||
* Annual incidence of 1% to 5% | |||
* | * No association with body height has been established except in the age 50 to 60 group. | ||
* | * Rarely occurs before age 20 (unless traumatic) | ||
* | * [[Physical Activity|Physical activity]] increases incidence in those with prior sciatic symptoms and decreased in those with no prior symptoms. | ||
* | * Occupational predisposition has been shown in machine operators, truck drivers, and jobs where workers are subject to physically awkward positions<ref name=":0" />. | ||
* | |||
* | |||
* | |||
== Clinical Presentation == | == Clinical Presentation == | ||
[[File:Lower-dermatomes.jpg|right|frameless]] | |||
<span style="line-height: 1.5em;">Patient with sciatica can present with neurological symptoms such as: </span> | <span style="line-height: 1.5em;">Patient with sciatica can present with neurological symptoms such as: </span> | ||
*<span style="line-height: 1.5em;">Pain (intense pain in the buttock)</span> | *<span style="line-height: 1.5em;">Pain (intense pain in the buttock)</span> | ||
| Line 52: | Line 43: | ||
*<span style="line-height: 1.5em;">Hot and cold or tinglings or burning sensations in the legs</span> | *<span style="line-height: 1.5em;">Hot and cold or tinglings or burning sensations in the legs</span> | ||
*<span style="line-height: 1.5em;">Reflex impairment</span> | *<span style="line-height: 1.5em;">Reflex impairment</span> | ||
*<span style="line-height: 1.5em;">Paresthesias or dysesthesias and oedema in the lower extremity that can be caused by the irritation of the sciatic nerves (the lumbar nerve L4 and L5 and the sacral nerves S1,S2 and S3).<ref name="Ardman et al." /><ref name="Jacobs et al.">Jacobs W. et al., Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review (of RCT’s) (1A)</ref><ref name="Ailianou et al." /> | *<span style="line-height: 1.5em;">Paresthesias or dysesthesias and oedema in the lower extremity that can be caused by the irritation of the sciatic nerves (the lumbar nerve L4 and L5 and the sacral nerves S1,S2 and S3).<ref name="Ardman et al.">Ardman C. et al., Sciatica Solutions: Diagnosis, treatment and cure of spinal and piriformis problems, 1st edition, W.W. Norton & Company, 2007</ref><ref name="Jacobs et al.">Jacobs W. et al., Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review (of RCT’s) (1A)</ref><ref name="Ailianou et al.">Ailianou A. et al., Review of the principal extra spinal pathologies causing sciatica and new MRI approaches., The Britisch Journal of Radiology, 2012, 85(1014): 672-681 (2C)</ref> | ||
<span style="line-height: 1.5em;">Sciatica symptoms can also differ, depending on which nerve is affected.</span> | <span style="line-height: 1.5em;">Sciatica symptoms can also differ, depending on which nerve is affected.</span> | ||
| Line 58: | Line 49: | ||
*L5: When the L5 nerve is compressed or irritated, the pain, tingling and numbness may extend to the foot and big toes.<br> | *L5: When the L5 nerve is compressed or irritated, the pain, tingling and numbness may extend to the foot and big toes.<br> | ||
*S1: When the S1 nerve is compressed or irritated, the patient feels pain, tingling and numbness on the outer part of the foot. The patient also experiences weakness when elevating the heel off the ground and standing on tiptoes. The ankle jerk reflex may be diminished. | *S1: When the S1 nerve is compressed or irritated, the patient feels pain, tingling and numbness on the outer part of the foot. The patient also experiences weakness when elevating the heel off the ground and standing on tiptoes. The ankle jerk reflex may be diminished. | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
A thorough differential list is important in considering a diagnosis of sciatica and should include. | |||
* Herniated lumbosacral disc | |||
* Muscle spasm | |||
* Nerve root impingement | |||
* Epidural abscess | |||
* Epidural hematoma | |||
* Tumor | |||
* [[Pott's Disease|Potts Disease]], also known as spinal tuberculosis | |||
* [[Piriformis Syndrome|Piriformis syndrome]]<ref name=":0" /> | |||
== Evaluation == | |||
Sciatica is most commonly diagnosed by:<br>1. History | |||
* Complaints of radiating pain in the leg, which follows a dermatomal pattern<ref name="Koes">B.W Koes, M.W Van Tulder, W.C Peul. Diagnosis and treatment of sciatica. BMJ, 23 JUNE 2007, VOLUME 334, p.1313-1314 (1A)</ref>. | |||
* Pain generally radiates below the knee, into the foot<ref name="Kika">Kika Konstantinou, Martyn Lewis, Kate M. Dunn. Agreement of self-reported items and clinically assessed nerve root involvement (or sciatica) in a primary care setting. Eur Spine J (2012) 21:2306–2315. (1B)</ref>. | |||
* Dermatome maps used to locate the distribution of the pain<ref name="Koes" />. | |||
Sciatica is most commonly diagnosed by:<br> | * Patients complain about low back pain, which is usually less severe than the leg pain<ref name="Koes" />. | ||
* Patients may also report sensory symptoms). | |||
2. Imaging (if warranted) | |||
* Plain films of the lumbosacral spine may evaluate for fracture or spondylolisthesis. | |||
* Noncontrast CT scan may be performed to evaluate fracture if plain films are negative. Pain that has been persistent for 6 to 8 weeks and not responding to conservative management should be imaged. | |||
* In cases where the neurologic deficit is the present or mass effect is suspected, immediate MRI is the standard of care in establishing the cause of the pain and ruling out pressing surgical pathology<ref name=":0" /> | |||
== Outcome Measures == | == Outcome Measures == | ||
*[[Oswestry Disability Index|The Oswestry Disability Index (ODI)<ref name="p0">Dionne CE. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. 2008</ref>]][[Sciatica|<span class="mw-reflink-text">[ | *[[Oswestry Disability Index|The Oswestry Disability Index (ODI)<ref name="p0">Dionne CE. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. 2008</ref>]][[Sciatica|<span class="mw-reflink-text">[11]</span>]][[Sciatica|<span class="mw-reflink-text">[10]</span>]][[Sciatica|<span class="mw-reflink-text">[10]</span>]][[Sciatica|<span class="mw-reflink-text">[10]</span>]][[Sciatica|<span class="mw-reflink-text">[10]</span>]][[Sciatica|<span class="mw-reflink-text">[10]</span>]]<span class="mw-reflink-text">[10]</span>. | ||
*[https://www.duo.uio.no/bitstream/handle/10852/28055/dravhandling-haugen.pdf?sequence=3 Sciatica Bothersomeness Index (SBI)<ref name="Patrick">Patrick DL. Assessing health-related quality of life in patients with sciatica. 1995 (2B)</ref>][[Sciatica|<span class="mw-reflink-text">[12]</span>]][[Sciatica|<span class="mw-reflink-text">[11]</span>]][[Sciatica|<span class="mw-reflink-text">[11]</span>]][[Sciatica|<span class="mw-reflink-text">[11]</span>]][[Sciatica|<span class="mw-reflink-text">[11]</span>]][[Sciatica|<span class="mw-reflink-text">[11]</span>]]<span class="mw-reflink-text">[11]</span>,<ref name="Grovle">Grøvle L. Reliability, validity, and responsiveness of the Norwegian versions of the Maine-Seattle Back Questionnaire and the Sciatica Bothersomeness and Frequency Indices. 2008. (2B)</ref> | |||
*[https://www.duo.uio.no/bitstream/handle/10852/28055/dravhandling-haugen.pdf?sequence=3 Sciatica Bothersomeness Index (SBI)<ref name="Patrick">Patrick DL. Assessing health-related quality of life in patients with sciatica. 1995 (2B)</ref>][[Sciatica|<span class="mw-reflink-text">[ | |||
== Examination == | == Examination == | ||
* | *See [[Lumbar Assessment]] | ||
== Medical Management == | == Medical Management == | ||
'''Patient Education''' | |||
* Use of hot or cold packs for comfort and to decreased inflammation | |||
* Avoidance of inciting activities or prolonged sitting/standing | |||
* Practicing good, erect posture | |||
* Engaging in exercises to increase core strength | |||
* Gentle stretching of the lumbar spine and hamstrings | |||
* Regular light exercises such as walking, swimming, or aquatherapy | |||
* Use of proper lifting techniques | |||
'''Medical Therapies''' | |||
* A short course of oral NSAIDs | |||
* Opioid and nonopioid analgesics | |||
* Muscle relaxants | |||
* Anticonvulsants for neurogenic pain | |||
* In the event oral NSAIDs are insufficient, a course of oral corticosteroids may be beneficial | |||
* Localized corticosteroid injections | |||
* Deep tissue massage may be helpful | |||
* Physical therapy consultation | |||
* Surgical evaluation and correction of any structural abnormalities such as disc herniation, epidural hematoma, epidural abscess or tumor | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
| Line 111: | Line 108: | ||
In most cases of sciatica, conservative treatment is favored. However, there is still some controversy surrounding it. The evidence does not show that one treatment is superior to the other<ref name="p2">Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Pim A. J. Luijsterburg, Arianne P. Verhagen, Raymond W. J. G. Ostelo, Ton A. G. van Os, Wilco C. Peul, Bart W. Koes. European Spine Journal July 2007, Volume 16, Issue 7, pp 881-899 (1A)</ref> (LOE 1A). Therefore we will discuss the several treatment options.<br> | In most cases of sciatica, conservative treatment is favored. However, there is still some controversy surrounding it. The evidence does not show that one treatment is superior to the other<ref name="p2">Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Pim A. J. Luijsterburg, Arianne P. Verhagen, Raymond W. J. G. Ostelo, Ton A. G. van Os, Wilco C. Peul, Bart W. Koes. European Spine Journal July 2007, Volume 16, Issue 7, pp 881-899 (1A)</ref> (LOE 1A). Therefore we will discuss the several treatment options.<br> | ||
A very important part of the therapy can be informing the patient about sciatica and giving him advice<ref name="p3" /> (LOE 2A),<ref name="p0" /> (LOE 5). But the education of sciatica is not yet investigated in randomized controlled trials<ref name="Koes" /> (LOE 1A),<ref name="p0" />. During therapy it is very important to give patients necessary information, advice them about staying active and give them information about treatment modalities. It is very important that the patient is physically an active participant in therapy and can take responsibility in the treatment process. The physical therapist also needs to be a coach for the patient<ref name="p4" /> (LOE 1A).<br> | A very important part of the therapy can be informing the patient about sciatica and giving him advice<ref name="p3">Lawrence M. Urban, BA, DPT. The Straight-Leg-Raising Test: A Review. JOSPT Vol. 2. No. 3, p.117-129</ref> (LOE 2A),<ref name="p0" /> (LOE 5). But the education of sciatica is not yet investigated in randomized controlled trials<ref name="Koes" /> (LOE 1A),<ref name="p0" />. During therapy it is very important to give patients necessary information, advice them about staying active and give them information about treatment modalities. It is very important that the patient is physically an active participant in therapy and can take responsibility in the treatment process. The physical therapist also needs to be a coach for the patient<ref name="p4">Jacobs W. et al., Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review (of RCT’s) (1A)</ref> (LOE 1A).<br> | ||
Corticosteroid injections and traction are two treatment options that have limited evidence and are therefore not recommended for the treatment of sciatica<ref name="p3" /> (LOE 2A),<ref name="p4" /> (LOE 1A),<ref name="p5" />. If we compare bed rest as a treatment for sciatica with doing nothing at all, there seems to be no difference. On a short term there is no difference regarding overall improvement and pain and disability<ref name="p2" /> (LOE 1A),<ref name="p6" /> (LOE 1A),<ref name="p0" /> (LOE 5).<br> | Corticosteroid injections and traction are two treatment options that have limited evidence and are therefore not recommended for the treatment of sciatica<ref name="p3" /> (LOE 2A),<ref name="p4" /> (LOE 1A),<ref name="p5">Sciatica (lumbar radiculopathy) - Management". http://www.cks.nhs.uk/sciatica_lumbar_radiculopathy/management/scenario_sciatica_lumbar_radiculopathy/treatment/basis_for_recommendation.</ref>. If we compare bed rest as a treatment for sciatica with doing nothing at all, there seems to be no difference. On a short term there is no difference regarding overall improvement and pain and disability<ref name="p2" /> (LOE 1A),<ref name="p6">Vroomen, PC; De Krom, MC; Slofstra, PD; Knottnerus, JA (2000). "Conservative treatment of sciatica: a systematic review". Journal of Spinal Disorders 13 (6): 463–469. doi:10.1097/00002517-200012000-00001. PMID 11132976. (1A)</ref> (LOE 1A),<ref name="p0" /> (LOE 5).<br> | ||
In a few articles acupuncture has been proven to reduce pain in the back. The practice is centered on the philosophy of achieving or maintaining well being through the open flow of energy via specific pathways in the body. Hair-thin needles are inserted into the skin near the area of pain<ref name="p7" />(LOE 1A) <ref name="p8" />(LOE 2C) <ref name="p0" />(LOE 5). Other articles have found no reduction of pain with acupuncture<ref name="p2" />.<br> | In a few articles acupuncture has been proven to reduce pain in the back. The practice is centered on the philosophy of achieving or maintaining well being through the open flow of energy via specific pathways in the body. Hair-thin needles are inserted into the skin near the area of pain<ref name="p7">Roelofs, Pepijn DDM; Deyo, Rick A; Koes, Bart W; Scholten, Rob JPM; Van Tulder, Maurits W (2008). "Non-steroidal anti-inflammatory drugs for low back pain". In Roelofs, Pepijn DDM. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD000396.pub3. PMID 18253976. (1A)</ref>(LOE 1A) <ref name="p8">Kenneth Jeffrey Miller DC, DABCO. Physical assessment of lower extremity radiculopathy and sciatica. Journal of Chiropractic Medicine (2007) 6, 75–82 (2C)</ref>(LOE 2C) <ref name="p0" />(LOE 5). Other articles have found no reduction of pain with acupuncture<ref name="p2" />.<br> | ||
Massage therapy has proven to be useful with the treatment of back pain. It promotes blood circulation, muscle relaxation and the release of endorphins<ref name="p9" />(LOE 1B),<ref name="p0" />(LOE 5),<ref name="p1" />. <br> | Massage therapy has proven to be useful with the treatment of back pain. It promotes blood circulation, muscle relaxation and the release of endorphins<ref name="p9">Abdelilah el Barzouhi, M.D., Carmen L.A.M. Vleggeert-Lankamp, M.D., Ph.D., Geert J. Lycklama, Nijeholt, M.D., Ph.D., Bas F. Van der Kallen, M.D.,Wilbert B. van den Hout, Ph.D., Wilco C.H. Jacobs, Ph.D.,Bart W. Koes, Ph.D., and Wilco C. Peul, M.D., Ph.D. Magnetic Resonance Imaging in Follow-up Assessment of Sciatica. New England Journal of Medicine, 368;11 nejm.org march 14, 2013, P.1000 (1B)</ref>(LOE 1B),<ref name="p0" />(LOE 5),<ref name="p1">John Barrett,Douglas Noel Golding. The practical treatment of backache and sciatica. Redwood Burn Limited. 1984.p97-103.</ref>. <br> | ||
<u>Herniated Disc Sciatica Management</u>: | <u>Herniated Disc Sciatica Management</u>: | ||
Revision as of 00:25, 13 September 2020
Description[edit | edit source]
Sciatica is a debilitating condition in which the patient experiences pain and/or paresthesias in the distribution of the sciatic nerve or an associated lumbosacral nerve root.
- A common mistake is referring to any low back pain or radicular leg pain as sciatica.
- Sciatica is specific to the pain that is a direct result of sciatic nerve or sciatic nerve root pathology.
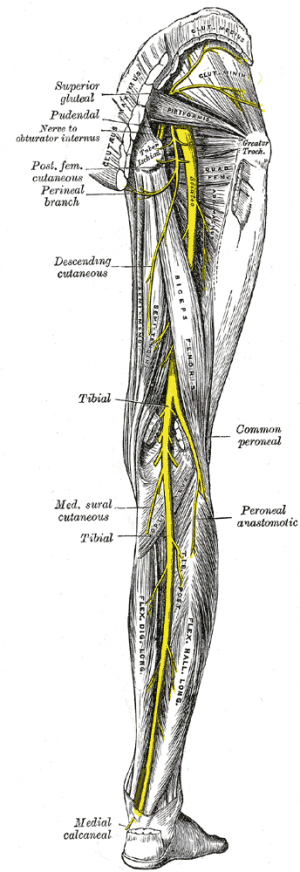
The sciatic nerve is made up of the L4 through S2 nerve roots which coalesce at the pelvis to form the sciatic nerve. At up to 2 cm in diameter, the sciatic nerve is easily the largest nerve in the body.
- Sciatica pain often is worsened with flexion of the lumbar spine, twisting, bending, or coughing.
- The sciatic nerve provides direct motor function to the hamstrings, lower extremity adductors, and indirect motor function to the calf muscles, anterior lower leg muscles, and some intrinsic foot muscles.
- Indirectly through its terminal branches, the sciatic nerve provides sensation to the posterior and lateral lower leg as well as the plantar foot.
Most cases of sciatica result from an inflammatory condition leading to an irritation of the sciatic nerve. [1]
Etiology[edit | edit source]
Any condition that may structurally impact or compress the sciatic nerve may cause sciatica symptoms.
- The most common cause of sciatica is a herniated or bulging lumbar intervertebral disc.
- In the older persons, lumbar spinal stenosis may cause these symptoms as well.
- Spondylolisthesis or a relative misalignment of one vertebra relative to another may also result in sciatic symptoms.
- Lumbar or pelvic muscular spasm and/or inflammation may impinge a lumbar or sacral nerve root causing sciatic symptoms.
- A spinal or paraspinal mass including malignancy, epidural hematoma, or epidural abscess may also cause a mass-like effect and sciatica symptoms[1]
Epidemiology[edit | edit source]
- No gender predominance
- Peak incidence occurs in patients in their fourth decade
- Lifetime incidence reported between 10% to 40%
- Annual incidence of 1% to 5%
- No association with body height has been established except in the age 50 to 60 group.
- Rarely occurs before age 20 (unless traumatic)
- Physical activity increases incidence in those with prior sciatic symptoms and decreased in those with no prior symptoms.
- Occupational predisposition has been shown in machine operators, truck drivers, and jobs where workers are subject to physically awkward positions[1].
Clinical Presentation[edit | edit source]
Patient with sciatica can present with neurological symptoms such as:
- Pain (intense pain in the buttock)
- Lumbosacral radicular leg pain
- Numbness
- Muscular weakness
- Gait dysfunction
- Sensory impairment
- Sensory disturbance
- Hot and cold or tinglings or burning sensations in the legs
- Reflex impairment
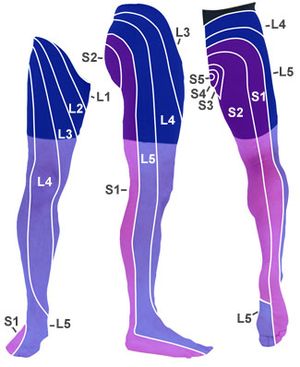
- Paresthesias or dysesthesias and oedema in the lower extremity that can be caused by the irritation of the sciatic nerves (the lumbar nerve L4 and L5 and the sacral nerves S1,S2 and S3).[2][3][4]
Sciatica symptoms can also differ, depending on which nerve is affected.
- L4: When the L4 nerve is compressed or irritated, the patient feels pain, tingling and numbness in the thigh. The patient also feels weak when straightening the leg and may have a diminished knee jerk reflex.
- L5: When the L5 nerve is compressed or irritated, the pain, tingling and numbness may extend to the foot and big toes.
- S1: When the S1 nerve is compressed or irritated, the patient feels pain, tingling and numbness on the outer part of the foot. The patient also experiences weakness when elevating the heel off the ground and standing on tiptoes. The ankle jerk reflex may be diminished.
Differential Diagnosis[edit | edit source]
A thorough differential list is important in considering a diagnosis of sciatica and should include.
- Herniated lumbosacral disc
- Muscle spasm
- Nerve root impingement
- Epidural abscess
- Epidural hematoma
- Tumor
- Potts Disease, also known as spinal tuberculosis
- Piriformis syndrome[1]
Evaluation[edit | edit source]
Sciatica is most commonly diagnosed by:
1. History
- Complaints of radiating pain in the leg, which follows a dermatomal pattern[5].
- Pain generally radiates below the knee, into the foot[6].
- Dermatome maps used to locate the distribution of the pain[5].
- Patients complain about low back pain, which is usually less severe than the leg pain[5].
- Patients may also report sensory symptoms).
2. Imaging (if warranted)
- Plain films of the lumbosacral spine may evaluate for fracture or spondylolisthesis.
- Noncontrast CT scan may be performed to evaluate fracture if plain films are negative. Pain that has been persistent for 6 to 8 weeks and not responding to conservative management should be imaged.
- In cases where the neurologic deficit is the present or mass effect is suspected, immediate MRI is the standard of care in establishing the cause of the pain and ruling out pressing surgical pathology[1]
Outcome Measures[edit | edit source]
- The Oswestry Disability Index (ODI)[7][11][10][10][10][10][10][10].
- Sciatica Bothersomeness Index (SBI)[8][12][11][11][11][11][11][11],[9]
Examination[edit | edit source]
Medical Management[edit | edit source]
Patient Education
- Use of hot or cold packs for comfort and to decreased inflammation
- Avoidance of inciting activities or prolonged sitting/standing
- Practicing good, erect posture
- Engaging in exercises to increase core strength
- Gentle stretching of the lumbar spine and hamstrings
- Regular light exercises such as walking, swimming, or aquatherapy
- Use of proper lifting techniques
Medical Therapies
- A short course of oral NSAIDs
- Opioid and nonopioid analgesics
- Muscle relaxants
- Anticonvulsants for neurogenic pain
- In the event oral NSAIDs are insufficient, a course of oral corticosteroids may be beneficial
- Localized corticosteroid injections
- Deep tissue massage may be helpful
- Physical therapy consultation
- Surgical evaluation and correction of any structural abnormalities such as disc herniation, epidural hematoma, epidural abscess or tumor
Physical Therapy Management[edit | edit source]
In most cases of sciatica, conservative treatment is favored. However, there is still some controversy surrounding it. The evidence does not show that one treatment is superior to the other[10] (LOE 1A). Therefore we will discuss the several treatment options.
A very important part of the therapy can be informing the patient about sciatica and giving him advice[11] (LOE 2A),[7] (LOE 5). But the education of sciatica is not yet investigated in randomized controlled trials[5] (LOE 1A),[7]. During therapy it is very important to give patients necessary information, advice them about staying active and give them information about treatment modalities. It is very important that the patient is physically an active participant in therapy and can take responsibility in the treatment process. The physical therapist also needs to be a coach for the patient[12] (LOE 1A).
Corticosteroid injections and traction are two treatment options that have limited evidence and are therefore not recommended for the treatment of sciatica[11] (LOE 2A),[12] (LOE 1A),[13]. If we compare bed rest as a treatment for sciatica with doing nothing at all, there seems to be no difference. On a short term there is no difference regarding overall improvement and pain and disability[10] (LOE 1A),[14] (LOE 1A),[7] (LOE 5).
In a few articles acupuncture has been proven to reduce pain in the back. The practice is centered on the philosophy of achieving or maintaining well being through the open flow of energy via specific pathways in the body. Hair-thin needles are inserted into the skin near the area of pain[15](LOE 1A) [16](LOE 2C) [7](LOE 5). Other articles have found no reduction of pain with acupuncture[10].
Massage therapy has proven to be useful with the treatment of back pain. It promotes blood circulation, muscle relaxation and the release of endorphins[17](LOE 1B),[7](LOE 5),[18].
Herniated Disc Sciatica Management:
- Extension exercises or press ups are often prescribed; for example, Upper Back Extension[10](LOE 1A).
Spinal Stenosis Sciatica Management:
- Flexion exercises of the lower back are suggested. Flexing the lower spine opens the spinal canal and allows the irritation or impingement to resolve. Stretching exercises for the back are forward flexion. For strengthening the abdominal muscles Hook-lying March and Curl-Ups exercises are frequently used[11](LOE 2A).
There is no evidence found for this management. Physical therapists use these exercises since it has been shown to have efficacy for some patients.
Degenerative Disc Disease Sciatica Management:
- A dynamic lumbar stabilization program is recommended. Through this program the patient finds the most comfortable position for the lumbar spine and pelvis and attempts to maintain this position during activities. When performed correctly, this exercise can improve the proprioception of the lumbar spine and reduce the excess motion at the spinal segments. This reduces the amount of irritation at these segments, relieving pain and protecting the area from further damage. Examples of these exercises are; Hook-lying March, Hook-lying March Combination and Bridging[11](LOE 2A).
Spondylolisthesis Sciatica Management:
- Flexion based exercises and stabilization exercises are included in this program. The objective of this program is to improve the stability of the lumbar spine in flexed positions. A few examples of exercises are: Hooked-lying March; Curl-Ups and Pelvic Tilt[11](LOE 2A),[12](LOE 1A).
Piriformis Syndrome Sciatica Management:
- Stretching the piriformis muscle, hamstring muscles and hip extensor muscles may decrease and improve range of motion[11](LOE 2A).
There is no evidence found for this management. Physical therapists use these exercises since it has been shown to have some efficacy for some patients.
Sacroiliac Joint Dysfunction Sciatica Management:
- This management strategy consists of range of motion exercises for the SI joint; this can help restore normal movement and alleviate irritation of the sciatic nerve. The three most important exercises are: Single Knee to Chest Stretch[13]; Press-Up and Lumbar Rotation[14](LOE 1A) (non-weight bearing).
Chiropractic treatment is based on the hypothesis that vertebral decompression can be prevented by a flexion-distraction procedure. During this procedure, there is greater intervertebral space and less compression on the vertebral elements: for example, the patient lies on his/her stomach with a little flexion in the spine and due to downward flexion a distraction occurs. It has been proven that this treatment decreases the interdiscal pressure[15](LOE 1A),[16](LOE 2C)
A study by Albert et al examined the efficacy of systematic active conservative treatment. Two treatments contained identical information and advice, but differed in the type of exercise program.
- Treatment 1 contained symptom-guided exercises. These consisted of back-related exercises[17](LOE 1B).
- The patient’s directional preference guided the directional end-range exercise[17],[18] and
postural instructions (based on the McKenzie method of assessing pain-related-physical impairment)[17].
- Stabilizing exercises[17],[18] for the transverse abdominis and multifidus muscles[17].
- Dynamic exercises for the outer layers of the abdominal wall and back extensors.
You can see the full treatment strategies and exercises in the link below: treatment program sciatica (→ Link plaatsen)
There is no evidence found for these exercises but physical therapists use these exercises since it has been shown to have some efficacy for some patients.
- Treatment 2 contained Sham exercises. The exercises were not back related and were low-dose exercises to stimulate an increase in systemic blood circulation. Examples of exercises:
- Exercise 1: Squeeze buttocks
The patient lies supine and squeezes the buttocks. Contraction is held for 5 seconds. The exercises are repeated 10 times.
The patient only contracts the gluteal muscles.
- Exercise 2: Swing
The patient is standing with the legs slightly apart. The shoulders are relaxed and the patient swings the arms loosely
alongside the body. This exercise is repeated 20 times.
You can see the full document of Sham exercises below: Sham exercises (→ Link plaatsen)
There is no evidence found for these exercises but physical therapists use these exercises since it has been shown to have some efficacy for some patients.
The patients had more faith in the Sham exercises but the outcomes of the symptom-guided exercise treatment were better. This cannot be used as an standard procedure because every patient is different and reacts differently to treatment[17](LOE 1B).
Key Research[edit | edit source]
- Genevay S, Finckh A, Zufferey P, Viatte S, Balagué F, Gabay C. Adalimumab. In acute sciatica reduces the long-term need for surgery: a 3-year follow-up of a randomised double-blind placebo-controlled trial. 2011 Oct 13.(C)
- Ashworth J, Konstantinou K, Dunn KM. Prognostic Factors in Non-Surgically Treated Sciatica: A Systematic Review. 2011 Sep 25.(A1)
- Wassenaar M, van Rijn RM, van Tulder MW, Verhagen AP, van der Windt DA, Koes BW, de Boer MR, Ginai AZ, Ostelo RW. Magnetic resonance imaging for diagnosing lumbar spinal pathology in adult patients with low back pain or sciatica: a diagnostic systematic review. 2011 Sep 16.(A1)
- Van Rijn RM, Wassenaar M, Verhagen AP, Ostelo RW, Ginai AZ, de Boer MR, van Tulder MW, Koes BW. Computed tomography for the diagnosis of lumbar spinal pathology in adult patients with low back pain or sciatica: a diagnostic systematic review. 2011 Sep 14.(A1)
- Righesso O, Falavigna A, Avanzi O. Correlation between persistent neurological impairment and clinical outcome following microdiscectomy for treatment of lumbar disc herniation. 2011 Aug 10.(C)
- Erginousakis D, Filippiadis DK, Malagari A, Kostakos A, Brountzos E, Kelekis NL, Kelekis A. Comparative prospective randomized study comparing conservative treatment and percutaneous disc decompression for treatment of intervertebral disc herniation. 2011 Aug.(B)
Resources[edit | edit source]
- Loren Fishman, Carol Ardman. Sciatica Solutions: Diagnosis, Treatment, and Cure of Spinal and Piriformis Problems. W W Norton & Co Inc. 2007. (D)
- John Barrett, Douglas Noel Golding. The practical treatment of backache and sciatica.1984. (D)
- Larry P. Credit,Sharon G. Hartunian,Margaret J. Nowak .Relieving sciatica. Old Broadway.2000.p 30-34. (D)
- http://www.spinecentre.com.hk/thumbnail-list-layout-en/case-study-2-sciatica-and-disc-protrusion#2 - Sciatica and Disc Protrusion[19]
Clinical Bottom Line[edit | edit source]
add text here
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Davis DH, Wilkinson JT, Teaford AK, Smigiel MR. Sciatica produced by a sacral perineurial cyst. Texas Medicine. 1987 Mar 1;83(3):55-6.Available from:https://www.statpearls.com/kb/viewarticle/28772/ (last accessed 12.9.2020)
- ↑ Ardman C. et al., Sciatica Solutions: Diagnosis, treatment and cure of spinal and piriformis problems, 1st edition, W.W. Norton & Company, 2007
- ↑ Jacobs W. et al., Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review (of RCT’s) (1A)
- ↑ Ailianou A. et al., Review of the principal extra spinal pathologies causing sciatica and new MRI approaches., The Britisch Journal of Radiology, 2012, 85(1014): 672-681 (2C)
- ↑ 5.0 5.1 5.2 5.3 B.W Koes, M.W Van Tulder, W.C Peul. Diagnosis and treatment of sciatica. BMJ, 23 JUNE 2007, VOLUME 334, p.1313-1314 (1A)
- ↑ Kika Konstantinou, Martyn Lewis, Kate M. Dunn. Agreement of self-reported items and clinically assessed nerve root involvement (or sciatica) in a primary care setting. Eur Spine J (2012) 21:2306–2315. (1B)
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Dionne CE. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. 2008
- ↑ Patrick DL. Assessing health-related quality of life in patients with sciatica. 1995 (2B)
- ↑ Grøvle L. Reliability, validity, and responsiveness of the Norwegian versions of the Maine-Seattle Back Questionnaire and the Sciatica Bothersomeness and Frequency Indices. 2008. (2B)
- ↑ 10.0 10.1 10.2 10.3 Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Pim A. J. Luijsterburg, Arianne P. Verhagen, Raymond W. J. G. Ostelo, Ton A. G. van Os, Wilco C. Peul, Bart W. Koes. European Spine Journal July 2007, Volume 16, Issue 7, pp 881-899 (1A)
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 Lawrence M. Urban, BA, DPT. The Straight-Leg-Raising Test: A Review. JOSPT Vol. 2. No. 3, p.117-129
- ↑ 12.0 12.1 12.2 Jacobs W. et al., Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review (of RCT’s) (1A)
- ↑ 13.0 13.1 Sciatica (lumbar radiculopathy) - Management". http://www.cks.nhs.uk/sciatica_lumbar_radiculopathy/management/scenario_sciatica_lumbar_radiculopathy/treatment/basis_for_recommendation.
- ↑ 14.0 14.1 Vroomen, PC; De Krom, MC; Slofstra, PD; Knottnerus, JA (2000). "Conservative treatment of sciatica: a systematic review". Journal of Spinal Disorders 13 (6): 463–469. doi:10.1097/00002517-200012000-00001. PMID 11132976. (1A)
- ↑ 15.0 15.1 Roelofs, Pepijn DDM; Deyo, Rick A; Koes, Bart W; Scholten, Rob JPM; Van Tulder, Maurits W (2008). "Non-steroidal anti-inflammatory drugs for low back pain". In Roelofs, Pepijn DDM. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD000396.pub3. PMID 18253976. (1A)
- ↑ 16.0 16.1 Kenneth Jeffrey Miller DC, DABCO. Physical assessment of lower extremity radiculopathy and sciatica. Journal of Chiropractic Medicine (2007) 6, 75–82 (2C)
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 Abdelilah el Barzouhi, M.D., Carmen L.A.M. Vleggeert-Lankamp, M.D., Ph.D., Geert J. Lycklama, Nijeholt, M.D., Ph.D., Bas F. Van der Kallen, M.D.,Wilbert B. van den Hout, Ph.D., Wilco C.H. Jacobs, Ph.D.,Bart W. Koes, Ph.D., and Wilco C. Peul, M.D., Ph.D. Magnetic Resonance Imaging in Follow-up Assessment of Sciatica. New England Journal of Medicine, 368;11 nejm.org march 14, 2013, P.1000 (1B)
- ↑ 18.0 18.1 18.2 John Barrett,Douglas Noel Golding. The practical treatment of backache and sciatica. Redwood Burn Limited. 1984.p97-103.
- ↑ Hong Kong Spine Centre. Clinical Case Studies:case study #2: Sciatica and Disc Protrusion.http://www.spinecentre.com.hk/thumbnail-list-layout-en/case-study-2-sciatica-and-disc-protrusion. (accessed 17 August 2013)