Plantar Fibromatosis: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 8: | Line 8: | ||
== Definition/Description == | == Definition/Description == | ||
Ledderhose disease, also known as plantar fibromatosis or Morbus Ledderhose, is a (typically) small slow-growing thickening of the superficial fibromatoses which is actually a soft tissue tumor of the plantar aponeurosis similar in appearance to the disease which occurs in the palm of the hand ([http://www.physio-pedia.com/Dupuytren%E2%80%99s_Contracture disease of Dupuytren]). Basically it can be described as a benign fibroblastic proliferative disorder in which fibrous nodules may develop in the plantar aponeurosis, more specifically on the medial plantar side of the foot arch and on the forefoot region. The symptoms are swelling, pain is not usual and also a contraction is not applicable in the first stage. <ref name=" | Ledderhose disease, also known as plantar fibromatosis or Morbus Ledderhose, is a (typically) small slow-growing thickening of the superficial fibromatoses which is actually a soft tissue tumor of the plantar aponeurosis similar in appearance to the disease which occurs in the palm of the hand ([http://www.physio-pedia.com/Dupuytren%E2%80%99s_Contracture disease of Dupuytren]). Basically it can be described as a benign fibroblastic proliferative disorder in which fibrous nodules may develop in the plantar aponeurosis, more specifically on the medial plantar side of the foot arch and on the forefoot region. The symptoms are swelling, pain is not usual and also a contraction is not applicable in the first stage. <ref name="p4">Haedicke, G.J., Sturim, H.S. (1989). Plantar fibromatosis: an isolated disease. Plast Reconstr Surg. Level of evidence: 4</ref> <ref name="p6">Knobloch, K. and Vogt, K.M. (2012). High-energy focussed extracorporeal shockwave therapy reduces pain in plantar fibromatosis (Ledderhose’s disease). BMC Res Notes. Level of evidence: 2A</ref> <ref name="p9">Griffith, J.F., Wong, T.Y., Wong, S.M., and Metrweli, C. (2002). Sonography of plantar fibromatosis. AJR Am J Roentgenol. Level of evidence: 2A</ref> <ref name="p0">Murphey, M.D., Ruble, C.M., Tyszko, S.M., Zbojniewicz, A.M., Potter, B.K., and Miettinen, M. (2009). Musculoskeletal fibromatoses: radiologic-pathologic correlation. Radiographics. Level of evidence: 2C</ref><br> | ||
== Clinical Relevant Anatomy == | == Clinical Relevant Anatomy == | ||
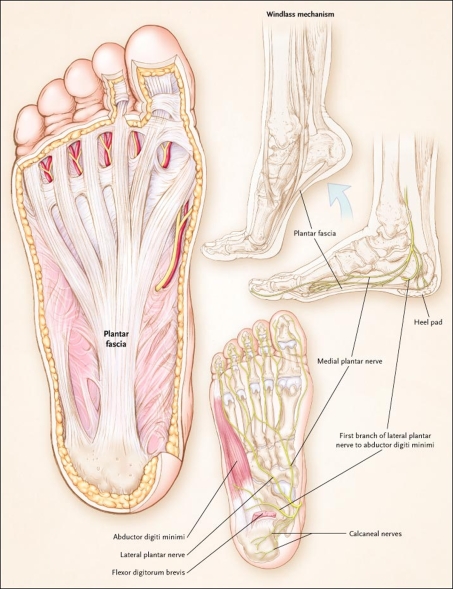
The plantar fascia, or aponeurosis is synonymous with the deep fascia of the sole of the foot. The plantar fascia is a strong connective tissue structure that consists of pearly white longitudinally-organized fibers. It begins at the medial tuberosity of the calcaneus where it is thinner and extends into a thicker center portion. This thicker portion is flanked by thinner lateral and medial portions. The thicker central portion of the plantar fascia then extends, into five different bands surrounding the digital tendons, to the plantar plates of the metatarsophalangeal joints and the bases of the proximal phalanges. <ref name=" | The plantar fascia, or aponeurosis is synonymous with the deep fascia of the sole of the foot. The plantar fascia is a strong connective tissue structure that consists of pearly white longitudinally-organized fibers. It begins at the medial tuberosity of the calcaneus where it is thinner and extends into a thicker center portion. This thicker portion is flanked by thinner lateral and medial portions. The thicker central portion of the plantar fascia then extends, into five different bands surrounding the digital tendons, to the plantar plates of the metatarsophalangeal joints and the bases of the proximal phalanges. <ref name="p1">Yusuf Ziya Tatli - Sameer Kapasi, The real risks of steroid injection for plantar fasciitis, with a review of conservative therapies, Human Press 2:3-9 (2008). Level of evidence 2A</ref> <ref name="p9" /> <ref name="p3">Eugene G. McNally, Shilpa Shetty. (2010). Plantar Fascia: Imaging Diagnosis and Guided Treatment. Department of Radiology, Nuffield Orthopaedic Centre, Oxford, Oxfordshire, United Kingdom. Level of evidence 1B</ref><br> | ||
<br> | <br> | ||
| Line 18: | Line 18: | ||
[[Image:Plantar and medial views.jpg]] | [[Image:Plantar and medial views.jpg]] | ||
'''Figure 1:''' Plantar and medial views of the foot demonstrating the origin and insertion of the plantar fascia and the location of nerves in proximity to the heel. <ref name=" | '''Figure 1:''' Plantar and medial views of the foot demonstrating the origin and insertion of the plantar fascia and the location of nerves in proximity to the heel. <ref name="p1" /> | ||
<br> | <br> | ||
| Line 24: | Line 24: | ||
== Epidemiology/ etiology == | == Epidemiology/ etiology == | ||
Ledderhose’s disease, is named after a German surgeon, Dr. Georg Ledderhose. He described the condition first in 1894 as an uncommon hyperproliferative plantar aponeurosis. <ref name=" | Ledderhose’s disease, is named after a German surgeon, Dr. Georg Ledderhose. He described the condition first in 1894 as an uncommon hyperproliferative plantar aponeurosis. <ref name="p2">Fausto de Souza, D. et al. (2010). Ledderhose Disease: An Unusual Presentation. The journal of Clinical and Aesthetic Dermatology, 3. Level of evidence: 3B</ref> <ref name="p6" /> | ||
Ledderhose’s disease is listed as a “rare disease” by the Office of Rare Diseases (ORD) of the National Institutes of Health (NIH), which means that it affects fewer than 200,000 people in the United State’s population. <ref name=" | Ledderhose’s disease is listed as a “rare disease” by the Office of Rare Diseases (ORD) of the National Institutes of Health (NIH), which means that it affects fewer than 200,000 people in the United State’s population. <ref name="p2" /> | ||
Plantar Fibromatosis occurs less frequently than the palmar disease, with a prevalence of 0.23% and usually more frequently in middle aged male individuals (30 – 50 years), thus men are affected twice as often as females and incidence increases with advancing age. Bilateral involvement is seen in 25% of patients.<ref name=" | Plantar Fibromatosis occurs less frequently than the palmar disease, with a prevalence of 0.23% and usually more frequently in middle aged male individuals (30 – 50 years), thus men are affected twice as often as females and incidence increases with advancing age. Bilateral involvement is seen in 25% of patients.<ref name="p5">Walker, E.A., Petscavage, J.M., Brian, P.L., Logie, C.I., Montini, K.M., Murphey, M.D. (2012). Imaging features of superficial and deep fibromatoses in the adult population. Sarcoma. Level of evidence: 2A</ref> <ref name="p0" /> | ||
Due to the lack of information about the formation of this condition, the etiology is still controversial. However, the plantar disease seems to have a multifactorial etiology, including potential factors such as diabetis mellitus, genetic and traumatic causes (like a puncture wound or a micro-tear), family history and cancer incidence. <ref name=" | Due to the lack of information about the formation of this condition, the etiology is still controversial. However, the plantar disease seems to have a multifactorial etiology, including potential factors such as diabetis mellitus, genetic and traumatic causes (like a puncture wound or a micro-tear), family history and cancer incidence. <ref name="p5" /> <ref name="p0" /> <ref name="p2">Pack, G.T. and Ariel, I.M. (1964). Treatment of cancer and allied diseases Volume VIII: Tumors of the soft somatic tissues and bone / by thirty-nine authors. P.B. Hoeber. Level of evidence: 4</ref><br> <br>Patients with the [http://www.physio-pedia.com/Dupuytren%E2%80%99s_Contracture contracture of Dupuytren], [http://www.physio-pedia.com/Diabetes diabetes mellitus], epilepsy, alcoholics with liver disease, stressfull work and keloids have more risk to develop the disease of Ledderhose and/or the disease of Peyronie's. <ref name="p5" /> <ref name="p6" /> <ref name="p9" /> <ref name="p0" /><br> | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
There will be a visible bulge, a soft- tissue mass composed of one or more subcutaneous nodules, on the medial (60%) or central (40%) plantar area of the foot same as a reduced capacity of bending the foot. The nodules may be multiple in 33% of cases and are typically slow growing. <ref name=" | There will be a visible bulge, a soft- tissue mass composed of one or more subcutaneous nodules, on the medial (60%) or central (40%) plantar area of the foot same as a reduced capacity of bending the foot. The nodules may be multiple in 33% of cases and are typically slow growing. <ref name="p2" /> <ref name="p4" /> <ref name="p7">Van der Veer, W.M., Hamburg, S.M., de Gast, A., and Niessen, F.B. (2008). Recurrence of plantar fibromatosis after plantar fasciectomy: single-center long-term results. Plast Reconstr Surg. Level of evidence: 2A</ref> <ref name="p8">Beckmann, J., Kalteis, T., Baer, W., Grifka J., and Lerch, K. (2004). Plantar fibromatosis: therapy by total plantarfasciectomy. Zentralbl Chir. Level of evidence: 4</ref> <ref name="p0" /><br> | ||
Not all patients have symptomatic complains. Complaints such as pain can occur after standing or walking for a long time, or when those nodules happen to grow and stiffen the affected structures of the foot due to a lack of space (e.g. neurovascular bundles, muscles or tendons). Nevertheless this disease typically does not cause symptoms such as contractures and patients frequently have normal radiographs.<ref name=" | Not all patients have symptomatic complains. Complaints such as pain can occur after standing or walking for a long time, or when those nodules happen to grow and stiffen the affected structures of the foot due to a lack of space (e.g. neurovascular bundles, muscles or tendons). Nevertheless this disease typically does not cause symptoms such as contractures and patients frequently have normal radiographs.<ref name="p5" /> <ref name="p0" /> | ||
Plantar fibromatosis is thought to have three phases: | Plantar fibromatosis is thought to have three phases: | ||
1) Proliferative phase: with nodular fibroblastic proliferation<br>2) Active phase: with collagen synthesis and deposition<br>3) Mature phase: with reduced fibroblastic activity and collagen maturation <ref name=" | 1) Proliferative phase: with nodular fibroblastic proliferation<br>2) Active phase: with collagen synthesis and deposition<br>3) Mature phase: with reduced fibroblastic activity and collagen maturation <ref name="p9" /><br> | ||
<br> | <br> | ||
| Line 46: | Line 46: | ||
[[Image:Subcutaneous nodules.png]] | [[Image:Subcutaneous nodules.png]] | ||
'''Figure 2''': Subcutaneous nodules on the lateral aspect of the right foot and medial aspect of left foot and retraction. <ref name=" | '''Figure 2''': Subcutaneous nodules on the lateral aspect of the right foot and medial aspect of left foot and retraction. <ref name="p2" /><br> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Ledderhose’s disease is sometimes associated with other forms of fibromatosis, such as:<br>• [http://www.physio-pedia.com/Dupuytren%E2%80%99s_Contracture Dupuytren’s disease]<br>• Peyronie's disease<br>• knuckle pads <ref name=" | Ledderhose’s disease is sometimes associated with other forms of fibromatosis, such as:<br>• [http://www.physio-pedia.com/Dupuytren%E2%80%99s_Contracture Dupuytren’s disease]<br>• Peyronie's disease<br>• knuckle pads <ref name="p2" /> | ||
Some others main differential diagnoses are: <br>• [http://www.physio-pedia.com/Plantarfasciitis plantar fasciitis ]<br>• chronic rupture of the plantar fascia <ref name=" | Some others main differential diagnoses are: <br>• [http://www.physio-pedia.com/Plantarfasciitis plantar fasciitis ]<br>• chronic rupture of the plantar fascia <ref name="p9" /> <br> | ||
== Diagnostic Procedures<br> == | == Diagnostic Procedures<br> == | ||
| Line 60: | Line 60: | ||
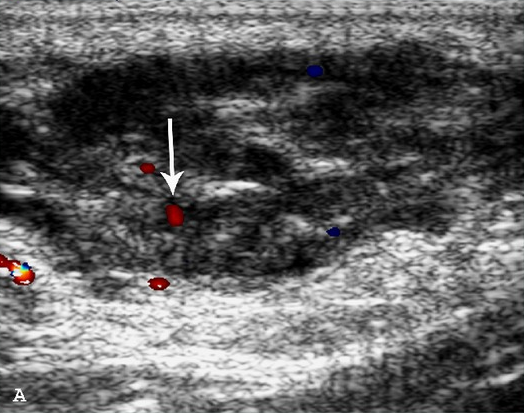
Evaluation is therefore most commonly performed with ultrasound and MRI. Sonographic imaging demonstrates a well-defined (64%) or poorly defined (36%) fusiform mass in the soft tissues adjacent to the plantar aponeurosis. <br> | Evaluation is therefore most commonly performed with ultrasound and MRI. Sonographic imaging demonstrates a well-defined (64%) or poorly defined (36%) fusiform mass in the soft tissues adjacent to the plantar aponeurosis. <br> | ||
Plantar fibroma may be heterogeneous and hypoechoic (76%) or isoechoic (24%) relative to the plantar fascia. Posterior acoustic enhancement (20%), cystic components, and intratumoral hypervascularity (8%) have also been described. <ref name=" | Plantar fibroma may be heterogeneous and hypoechoic (76%) or isoechoic (24%) relative to the plantar fascia. Posterior acoustic enhancement (20%), cystic components, and intratumoral hypervascularity (8%) have also been described. <ref name="p5" /> <ref name="p9" /> <ref name="p0" /> <ref name="p1">Robbin M.R., Murphey M.D., Temple H.T., Kransdorf M.J., Choi J.J. (2001). Imaging of Musculoskeletal Fibromatosis. RadioGraphics, the journal of continuing medical education in radiology. Level of evidence: 1B</ref><br> | ||
[[Image:Doppler image.png]] | [[Image:Doppler image.png]] | ||
'''Figure 3''': A 54-year-old male who presents with left foot pain for one year. A longitudinal ultrasound color Doppler image demonstrates a soft tissue mass with heterogeneous echotexture and internal color Doppler flow (arrow). <ref name=" | '''Figure 3''': A 54-year-old male who presents with left foot pain for one year. A longitudinal ultrasound color Doppler image demonstrates a soft tissue mass with heterogeneous echotexture and internal color Doppler flow (arrow). <ref name="p5" /> | ||
<br> | <br> | ||
| Line 70: | Line 70: | ||
[[Image:T1 weighted.png]] | [[Image:T1 weighted.png]] | ||
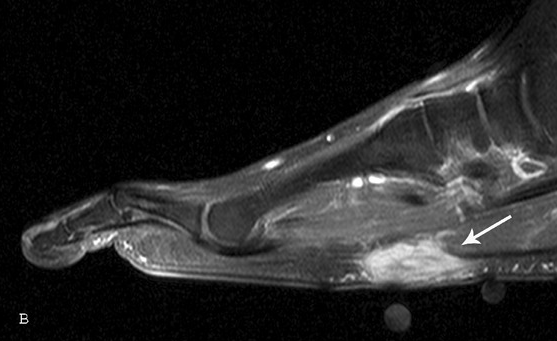
'''Figure 4:''' Sagittal T1-weighted fat saturation postcontrast sequence demonstrates a fusiform, enhancing lesion with linear extension along the plantar aponeurosis (arrow). <ref name=" | '''Figure 4:''' Sagittal T1-weighted fat saturation postcontrast sequence demonstrates a fusiform, enhancing lesion with linear extension along the plantar aponeurosis (arrow). <ref name="p5" /> | ||
<br> | <br> | ||
| Line 76: | Line 76: | ||
[[Image:T1 weighted 2.png]] | [[Image:T1 weighted 2.png]] | ||
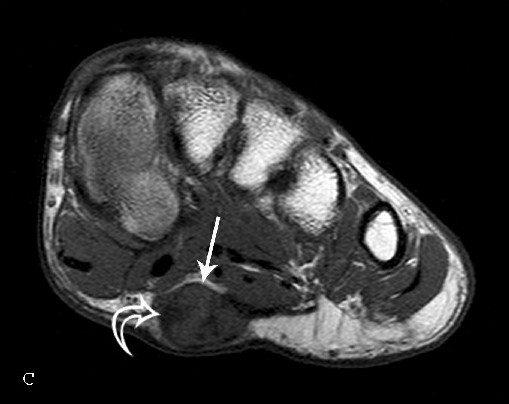
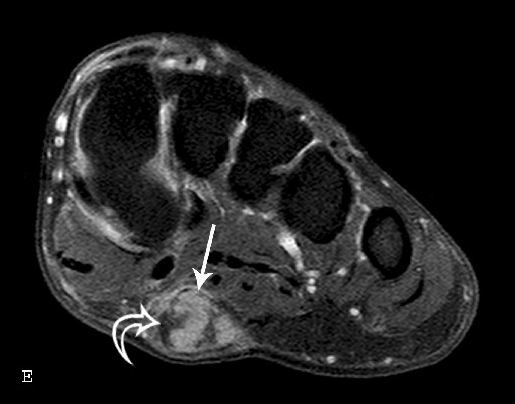
'''Figure 5''': Short axis T1-weighted sequence reveals lesion signal intensity similar to skeletal muscle. There is heterogeneity with several foci of low signal (curved arrows) within the lesion. <ref name=" | '''Figure 5''': Short axis T1-weighted sequence reveals lesion signal intensity similar to skeletal muscle. There is heterogeneity with several foci of low signal (curved arrows) within the lesion. <ref name="p5" /> | ||
<br> | <br> | ||
| Line 82: | Line 82: | ||
[[Image:T1 weighted 3.png]] | [[Image:T1 weighted 3.png]] | ||
'''Figure 6''': T1- weighted postcontrast fat saturation sequence demonstrate marked heterogeneous enhancement (arrow).<ref name=" | '''Figure 6''': T1- weighted postcontrast fat saturation sequence demonstrate marked heterogeneous enhancement (arrow).<ref name="p5" /> | ||
== Conservative Management == | == Conservative Management == | ||
Treatment of plantar fibromatosis is conservative in the majority of patients and consists of stretching, physiotherapy, footwear modifications, pads or orthotics aimed at relieving symptoms. <ref name=" | Treatment of plantar fibromatosis is conservative in the majority of patients and consists of stretching, physiotherapy, footwear modifications, pads or orthotics aimed at relieving symptoms. <ref name="p2" /> <ref name="p8" /> <ref name="p0" /> Shockwave therapy seems also to be effective by reducing pain and softening the nodules. <ref name="p6" /> <ref name="p5">Knobloch K., Vogt PM., (2012), High-energy focused extracorporal shockwave therapy reduces pain in plantar fibromatosis (Ledderhose’s disease). Hannover Medical School, Germany. Level of evidence 2B</ref><br> | ||
== Medical Management == | == Medical Management == | ||
Even though recovery with non-invasive treatment is possible, more severe lesions require more invasive approaches. Surgical treatment is indicated in cases of persistent pain or if large, infiltrative lesions cause significant disability and/or are refractory to conservative management. The standard procedure and the most functional surgery includes a partial fasciectomy of the plantar aponeurosis in order to release the tension. After partial resection, there is a high recurrence rate with increased risk of complications and more aggressive ingrowth into anatomical structures. Some authors recommend a complete fasciectomy as the primary procedure of choice. Postoperative radiotherapy can be used to diminish the chance of recurrence. <ref name=" | Even though recovery with non-invasive treatment is possible, more severe lesions require more invasive approaches. Surgical treatment is indicated in cases of persistent pain or if large, infiltrative lesions cause significant disability and/or are refractory to conservative management. The standard procedure and the most functional surgery includes a partial fasciectomy of the plantar aponeurosis in order to release the tension. After partial resection, there is a high recurrence rate with increased risk of complications and more aggressive ingrowth into anatomical structures. Some authors recommend a complete fasciectomy as the primary procedure of choice. Postoperative radiotherapy can be used to diminish the chance of recurrence. <ref name="p2" /><ref name="p6" /><ref name="p7" /><ref name="p8" /><ref name="p0" /><ref name="p1" /><ref name="p6">Seegenschmiedt MH, Attassi M,. (2003), Radiation therapy for Morbus Ledderhose – Indication and clinical results. Essen, Germany. Level of evidence 2B</ref> | ||
{| width="100%" cellspacing="1" cellpadding="1" | {| width="100%" cellspacing="1" cellpadding="1" | ||
| Line 98: | Line 98: | ||
|} | |} | ||
<br>Medical treatment can also consist of non-steroidal anti-rheumatic drugs or local cortisone injections. <ref name=" | <br>Medical treatment can also consist of non-steroidal anti-rheumatic drugs or local cortisone injections. <ref name="p3">Thomas G.MCP., Robroy L.M., Mark W.C., Dane K.W., James J.R., Joseph J.G., (2008) , Heel Pain – Plantar Fasciitis : Clinical Practice Guidelines Linked to the International Classification of Function, Disability and Health from the Orthopaedic Section of the American Physical Therapy Association, J Orthop Sports Phys Therp. Level of evidence : 2</ref> | ||
During the first phase (1st-3rd day), the foot of the patient will be placed in a position of function. Mainly this phase will consist of: prevention of post-operative oedema by raising the foot and having the patient mobilize his/her toes. If postoperative immobilization is not provided, active mobilization will be required from the first day. | During the first phase (1st-3rd day), the foot of the patient will be placed in a position of function. Mainly this phase will consist of: prevention of post-operative oedema by raising the foot and having the patient mobilize his/her toes. If postoperative immobilization is not provided, active mobilization will be required from the first day. | ||
<br> Prefabricated or custom foot orthoses can be used to provide short-term (3 months) reduction in pain and improvement in function. There appear to be no differences in the amount of pain reduction or improved function created by custom foot orthoses in comparison to prefabricated orthoses. There is currently no evidence to support the use of prefabricated or custom foot orthoses for long-term (1 year) pain management or function improvement. <ref name=" | <br> Prefabricated or custom foot orthoses can be used to provide short-term (3 months) reduction in pain and improvement in function. There appear to be no differences in the amount of pain reduction or improved function created by custom foot orthoses in comparison to prefabricated orthoses. There is currently no evidence to support the use of prefabricated or custom foot orthoses for long-term (1 year) pain management or function improvement. <ref name="p3">Thomas G.MCP., Robroy L.M., Mark W.C., Dane K.W., James J.R., Joseph J.G., (2008) , Heel Pain – Plantar Fasciitis : Clinical Practice Guidelines Linked to the International Classification of Function, Disability and Health from the Orthopaedic Section of the American Physical Therapy Association, J Orthop Sports Phys Therp. Level of evidence : 2</ref><ref name="p2" /><ref name="p6" /><ref name="p7" /><ref name="p8" /> | ||
=== Postoperative Physical Therapy Management === | === Postoperative Physical Therapy Management === | ||
| Line 108: | Line 108: | ||
The wound healing phase (8-15th day) will consist of: mobilization of the free articulations, circulatory and scar tissue massage (although there is only weak evidence for massage in scar management), lymphatic drainage, pneumatic/air pressure therapy, recovery of the joint capsulas, cartilage and muscles of the toes (slow and painless passive mobilization, active mobilization, work on the posture extension), ionization, lasers, ultrasound if there is a bad wound healing. <br> | The wound healing phase (8-15th day) will consist of: mobilization of the free articulations, circulatory and scar tissue massage (although there is only weak evidence for massage in scar management), lymphatic drainage, pneumatic/air pressure therapy, recovery of the joint capsulas, cartilage and muscles of the toes (slow and painless passive mobilization, active mobilization, work on the posture extension), ionization, lasers, ultrasound if there is a bad wound healing. <br> | ||
Calf muscle and/or plantar fascia-specific stretching can be applied to provide short-term (2-4 months) pain relief and improvement in calf muscle flexibility. The dosage for this stretching can be either 3 times a day or 2 times a day utilizing either a sustained (3 minutes) or intermittent (20 seconds) stretching time, as neither dosage produced a better effect. <ref name=" | Calf muscle and/or plantar fascia-specific stretching can be applied to provide short-term (2-4 months) pain relief and improvement in calf muscle flexibility. The dosage for this stretching can be either 3 times a day or 2 times a day utilizing either a sustained (3 minutes) or intermittent (20 seconds) stretching time, as neither dosage produced a better effect. <ref name="p3" /> <ref name="p4">Shin TM, Bordeaux JS.(2012). The role of massage in scar management: a literature revision. Department of Dermatology, Cleveland, Ohio, USA. Level of evidence 1A</ref> | ||
The phase after the wound healing will consist of: circulation and scar massage, bath of hot water or paraffin with active movements, total recovery of the articular amplitudes (by using analytic and global active-passive exercises and postural extension if needed with a dynamic brace), recovery of the muscle force (manually and later on with growing mechano-therapy appliances).<br> | The phase after the wound healing will consist of: circulation and scar massage, bath of hot water or paraffin with active movements, total recovery of the articular amplitudes (by using analytic and global active-passive exercises and postural extension if needed with a dynamic brace), recovery of the muscle force (manually and later on with growing mechano-therapy appliances).<br> | ||
There is minimal evidence to support the use of manual therapy to provide short-term (1 to 3 months) pain relief and improved function. Suggested manual therapy procedures include anterior and posterior glides of tarsometatarsal, metatarsalphalangeal and interphalangeal joints.<ref name=" | There is minimal evidence to support the use of manual therapy to provide short-term (1 to 3 months) pain relief and improved function. Suggested manual therapy procedures include anterior and posterior glides of tarsometatarsal, metatarsalphalangeal and interphalangeal joints.<ref name="p3" /><br> | ||
== References<br> == | == References<br> == | ||
Revision as of 12:44, 6 June 2017
Original Editor - Anja Vanroelen
Top Contributors - Anja Vanroelen, Laura Ritchie, Kirenga Bamurange Liliane, Kim Jackson, Lucinda hampton, Admin, WikiSysop, 127.0.0.1 and Evan Thomas
Definition/Description[edit | edit source]
Ledderhose disease, also known as plantar fibromatosis or Morbus Ledderhose, is a (typically) small slow-growing thickening of the superficial fibromatoses which is actually a soft tissue tumor of the plantar aponeurosis similar in appearance to the disease which occurs in the palm of the hand (disease of Dupuytren). Basically it can be described as a benign fibroblastic proliferative disorder in which fibrous nodules may develop in the plantar aponeurosis, more specifically on the medial plantar side of the foot arch and on the forefoot region. The symptoms are swelling, pain is not usual and also a contraction is not applicable in the first stage. [1] [2] [3] [4]
Clinical Relevant Anatomy[edit | edit source]
The plantar fascia, or aponeurosis is synonymous with the deep fascia of the sole of the foot. The plantar fascia is a strong connective tissue structure that consists of pearly white longitudinally-organized fibers. It begins at the medial tuberosity of the calcaneus where it is thinner and extends into a thicker center portion. This thicker portion is flanked by thinner lateral and medial portions. The thicker central portion of the plantar fascia then extends, into five different bands surrounding the digital tendons, to the plantar plates of the metatarsophalangeal joints and the bases of the proximal phalanges. [5] [3] [6]
Figure 1: Plantar and medial views of the foot demonstrating the origin and insertion of the plantar fascia and the location of nerves in proximity to the heel. [5]
Epidemiology/ etiology[edit | edit source]
Ledderhose’s disease, is named after a German surgeon, Dr. Georg Ledderhose. He described the condition first in 1894 as an uncommon hyperproliferative plantar aponeurosis. [7] [2]
Ledderhose’s disease is listed as a “rare disease” by the Office of Rare Diseases (ORD) of the National Institutes of Health (NIH), which means that it affects fewer than 200,000 people in the United State’s population. [7]
Plantar Fibromatosis occurs less frequently than the palmar disease, with a prevalence of 0.23% and usually more frequently in middle aged male individuals (30 – 50 years), thus men are affected twice as often as females and incidence increases with advancing age. Bilateral involvement is seen in 25% of patients.[8] [4]
Due to the lack of information about the formation of this condition, the etiology is still controversial. However, the plantar disease seems to have a multifactorial etiology, including potential factors such as diabetis mellitus, genetic and traumatic causes (like a puncture wound or a micro-tear), family history and cancer incidence. [8] [4] [7]
Patients with the contracture of Dupuytren, diabetes mellitus, epilepsy, alcoholics with liver disease, stressfull work and keloids have more risk to develop the disease of Ledderhose and/or the disease of Peyronie's. [8] [2] [3] [4]
Characteristics/Clinical Presentation[edit | edit source]
There will be a visible bulge, a soft- tissue mass composed of one or more subcutaneous nodules, on the medial (60%) or central (40%) plantar area of the foot same as a reduced capacity of bending the foot. The nodules may be multiple in 33% of cases and are typically slow growing. [7] [1] [9] [10] [4]
Not all patients have symptomatic complains. Complaints such as pain can occur after standing or walking for a long time, or when those nodules happen to grow and stiffen the affected structures of the foot due to a lack of space (e.g. neurovascular bundles, muscles or tendons). Nevertheless this disease typically does not cause symptoms such as contractures and patients frequently have normal radiographs.[8] [4]
Plantar fibromatosis is thought to have three phases:
1) Proliferative phase: with nodular fibroblastic proliferation
2) Active phase: with collagen synthesis and deposition
3) Mature phase: with reduced fibroblastic activity and collagen maturation [3]
Figure 2: Subcutaneous nodules on the lateral aspect of the right foot and medial aspect of left foot and retraction. [7]
Differential Diagnosis[edit | edit source]
Ledderhose’s disease is sometimes associated with other forms of fibromatosis, such as:
• Dupuytren’s disease
• Peyronie's disease
• knuckle pads [7]
Some others main differential diagnoses are:
• plantar fasciitis
• chronic rupture of the plantar fascia [3]
Diagnostic Procedures
[edit | edit source]
The identification of characteristics of plantar fibromatosis on imaging can greatly assist with the clinical diagnosis. Cross-sectional imaging (ultrasonography, computer tomography, MRI) reveals the lesions location, extension and involvement of neighboring structures.
Evaluation is therefore most commonly performed with ultrasound and MRI. Sonographic imaging demonstrates a well-defined (64%) or poorly defined (36%) fusiform mass in the soft tissues adjacent to the plantar aponeurosis.
Plantar fibroma may be heterogeneous and hypoechoic (76%) or isoechoic (24%) relative to the plantar fascia. Posterior acoustic enhancement (20%), cystic components, and intratumoral hypervascularity (8%) have also been described. [8] [3] [4] [5]
Figure 3: A 54-year-old male who presents with left foot pain for one year. A longitudinal ultrasound color Doppler image demonstrates a soft tissue mass with heterogeneous echotexture and internal color Doppler flow (arrow). [8]
Figure 4: Sagittal T1-weighted fat saturation postcontrast sequence demonstrates a fusiform, enhancing lesion with linear extension along the plantar aponeurosis (arrow). [8]
Figure 5: Short axis T1-weighted sequence reveals lesion signal intensity similar to skeletal muscle. There is heterogeneity with several foci of low signal (curved arrows) within the lesion. [8]
Figure 6: T1- weighted postcontrast fat saturation sequence demonstrate marked heterogeneous enhancement (arrow).[8]
Conservative Management[edit | edit source]
Treatment of plantar fibromatosis is conservative in the majority of patients and consists of stretching, physiotherapy, footwear modifications, pads or orthotics aimed at relieving symptoms. [7] [10] [4] Shockwave therapy seems also to be effective by reducing pain and softening the nodules. [2] [8]
Medical Management[edit | edit source]
Even though recovery with non-invasive treatment is possible, more severe lesions require more invasive approaches. Surgical treatment is indicated in cases of persistent pain or if large, infiltrative lesions cause significant disability and/or are refractory to conservative management. The standard procedure and the most functional surgery includes a partial fasciectomy of the plantar aponeurosis in order to release the tension. After partial resection, there is a high recurrence rate with increased risk of complications and more aggressive ingrowth into anatomical structures. Some authors recommend a complete fasciectomy as the primary procedure of choice. Postoperative radiotherapy can be used to diminish the chance of recurrence. [7][2][9][10][4][5][2]
| [11] | [12] |
Medical treatment can also consist of non-steroidal anti-rheumatic drugs or local cortisone injections. [6]
During the first phase (1st-3rd day), the foot of the patient will be placed in a position of function. Mainly this phase will consist of: prevention of post-operative oedema by raising the foot and having the patient mobilize his/her toes. If postoperative immobilization is not provided, active mobilization will be required from the first day.
Prefabricated or custom foot orthoses can be used to provide short-term (3 months) reduction in pain and improvement in function. There appear to be no differences in the amount of pain reduction or improved function created by custom foot orthoses in comparison to prefabricated orthoses. There is currently no evidence to support the use of prefabricated or custom foot orthoses for long-term (1 year) pain management or function improvement. [6][7][2][9][10]
Postoperative Physical Therapy Management[edit | edit source]
The wound healing phase (8-15th day) will consist of: mobilization of the free articulations, circulatory and scar tissue massage (although there is only weak evidence for massage in scar management), lymphatic drainage, pneumatic/air pressure therapy, recovery of the joint capsulas, cartilage and muscles of the toes (slow and painless passive mobilization, active mobilization, work on the posture extension), ionization, lasers, ultrasound if there is a bad wound healing.
Calf muscle and/or plantar fascia-specific stretching can be applied to provide short-term (2-4 months) pain relief and improvement in calf muscle flexibility. The dosage for this stretching can be either 3 times a day or 2 times a day utilizing either a sustained (3 minutes) or intermittent (20 seconds) stretching time, as neither dosage produced a better effect. [6] [1]
The phase after the wound healing will consist of: circulation and scar massage, bath of hot water or paraffin with active movements, total recovery of the articular amplitudes (by using analytic and global active-passive exercises and postural extension if needed with a dynamic brace), recovery of the muscle force (manually and later on with growing mechano-therapy appliances).
There is minimal evidence to support the use of manual therapy to provide short-term (1 to 3 months) pain relief and improved function. Suggested manual therapy procedures include anterior and posterior glides of tarsometatarsal, metatarsalphalangeal and interphalangeal joints.[6]
References
[edit | edit source]
- ↑ 1.0 1.1 1.2 Haedicke, G.J., Sturim, H.S. (1989). Plantar fibromatosis: an isolated disease. Plast Reconstr Surg. Level of evidence: 4 Cite error: Invalid
<ref>tag; name "p4" defined multiple times with different content - ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Knobloch, K. and Vogt, K.M. (2012). High-energy focussed extracorporeal shockwave therapy reduces pain in plantar fibromatosis (Ledderhose’s disease). BMC Res Notes. Level of evidence: 2A Cite error: Invalid
<ref>tag; name "p6" defined multiple times with different content - ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Griffith, J.F., Wong, T.Y., Wong, S.M., and Metrweli, C. (2002). Sonography of plantar fibromatosis. AJR Am J Roentgenol. Level of evidence: 2A
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Murphey, M.D., Ruble, C.M., Tyszko, S.M., Zbojniewicz, A.M., Potter, B.K., and Miettinen, M. (2009). Musculoskeletal fibromatoses: radiologic-pathologic correlation. Radiographics. Level of evidence: 2C
- ↑ 5.0 5.1 5.2 5.3 Yusuf Ziya Tatli - Sameer Kapasi, The real risks of steroid injection for plantar fasciitis, with a review of conservative therapies, Human Press 2:3-9 (2008). Level of evidence 2A Cite error: Invalid
<ref>tag; name "p1" defined multiple times with different content - ↑ 6.0 6.1 6.2 6.3 6.4 Eugene G. McNally, Shilpa Shetty. (2010). Plantar Fascia: Imaging Diagnosis and Guided Treatment. Department of Radiology, Nuffield Orthopaedic Centre, Oxford, Oxfordshire, United Kingdom. Level of evidence 1B Cite error: Invalid
<ref>tag; name "p3" defined multiple times with different content Cite error: Invalid<ref>tag; name "p3" defined multiple times with different content - ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 Fausto de Souza, D. et al. (2010). Ledderhose Disease: An Unusual Presentation. The journal of Clinical and Aesthetic Dermatology, 3. Level of evidence: 3B Cite error: Invalid
<ref>tag; name "p2" defined multiple times with different content - ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 8.9 Walker, E.A., Petscavage, J.M., Brian, P.L., Logie, C.I., Montini, K.M., Murphey, M.D. (2012). Imaging features of superficial and deep fibromatoses in the adult population. Sarcoma. Level of evidence: 2A Cite error: Invalid
<ref>tag; name "p5" defined multiple times with different content - ↑ 9.0 9.1 9.2 Van der Veer, W.M., Hamburg, S.M., de Gast, A., and Niessen, F.B. (2008). Recurrence of plantar fibromatosis after plantar fasciectomy: single-center long-term results. Plast Reconstr Surg. Level of evidence: 2A
- ↑ 10.0 10.1 10.2 10.3 Beckmann, J., Kalteis, T., Baer, W., Grifka J., and Lerch, K. (2004). Plantar fibromatosis: therapy by total plantarfasciectomy. Zentralbl Chir. Level of evidence: 4
- ↑ Donald Pelto. Plantar Fibroma . Available from: http://www.youtube.com/watch?v=pjoLXaeD4E0 [last accessed 11/01/17]
- ↑ Nagler Foot Center. Plantar Fibromatosis - Dr. Sherman Nagler. Available from: http://www.youtube.com/watch?v=we8NXXYfCgk [last accessed 11/01/17]