Urinary Incontinence
Original Editor - Kirsten Ryan
Top Contributors - Kirsten Ryan, Nicole Sandhu, Admin, Nicole Hills, Vidya Acharya, Wendy Walker, Kim Jackson, Agoro Bukola Zainab, Merve Demirayak, Temitope Olowoyeye, Laura Ritchie, Evan Thomas, WikiSysop, Lauren Lopez and Lucinda hampton
Introduction[edit | edit source]
Urinary Incontinence (UI) is a common condition that often goes untreated. Estimates of prevalence vary depending on the population studied, the measurement period (e.g., daily or weekly), and the instruments used to assess severity. It is estimated to affect about 50% of adult women and 3% to 11% of adult men; however, only 25% to 61% of those women seek care.[1][2] This may be due to embarrassment, a lack of knowledge about treatment options, or a belief that urinary incontinence is a normal and inevitable part of aging.[3]
Definitions[edit | edit source]
Urinary incontinence defined by International Continence Society as an involuntary urinary leakage. There are different types of urinary incontinence[5] and identifying the classification of urinary incontinence can help to guide treatment, however, an individual could exhibit symptoms from more than one of the classifications.[6]
- Stress urinary incontinence is the most common type, affecting an estimated 50% of all incontinent women.[7] It is defined as a complaint of involuntary loss of urine on effort or physical exertion (e.g., sporting activities), or on sneezing or coughing.
- Urgency urinary incontinence is more prevalent in older women and accounts for a small proportion of women with urinary incontinence. It is a complaint of involuntary loss of urine associated with urgency. A compelling desire to pass urine which is difficult to defer.
- Mixed urinary incontinence is a complaint of involuntary loss of urine associated with urgency and also effort or physical exertion or on sneezing or coughing.
- Overactive bladder (OAB, urgency) syndrome is a urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection or other obvious pathology.[8]
- Nocturnal enuresis is an involuntary loss of urine occur during sleep.
- Other types of urinary incontinence may define as urinary leakage during the sexual intercourse or giggle incontinence.[5]
Epidemiology[edit | edit source]
Urinary incontinence remains a worldwide problem, affecting both males and females, across different cultures and races. As mentioned above, the worldwide prevalence is difficult to determine due to differences in definitions used, the population surveyed, survey type, response rate, age, gender, availability and efficacy of health care, and other factors.[9]
Pathophysiology[edit | edit source]
Urinary incontinence is more frequent in women than men because of the differences in the anatomy of the pelvic floor muscles, the ligament structures and the effect of childbirth and maternal injury.[10]
Although female urinary incontinence pathophysiology is not yet elucidated[11], some possible mechanisms of UI can be found in the literature. First, a deficient urethral closure mechanism result in weak pelvic floor muscles and urethral hypermobility following childbirth cause UI.[12] Additionally, the baby's head distends and stretches the PFM and deteriorates the normal function of connective tissues and nerves during the vaginal delivery.[13] Another possible mechanism is the change of the hormone levels such as progesterone and relaxin during pregnancy, breastfeeding and postpartum.[14]
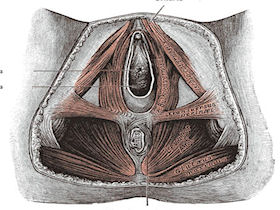
Clinically Relevant Anatomy: Pelvic Floor[edit | edit source]
The pelvic floor is made up of the muscles, ligaments, and fascial structures that act together to support the pelvic organs and to provide compressive forces to the urethra during increased intra-abdominal pressure.
The pelvic floor muscles refer to the muscular layer of the pelvic floor. It includes the levator ani, striated urogenital sphincter, external anal sphincter, ischiocavernosus, and bulbospongiosus.[7]
The urethra, vagina, and rectum pass through the pelvic floor and are surrounded by the pelvic floor muscles. During increased intra-abdominal pressure, the pelvic floor muscles must contract to provide support. When the pelvic floor muscles contract the urethra, anus, and vagina close. The contraction is important in preventing the involuntary loss of urine or rectal contents. The pelvic floor muscles must also relax in order to void.[7]
Etiology[edit | edit source]
Stress urinary incontinence:
- Urethral hypermobility: Increases in intra-abdominal pressure (eg, from coughing or sneezing) with insufficient support of the pelvic floor musculature and vaginal connective tissue to the urethra and bladder neck can lead to incontinence.[16]
- Pregnancy and vaginal birth, post-partum, obesity, chronic cough, chronic heavy lifting, and constipation: If there is an increase in abdominal pressure that is greater than the opposing force of the pelvic floor muscles, it can result in stress incontinence[17][18] A systematic review[19] identifying the pregnancy and obstetric-related risk factors that predict pelvic floor disorders for women later in life suggests that: urinary incontinence during pregnancy, an instrumental vaginal delivery, an episiotomy, tears, and constipation are the considerable risk factors leading to urinary incontinence postpartum.
- Intrinsic sphincteric deficiency (ISD): This results from a loss of intrinsic urethral mucosal and muscular tone that normally keeps the urethra closed, it can occur in the presence or absence of urethral hypermobility and with minimal abdominal pressure.[20][21]
Urgency urinary incontinence:
- This may be secondary to neurologic disorders (eg, spinal cord injury), bladder abnormalities, increased or altered bladder microbiome, or may be idiopathic.[22][23]
Overactive bladder:
- This could be due to neuropathic, an infection (i.e. urinary tract infection), weak pelvic floor muscles, diet (i.e. consumption of diuretics), medications, excess weight[24]
Mixed Incontinence:
- Individuals can present with more than one type of incontinence
- For example, stress incontinence and/or urge incontinence might be "masked" by an overactive bladder (frequenting the washroom often to avoid leakage).
Risk Factors[edit | edit source]
| Risk factors for urinary incontinence (UI) | |
|---|---|
| Age | The prevalence and severity of UI increases with age.[25][26]
Age may not be an independent risk factor, when studies have controlled for co-morbidities.[27] |
| Obesity | This is a strong risk factor for UI. Additionally, weight reduction is associated with improvement or resolution of symptoms, particularly with stress urinary incontinence.[26][28][29] |
| Parity | Increasing parity is a risk factor for UI, however, nulliparous women also report bothersome UI.[30][29] |
| Mode of delivery | Women who have had a vaginal delivery have an increased risk of UI, however, cesarean delivery does not protect women from UI.[31] |
| Family history | This may be a risk factor for UI, particularily with urge incontinence and overactive bladder.[32][33] |
| Other | Conditions such as diabetes, stroke, and depression are associated with an increased risk of UI. [28][34][35] |
Clinical Presentation[edit | edit source]
- Urine Leaking
- Urinary Frequency
- Urinary Urgency
- Nocturia
- Prolapse
Diagnostic Procedures[edit | edit source]
A large portion of women with urinary stress incontinence can be diagnosed from clinical history alone. In a systematic review performed in 2006[36], little evidence was found to support the use of urinary diaries, and pad tests although these measures are common diagnostic assessments used in physical therapy.[36]
Clinical history[edit | edit source]
Clinical history taking compared with multi-channel urodynamics was found to have 0.92 sensitivity and 0.56 specificity for the diagnosis of urinary stress incontinence based on the presence of stress incontinence symptoms.[36]
Pelvic Floor Muscle Function and Strength[edit | edit source]
Modified Oxford grading system:
- 0 - no contraction
- 1 - flicker
- 2 - weak squeeze, no lift
- 3 - fair squeeze, definite lift
- 4 - good squeeze with lift
- 5 - strong squeeze with a lift
Palpation[edit | edit source]
Palpation of the pelvic floor muscles per the vagina in females and per the rectum in male patients.[37]
PERFECT mnemonic assessment[37]:
P - power, may use the Modified Oxford grading scale
E - endurance, the time (in seconds) that a maximum contraction can be sustained
R - repetition, the number of repetitions of a maximum voluntary contraction
F - fast contractions, the number of fast (one second) maximum contractions
ECT - every contraction timed, reminds the therapist to continually overload the muscle activity for strengthening[37]
Evaluation Of Urinary Incontinence[edit | edit source]
Pad Test[edit | edit source]
The 1 hour pad test was found to have 0.94 sensitivity and 0.44 specificity for diagnosing any leakage compared with multi-channel urodynamics. The 48 hour pad-test was found to have 0.92 sensitivity and 0.72 specificity for the diagnosis of urinary stress incontinence.[36]
While the 48-hour pad test is better used in clinical research due to its high reproducibility, the 1-hour pad test is the standardized method in a clinical setting.[38]
The test involves the patient wearing a pre-weighed pad, next the patient drinks 500 ml of sodium-free liquid in < 15 minutes, resting, after which he/she exercises for 30 minutes. The exercise would include activities such as walking, climbing up and down a flight of stairs, standing up from sitting, coughing vigorously, and running on the spot for 1 minute. The pad is then re-weighed and the resulting measurement given in grams of urine lost.[39]
Urinary (Voiding) Diary[edit | edit source]
One study found a scale derived from a 7-day diary was 0.88 sensitive and 0.83 specific for the diagnosis of detrusor overactivity in women.[36] The National Institute for Diabetes and Digestive and Kidney Diseases provides clinicians with an easy to use Bladder Diary pdf that may be used in clinical practice[40].
Outcome Measures[edit | edit source]
- Incontinence Quality of Life Instrument (I-QOL)
- International Consultation on Incontinence Modular Questionnaires (ICIQ)
- Male Urogenital Distress Inventory (MUDI)
- Male Urinary Symptom Impact Questionnaire (MUSIQ)
- Patient Global Impression of Improvement (PGI-I)
- Patient Global Impression of Severity (PGI-S)
- Pelvic Floor Distress Inventory - 20 (PFDI - 20)
- Pelvic Floor Impact Questionnaire - 7 (PFIQ - 7)
- The International Consultation on Incontinence Questionnaire of Female Lower Urinary Tract Symptoms Questionnaire (ICIQ-FLUTS)
- The Bristol Female Lower Urinary Tract Symptoms Questionnaire
- The International Consultation on Incontinence Questionnaire of Urinary Incontinence Short Form (ICIQ-UI SF)
Management of Urinary Incontinence[edit | edit source]
There are plenty of conservative treatment options consist of electric stimulation, pelvic floor muscle training, vaginal cones, biofeedback and behavioural therapy.[41]
Pelvic Floor Muscle Training (PFMT)[edit | edit source]
The American Urogynecologic Society[42] and NICE Guidelines [43] suggest PFMT as a first-line treatment option. This brief video gives a good run down on how to teach pelvic floor exercises.
The pelvic floor muscles are known as the levator ani, made up of the pubococcygeus - puborectalis complex. Those muscles form a sling around the anorectal junction. They are made up of both Type I (slow-twitch) and Type II (fast-twitch) fibers. The majority are Type I (about 70%) which provide sustained support and are fatigue resistant. The remaining Type II fibers provide the quick compressive forces necessary to oppose leakage during increased abdominal pressure. A contraction of the pelvic floor muscles also causes a reflex inhibition of the detrusor muscle.[45]
Patient specific training is necessary to ensure a proper contraction of the pelvic floor muscle group. It is also essential to train both the fast and slow-twitch muscle fibers. Also, training must include instruction in volitional contractions before and during an activity that may cause incontinence, such as coughing, sneezing, and lifting.[37] Patients are typically recommended to perform exercises four to five times daily.[46][37]
A non-controlled trial studying the effects of a home-based pelvic floor muscle training and bladder training in women with urinary incontinence showed that combined pelvic floor muscle training and bladder training decreased the symptoms and improved the quality of life[47].
PFMT for the prevention of postpartum incontinence[edit | edit source]
Pelvic floor muscle training (PFMT) performed during pregnancy helps to decrease the short-term risk of urinary incontinence in women without prior incontinence. A meta-analysis that included randomized or quasi-randomized trials on pregnant or postnatal women, found that women assigned to antenatal PFMT had a significant decrease in the rate of urinary incontinence at up to three months postpartum.[48]
A systematic review including randomized or quasi-randomized trials on primiparous or multiparous pregnant or postpartum women found that PFMT during pregnancy and after delivery can prevent and treat urinary incontinence. The authors recommended a supervised training protocol following strength-training principles, emphasizing close to maximum contractions and lasting at least 8 weeks.[49]
PFMT for stress urinary incontinence[edit | edit source]
Similarly to the findings stated above, PFMT has been found to be effective for treating stress urinary incontinence as well.[50][51] A systematic review looking at the effects of PFMT by comparing the effects of this training with no treatment, or with any inactive treatment (for example, advice on management with pads). The authors found women with stress urinary incontinence in the PFMT group were, on average, eight times more likely to report being cured. In addition, the participants reported an improved QoL. A recent review suggested that integrating PFMT with self-management strategies-lifestyle changes to maintain a healthy weight and quit smoking had a good outcome in mild-to-moderate stress urinary incontinence[52].
A Randomized Controlled Trial in women with stress urinary incontinence suggests that Pelvic floor Muscle Training and Extracorporeal Magnetic Innervation are effective in improving stress urinary incontinence and quality of life in women[53]. Another randomized control study suggested better outcomes with a combined training of PFMT and Transversus Abdominis muscle than with PFMT alone in patients with stress urinary incontinence. However, the training was more effective in the group of women who had lesser than three vaginal births[54]. A study examining the training parameter for strengthening the pelvic floor found the most effective protocol to consists of digital palpation combined with biofeedback monitoring and vaginal cones, including 12 week training parameters, and ten repetitions per series in different positions.[50]
Also, there has been a rise in the number of women experiencing incontinence among non-pregnant or pre-partum women in the last few decades. A new systematic review [55]analyzing the efficacy of pelvic floor muscle training (PFMT) in the treatment of UI and its effect on the improvement in muscle strength, endurance, and urinary leakage among non-pregnant women suggests pelvic floor muscle training with education as the most effective treatment and recommends it as the first line of treatment for improving urinary incontinence in non-pregnant women. The review demonstrated that PFMT effectively reduced urinary leakage and improved pelvic floor muscle contraction. Other interventions such as electrostimulation, vaginal cones, whole body vibration therapy, extra-corporeal magnetic innervation, etc., along with PFMT, were equally effective in treating UI and significantly decreased incontinence and improved quality of life.[55]
PFMT for urgency incontinence[edit | edit source]
PFMT has been shown to improve or cure symptoms of urge urinary incontinence.[51] In addition to PFMT, behavioural therapies and bladder training (described below) may be beneficial in this population.[56][57]
Behavioral Therapy[edit | edit source]
The focus of behavioral therapy is on lifestyle changes such as fluid or diet management, weight control, and bowel regulation. Education about bladder irritants, like caffeine, is an important consideration. Also, discussing bowel habits to determine if constipation is an issue as it is important to educate the patient about avoiding straining.[56] Education and explanation about normal lower urinary tract function is also included. Patients should understand the role of the bladder and the pelvic floor muscles.[58] A randomized clinical trial examined the effects of a group-administered behavioural therapy for urinary incontinence in older women and found it to be a modestly effective treatment for reducing symptoms of urinary incontinence. The group behavioural therapy included a one-time, two hour bladder health class, including written material and an audio CD.[59]
Bladder Training[edit | edit source]
The information gathered from the bladder diary is used to guide decision making for bladder re-training, including a voiding schedule if necessary to increase the capacity of the bladder for people with frequency issues. Bladder training attempts to break the cycle by teaching patients to void on a schedule, rather than in response to urgency. Urge suppression techniques are taught, such as distraction and relaxation. It is also important to teach the patient to contract the pelvic floor to cause detrusor inhibition. A voluntary contraction of the pelvic floor muscles helps increase pressure in the urethra, inhibit detrusor contractions, and control urinary leakage.[56] [58]
Differential Diagnosis[edit | edit source]
Multi-channel urodynamics testing is the gold standard for making a condition-specific diagnosis. This testing is typically done in secondary care, not in primary care or physical therapy.[36]
Key Evidence[edit | edit source]
A systematic review published in the Annals of Internal Medicine in 2008[60] found good evidence that pelvic floor muscle training and bladder training resolved urinary incontinence in women. However, the effects of electrostimulation, medical devices, injectable bulking agents, and local estrogen therapy were inconsistent.[60]
The study suggests surface electromyographic (sEMG) assisted biofeedback training and Pilates exercises have positive outcomes on the pelvic floor muscles in women with stress urinary incontinence[61].
Resources[edit | edit source]
Physiopedia's Clinical Guidelines: Pelvic Health Page
Websites[edit | edit source]
- American Urogynecologic Society (AUGS) at www.augs.org
- American Urological Association (AUA) at www.auanet.org
- International Continence Society (ICS) at www.icsoffice.org
- National Association for Continence (NAFC) at www.nafc.org
- National Institute on Aging at www.nia.nih.gov
- National Institute for Diabetes and Digestive and Kidney Diseases at https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems/diagnosis
- Section on Women's Health, APTA at www.women'shealthapta.org
- The Simon Foundation for Continence at www.simonfoundation.org
- Chartered Society of Physiotherapy: Physiotherapy Works! for urinary incontinence
Presentations[edit | edit source]
 |
Pelvic Physiotherapy - to Kegel or Not?
This presentation was created by Carolyn Vandyken, a physiotherapist who specializes in the treatment of male and female pelvic dysfunction. She also provides education and mentorship to physiotherapists who are similarly interested in treating these dysfunctions. In the presentation, Carolyn reviews pelvic anatomy, the history of Kegel exercises and what the evidence tells us about when Kegels are and aren't appropriate for our patients. |
References[edit | edit source]
- ↑ Minassian VA, Yan X, Lichtenfeld MJ, Sun H, Stewart WF. The iceberg of health care utilization in women with urinary incontinence. International urogynecology journal. 2012 Aug 1;23(8):1087-93.
- ↑ Hannestad YS, Rortveit G, Hunskaar S. Help-seeking and associated factors in female urinary incontinence. The Norwegian EPINCONT Study. Scandinavian journal of primary health care. 2002 Jan 1;20(2):102-7.
- ↑ University of Michigan. National poll on healthy aging. Available from: https://www.healthyagingpoll.org/sites/default/files/2018-11/NPHA_Incontinence-Report_FINAL-110118.pdf
- ↑ Griffith Health Physiotherapy for Urinary Incontinence - Griffith Physiotherapy Clinic Available from: https://www.youtube.com/watch?v=lg3PnVQ21Bs (last accessed 298.11.2019)
- ↑ 5.0 5.1 Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A. The standardisation of terminology of lower urinary tract function: Report from the standardisation sub‐committee of the International Continence Society. Neurourology and Urodynamics: Official Journal of the International Continence Society. 2002 Mar;21(2):167-78.
- ↑ Barry MJ, Link CL, McNaughton‐Collins MF, McKinlay JB, Boston Area Community Health (BACH) Investigators. Overlap of different urological symptom complexes in a racially and ethnically diverse, community‐based population of men and women. BJU international. 2008 Jan;101(1):45-51.
- ↑ 7.0 7.1 7.2 Ayeleke RO, Hay‐Smith EJ, Omar MI. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database of Systematic Reviews. 2013(11).
- ↑ Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003 Jan 1;61(1):37-49.
- ↑ Minassian VA, Drutz HP, Al‐Badr A. Urinary incontinence as a worldwide problem. International Journal of Gynecology & Obstetrics. 2003 Sep;82(3):327-38.
- ↑ Di Benedetto P, Coidessa A, Floris S. Rationale of pelvic floor muscles training in women with urinary incontinence. Minerva ginecologica. 2008 Dec 1;60(6):529.
- ↑ Fritel X, Ringa V, Quiboeuf E, Fauconnier A. Female urinary incontinence, from pregnancy to menopause: a review of epidemiological and pathophysiological findings. Acta obstetricia et gynecologica Scandinavica. 2012 Aug;91(8):901-10.
- ↑ Aoki Y, Brown HW, Brubaker L, Cornu JN, Daly JO, Cartwright R. Urinary incontinence in women. Nature reviews Disease primers. 2017 Jul 6;3(1):1-20.
- ↑ Van Delft K, Sultan AH, Thakar R, Schwertner‐Tiepelmann N, Kluivers K. The relationship between postpartum levator ani muscle avulsion and signs and symptoms of pelvic floor dysfunction. BJOG: An International Journal of Obstetrics & Gynaecology. 2014 Aug;121(9):1164-72.
- ↑ Cuadras D, Parés D. Hormonal Influence in Stress Urinary Incontinence During Pregnancy and Postpartum. Reproductive Sciences (Thousand Oaks, Calif.). 2022 Apr 26.
- ↑ Natural Childbirth. Childbirth and your pelvic floor. http://childbirth.amuchbetterway.com/childbirth-and-your-pelvic-floor/ (accessed 15 March 2011).
- ↑ Pirpiris A, Shek KL, Dietz HP. Urethral mobility and urinary incontinence. Ultrasound in Obstetrics and Gynecology. 2010 Oct;36(4):507-11.
- ↑ International Urogynecological Association. Stress urinary incontinence. Available from: https://www.yourpelvicfloor.org/media/Stress_Urinary_Incontinence_RV1.pdf
- ↑ McGuire EJ. Pathophysiology of stress urinary incontinence. Reviews in urology. 2004;6(Suppl 5):S11.
- ↑ Hage‐Fransen MA, Wiezer M, Otto A, Wieffer‐Platvoet MS, Slotman MH, Nijhuis‐van der Sanden MW, Pool‐Goudzwaard AL. Pregnancy‐and obstetric‐related risk factors for urinary incontinence, fecal incontinence, or pelvic organ prolapse later in life: A systematic review and meta‐analysis. Acta Obstetricia et Gynecologica Scandinavica. 2021 Mar;100(3):373-82.
- ↑ Lim YN, Dwyer PL. Effectiveness of midurethral slings in intrinsic sphincteric-related stress urinary incontinence. Current Opinion in Obstetrics and Gynecology. 2009 Oct 1;21(5):428-33.
- ↑ Pizzoferrato AC, Fauconnier A, Fritel X, Bader G, Dompeyre P. Urethral closure pressure at stress: A predictive measure for the diagnosis and severity of urinary incontinence in women. International neurourology journal. 2017 Jun;21(2):121.
- ↑ Schneeweiss J, Koch M, Umek W. The human urinary microbiome and how it relates to urogynecology. International urogynecology journal. 2016 Sep 1;27(9):1307-12.
- ↑ Pearce MM, Zilliox MJ, Rosenfeld AB, Thomas-White KJ, Richter HE, Nager CW, Visco AG, Nygaard IE, Barber MD, Schaffer J, Moalli P. The female urinary microbiome in urgency urinary incontinence. American journal of obstetrics and gynecology. 2015 Sep 1;213(3):347-e1.
- ↑ Steers WD. Pathophysiology of overactive bladder and urge urinary incontinence. Reviews in urology. 2002;4(Suppl 4):S7.
- ↑ Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, Markland AD. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstetrics and gynecology. 2014 Jan;123(1):141.
- ↑ 26.0 26.1 Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ, Pelvic Floor Disorders Network. Prevalence of symptomatic pelvic floor disorders in US women. Jama. 2008 Sep 17;300(11):1311-6.
- ↑ Lawrence JM, Lukacz ES, Nager CW, Hsu JW, Luber KM. Prevalence and co-occurrence of pelvic floor disorders in community-dwelling women. Obstetrics & Gynecology. 2008 Mar 1;111(3):678-85.
- ↑ 28.0 28.1 Lawrence JM, Lukacz ES, Liu IL, Nager CW, Luber KM. Pelvic floor disorders, diabetes, and obesity in women: findings from the Kaiser Permanente Continence Associated Risk Epidemiology Study. Diabetes Care. 2007 Oct 1;30(10):2536-3541.
- ↑ 29.0 29.1 Othman JA, Åkervall S, Milsom I, Gyhagen M. Urinary incontinence in nulliparous women aged 25-64 years: a national survey. American journal of obstetrics and gynecology. 2017 Feb 1;216(2):149-e1.
- ↑ Lukacz ES, Lawrence JM, Contreras R, Nager CW, Luber KM. Parity, mode of delivery, and pelvic floor disorders. Obstetrics & Gynecology. 2006 Jun 1;107(6):1253-60.
- ↑ Hutton EK, Hannah ME, Willan AR, Ross S, Allen AC, Armson BA, Gafni A, Joseph KS, Mangoff K, Ohlsson A, Sanchez JJ. Urinary stress incontinence and other maternal outcomes 2 years after caesarean or vaginal birth for twin pregnancy: a multicentre randomised trial. BJOG: An International Journal of Obstetrics & Gynaecology. 2018 Dec;125(13):1682-90.
- ↑ Hannestad YS, Lie RT, Rortveit G, Hunskaar S. Familial risk of urinary incontinence in women: population based cross sectional study. Bmj. 2004 Oct 14;329(7471):889-91.
- ↑ Wennberg AL, Altman D, Lundholm C, Klint Å, Iliadou A, Peeker R, Fall M, Pedersen NL, Milsom I. Genetic influences are important for most but not all lower urinary tract symptoms: a population-based survey in a cohort of adult Swedish twins. European urology. 2011 Jun 1;59(6):1032-8.
- ↑ Phelan S, Grodstein F, Brown JS. Clinical research in diabetes and urinary incontinence: what we know and need to know. The Journal of urology. 2009 Dec 1;182(6):S14-7.
- ↑ Matthews CA, Whitehead WE, Townsend MK, Grodstein F. Risk factors for urinary, fecal or dual incontinence in the Nurses’ Health Study. Obstetrics and gynecology. 2013 Sep;122(3):539.
- ↑ 36.0 36.1 36.2 36.3 36.4 36.5 Martin JL, Williams KS, Sutton AJ, Abrams KR, Assassa RP. Systematic review and meta-analysis of methods of diagnostic assessment for urinary incontinence. Neurourol Dynam 2006;25:674-683.
- ↑ 37.0 37.1 37.2 37.3 37.4 Laycock J. Pelvic muscle exercises: physiotherapy for the pelvic floor. Urologic Nursing 1994;14:136-40.
- ↑ Krhut J, Zachoval R, Smith PP, Rosier PF, Valanský L, Martan A, Zvara P. Pad weight testing in the evaluation of urinary incontinence. Neurourology and urodynamics. 2014 Jun;33(5):507-10.
- ↑ Ferreira CH, Bø K. The Pad Test for urinary incontinence in women. Journal of physiotherapy. 2015 Mar 3;61(2):98-.
- ↑ The National Institute for Diabetes and Digestive and Kidney Diseases Bladder Diary. Available from: https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems/diagnosis. [last accessed 17/8/2018]
- ↑ Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: a review. Jama. 2017 Oct 24;318(16):1592-604.
- ↑ Kenton KS, Smilen SW. Urinary Incontinence in Women. Obstetrics and gynecology. 2015 Nov 1;126(5):E66-81.
- ↑ NICE, N 2019, National Institute for Health and Care Excellence, Urinary incontinence in women: the management of urinary incontinence in women
- ↑ M Kenway Physical Therapist Pelvic Floor Exercises for Beginners Available from: https://www.youtube.com/watch?v=kQKR5uLkeUM (last accessed 28.11.2019)
- ↑ Doughty DB. Promoting continence: simple strategies with major impact. Ostomy Wound Management 2003;49:46-52.
- ↑ Alewijnse D, Metsemakers JFM, Mesters I, van den Borne. Effectiveness of pelvic floor muscle exercise therapy supplemented with a health education program to promote long-term adherence among women with urinary incontinence. Neurology and Urodynamics 2003;22:284-295.
- ↑ Ersin A, Demirbas SB, Tarhan F. Short term effects of home-based bladder training and pelvic floor muscle training in symptoms of urinary incontinence. Archivio Italiano di Urologia e Andrologia. 2020 Jun 24;92(2).
- ↑ Woodley SJ, Boyle R, Cody JD, Mørkved S, Hay‐Smith EJ. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database of Systematic Reviews. 2017(12).
- ↑ Mørkved S, Bø K. Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: a systematic review. Br J Sports Med. 2014 Feb 1;48(4):299-310.
- ↑ 50.0 50.1 Oliveira M, Ferreira M, Azevedo MJ, Firmino-Machado J, Santos PC. Pelvic floor muscle training protocol for stress urinary incontinence in women: A systematic review. Revista da Associação Médica Brasileira. 2017 Jul;63(7):642-50.
- ↑ 51.0 51.1 Dumoulin C, Cacciari LP, Hay‐Smith EJ. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews. 2018(10).
- ↑ Titman SC, Radley SC, Gray TG. Self-management in women with stress incontinence: strategies, outcomes and integration into clinical care. Research and reports in urology. 2019;11:111.
- ↑ Weber-Rajek M, Strączyńska A, Strojek K, Piekorz Z, Pilarska B, Podhorecka M, Sobieralska-Michalak K, Goch A, Radzimińska A. Assessment of the Effectiveness of Pelvic Floor Muscle Training (PFMT) and Extracorporeal Magnetic Innervation (ExMI) in Treatment of Stress Urinary Incontinence in Women: A Randomized Controlled Trial. BioMed Research International. 2020;2020.
- ↑ Ptak M, Ciećwież S, Brodowska A, Starczewski A, Nawrocka-Rutkowska J, Diaz-Mohedo E, Rotter I. The Effect of Pelvic Floor Muscles Exercise on Quality of Life in Women with Stress Urinary Incontinence and Its Relationship with Vaginal Deliveries: A Randomized Trial. BioMed research international. 2019;2019.
- ↑ 55.0 55.1 Alouini S, Memic S, Couillandre A. Pelvic Floor Muscle Training for Urinary Incontinence with or without Biofeedback or Electrostimulation in Women: A Systematic Review. International Journal of Environmental Research and Public Health. 2022 Feb 27;19(5):2789.
- ↑ 56.0 56.1 56.2 Burgio KL. Current perspectives on management of urgency using bladder and behavioral training. J Am Academy Nurse Pract 2004;16:4-7.
- ↑ The Canadian Continence Foundation. Treating incontinence. Available from: http://www.canadiancontinence.ca/EN/treatment.php
- ↑ 58.0 58.1 Payne CK. Behavioral therapy for overactive bladder. Urology 2000;55:3-6.
- ↑ Diokno AC, Newman DK, Low LK, Griebling TL, Maddens ME, Goode PS, Raghunathan TE, Subak LL, Sampselle CM, Boura JA, Robinson AE. Effect of Group-Administered Behavioral Treatment on Urinary Incontinence in Older Women: A Randomized Clinical Trial. JAMA internal medicine. 2018 Oct 1;178(10):1333-41.
- ↑ 60.0 60.1 Shamliyan TA, Kane RL, Wyman J, Wilt TJ. Systematic review: randomized, controlled trials of nonsurgical treatments for urinary incontinence in women. Ann Intern Med 2008;148:459-474.
- ↑ Chmielewska D, Stania M, Kucab–Klich K, Błaszczak E, Kwaśna K, Smykla A, Hudziak D, Dolibog P. Electromyographic characteristics of pelvic floor muscles in women with stress urinary incontinence following sEMG-assisted biofeedback training and Pilates exercises. PloS one. 2019;14(12).