Posture: Difference between revisions
Kim Jackson (talk | contribs) (Updated references) |
Tony Varela (talk | contribs) (Corrections to intext citations) |
||
| (70 intermediate revisions by 13 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- The [[Open Physio]] project '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}<br> | |||
</div><blockquote>Welcome to [[Arkansas Colleges of Health Education School of Physical Therapy Musculoskeletal 1 Project|Arkansas Colleges of Health Education School of Physical Therapy Musculoskeletal 1 Project]]. This space was created by and for the students at Arkansas Colleges of Health Education School in the United States. Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!</blockquote> | |||
< | == Introduction == | ||
[[File:Indian-yogi-yogi-madhav-P SxnJhID1s-unsplash (1).jpg|right|frameless]] | |||
Posture is a highly individual and dynamic aspect of human physiology. It is more about how your body adapts and interacts with different situations than a fixed 'correct' or 'incorrect' state. Posture can be simply defined as the way in which we hold our bodies while standing, sitting, or lying down.<ref>Caneiro, J. P., O'Sullivan, P., Burnett, A., Barach, A., O'Neil, D., Tveit, O., & Olafsdottir, K. (2010). The influence of different sitting postures on head/neck posture and muscle activity. Manual Therapy, 15(1), 54-60</ref> | |||
A growing body of research suggests that the concept of a 'bad posture' is subjective, and there is no definitive link between specific postural habits and pain.<ref>Slater D, Korakakis V, O'Sullivan P, Nolan D, O'Sullivan K. “Sit up straight”: time to re-evaluate. journal of orthopaedic & sports physical therapy. 2019 Aug;49(8):562-4.</ref> In fact, posture varies greatly among individuals, and what may be considered a 'good posture' for one person may not work or feel comfortable for another.<ref>Barrett, E., O'Keeffe, M., O'Sullivan, K., Lewis, J., & McCreesh, K. (2016). Is thoracic spine posture associated with shoulder pain, range of motion and function? A systematic review. Manual Therapy, 26, 38-46</ref> | |||
=== '''What is Posture?''' === | |||
Posture is the attitude assumed by the body either with support during muscular inactivity, or the coordinated action of many [[Muscle|muscles]] working to maintain stability. It forms an essential basis that is being adapted constantly.<ref name=":1">Gardiner, Mary Dena. (1973). ''The principles of exercise therapy''. London : Bell</ref> | |||
Our posture is an active process involving not only our muscles and [[Joint Classification|joints]] but also our perception, emotions, and the environment we are in. Even seemingly static positions, like sitting or standing, are full of tiny adjustments and movements.<ref>Dunk, N. M., Callaghan, J. P., & McGill, S. M. (2005). Lumbar spine movement patterns during prolonged sitting differentiate low back pain developers from matched asymptomatic controls. Work, 24(2), 181-188.</ref> | |||
'''Inactive Posture:''' Describe postures adopted during resting or sleeping, and they are more suitable for this purpose when all the essential muscular activity required to maintain life is reduced to a minimum. | |||
'''Active Posture:''' The integrated action of many muscles is required to maintain active postures, which may be either static or dynamic.<ref name=":1" /> | |||
#'''Static posture-''' the body and its segments are aligned and maintained in certain positions. Examples include standing, sitting, lying, and kneeling. | |||
# '''Dynamic posture-''' the body or its segments are moving—walking, running, jumping, throwing, and lifting. | |||
== Understanding 'Good' and 'Bad' Posture == | |||
[[File:Posture .gif|frame|Optimal posture]]The traditional view of posture insists on a 'correct' or 'incorrect' way to hold one's body, often associated with ideas about aesthetics, fitness, or health. However, current research indicates that this may be an oversimplified view. | |||
Several studies have found no consistent link between posture and musculoskeletal pain<ref>Dankaerts, W., O'Sullivan, P., Burnett, A., Straker, L., & Davey, P. (2007). Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine, 32(6), 698-704.</ref>, questioning the widely held belief that 'bad posture' leads to back or neck pain. This includes research showing no clear correlation between postural deviations and pain among adolescents<ref>Dolphens, M., Cagnie, B., Coorevits, P., Vanderstraeten, G., Cardon, G., D'hooge, R., & Danneels, L. (2012). Sagittal standing posture and its association with spinal pain: a school-based epidemiological study of 1196 Flemish adolescents before age at peak height velocity. Spine, 37(19), 1657-1666.</ref>, and studies showing that correcting posture does not necessarily alleviate chronic pain.<ref>Christensen, S. T., & Hartvigsen, J. (2008). Spinal curves and health: a systematic critical review of the epidemiological literature dealing with associations between sagittal spinal curves and health. Journal of Manipulative and Physiological Therapeutics, 31(9), 690-714</ref> | |||
The emerging view in physiotherapy and related fields is that rather than striving for an arbitrarily 'ideal' posture, it may be more beneficial to cultivate postural variability - the ability to comfortably change and adapt one's posture to different situations.<ref>Burgess-Limerick, R., Plooy, A., Fraser, K., & Hargreaves, M. (2000). The influence of computer monitor height on head and neck posture. International Journal of Industrial Ergonomics, 25(3), 339-345</ref> Indeed, according to some ergonomists, "your next posture is your best posture." Alternating between sitting and standing may practically eliminate lower back pain while easing pressure on the vertebrae and improving blood flow to the legs. | |||
== Optimizing Posture (The Importance of the Pelvic Girdle) == | |||
According to Vleeming et al., the sacral base is the geometric center of the postural system. Unlevelness of the base of the sacrum contributes to decreased postural balance and can be a chronic postural stressor. If posture is misaligned, to maintain postural balance, the lumbar spine tends to angle laterally and concave towards the high side of the sacral base. <ref>Mooney V, Stoeckart R, Vleeming A. Movement, stability & lumbopelvic pain: integration of research and therapy. Edinburgh; New York: Churchill Livingstone Elsevier, 2007. | |||
</ref> | |||
Impairments that can cause unlevelness of the base of the sacrum include, but are not limited to: | |||
* Leg length discrepancies | |||
** If there is a leg length discrepancy, the pelvis will present as asymmetrical.<ref name=":4">Magee D, Manske R. Orthopedic physical assessment. St. Louis: Elsevier. 2021. </ref> | |||
* [[Piriformis syndrome]] | |||
** Piriformis syndrome has the ability to increase the tension on muscles of the pelvis as they try to stabilize the pelvis and the spine. This can throw the sacral base off of its geometric center.<ref>Boyle P, Weitz M. editors. Dutton’s orthopaedic examination evaluation and intervention. McGraw-Hill. 2019.</ref> | |||
* Tight adductor muscles | |||
** Tight or weak hip adductors can cause a lateral pelvic tilt, which leads to issues with long-standing and standing posture.<ref name=":4" /> | |||
* Asymmetrical dynamic postures | |||
** A common asymmetrical dynamic posture is generally identified as the "Statue of David" posture. During this, one lower extremity is externally rotated, which potentially causes weakness in the internal rotators of the hip, and the opposing lower extremity is internally rotated, potentially causing weakness in the external rotators of the hip. To combat these weaknesses, strengthening of the weaker muscles is recommended. | |||
== Posture and Health == | |||
[[File:Engin-akyurt-hkd1xxzyQKw-unsplash.jpg|right|frameless|400x400px]] | |||
Poor posture can be bad for your health. Maintaining a posture that puts stress on a joint such as prolonged slouching (see image at R) or slumping over can: | |||
* Increase pressure on the spine, making it more prone to injury and degeneration | |||
* Cause neck, shoulder, and back pain<ref name=":2">Kang BR, Her JG, Lee JS, Ko TS, You YY. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6378006/ Effects of the computer desk level on the musculoskeletal discomfort of neck and upper extremities and EMG activities in patients with spinal cord injuries]. Occupational therapy international. 2019 Feb 3;2019.</ref><ref>Borhany T, Shahid E, Siddique WA, Ali H. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6060916/pdf/JFMPC-7-337.pdf Musculoskeletal problems in frequent computer and internet users.] Journal of family medicine and primary care. 2018 Mar;7(2):337.</ref><ref>Daneshmandi H, Choobineh A, Ghaem H, Karimi M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5618737/pdf/jlm-07-069.pdf Adverse effects of prolonged sitting behavior on the general health of office workers]. Journal of lifestyle medicine. 2017 Jul;7(2):69.</ref> | |||
* Decrease flexibility | |||
* Affect how well joints move | |||
* Affect [[balance]] and increase risk of [[Falls|falling]] | |||
* Make it harder to digest food | |||
* Induce breathing disorder and affect surrounding structures including the [[Anatomy of the Human Heart|heart]] and [[Phrenic Nerve|phrenic]] nerve<ref>Albarrati A, Zafar H, Alghadir AH, Anwer S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5845520/ Effect of upright and slouched sitting postures on the respiratory muscle strength in healthy young males.] BioMed research international. 2018 Feb 25;2018.</ref> | |||
* In women it can lead to imbalance in the core muscle leading to [[incontinence]] and/or pelvic organ prolapse | |||
'''Age-Related Postural Changes''' | |||
[[Ageing and the Locomotor System|Ageing]] inevitably affects posture. The main contributing factors for postural instability are:<ref>Fernandes VL, Ribeiro DM, Fernandes LC, Menezes RL. [https://www.scielo.br/j/fm/a/mmzJ63RxVcmrcrhnSSLF7bK/?lang=en Postural changes versus balance control and falls in community-living older adults: a systematic review.] Fisioterapia em Movimento. 2018 Jun 7;31.</ref> | |||
* Thoracic [[Thoracic Hyperkyphosis|hyperkyphosis]] | |||
* Loss of lumbar lordosis | |||
* Decreased plantar arch | |||
== The Importance of Posture in Different Populations == | |||
Geriatric Patients: | |||
For geriatric patients, it is important for physical therapists to focus on muscle imbalance and alignments which will better improve their overall posture and balance. <ref name=":8">Hsu WL, Chen CY, Tsauo JY, Yang RS. Balance control in elderly people with osteoporosis. Journal of the Formosan Medical Association. 2014 Jun;113(6):334–9. | |||
</ref> As we age, we begin to lose our height. This is due to our vertebrae and disc breaking down and our connective tissue beginning to lose their stretch. <ref>Ahmed T, Haboubi N. Assessment and management of nutrition in older people and its importance to health. Clinical Interventions in Aging. 2010 Jul;5:207. | |||
</ref> | |||
Overall improvement of their posture can lead to: | |||
* Improved balance, decreased fall risk <ref name=":8" /> | |||
* Prevents osteoporosis <ref name=":8" /> | |||
* Decreased feelings of depression <ref name=":5">Matthieu Casteran, Alain Putot, François Pfitzenmeyer, Thomas E, Manckoundia P. Analysis of the impact of a cognitive task on the posture of elderly subjects with depression compared with healthy elderly subjects. Clinical neurophysiology. 2016 Nov 1;127(11):3406–11. | |||
</ref> | |||
* Increased cognitive function <ref name=":5" /> | |||
Pediatric Patients: | |||
It is important for children to have good posture to help prevent any dysfunctions to their developing bodies. In order to improve their posture, children should regularly participate in exercise.<ref name=":9" /> A child’s posture can be influenced by:<ref name=":9">Good posture and Spine Care in children. Royal Children’s Hospital. Victorian Paediatric Orthopaedic; 2011. | |||
</ref> | |||
* Activity level | |||
* Age and gender | |||
* Self-confidence | |||
* Height | |||
* Weight | |||
* Seating equipment at school and home | |||
* The weight and size of their backpack | |||
Athletic Posture: | |||
Athletes are expected to maintain high energy over an extended amount of time. During this time, they should be able to demonstrate agility, while also effectively playing their role or position. Due to this, an athletic stance is an example of the dynamic aspect of posture. Poor posture in athletics can limit their range of motion, causing them to generate less power and perform poorly. Having poor posture while performing these dynamic movements increases the chances for an athlete to be injured<ref>Dawid Koźlenia, Katarzyna Kochan-Jacheć. The Impact of Interaction between Body Posture and Movement Pattern Quality on Injuries in Amateur Athletes. Journal of clinical medicine. 2024 Mar 2;13(5):1456–6. | |||
</ref>. An athlete’s posture differs from a regular posture. An athletic stance allows players to be ready for any movement they need to perform. A proper athletic stance is as follows: <ref name=":6">Athletic stance [Internet]. 205 Sports. Available from: <nowiki>https://205sports.org/player-development/205-training/ltad/athletic-stance/</nowiki> | |||
</ref> | |||
[[File:Screenshot 2024-04-06 9.15.26 PM.png|thumb|Athletic Stance]] | |||
* Feet hip-width apart to shoulder-width apart | |||
* Quarter-squat position | |||
* Body weight evenly distributed through both feet | |||
* Center of gravity directly above base of support | |||
* Shoulders level | |||
* Torso flat and at a slightly bent vertical 75° incline | |||
Teaching proper athletic posture is fundamentally important to an athlete’s ability to practice and effectively perform the skills necessary to fulfill the requirement of any sport activity.<ref name=":6" /> | |||
Neurologic Patients: | |||
The importance of posture in patients with spinal cord injury (SCI) is to allow them to participate in their daily activities without the possibility of them injuring themself or creating chronic issues.<ref name=":7">Innovation A for C. The importance of posture for SCI clients [Internet]. aci.health.nsw.gov.au. 2017. Available from: <nowiki>https://aci.health.nsw.gov.au/networks/spinal-cord-injury/spinal-seating/module-7/the-importance-of-posture-for-sci-clients</nowiki> | |||
= | </ref> Physical therapists should observe patients' functional capability, postural support, and comfort.<ref name=":7" /> Any patient presenting these signs should be assessed:<ref name=":7" /> | ||
* Current or recurring pressure injuries | |||
* Pain and discomfort with sitting | |||
* Risk of falls and safety concerns of client or their caregivers | |||
* Postural asymmetry and risk of fixed deformity | |||
* Difficulty with balance during static sitting, dynamic tasks, or when attempting weight shift for pressure management | |||
* Changes in body size | |||
* Reduced function | |||
* Replacement of seating and wheeled mobility system | |||
* Posture-related aspirations | |||
* Respiratory restrictions | |||
Through assessing a patient with SCI, the physical therapist is able to make the appropriate choice of wheelchair and seat for the patient, if required. <ref>Wadhwa G, Aikat R. Development, validity and reliability of the “Sitting Balance Measure” (SBM) in spinal cord injury. Spinal Cord. 2015 Oct 13;54(4):319–23. | |||
</ref> | |||
== Physiotherapy == | |||
Rather than 'correcting' posture, physiotherapy can play a crucial role in improving postural awareness and promoting postural variability. Physiotherapists can help individuals explore a range of postures and movements, enhancing their ability to adapt to different activities and environments comfortably. | |||
Important advice could include: | |||
* Be mindful of posture during everyday activities, like watching television, washing dishes, or walking | |||
* Stay active. Any kind of exercise may help improve your posture, but certain types of exercises can be especially helpful. eg. yoga, tai chi, and other classes that focuses on body awareness. It is also a good idea to do exercises that strengthen your [[Core Stability|core]]. | |||
* Maintain a healthy weight. [[Obesity|Extra weight]] can weaken [[Abdominal Muscles|abdominal muscles]], cause problems for pelvis and spine, and contribute to low back pain. | |||
* Wear comfortable, low-heeled shoes. High heels, for example, can throw off balance and force person to walk differently. This puts more stress on muscles and harms posture. | |||
* Make sure work surfaces are at a comfortable height for you, whether sitting in front of a computer, making dinner, or eating a meal.<ref name=":0">Medlineplus [https://medlineplus.gov/guidetogoodposture.html Good Posture] Available from:https://medlineplus.gov/guidetogoodposture.html (last accessed 21.4.2020)</ref> | |||
* Ensure to engage your core (example deep abdominal and pelvic floor muscles ) during strenuous activities and breath out as you lift. This helps to stabilise your spine.<ref>Frizziero A, Pellizzon G, Vittadini F, Bigliardi D, Costantino C. Efficacy of Core Stability in Non-Specific Chronic Low Back Pain. J Funct Morphol Kinesiol. 2021 Apr 22;6(2):37. </ref> | |||
* Remember to maintain a neutral posture as this helps body to function optimally. | |||
And to avoid: | |||
The balanced posture of the body reduces the work done by the muscles in maintaining it in an erect posture. It has been determined (using electromyography) that, in general<ref>Chiba R, Takakusaki K, Ota J, Yozu A, Haga N. Human upright posture control models based on multisensory inputs; in fast and slow dynamics. Neuroscience research. 2016 Mar 1;104:96-104.</ref> | * Static postures such as prolonged sitting and standing. | ||
** Prolonged cross-legged sitting can lead to a bent and asymmetrical posture, especially for people with low back pain.<ref>Jung KS, Jung JH, In TS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7370107/ The effects of cross-legged sitting on the trunk and pelvic angles and gluteal pressure in people with and without low back pain]. International Journal of Environmental Research and Public Health. 2020 Jul;17(13):4621.</ref> Erect sitting for long hours can also cause postural problems. It is recommended to get up from your chair and move around at least every 30 minutes.<ref>Wongpipit W, Zhang X, Miyashita M, Wong SH. Interrupting Prolonged Sitting Reduces Postprandial Glucose Concentration in Young Men With Central Obesity. J Clin Endocrinol Metab. 2021 Jan 23;106(2):e791-e802. doi: 10.1210/clinem/dgaa834. PMID: 33186451.</ref> | |||
** Prolonged standing, usually at work, can lead to musculoskeletal pain and vascular disorders. Seated breaks are necessary to prevent the risk of causing associated pain or discomfort.<ref>Jo H, Lim OB, Ahn YS, Chang SJ, Koh SB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8149936/ Negative impacts of prolonged standing at work on musculoskeletal symptoms and physical fatigue: The fifth korean working conditions survey.] Yonsei medical journal. 2021 Jun 6;62(6):510.</ref> | |||
* Smoking. Smoking habits were suggested to have a long-term-effect on the posture control system as it increases risk for lumbar disc degeneration.<ref>Kiraz M, Demir E. [https://www.sciencedirect.com/science/article/abs/pii/S0028377020303933 Relationship of lumbar disc degeneration with hemoglobin value and smoking.] Neurochirurgie. 2020 Nov 1;66(5):373-7.</ref> | |||
=== Muscle Action in Posture === | |||
The balanced posture of the body reduces the work done by the muscles in maintaining it in an erect posture. It has been determined (using electromyography) that, in general:<ref>Chiba R, Takakusaki K, Ota J, Yozu A, Haga N. [https://www.sciencedirect.com/science/article/pii/S0168010215002928 Human upright posture control models based on multisensory inputs; in fast and slow dynamics.] Neuroscience research. 2016 Mar 1;104:96-104.</ref> | |||
*The intrinsic muscles of the feet are quiescent, because of the support provided by the ligaments. | *The intrinsic muscles of the feet are quiescent, because of the support provided by the ligaments. | ||
*[[Soleus]] is constantly active because gravity tends to pull the body forward over the feet. [[Gastrocnemius]] and the deep posterior tibial muscles are less frequently active. | *[[Soleus]] is constantly active because gravity tends to pull the body forward over the feet. [[Gastrocnemius]] and the deep posterior tibial muscles are less frequently active. | ||
*[[Tibialis Anterior|Tibialis anterior]] is less active (unless high heels are being worn). | *[[Tibialis Anterior|Tibialis anterior]] is less active (unless high heels are being worn). | ||
*[[Rectus Femoris|Quadriceps]] and the [[Hamstrings]] are generally not as active<ref>Tikkanen O, Haakana P, Pesola AJ, Häkkinen K, Rantalainen T, Havu M, Pullinen T, Finni T. Muscle activity and inactivity periods during normal daily life. PloS one. 2013;8(1).</ref> | *[[Rectus Femoris|Quadriceps]] and the [[Hamstrings]] are generally not as active.<ref>Tikkanen O, Haakana P, Pesola AJ, Häkkinen K, Rantalainen T, Havu M, Pullinen T, Finni T. [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0052228 Muscle activity and inactivity periods during normal daily life.] PloS one. 2013 Jan 18;8(1):e52228.</ref> | ||
*[[Hip Anatomy|Iliopsoas]] is constantly active. | *[[Hip Anatomy|Iliopsoas]] is constantly active. | ||
*[[Gluteus Maximus|Gluteus maximus]] is inactive. | *[[Gluteus Maximus|Gluteus maximus]] is inactive. | ||
*[[Gluteus Medius|Gluteus medius]] and tensor fascia latae are active to counteract lateral postural sway. | *[[Gluteus Medius|Gluteus medius]] and tensor fascia latae are active to counteract lateral postural sway. | ||
*[[Erector | *[[Erector Spinae]] is active, counteracting gravity's pull forwards. | ||
*The abdominal muscles remain quiescent, although the lower fibres of the [[Abdominal | *The abdominal muscles remain quiescent, although the lower fibres of the [[Internal Abdominal Oblique |Internal obliques]] are active in order to protect the inguinal canal | ||
=== Examples of Abnormal Posture === | |||
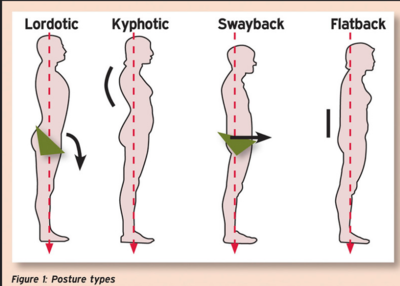
Examples of abnormal posture are as follows: | |||
[[File:Posture Types.png|right|frameless|400x400px]] | |||
*[[Low Back Pain Related to Hyperlordosis|Lordotic Posture]]- Lordosis refers to the normal inward curvature of the spine. When this curve is exaggerated it is usually referred to as hyperlordosis. The head, neck, and thoracic spine are in neutral. The lumbar spine is hyperextended, producing an anterior tilt of the pelvis. The hip is flexed, the knees are hyperextended, and the ankles are plantar flexed. <ref name=":3">Kendall FP. Muscles: Testing and function with posture and pain. Baltimore, MD etc.: Lippincott Williams & Wilkins; 2010. </ref> | |||
*[[Sway Back Posture]]- In this type of posture, there is forward head, hyper-extension of the cervical spine, flexion of the thoracic spine, lumbar spine extension, posterior tilt of the pelvis, hip and knee hyper-extension and ankle slightly plantar flexed. <ref name=":3" /> | |||
*Flat-Back Posture- In this type of posture, the head is forward with cervical spine extension. There is slight flexion of the upper thoracic spine and a straight or flattened appearance of the lower thoracic and lumbar spine. The pelvis is in a posterior tilt, the knees are in extension, and the ankles are plantar flexed.<ref name=":3" /> | |||
*[[Forward Head Posture|Forward Head]] posture - Describes the shift of the head forward with the chin poking out. It is caused by increased flexion of the lower cervical spine and upper thoracic spine with increased extension of the upper cervical spine and extension of the occiput on C1. | |||
|- | *[[Scoliosis]] - A deviation of the normal vertical line of the spine, consisting of a lateral curvature and rotation of the vertebrae. Scoliosis is considered when there is at least 10° of spinal angulation on the posterior-anterior radiograph associated with vertebral rotation.<ref>Janicki JA, Alman B. [https://academic.oup.com/pch/article-abstract/12/9/771/2648067 Scoliosis: Review of diagnosis and treatment.] Paediatrics & child health. 2007 Nov 1;12(9):771-6. | ||
</ref> This is a 3 dimensional C or S shaped sideways curve of the spine. | |||
*[[Kyphosis]] - An increased convex curve observed in the thoracic or sacral regions of the spine. The head is forward, and there is hyperextension of the cervical spine. The scapula is abducted, and there is increased flexion in the thoracic spine. The lumbar spine is hyperextended. The pelvis is anteriorly tilted; the hips are flexed. The knees are in hyperextension, and the ankles are plantar flexed .<ref name=":3" /> | |||
== | == Muscle Imbalances in Abnormal Postures == | ||
* Kypholordotic Posture- The neck flexors, thoracic paraspinals, external obliques, and middle/lower trapezius are long and weak. The neck extensors, hip flexors, and lower back muscles are short and strong.<ref name=":3" /> | |||
* Lordotic Posture- The abdominal muscles are long and weak. The lower back muscles and hip flexors are short and strong.<ref name=":3" /> | |||
* Flat-Back Posture- The hip flexors are long and weak. The hip extensors are short and tight.<ref name=":3" /> | |||
* Sway-Back Posture- The neck flexors, middle/lower trapezius, thoracic paraspinals, external obliques, and Iliopsoas are long and weak. The hip extensors are short and strong. <ref name=":3" /> | |||
* | |||
* | |||
* | |||
== | == Summary == | ||
In conclusion, posture is not about adhering to an ideal standard but about how our bodies adapt and interact with different situations. The focus should be not to 'correct' posture but to enhance postural awareness, promote postural variability, and foster overall health and well-being. | |||
== References | == References == | ||
<references /> | <references /> | ||
| Line 105: | Line 202: | ||
[[Category:Movement Analysis]] | [[Category:Movement Analysis]] | ||
[[Category:Occupational Health]] | [[Category:Occupational Health]] | ||
[[Category:Assessment]] | |||
[[Category:Thoracic Spine]] | |||
[[Category:Lumbar Spine]] | |||
[[Category:Cervical Spine]] | |||
[[Category:Thoracic Spine - Assessment and Examination]] | |||
[[Category:Lumbar Spine - Assessment and Examination]] | |||
[[Category:Cervical Spine - Assessment and Examination]] | |||
Revision as of 22:58, 10 April 2024
Welcome to Arkansas Colleges of Health Education School of Physical Therapy Musculoskeletal 1 Project. This space was created by and for the students at Arkansas Colleges of Health Education School in the United States. Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!
Introduction [edit | edit source]
Posture is a highly individual and dynamic aspect of human physiology. It is more about how your body adapts and interacts with different situations than a fixed 'correct' or 'incorrect' state. Posture can be simply defined as the way in which we hold our bodies while standing, sitting, or lying down.[1]
A growing body of research suggests that the concept of a 'bad posture' is subjective, and there is no definitive link between specific postural habits and pain.[2] In fact, posture varies greatly among individuals, and what may be considered a 'good posture' for one person may not work or feel comfortable for another.[3]
What is Posture?[edit | edit source]
Posture is the attitude assumed by the body either with support during muscular inactivity, or the coordinated action of many muscles working to maintain stability. It forms an essential basis that is being adapted constantly.[4]
Our posture is an active process involving not only our muscles and joints but also our perception, emotions, and the environment we are in. Even seemingly static positions, like sitting or standing, are full of tiny adjustments and movements.[5]
Inactive Posture: Describe postures adopted during resting or sleeping, and they are more suitable for this purpose when all the essential muscular activity required to maintain life is reduced to a minimum.
Active Posture: The integrated action of many muscles is required to maintain active postures, which may be either static or dynamic.[4]
- Static posture- the body and its segments are aligned and maintained in certain positions. Examples include standing, sitting, lying, and kneeling.
- Dynamic posture- the body or its segments are moving—walking, running, jumping, throwing, and lifting.
Understanding 'Good' and 'Bad' Posture[edit | edit source]
The traditional view of posture insists on a 'correct' or 'incorrect' way to hold one's body, often associated with ideas about aesthetics, fitness, or health. However, current research indicates that this may be an oversimplified view.
Several studies have found no consistent link between posture and musculoskeletal pain[6], questioning the widely held belief that 'bad posture' leads to back or neck pain. This includes research showing no clear correlation between postural deviations and pain among adolescents[7], and studies showing that correcting posture does not necessarily alleviate chronic pain.[8]
The emerging view in physiotherapy and related fields is that rather than striving for an arbitrarily 'ideal' posture, it may be more beneficial to cultivate postural variability - the ability to comfortably change and adapt one's posture to different situations.[9] Indeed, according to some ergonomists, "your next posture is your best posture." Alternating between sitting and standing may practically eliminate lower back pain while easing pressure on the vertebrae and improving blood flow to the legs.
Optimizing Posture (The Importance of the Pelvic Girdle)[edit | edit source]
According to Vleeming et al., the sacral base is the geometric center of the postural system. Unlevelness of the base of the sacrum contributes to decreased postural balance and can be a chronic postural stressor. If posture is misaligned, to maintain postural balance, the lumbar spine tends to angle laterally and concave towards the high side of the sacral base. [10]
Impairments that can cause unlevelness of the base of the sacrum include, but are not limited to:
- Leg length discrepancies
- If there is a leg length discrepancy, the pelvis will present as asymmetrical.[11]
- Piriformis syndrome
- Piriformis syndrome has the ability to increase the tension on muscles of the pelvis as they try to stabilize the pelvis and the spine. This can throw the sacral base off of its geometric center.[12]
- Tight adductor muscles
- Tight or weak hip adductors can cause a lateral pelvic tilt, which leads to issues with long-standing and standing posture.[11]
- Asymmetrical dynamic postures
- A common asymmetrical dynamic posture is generally identified as the "Statue of David" posture. During this, one lower extremity is externally rotated, which potentially causes weakness in the internal rotators of the hip, and the opposing lower extremity is internally rotated, potentially causing weakness in the external rotators of the hip. To combat these weaknesses, strengthening of the weaker muscles is recommended.
Posture and Health[edit | edit source]
Poor posture can be bad for your health. Maintaining a posture that puts stress on a joint such as prolonged slouching (see image at R) or slumping over can:
- Increase pressure on the spine, making it more prone to injury and degeneration
- Cause neck, shoulder, and back pain[13][14][15]
- Decrease flexibility
- Affect how well joints move
- Affect balance and increase risk of falling
- Make it harder to digest food
- Induce breathing disorder and affect surrounding structures including the heart and phrenic nerve[16]
- In women it can lead to imbalance in the core muscle leading to incontinence and/or pelvic organ prolapse
Age-Related Postural Changes
Ageing inevitably affects posture. The main contributing factors for postural instability are:[17]
- Thoracic hyperkyphosis
- Loss of lumbar lordosis
- Decreased plantar arch
The Importance of Posture in Different Populations[edit | edit source]
Geriatric Patients:
For geriatric patients, it is important for physical therapists to focus on muscle imbalance and alignments which will better improve their overall posture and balance. [18] As we age, we begin to lose our height. This is due to our vertebrae and disc breaking down and our connective tissue beginning to lose their stretch. [19]
Overall improvement of their posture can lead to:
- Improved balance, decreased fall risk [18]
- Prevents osteoporosis [18]
- Decreased feelings of depression [20]
- Increased cognitive function [20]
Pediatric Patients:
It is important for children to have good posture to help prevent any dysfunctions to their developing bodies. In order to improve their posture, children should regularly participate in exercise.[21] A child’s posture can be influenced by:[21]
- Activity level
- Age and gender
- Self-confidence
- Height
- Weight
- Seating equipment at school and home
- The weight and size of their backpack
Athletic Posture:
Athletes are expected to maintain high energy over an extended amount of time. During this time, they should be able to demonstrate agility, while also effectively playing their role or position. Due to this, an athletic stance is an example of the dynamic aspect of posture. Poor posture in athletics can limit their range of motion, causing them to generate less power and perform poorly. Having poor posture while performing these dynamic movements increases the chances for an athlete to be injured[22]. An athlete’s posture differs from a regular posture. An athletic stance allows players to be ready for any movement they need to perform. A proper athletic stance is as follows: [23]
- Feet hip-width apart to shoulder-width apart
- Quarter-squat position
- Body weight evenly distributed through both feet
- Center of gravity directly above base of support
- Shoulders level
- Torso flat and at a slightly bent vertical 75° incline
Teaching proper athletic posture is fundamentally important to an athlete’s ability to practice and effectively perform the skills necessary to fulfill the requirement of any sport activity.[23]
Neurologic Patients:
The importance of posture in patients with spinal cord injury (SCI) is to allow them to participate in their daily activities without the possibility of them injuring themself or creating chronic issues.[24] Physical therapists should observe patients' functional capability, postural support, and comfort.[24] Any patient presenting these signs should be assessed:[24]
- Current or recurring pressure injuries
- Pain and discomfort with sitting
- Risk of falls and safety concerns of client or their caregivers
- Postural asymmetry and risk of fixed deformity
- Difficulty with balance during static sitting, dynamic tasks, or when attempting weight shift for pressure management
- Changes in body size
- Reduced function
- Replacement of seating and wheeled mobility system
- Posture-related aspirations
- Respiratory restrictions
Through assessing a patient with SCI, the physical therapist is able to make the appropriate choice of wheelchair and seat for the patient, if required. [25]
Physiotherapy[edit | edit source]
Rather than 'correcting' posture, physiotherapy can play a crucial role in improving postural awareness and promoting postural variability. Physiotherapists can help individuals explore a range of postures and movements, enhancing their ability to adapt to different activities and environments comfortably.
Important advice could include:
- Be mindful of posture during everyday activities, like watching television, washing dishes, or walking
- Stay active. Any kind of exercise may help improve your posture, but certain types of exercises can be especially helpful. eg. yoga, tai chi, and other classes that focuses on body awareness. It is also a good idea to do exercises that strengthen your core.
- Maintain a healthy weight. Extra weight can weaken abdominal muscles, cause problems for pelvis and spine, and contribute to low back pain.
- Wear comfortable, low-heeled shoes. High heels, for example, can throw off balance and force person to walk differently. This puts more stress on muscles and harms posture.
- Make sure work surfaces are at a comfortable height for you, whether sitting in front of a computer, making dinner, or eating a meal.[26]
- Ensure to engage your core (example deep abdominal and pelvic floor muscles ) during strenuous activities and breath out as you lift. This helps to stabilise your spine.[27]
- Remember to maintain a neutral posture as this helps body to function optimally.
And to avoid:
- Static postures such as prolonged sitting and standing.
- Prolonged cross-legged sitting can lead to a bent and asymmetrical posture, especially for people with low back pain.[28] Erect sitting for long hours can also cause postural problems. It is recommended to get up from your chair and move around at least every 30 minutes.[29]
- Prolonged standing, usually at work, can lead to musculoskeletal pain and vascular disorders. Seated breaks are necessary to prevent the risk of causing associated pain or discomfort.[30]
- Smoking. Smoking habits were suggested to have a long-term-effect on the posture control system as it increases risk for lumbar disc degeneration.[31]
Muscle Action in Posture[edit | edit source]
The balanced posture of the body reduces the work done by the muscles in maintaining it in an erect posture. It has been determined (using electromyography) that, in general:[32]
- The intrinsic muscles of the feet are quiescent, because of the support provided by the ligaments.
- Soleus is constantly active because gravity tends to pull the body forward over the feet. Gastrocnemius and the deep posterior tibial muscles are less frequently active.
- Tibialis anterior is less active (unless high heels are being worn).
- Quadriceps and the Hamstrings are generally not as active.[33]
- Iliopsoas is constantly active.
- Gluteus maximus is inactive.
- Gluteus medius and tensor fascia latae are active to counteract lateral postural sway.
- Erector Spinae is active, counteracting gravity's pull forwards.
- The abdominal muscles remain quiescent, although the lower fibres of the Internal obliques are active in order to protect the inguinal canal
Examples of Abnormal Posture[edit | edit source]
Examples of abnormal posture are as follows:
- Lordotic Posture- Lordosis refers to the normal inward curvature of the spine. When this curve is exaggerated it is usually referred to as hyperlordosis. The head, neck, and thoracic spine are in neutral. The lumbar spine is hyperextended, producing an anterior tilt of the pelvis. The hip is flexed, the knees are hyperextended, and the ankles are plantar flexed. [34]
- Sway Back Posture- In this type of posture, there is forward head, hyper-extension of the cervical spine, flexion of the thoracic spine, lumbar spine extension, posterior tilt of the pelvis, hip and knee hyper-extension and ankle slightly plantar flexed. [34]
- Flat-Back Posture- In this type of posture, the head is forward with cervical spine extension. There is slight flexion of the upper thoracic spine and a straight or flattened appearance of the lower thoracic and lumbar spine. The pelvis is in a posterior tilt, the knees are in extension, and the ankles are plantar flexed.[34]
- Forward Head posture - Describes the shift of the head forward with the chin poking out. It is caused by increased flexion of the lower cervical spine and upper thoracic spine with increased extension of the upper cervical spine and extension of the occiput on C1.
- Scoliosis - A deviation of the normal vertical line of the spine, consisting of a lateral curvature and rotation of the vertebrae. Scoliosis is considered when there is at least 10° of spinal angulation on the posterior-anterior radiograph associated with vertebral rotation.[35] This is a 3 dimensional C or S shaped sideways curve of the spine.
- Kyphosis - An increased convex curve observed in the thoracic or sacral regions of the spine. The head is forward, and there is hyperextension of the cervical spine. The scapula is abducted, and there is increased flexion in the thoracic spine. The lumbar spine is hyperextended. The pelvis is anteriorly tilted; the hips are flexed. The knees are in hyperextension, and the ankles are plantar flexed .[34]
Muscle Imbalances in Abnormal Postures[edit | edit source]
- Kypholordotic Posture- The neck flexors, thoracic paraspinals, external obliques, and middle/lower trapezius are long and weak. The neck extensors, hip flexors, and lower back muscles are short and strong.[34]
- Lordotic Posture- The abdominal muscles are long and weak. The lower back muscles and hip flexors are short and strong.[34]
- Flat-Back Posture- The hip flexors are long and weak. The hip extensors are short and tight.[34]
- Sway-Back Posture- The neck flexors, middle/lower trapezius, thoracic paraspinals, external obliques, and Iliopsoas are long and weak. The hip extensors are short and strong. [34]
Summary[edit | edit source]
In conclusion, posture is not about adhering to an ideal standard but about how our bodies adapt and interact with different situations. The focus should be not to 'correct' posture but to enhance postural awareness, promote postural variability, and foster overall health and well-being.
References[edit | edit source]
- ↑ Caneiro, J. P., O'Sullivan, P., Burnett, A., Barach, A., O'Neil, D., Tveit, O., & Olafsdottir, K. (2010). The influence of different sitting postures on head/neck posture and muscle activity. Manual Therapy, 15(1), 54-60
- ↑ Slater D, Korakakis V, O'Sullivan P, Nolan D, O'Sullivan K. “Sit up straight”: time to re-evaluate. journal of orthopaedic & sports physical therapy. 2019 Aug;49(8):562-4.
- ↑ Barrett, E., O'Keeffe, M., O'Sullivan, K., Lewis, J., & McCreesh, K. (2016). Is thoracic spine posture associated with shoulder pain, range of motion and function? A systematic review. Manual Therapy, 26, 38-46
- ↑ 4.0 4.1 Gardiner, Mary Dena. (1973). The principles of exercise therapy. London : Bell
- ↑ Dunk, N. M., Callaghan, J. P., & McGill, S. M. (2005). Lumbar spine movement patterns during prolonged sitting differentiate low back pain developers from matched asymptomatic controls. Work, 24(2), 181-188.
- ↑ Dankaerts, W., O'Sullivan, P., Burnett, A., Straker, L., & Davey, P. (2007). Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine, 32(6), 698-704.
- ↑ Dolphens, M., Cagnie, B., Coorevits, P., Vanderstraeten, G., Cardon, G., D'hooge, R., & Danneels, L. (2012). Sagittal standing posture and its association with spinal pain: a school-based epidemiological study of 1196 Flemish adolescents before age at peak height velocity. Spine, 37(19), 1657-1666.
- ↑ Christensen, S. T., & Hartvigsen, J. (2008). Spinal curves and health: a systematic critical review of the epidemiological literature dealing with associations between sagittal spinal curves and health. Journal of Manipulative and Physiological Therapeutics, 31(9), 690-714
- ↑ Burgess-Limerick, R., Plooy, A., Fraser, K., & Hargreaves, M. (2000). The influence of computer monitor height on head and neck posture. International Journal of Industrial Ergonomics, 25(3), 339-345
- ↑ Mooney V, Stoeckart R, Vleeming A. Movement, stability & lumbopelvic pain: integration of research and therapy. Edinburgh; New York: Churchill Livingstone Elsevier, 2007.
- ↑ 11.0 11.1 Magee D, Manske R. Orthopedic physical assessment. St. Louis: Elsevier. 2021.
- ↑ Boyle P, Weitz M. editors. Dutton’s orthopaedic examination evaluation and intervention. McGraw-Hill. 2019.
- ↑ Kang BR, Her JG, Lee JS, Ko TS, You YY. Effects of the computer desk level on the musculoskeletal discomfort of neck and upper extremities and EMG activities in patients with spinal cord injuries. Occupational therapy international. 2019 Feb 3;2019.
- ↑ Borhany T, Shahid E, Siddique WA, Ali H. Musculoskeletal problems in frequent computer and internet users. Journal of family medicine and primary care. 2018 Mar;7(2):337.
- ↑ Daneshmandi H, Choobineh A, Ghaem H, Karimi M. Adverse effects of prolonged sitting behavior on the general health of office workers. Journal of lifestyle medicine. 2017 Jul;7(2):69.
- ↑ Albarrati A, Zafar H, Alghadir AH, Anwer S. Effect of upright and slouched sitting postures on the respiratory muscle strength in healthy young males. BioMed research international. 2018 Feb 25;2018.
- ↑ Fernandes VL, Ribeiro DM, Fernandes LC, Menezes RL. Postural changes versus balance control and falls in community-living older adults: a systematic review. Fisioterapia em Movimento. 2018 Jun 7;31.
- ↑ 18.0 18.1 18.2 Hsu WL, Chen CY, Tsauo JY, Yang RS. Balance control in elderly people with osteoporosis. Journal of the Formosan Medical Association. 2014 Jun;113(6):334–9.
- ↑ Ahmed T, Haboubi N. Assessment and management of nutrition in older people and its importance to health. Clinical Interventions in Aging. 2010 Jul;5:207.
- ↑ 20.0 20.1 Matthieu Casteran, Alain Putot, François Pfitzenmeyer, Thomas E, Manckoundia P. Analysis of the impact of a cognitive task on the posture of elderly subjects with depression compared with healthy elderly subjects. Clinical neurophysiology. 2016 Nov 1;127(11):3406–11.
- ↑ 21.0 21.1 Good posture and Spine Care in children. Royal Children’s Hospital. Victorian Paediatric Orthopaedic; 2011.
- ↑ Dawid Koźlenia, Katarzyna Kochan-Jacheć. The Impact of Interaction between Body Posture and Movement Pattern Quality on Injuries in Amateur Athletes. Journal of clinical medicine. 2024 Mar 2;13(5):1456–6.
- ↑ 23.0 23.1 Athletic stance [Internet]. 205 Sports. Available from: https://205sports.org/player-development/205-training/ltad/athletic-stance/
- ↑ 24.0 24.1 24.2 Innovation A for C. The importance of posture for SCI clients [Internet]. aci.health.nsw.gov.au. 2017. Available from: https://aci.health.nsw.gov.au/networks/spinal-cord-injury/spinal-seating/module-7/the-importance-of-posture-for-sci-clients
- ↑ Wadhwa G, Aikat R. Development, validity and reliability of the “Sitting Balance Measure” (SBM) in spinal cord injury. Spinal Cord. 2015 Oct 13;54(4):319–23.
- ↑ Medlineplus Good Posture Available from:https://medlineplus.gov/guidetogoodposture.html (last accessed 21.4.2020)
- ↑ Frizziero A, Pellizzon G, Vittadini F, Bigliardi D, Costantino C. Efficacy of Core Stability in Non-Specific Chronic Low Back Pain. J Funct Morphol Kinesiol. 2021 Apr 22;6(2):37.
- ↑ Jung KS, Jung JH, In TS. The effects of cross-legged sitting on the trunk and pelvic angles and gluteal pressure in people with and without low back pain. International Journal of Environmental Research and Public Health. 2020 Jul;17(13):4621.
- ↑ Wongpipit W, Zhang X, Miyashita M, Wong SH. Interrupting Prolonged Sitting Reduces Postprandial Glucose Concentration in Young Men With Central Obesity. J Clin Endocrinol Metab. 2021 Jan 23;106(2):e791-e802. doi: 10.1210/clinem/dgaa834. PMID: 33186451.
- ↑ Jo H, Lim OB, Ahn YS, Chang SJ, Koh SB. Negative impacts of prolonged standing at work on musculoskeletal symptoms and physical fatigue: The fifth korean working conditions survey. Yonsei medical journal. 2021 Jun 6;62(6):510.
- ↑ Kiraz M, Demir E. Relationship of lumbar disc degeneration with hemoglobin value and smoking. Neurochirurgie. 2020 Nov 1;66(5):373-7.
- ↑ Chiba R, Takakusaki K, Ota J, Yozu A, Haga N. Human upright posture control models based on multisensory inputs; in fast and slow dynamics. Neuroscience research. 2016 Mar 1;104:96-104.
- ↑ Tikkanen O, Haakana P, Pesola AJ, Häkkinen K, Rantalainen T, Havu M, Pullinen T, Finni T. Muscle activity and inactivity periods during normal daily life. PloS one. 2013 Jan 18;8(1):e52228.
- ↑ 34.0 34.1 34.2 34.3 34.4 34.5 34.6 34.7 Kendall FP. Muscles: Testing and function with posture and pain. Baltimore, MD etc.: Lippincott Williams & Wilkins; 2010.
- ↑ Janicki JA, Alman B. Scoliosis: Review of diagnosis and treatment. Paediatrics & child health. 2007 Nov 1;12(9):771-6.