Pes Planus: Difference between revisions
No edit summary |
(grammer correction, references) |
||
| (44 intermediate revisions by 14 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors ''' | '''Original Editors '''- [[User:Uchechukwu Chukwuemeka |Uchechukwu Chukwuemeka]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Download (2).jpg|thumb|alt=|Pes Planus A.k.a flat foot]] | |||
Pes planus/ pes planovalgus (or flat foot) is the loss of the medial longitudinal [[Arches of the Foot|arch of the foot]], heel valgus deformity, and medial [[Talus|talar]] prominence.<ref name=":0">Troiano G, Nante N, Citarelli GL. [https://annali.iss.it/index.php/anna/article/view/485 Pes planus and pes cavus in Southern]. Annali dell'Istituto superiore di sanita. 2017 Jun 7;53(2):142-5.</ref> This is often observed with the medial arch of the foot coming closer (than typically expected) to the ground or making contact with the ground. | |||
All typically developing infants are born with flexible flat feet, with arch development first seen around 3 years of age and then often only attaining adult values in arch height between 7 and 10 years of age.<ref>Squibb M, Sheerin K, Francis P. [https://www.mdpi.com/2227-9067/9/5/750 Measurement of the Developing Foot in Shod and Barefoot Paediatric Populations: A Narrative Review.] Children. 2022 May 19;9(5):750.</ref><ref name=":8">Evans AM, Karimi L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4551386/ The relationship between paediatric foot posture and body mass index: do heavier children really have flatter feet?]. Journal of foot and ankle research. 2015 Dec;8(1):1-7.</ref> | |||
== Classification == | |||
The classification of the pes planus is based on '''two aspects''': | |||
| *'''Arch height:''' The best parameter to characterize medial longitudinal arch structure was found to be a '''ratio of navicular height to foot length.''' It is accepted that the flatness of normal children’s feet and their age are ''inversely proportioned.''<ref name="p1" /> | ||
*'''Heel eversion angle:''' Heel eversion or hindfoot valgus is generally accepted as a normal finding in young, newly walking children and is expected to reduce with age. The eversion of the heel has been repeatedly used for determining the posture of the child’s foot. Resting calcaneal stance position is a more recent method. It has guided clinicians in assessment of the child’s foot posture and calcaneal eversion has been suggested to reduce by a degree every 12 months to a vertical position by age 7 years. A vertical heel is optimal for foot function. The average rear foot angle for children from 6 to16 years is 4° (raging from 0 to 9° valgus).<ref name="p7" /><ref name="p1" /> | |||
<nowiki/>''<nowiki/>'' | |||
*'''Whether the flat foot structure is rigid or flexible''' | |||
== | # '''Flexible flat foot (flexible FF)''': The longitudinal arches of the foot are present on heel elevation (tiptoe standing) and non-bearing but disappear with full weight bearing on the foot. | ||
#* FF is termed '''developmental''' FF when observed in infants and toddlers and is part of normal development. Between the ages of 8 and 10 however, a clinician may consider this a true FF.<ref name=":9">Kothari A, Bhuva S, Stebbins J, Zavatsky AB, Theologis T. [https://online.boneandjoint.org.uk/doi/full/10.1302/0301-620X.98B4.36059?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org An investigation into the aetiology of flexible flat feet: the role of subtalar joint morphology.]A The Bone & Joint Journal. 2016 Apr;98(4):564-8.</ref> | |||
# '''Rigid flat foot:''' The longitudinal arches of the foot are absent in both heel elevation (tiptoe standing) and weight bearing.<ref name=":1">Wilson DJ. Flexible vs Rigid Flat Foot, 2019. Available from: https://www.news-medical.net/health/Flexible-vs-Rigid-Flat-Foot.aspx (Accessed 29 June 2020)</ref>This is normally associated with underlying pathology.<ref name=":11">Halabchi F, Mazaheri R, Mirshahi M, Abbasian L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3684468/pdf/IJPD-23-247.pdf Pediatric flexible flatfoot; clinical aspects and algorithmic approach]. Iranian journal of pediatrics. 2013 Jun;23(3):247.</ref> | |||
== Epidemiology == | |||
Roughly 20% to 37% of the population has some degree of pes planus, With most cases being the flexible variety. It is more common in children (about 20-30% of children with some form of flat feet) with most children going on to develop a normal arch by 10 years old. Genetics plays a strong role with it typically running in families.<ref name=":4">Suciati T, Adnindya MR, Septadina IS, Pratiwi PP. [https://iopscience.iop.org/article/10.1088/1742-6596/1246/1/012063/meta Correlation between flat feet and body mass index in primary school students]. InJournal of Physics: Conference Series 2019 Jul 1 (Vol. 1246, No. 1, p. 012063). IOP Publishing.</ref><ref name=":6">Raj MA, Tafti D, Kiel J Pes Planus Available: https://www.ncbi.nlm.nih.gov/books/NBK430802/ (accessed 2.7.2022)</ref> | |||
== Etiology/Causes == | |||
The etiology of pes planus has several factors implicated and can be either '''congenital''' or '''acquired.'''<ref name=":3">Raj MA, Tafti D, Kiel J. Pes Planus (Flat Feet). StatPearl-NCBI Bookshelf, 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430802/ (Accessed 29 June 2020) | |||
</ref> | |||
=== '''Congenital Pes Planus''' === | |||
'''Congenital pes planus''' is classified as developing in the first years of life. Both flexible FF and rigid FF can be present. | |||
At birth and within early childhood pes planus is a '''typical observation of development''' and is termed '''flexible''' flat foot (FF). It is attributed to osseous and ligamentous laxity, immature neuromuscular control, and the presence of adipose tissue under the medial longitudinal arch (MLA), making the arch appear flat.<ref>Banwell HA, Paris ME, Mackintosh S, Williams CM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5975578/ Paediatric flexible flat foot: how are we measuring it and are we getting it right? A systematic review. Journal of foot and ankle research]. 2018 Dec;11(1):1-3.</ref>In fact, during the early years of gait in toddler years, a child will use their entire foot on the ground for balance. A shift of their weight-bearing axis to the 1st or 2nd metatarsal joint induces a flatfoot posture.<ref name=":12">Atik A, Ozyurek S. [https://pubmed.ncbi.nlm.nih.gov/28058304/ Flexible flatfoot]. Northern clinics of Istanbul. 2014;1(1):57.</ref> | |||
When flexible FF is observed in older children (typically those above 8 years of age) and adults, the following must be considered: | |||
* General/ global hypermobility, including conditions such as [[Ehlers-Danlos Syndrome|Ehlers-Danlos syndrome]] (EDH) and [[Down Syndrome (Trisomy 21)|Down Syndrome]]. | |||
* Conditions with increased tone, e.g. [[Cerebral Palsy Introduction|cerebral palsy]].<ref name="p2">Turriago CA, Arbeláez MF, Becerra LC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2686809/ Talonavicular joint arthrodesis for the treatment of pes planus valgus in older children and adolescents with cerebral palsy.] Journal of children's orthopaedics. 2009 Jun;3(3):179-83.</ref> | |||
* Higher [[Body Mass Index|body mass index]] (BMI).<ref name="p1">Chen KC, Yeh CJ, Tung LC, Yang JF, Yang SF, Wang CH. [https://pubmed.ncbi.nlm.nih.gov/21174119/ Relevant factors influencing flatfoot in preschool-aged children]. European journal of pediatrics. 2011 Jul;170(7):931-6.</ref> | |||
** A note: While increased BMI and even obesity have been attributed to increased predisposition to flexible FF, more recent investigations call these findings into question.<ref name=":8" /> These studies, which have taken into account a more comprehensive foot morphology (not simply footprint measurements) have not found higher rates of flexible FF in paediatric populations. These have, however, been done with participants with higher BMI and not necessarily a diagnosis of obesity.<ref name="p4">Evans AM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3102032/ The paediatric flat foot and general anthropometry in 140 Australian school children aged 7-10 years. Journal of foot and ankle research]. 2011 Dec;4(1):1-8.</ref> | |||
* Subtalar joint morphology. | |||
** Recent research has highlighted the variance in subtalar joints. One such study highlighted 2 different types: The first, a firmer supporting joint, and another weaker joint where the anterior articulation in the subtalar joint is absent. The absent articulation allows the FF posture to develop.<ref name=":9" /><br /> | |||
An example of '''rigid FF''' is tarsal coalition, where there is a failure of the tarsal bones to separate. This causes a bony, sometimes cartilaginous, or even fibrous bridge between two or more of the tarsal bones.<ref name=":10">SM Javad M, Ramin E, Taghi B. [https://www.academia.edu/28235002/Flatfoot_in_children_How_to_approach Flatfoot in children: how to approach?] Iran Journal of Paediatrics.2007. 17(No.2): 163-170.</ref> | |||
Other examples of congenital pes planus include:<ref name=":3" /> | |||
== | * Congenital vertical talus | ||
* Congenital talipes equinovarus | |||
* Tibial torsional deformity | |||
* Presence of the accessory navicular bone.<ref>Cheong IY, Kang HJ, Ko H, Sung J, Song YM, Hwang JH. [https://www.cambridge.org/core/journals/twin-research-and-human-genetics/article/genetic-influence-on-accessory-navicular-bone-in-the-foot-a-korean-twin-and-family-study/46E640E6A73957E41EB565CF95F245C5 Genetic influence on accessory navicular bone in the foot: a Korean twin and family study]. Twin Research and Human Genetics. 2017 Jun;20(3):236-41. | |||
</ref> | |||
* General ligament laxity | |||
* Genetic malformations such as [[Down Syndrome (Trisomy 21)|Down syndrome]] and [[Marfan Syndrome|Marfan syndrome]]<ref name=":1" /> | |||
* Familial factors<ref>Mosca VS. Flexible flatfoot in children and adolescents. J Child Orthop. 2010;4(2):107–121 | |||
</ref> | |||
* Peroneal spasm<ref name="p7">Cass AD, Camasta CA. [https://www.jfas.org/article/S1067-2516(10)00043-8/fulltext A review of tarsal coalition and pes planovalgus: clinical examination, diagnostic imaging, and surgical planning]. The Journal of foot and ankle surgery. 2010 May 1;49(3):274-93.</ref> | |||
* Vertical [[talus]]<ref name="p7" /> | |||
=== '''Acquired Pes Planus''' === | |||
'''Acquired pes planus''' may arise from: | |||
* [[Diabetes]]<ref>Cleveland Clinic. 2019. Available from:https://my.clevelandclinic.org/health/diseases/15961-adult-acquired-flatfoot#:~:text=In%20people%20with%20diabetes%2C%20a,notice%20as%20their%20foot%20collapses. (Accessed 29 June 2020)</ref> | |||
* [[Ankle and Foot|Foot and ankle]] injury such as [[Tibialis posterior rupture|rupture or dysfunction of the posterior tibial tendon]]. | |||
* Some medical conditions such as [[arthritis]], [[Spina Bifida|spina bifida]], [[Cerebral Palsy Introduction|cerebral palsy]], [[Arthrogryposis Multiplex Congenita|Arthrogyroposis]], and [[Duchenne Muscular Dystrophy|muscular dystrophy]].<ref name=":2">Berlet GC. Pes Planus (Flatfoot). Medscape, 2019. Available from: https://emedicine.medscape.com/article/1236652-overview#a8 (accessed 29 June 2020) | |||
</ref> | |||
* Flat feet can also occur as a result of pregnancy.<ref>Indy Podiatry. Common foot and ankle problems during pregnancy, 2019. Available from: https://indypodiatry.com/your-feet-during-pregnancy/#:~:text=Over%2Dpronation%2C%20or%20flat%20feet,feet)%20leading%20to%20significant%20pain. (accessed 29 June 2020) | |||
</ref><ref>Conder R, Zamani R, Akrami M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7739277/ The biomechanics of pregnancy: A systematic review.] Journal of Functional Morphology and Kinesiology. 2019 Dec 2;4(4):72.</ref> | |||
* Iatrogenic factors such as [[Tibialis Posterior|posterior tibialis]] tendon (PTT) transfer.<ref name=":2" /><ref>Pecheva M, Devany A, Nourallah B, Cutts S, Pasapula C. [https://pubmed.ncbi.nlm.nih.gov/29454275/ Long-term follow-up of patients undergoing tibialis posterior transfer: is acquired pes planus a complication?]. The Foot. 2018 Mar 1;34:83-9. | |||
</ref> | |||
* Traumatic injury<ref name=":11" /> | |||
< | <div class="row"><div class="col-md-6"> {{#ev:youtube|GPS10HfgYDY|250}} <div class="text-right"><ref>Mount Sinai Health Systems. What causes flat foot? Available from: http://www.youtube.com/watch?v=GPS10HfgYDY [last accessed 29/6/2020]</ref></div></div> | ||
<div class="col-md-6">{{#ev:youtube|9tlzxA8o0w0|250}} <div class="text-right"><ref>East Coast Podiatry. Flat Feet (Pes Planus) - Georgina Tay, Singapore Podiatrist . Available from: http://www.youtube.com/watch?v=9tlzxA8o0w0 [last accessed 29/6/2020]</ref></div></div> | |||
</div> | |||
== Clinically Relevant Anatomy == | |||
[[File:Medial arch of the foot.gif|thumb|alt=|Medial arch of the foot]] | |||
The calcaneus, navicular, talus, first three cuneiforms, and the first three metatarsals make up the medial longitudinal arch. This arch is supported by posterior tibial tendon, [[Spring Ligament|plantar calcanea navicular ligament]], [[Medial ankle ligament|deltoid ligament]], [[Plantar Fasciitis|plantar aponeurosis]], and [[flexor hallucis longus]] and [[Flexor Hallucis Brevis|brevis]] muscles. Dysfunction or injury to any of these structures may cause acquired pes planus.[[File:Flat foot xray.jpg|thumb|Flat foot Xray |alt=]]See [[Arches of the Foot]] | |||
== | == Pathophysiology == | ||
The pathophysiology of pes planus can vary greatly depending on whether it is '''congenital''' or '''acquired''', and then whether it is '''flexible''' or '''fixed'''. | |||
In considering developmental flatfoot, the medial longitudinal arch of the foot normally develops by the age of 5 or 6. This occurs as the fat pad in babies is gradually absorbed, balance improves and skilled movements are acquired. In some children, however, the arch fails to develop which may be a result of tightness in the calf muscles, laxity in the [[Achilles Tendon|Achilles tendon]] or poor [[Core Stability|core]] stability in other areas such as around the hips.<ref name="p3">Oeffinger DJ, Pectol Jr RW, Tylkowski CM. [https://pubmed.ncbi.nlm.nih.gov/11154928/ Foot pressure and radiographic outcome measures of lateral column lengthening for pes planovalgus deformity]. Gait & posture. 2000 Dec 1;12(3):189-95.</ref><ref name="p6">Evans AM. [https://books.google.com/books?hl=en&lr=&id=9Kk19h5Ku-gC&oi=fnd&pg=PP1&dq=Pediatrics+%E2%80%93+Angela+Evans+and+Ian+Mathieson+%E2%80%93+Elsevier+%E2%80%93+2010+A1&ots=V7SxbdjzDx&sig=IRnIdSiA499Xlp7thF5vFO6TaFc Pocket Podiatry: Paediatrics E-Book]. Elsevier Health Sciences; 2010 Jan 26.</ref> | |||
''' | ===== Dynamic factors ===== | ||
'''Soft tissue factors''' | |||
< | * [[Posterior Tibial Tendon Dysfunction|Insufficiency of the posterior tibial tendon]]: When this occurs, forefoot valgus occurs. Over the long term this produces achilles tendon contractures and transforms the gastrocnemius and soleus muscle complex into heel everters (rather than inverters).<ref name=":10" /> | ||
< | * When a peroneal spastic flatfoot is seen, the peroneal tendon which crosses over the subtalar joint often goes into spasm. This is secondary to subtalar inflammation.<ref name=":10" /> | ||
* Other muscular dysfunctions can occur: | |||
** After illness or enforced recumbency, the muscles may temporarily be weak and the arch consequently falls when walking is resumed. | |||
** A more lasting form of muscle weakness accompanies a generally '''poor posture'''. | |||
** The child (often a pre-adolescent girl) presents a familiar flabby contour with head stuck forward, mouth open, chest flat, back rounded and abdomen protuberant. | |||
** The gluteal muscles are concerned largely with posture (Wiles 1949). They help to straighten the hip and knee, and to twist the limb outwards. This twist can not be imparted to the foot which is anchored to the ground, and so the rest of the limb turns outwards relative to the foot. As a result, ''the arch is lifted and the line of weight corrected only when the glutei work properly''. | |||
'''Neurological factors''' | |||
* In normal development, a baby has to learn to balance first its head, then its trunk, and eventually to balance the whole body on the feet. The difficult art is not required during the early months of life; but sometimes the balancing reflexes fail to develop even after the child has begun to walk. In that event, the arch inevitably collapses with body weight. Myelination of the pyramidal fibers to the foot is incomplete at birth and the plantar responses in babies is extensor. If the infantile flat foot persists into early childhood, the extensor responses may persist too, and it is tempting to assume that balancing cannot be easily learned until myelination is complete. | |||
===== Static factors ===== | |||
< | * Boney architecture of the medial longitudinal arch. Here '''altered morphology''' of the joints of the midfoot would affect stability.<ref name=":10" /> | ||
* Fixed or rigid pes planus is due to a '''structural abnormality'''. As noted in etiology, this most often presents as a tarsal coalition. Limited range is seen in the subtalar and midfoot motion when there is a failure of tarsal bones to separate. This coalition can be cartilaginous, fibrous or even boney. This condition often causes pain and inflammation of the joints.<ref name=":10" />Other conditions associated with rigid pes planus include accessory navicular bone, congenital vertical talus or other congenital hindfoot pathology.<ref name=":3" /> | |||
== | * The [[Spring Ligament|spring ligament complex]] has been noted as an important stabiliser, but clarity still lacks in the literature. Plantar fascia offers stability to the medial longitudinal arch via the [[Windlass Test|windlass effect]]. In conditions where the laxity of these tissues is affected, for example in EDH, arch stability can be compromised.<ref name=":10" />In a study performed in 1993 on cadavers, the most important structure found for supporting the foot arch was the plantar fascia, followed by the talonavicular and spring ligaments.<ref name=":12" /> | ||
* The bony arch of the foot is potentially unstable and is bound together by ligaments. They withstand short-term stresses. Their primary function is to act as sensory end organs, so when stretched, appropriate muscles are reflexively brought into action. Even the most anatomically perfect foot will become rapidly and grossly flat unless it has muscles of good bulk and tone to support it. The ''physiological fault'' may lie in the ''muscle'' itself or its ''nervous control.'' | |||
== Characteristics/Clinical Presentation == | |||
== | * '''History''' | ||
** In adults: Frequent "rolling of the ankle"/ ankle sprains | |||
** Children presenting with pes planus are generally asymptomatic, usually only becoming symptomatic during adolescence.<ref name=":10" /> | |||
** '''Pain''' is often felt by indicated at the medial longitudinal arch and ankle. In children and adolescents pain secondary to flatfeet may be described as pain in the arch of the feet or cramps at night.<ref name="p2" /> In adults there may be complaints of [[Pain-Modulation|pain]] due to strained muscles and connecting tissues in the midfoot, heel, lower leg, knee, hip, and or back. In more advanced changes client may complain of an altered gait pattern.<ref name=":6" /> | |||
- | *'''Observation:''' | ||
** The foot may present as flat or 'rocker-bottom'.<ref name=":10" /> | |||
** In standing - Calcaneal valgus is apparent, the medial arch will appear dropped and there will be foot eversion.<ref name=":10" /> | |||
** Gait<ref name=":10" /> | |||
*** Test stance on medial and lateral borders of feet to assess mobility of foot joints. | |||
*** Walking on heels. Being able to walk on heels demonstrates flexibility of the achilles tendon. | |||
** Viewed from posteriorly, looking for the "too many toes sign"<ref name=":6" /> | |||
** Look at running or walking shoes <ref name=":10" />Uneven distribution of body weight with resultant one-sided wear of shoes leading to further injuries.<ref name=":2" /> | |||
= | * '''With palpation:'''<ref name=":10" /> | ||
** A contracted [[Achilles Tendon|achilles tendon]] may show as a limitation in dorsiflexion. | |||
**''Test subtalar and transverse tarsal motion''. Flexible pes planus will allow for mobility in these joints. | |||
***''Subtalar motion'': Examiner stablises ankle with one hand, calcanues in the other. The calcaneus is then inverted and everted. Normal ROM is between 20° and 60°, Inversion being 2x the ROM of eversion. | |||
***''Tarsal motion'': Grasp the calcaneus in one hand and forefoot in the other. The normal adduction of forefoot is about 30°, abduction about 15°. If ranges are less consider coalition. | |||
Ask the client about the onset of deformity, timing of symptoms, severity of past and current symptoms, history of trauma, family history, surgical history, and past medical history (including hypertension, diabetes, rheumatoid arthritis, sensory neuropathies, seronegative spondyloarthropathies, and obesity<ref name=":6" />). [[File:Flat feet.jpg|thumb|170x170px|alt=|Flat foot]] | |||
== | == Associated Co-morbidities == | ||
Co-morbidities include but not limited to neurological conditions such as cerebral palsy; genetics e.g. [[Down Syndrome (Trisomy 21)|Down syndrome]], [[Marfan Syndrome|Marfan syndrome]] or [[Ehlers-Danlos Syndrome]]; [[Charcot-Marie-Tooth Disease: A Case Study|charcot joint]]; tibialis posterior dysfunction; Obesity; arthropathies;<ref>Lowth M. Pes Planus (Flat feet). Patient, 2016. Available from: https://patient.info/doctor/pes-planus-flat-feet (Accessed 30 June 2020)</ref> Shprintzen-Goldberg syndrome.<ref>Yadav S, Rawal G. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5052323/pdf/PAMJ-23-227.pdf Shprintzen-Goldberg syndrome: A rare disorder]. Pan African Medical Journal. 2016; 23:227 doi:10.11604/pamj.2016.23.227.7482</ref> | |||
== Diagnostic Procedure == | |||
[[File:Flat foot.jpg|alt=|right|frameless]] | |||
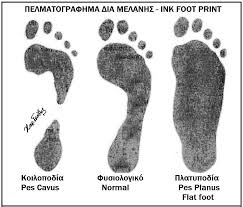
* '''Footprints:''' It is still controversial if footprints reflect the real morphology of the medial longitudinal arch. Recent development found an initial correlation between dynamic pressure patterns and static foot-prints.<ref name="p7" /> | |||
* '''X-rays''' are used to categorise the feet as having normal, slightly flat and moderate arches. In FF this is not routine.<ref name=":10" /> | |||
* [[Foot Posture Index (FP1-6)|Foot-posture index]] (FPI-6)<ref name="p6" /> | |||
* '''Supination resistance test''' <ref name="p6" /><ref name="p7" />: This test is used to estimate the magnitude of pronatory moments. The foot is manually supinated. The higher the force required, the greater the supination resistance and the stronger the pronatory forces. This test is subjective. | |||
* '''Jack’s test and [[Feiss Line Test|Feiss angle]] ('''are related) <ref name="p6" />: Performing the Jack’s test. The hallux is manually dorsiflexed while the child is standing. If the medial longitudinal arch rises due to dorsiflexion of the hallux, the foot is considered a flexible flat foot. If the medial longitudinal arch remains unchanged, the test designates a rigid flat foot. The purpose of this test is to check the foot flexibility and the onset of the windlass mechanism by tensioning the plantar fascia trough the extension of the first metatarsophalangeal joint. The Feiss line is the line interconnecting malleolus medialis, navicular and first metatarsal head. The inclination of this line with the ground increases when the first metatarsophalangeal joint is dorsiflexed (Jack’s test). This dorsiflexion activates forefoot supination and raises the arch height (140°± 6°).<ref name="p6" /> | |||
* '''Tip-toe'''<ref name=":10" />To differentiate fixed and flexible pes planus. | |||
* '''Ankle range''' <ref name="p6" /><ref name="p7" />: Children’s ankle range assessment is generally an unreliable measure, as typically assessed when the child is non-weight-bearing. So it is suggested that therapists look at a child’s ability to squat, heel walk and increase stride length.<ref name="p6" /> | |||
== Medical Management == | |||
=== Flexible Pes planus === | |||
The merit of treatment for all flexible FF remains ambiguous, with evidence showing that foot orthoses produces improvements in children with pes planus. It remains difficult to conclude if spontaneous physiological arch improvement occurred or the effect of intervention caused the arch improvement. | |||
* There is little evidence for treatment of asymptomatic, flexible, pediatric flat feet in a child who have no underlying medical issues.<ref name=":10" /> | |||
* Treatment of symptomatic, flexible flat feet is generally accepted for children with contributory background factors or secondary complications, or if pes planus persists past childhood.<ref name="p2" /> | |||
* Evidence supports the use of non surgical interventions for painful pes planus. | |||
* The child should be fitted with a flat, lace-up shoe with a firm heel and MLA support, a broad and deep toe box and the ‘toe break’ at the junction between the anterior third and posterior two-thirds of the shoe.<ref name=":7">Turner C, Gardiner MD, Midgley A, Stefanis A. [https://www1.racgp.org.au/ajgp/2020/may/paediatric-pes-planus A guide to the management of paediatric pes planus.] Australian journal of general practice. 2020 May;49(5):245-9.</ref>In children 10 years and older, FF is considered permanent, therefore long term othotics can be used to prevent secondary problems, especially in overweight or athletically active children.<ref name=":10" /> | |||
Treatment is based on etiology and [[NSAIDs in the Management of Rheumatoid Arthritis|NSAIDS]] are sufficient for [[Pain Medications|pain]]. | |||
== < | === Rigid Pes planus === | ||
Surgery is required in ''rigid pes planus'' and in cases resistant to therapy to reduce symptoms.<ref>Henry JK, Shakked R, Ellis SJ. [https://journals.sagepub.com/doi/pdf/10.1177/2473011418820847 Adult-acquired flatfoot deformity. Foot & ankle orthopaedics]. 2019 Jan 14;4(1):2473011418820847.</ref> Most surgical methods aim at realigning foot shape and mechanics. These surgeries could be tendon transfers, realignment osteotomies, arthrodesis and where other surgeries fail, triple arthrodesis is performed<ref name=":5">Carr JB, Yang S, Lather LA. [https://publications.aap.org/pediatrics/article-abstract/137/3/e20151230/81376 Pediatric pes planus: a state-of-the-art review]. Pediatrics. 2016 Mar 1;137(3). | |||
</ref> | |||
For the congenital pes valgus treatment, researchers have defined the best possible treatments depending on the age of the person/child. | |||
*In a child younger than 2 years, an extensive release with lengthening of the Achilles tendon and fixation procedure is recommended. It is less invasive than other techniques, because there is no tendon transfer or bony procedures needed. The explanation could be because of the greater adaptability of the cartilaginous structures. | |||
*In a child with neural tube defect, younger than 2 years of age, an extensive release with tendon transfer procedure is recommended. A neuromuscular imbalance between a weak Tibialis Posterior tendon and a strong evertor of the foot could be responsible for this condition. Good results are found for this operation which aims to correct this imbalance. | |||
= | *In a child older than 2 years of age, an extensive release with tendon transfer procedure is proposed. Surgical correction becomes increasingly difficult in older children because of secondary changes in the bone. This procedure resulted as the best for children whose walking and standing potential has been established. | ||
In case of failure of precedent procedures, a bony procedure may be considered. There are good results for children of 4 years and older with these procedures. Every surgery is usually followed by a plaster cast for two to three months. The recovery after surgery takes about 6 months to 1 year to heal completely and to recover completely on a functional level.<ref name="p1" /><ref name="p2" /><ref name="p4" /> | |||
== Physical Therapy Management == | |||
The aim of physical therapy is to minimize pain, increase foot flexibility, strengthen weak muscles, train proprioception, and patient education and reassurance. As part of the assessment process, the physiotherapist can assist in evaluating the gait, gross motor skills and the impact the foot deformity has on functional activities. Assess endurance, speed, fatigability, pain and ability to walk on different terrains, with a focus on '''assessing function, not just structural abnormalities.''' | |||
'''Pain management''' includes rest, activity modification, [[cryotherapy]], [[massage]], and nonsteroidal anti-inflammatory medication. [[Therapeutic Ultrasound|Ultrasound]] and [[Electrical Stimulation - Its role in upper limb recovery post-stroke|pulsed electrical stimulation]] can also be used for pain relief. Electric stimulation will aid blood circulation, promoting healing processes and diminishing discomfort and oedema. | |||
[[Category: | * Encouraging walking bear foot | ||
* [[Stretching|Flexibility]] [[Therapeutic Exercise|exercises]] are passive ROM exercises of the ankle and all foot joints; [[Stretching- an Evidence Based Guide|Stretching]] of [[gastrocnemius]] [[soleus]] complex and peroneus brevis muscles to facilitate varus and foot adduction; Heel-cord stretch for the Achilles tendon and calf muscles to relief tight heel cord.<ref>Blitz NM, Stabile RJ, Giorgini RJ, DiDomenico LA. [https://www.podiatric.theclinics.com/article/S0891-8422(09)00097-4/abstract Flexible pediatric and adolescent pes planovalgus: conservative and surgical treatment options]. Clinics in podiatric medicine and surgery. 2010 Jan 1;27(1):59-77.</ref> | |||
*[[Strength and Conditioning|Strengthening Exercises]]: | |||
** Strengthening exercises are given to anterior and posterior tibialis muscles and the flexor hallucis longus, Intrinsic, interosseus plantaris muscles, and the abductor hallucis to prevent valgus and flattening of the anterior arch.<ref name=":10" /> Arch muscle strengthening exercise with [[TheraTogs|theraband.]] | |||
** Global activation of the muscles known to support the medial longitudinal arch and the varus with and without resistance. | |||
** Single leg weight bearing | |||
** Toe walking | |||
* For [[Proprioception]], Toe and heel walking, Single leg weight bearing, and Descending an inclined surface are exercises that could be prescribed. Also, Toe clawing of towel and pebbles, forefoot standing on a stair, toe extension and toe fanning/spreading, and heel walking are all good exercises to maintain viable foot arches. | |||
* Counselling on proper footwear, recommendation on motion control shoes, orthotics and braces are also needed. Foot orthotics such as shoe inserts are used to support the arch for foot pain secondary to pes planus alone or combination with leg, knee, and back pain. | |||
* Obese and overweight individuals should be counseled on weight loss through exercise and dieting; Possibly refer to a dietician for appropriate insight. | |||
* Other co-morbidities amenable to physiotherapy can also be treated following a proper examination and treatment plan<ref name=":3" />.<ref name=":5" /> | |||
*For children with pes planus treatment includes: <ref name="p3" /><ref name="p4" /> | |||
**Advice on appropriate footwear. <ref name="p1" /><ref name="p6" /> | |||
**Advice on appropriate insoles to improve foot position and referral to an podiatrist and an orthotist: in-shoe wedging, foot splints, night stretch splints and cast orthoses. The primary action splint therapy is aimed at stabilising the rear foot and midfoot but not blocking the forefoot. Age-expected foot position, stance and gait are dynamic considerations and need to be well understood. <ref name="p6" /> | |||
**Reducing pain and risk of secondary joint problems. <ref name="p1" /><ref name="p3" /><ref name="p7" />. | |||
**Providing an exercise program to increase strength in the muscles that stabilise the arches. Examples being: walking up on tip-toes; walking on the heels; activities to improve the dynamic arch such as walking barefoot on soft sand, flexing the toes (eg picking up a tissue with the toes), rolling a ball under the arch of the foot when seared; encouraging climbing and other gross motor activities. Try to engage the family in the exercise therapy eg incorporating games and activities that can be part of child’s day<ref name=":7" /> | |||
{{#ev:youtube|y6b4GeYY9sg|400}}<ref>AskDoctorJo. 7 Best Flat Feet Treatments - Ask Doctor Jo. Available from: http://www.youtube.com/watch?v=y6b4GeYY9sg [last accessed 30/6/2020]</ref><div class="row"> | |||
== References == | |||
<references /> | |||
[[Category:Foot]] | |||
[[Category:Foot - Conditions]] | |||
[[Category:Conditions]] | |||
Latest revision as of 09:18, 4 January 2024
Original Editors - Uchechukwu Chukwuemeka
Top Contributors - Yoni Baetens, Derycker Andries, Andeela Hafeez, Lauren Heydenrych, Kim Jackson, Vidya Acharya, Lucinda hampton, Admin, WikiSysop, Rachael Lowe, Oyemi Sillo, Daniele Barilla, 127.0.0.1, Scott Buxton, Kai A. Sigel, Aminat Abolade and Evan Thomas
Introduction[edit | edit source]
Pes planus/ pes planovalgus (or flat foot) is the loss of the medial longitudinal arch of the foot, heel valgus deformity, and medial talar prominence.[1] This is often observed with the medial arch of the foot coming closer (than typically expected) to the ground or making contact with the ground.
All typically developing infants are born with flexible flat feet, with arch development first seen around 3 years of age and then often only attaining adult values in arch height between 7 and 10 years of age.[2][3]
Classification[edit | edit source]
The classification of the pes planus is based on two aspects:
- Arch height: The best parameter to characterize medial longitudinal arch structure was found to be a ratio of navicular height to foot length. It is accepted that the flatness of normal children’s feet and their age are inversely proportioned.[4]
- Heel eversion angle: Heel eversion or hindfoot valgus is generally accepted as a normal finding in young, newly walking children and is expected to reduce with age. The eversion of the heel has been repeatedly used for determining the posture of the child’s foot. Resting calcaneal stance position is a more recent method. It has guided clinicians in assessment of the child’s foot posture and calcaneal eversion has been suggested to reduce by a degree every 12 months to a vertical position by age 7 years. A vertical heel is optimal for foot function. The average rear foot angle for children from 6 to16 years is 4° (raging from 0 to 9° valgus).[5][4]
- Whether the flat foot structure is rigid or flexible
- Flexible flat foot (flexible FF): The longitudinal arches of the foot are present on heel elevation (tiptoe standing) and non-bearing but disappear with full weight bearing on the foot.
- FF is termed developmental FF when observed in infants and toddlers and is part of normal development. Between the ages of 8 and 10 however, a clinician may consider this a true FF.[6]
- Rigid flat foot: The longitudinal arches of the foot are absent in both heel elevation (tiptoe standing) and weight bearing.[7]This is normally associated with underlying pathology.[8]
Epidemiology[edit | edit source]
Roughly 20% to 37% of the population has some degree of pes planus, With most cases being the flexible variety. It is more common in children (about 20-30% of children with some form of flat feet) with most children going on to develop a normal arch by 10 years old. Genetics plays a strong role with it typically running in families.[9][10]
Etiology/Causes[edit | edit source]
The etiology of pes planus has several factors implicated and can be either congenital or acquired.[11]
Congenital Pes Planus[edit | edit source]
Congenital pes planus is classified as developing in the first years of life. Both flexible FF and rigid FF can be present.
At birth and within early childhood pes planus is a typical observation of development and is termed flexible flat foot (FF). It is attributed to osseous and ligamentous laxity, immature neuromuscular control, and the presence of adipose tissue under the medial longitudinal arch (MLA), making the arch appear flat.[12]In fact, during the early years of gait in toddler years, a child will use their entire foot on the ground for balance. A shift of their weight-bearing axis to the 1st or 2nd metatarsal joint induces a flatfoot posture.[13]
When flexible FF is observed in older children (typically those above 8 years of age) and adults, the following must be considered:
- General/ global hypermobility, including conditions such as Ehlers-Danlos syndrome (EDH) and Down Syndrome.
- Conditions with increased tone, e.g. cerebral palsy.[14]
- Higher body mass index (BMI).[4]
- A note: While increased BMI and even obesity have been attributed to increased predisposition to flexible FF, more recent investigations call these findings into question.[3] These studies, which have taken into account a more comprehensive foot morphology (not simply footprint measurements) have not found higher rates of flexible FF in paediatric populations. These have, however, been done with participants with higher BMI and not necessarily a diagnosis of obesity.[15]
- Subtalar joint morphology.
- Recent research has highlighted the variance in subtalar joints. One such study highlighted 2 different types: The first, a firmer supporting joint, and another weaker joint where the anterior articulation in the subtalar joint is absent. The absent articulation allows the FF posture to develop.[6]
- Recent research has highlighted the variance in subtalar joints. One such study highlighted 2 different types: The first, a firmer supporting joint, and another weaker joint where the anterior articulation in the subtalar joint is absent. The absent articulation allows the FF posture to develop.[6]
An example of rigid FF is tarsal coalition, where there is a failure of the tarsal bones to separate. This causes a bony, sometimes cartilaginous, or even fibrous bridge between two or more of the tarsal bones.[16]
Other examples of congenital pes planus include:[11]
- Congenital vertical talus
- Congenital talipes equinovarus
- Tibial torsional deformity
- Presence of the accessory navicular bone.[17]
- General ligament laxity
- Genetic malformations such as Down syndrome and Marfan syndrome[7]
- Familial factors[18]
- Peroneal spasm[5]
- Vertical talus[5]
Acquired Pes Planus[edit | edit source]
Acquired pes planus may arise from:
- Foot and ankle injury such as rupture or dysfunction of the posterior tibial tendon.
- Some medical conditions such as arthritis, spina bifida, cerebral palsy, Arthrogyroposis, and muscular dystrophy.[20]
- Flat feet can also occur as a result of pregnancy.[21][22]
- Iatrogenic factors such as posterior tibialis tendon (PTT) transfer.[20][23]
- Traumatic injury[8]
Clinically Relevant Anatomy[edit | edit source]
The calcaneus, navicular, talus, first three cuneiforms, and the first three metatarsals make up the medial longitudinal arch. This arch is supported by posterior tibial tendon, plantar calcanea navicular ligament, deltoid ligament, plantar aponeurosis, and flexor hallucis longus and brevis muscles. Dysfunction or injury to any of these structures may cause acquired pes planus.
Pathophysiology[edit | edit source]
The pathophysiology of pes planus can vary greatly depending on whether it is congenital or acquired, and then whether it is flexible or fixed.
In considering developmental flatfoot, the medial longitudinal arch of the foot normally develops by the age of 5 or 6. This occurs as the fat pad in babies is gradually absorbed, balance improves and skilled movements are acquired. In some children, however, the arch fails to develop which may be a result of tightness in the calf muscles, laxity in the Achilles tendon or poor core stability in other areas such as around the hips.[26][27]
Dynamic factors[edit | edit source]
Soft tissue factors
- Insufficiency of the posterior tibial tendon: When this occurs, forefoot valgus occurs. Over the long term this produces achilles tendon contractures and transforms the gastrocnemius and soleus muscle complex into heel everters (rather than inverters).[16]
- When a peroneal spastic flatfoot is seen, the peroneal tendon which crosses over the subtalar joint often goes into spasm. This is secondary to subtalar inflammation.[16]
- Other muscular dysfunctions can occur:
- After illness or enforced recumbency, the muscles may temporarily be weak and the arch consequently falls when walking is resumed.
- A more lasting form of muscle weakness accompanies a generally poor posture.
- The child (often a pre-adolescent girl) presents a familiar flabby contour with head stuck forward, mouth open, chest flat, back rounded and abdomen protuberant.
- The gluteal muscles are concerned largely with posture (Wiles 1949). They help to straighten the hip and knee, and to twist the limb outwards. This twist can not be imparted to the foot which is anchored to the ground, and so the rest of the limb turns outwards relative to the foot. As a result, the arch is lifted and the line of weight corrected only when the glutei work properly.
Neurological factors
- In normal development, a baby has to learn to balance first its head, then its trunk, and eventually to balance the whole body on the feet. The difficult art is not required during the early months of life; but sometimes the balancing reflexes fail to develop even after the child has begun to walk. In that event, the arch inevitably collapses with body weight. Myelination of the pyramidal fibers to the foot is incomplete at birth and the plantar responses in babies is extensor. If the infantile flat foot persists into early childhood, the extensor responses may persist too, and it is tempting to assume that balancing cannot be easily learned until myelination is complete.
Static factors[edit | edit source]
- Boney architecture of the medial longitudinal arch. Here altered morphology of the joints of the midfoot would affect stability.[16]
- Fixed or rigid pes planus is due to a structural abnormality. As noted in etiology, this most often presents as a tarsal coalition. Limited range is seen in the subtalar and midfoot motion when there is a failure of tarsal bones to separate. This coalition can be cartilaginous, fibrous or even boney. This condition often causes pain and inflammation of the joints.[16]Other conditions associated with rigid pes planus include accessory navicular bone, congenital vertical talus or other congenital hindfoot pathology.[11]
- The spring ligament complex has been noted as an important stabiliser, but clarity still lacks in the literature. Plantar fascia offers stability to the medial longitudinal arch via the windlass effect. In conditions where the laxity of these tissues is affected, for example in EDH, arch stability can be compromised.[16]In a study performed in 1993 on cadavers, the most important structure found for supporting the foot arch was the plantar fascia, followed by the talonavicular and spring ligaments.[13]
- The bony arch of the foot is potentially unstable and is bound together by ligaments. They withstand short-term stresses. Their primary function is to act as sensory end organs, so when stretched, appropriate muscles are reflexively brought into action. Even the most anatomically perfect foot will become rapidly and grossly flat unless it has muscles of good bulk and tone to support it. The physiological fault may lie in the muscle itself or its nervous control.
Characteristics/Clinical Presentation[edit | edit source]
- History
- In adults: Frequent "rolling of the ankle"/ ankle sprains
- Children presenting with pes planus are generally asymptomatic, usually only becoming symptomatic during adolescence.[16]
- Pain is often felt by indicated at the medial longitudinal arch and ankle. In children and adolescents pain secondary to flatfeet may be described as pain in the arch of the feet or cramps at night.[14] In adults there may be complaints of pain due to strained muscles and connecting tissues in the midfoot, heel, lower leg, knee, hip, and or back. In more advanced changes client may complain of an altered gait pattern.[10]
- Observation:
- The foot may present as flat or 'rocker-bottom'.[16]
- In standing - Calcaneal valgus is apparent, the medial arch will appear dropped and there will be foot eversion.[16]
- Gait[16]
- Test stance on medial and lateral borders of feet to assess mobility of foot joints.
- Walking on heels. Being able to walk on heels demonstrates flexibility of the achilles tendon.
- Viewed from posteriorly, looking for the "too many toes sign"[10]
- Look at running or walking shoes [16]Uneven distribution of body weight with resultant one-sided wear of shoes leading to further injuries.[20]
- With palpation:[16]
- A contracted achilles tendon may show as a limitation in dorsiflexion.
- Test subtalar and transverse tarsal motion. Flexible pes planus will allow for mobility in these joints.
- Subtalar motion: Examiner stablises ankle with one hand, calcanues in the other. The calcaneus is then inverted and everted. Normal ROM is between 20° and 60°, Inversion being 2x the ROM of eversion.
- Tarsal motion: Grasp the calcaneus in one hand and forefoot in the other. The normal adduction of forefoot is about 30°, abduction about 15°. If ranges are less consider coalition.
Ask the client about the onset of deformity, timing of symptoms, severity of past and current symptoms, history of trauma, family history, surgical history, and past medical history (including hypertension, diabetes, rheumatoid arthritis, sensory neuropathies, seronegative spondyloarthropathies, and obesity[10]).
Associated Co-morbidities[edit | edit source]
Co-morbidities include but not limited to neurological conditions such as cerebral palsy; genetics e.g. Down syndrome, Marfan syndrome or Ehlers-Danlos Syndrome; charcot joint; tibialis posterior dysfunction; Obesity; arthropathies;[28] Shprintzen-Goldberg syndrome.[29]
Diagnostic Procedure[edit | edit source]
- Footprints: It is still controversial if footprints reflect the real morphology of the medial longitudinal arch. Recent development found an initial correlation between dynamic pressure patterns and static foot-prints.[5]
- X-rays are used to categorise the feet as having normal, slightly flat and moderate arches. In FF this is not routine.[16]
- Foot-posture index (FPI-6)[27]
- Supination resistance test [27][5]: This test is used to estimate the magnitude of pronatory moments. The foot is manually supinated. The higher the force required, the greater the supination resistance and the stronger the pronatory forces. This test is subjective.
- Jack’s test and Feiss angle (are related) [27]: Performing the Jack’s test. The hallux is manually dorsiflexed while the child is standing. If the medial longitudinal arch rises due to dorsiflexion of the hallux, the foot is considered a flexible flat foot. If the medial longitudinal arch remains unchanged, the test designates a rigid flat foot. The purpose of this test is to check the foot flexibility and the onset of the windlass mechanism by tensioning the plantar fascia trough the extension of the first metatarsophalangeal joint. The Feiss line is the line interconnecting malleolus medialis, navicular and first metatarsal head. The inclination of this line with the ground increases when the first metatarsophalangeal joint is dorsiflexed (Jack’s test). This dorsiflexion activates forefoot supination and raises the arch height (140°± 6°).[27]
- Tip-toe[16]To differentiate fixed and flexible pes planus.
- Ankle range [27][5]: Children’s ankle range assessment is generally an unreliable measure, as typically assessed when the child is non-weight-bearing. So it is suggested that therapists look at a child’s ability to squat, heel walk and increase stride length.[27]
Medical Management[edit | edit source]
Flexible Pes planus[edit | edit source]
The merit of treatment for all flexible FF remains ambiguous, with evidence showing that foot orthoses produces improvements in children with pes planus. It remains difficult to conclude if spontaneous physiological arch improvement occurred or the effect of intervention caused the arch improvement.
- There is little evidence for treatment of asymptomatic, flexible, pediatric flat feet in a child who have no underlying medical issues.[16]
- Treatment of symptomatic, flexible flat feet is generally accepted for children with contributory background factors or secondary complications, or if pes planus persists past childhood.[14]
- Evidence supports the use of non surgical interventions for painful pes planus.
- The child should be fitted with a flat, lace-up shoe with a firm heel and MLA support, a broad and deep toe box and the ‘toe break’ at the junction between the anterior third and posterior two-thirds of the shoe.[30]In children 10 years and older, FF is considered permanent, therefore long term othotics can be used to prevent secondary problems, especially in overweight or athletically active children.[16]
Treatment is based on etiology and NSAIDS are sufficient for pain.
Rigid Pes planus[edit | edit source]
Surgery is required in rigid pes planus and in cases resistant to therapy to reduce symptoms.[31] Most surgical methods aim at realigning foot shape and mechanics. These surgeries could be tendon transfers, realignment osteotomies, arthrodesis and where other surgeries fail, triple arthrodesis is performed[32]
For the congenital pes valgus treatment, researchers have defined the best possible treatments depending on the age of the person/child.
- In a child younger than 2 years, an extensive release with lengthening of the Achilles tendon and fixation procedure is recommended. It is less invasive than other techniques, because there is no tendon transfer or bony procedures needed. The explanation could be because of the greater adaptability of the cartilaginous structures.
- In a child with neural tube defect, younger than 2 years of age, an extensive release with tendon transfer procedure is recommended. A neuromuscular imbalance between a weak Tibialis Posterior tendon and a strong evertor of the foot could be responsible for this condition. Good results are found for this operation which aims to correct this imbalance.
- In a child older than 2 years of age, an extensive release with tendon transfer procedure is proposed. Surgical correction becomes increasingly difficult in older children because of secondary changes in the bone. This procedure resulted as the best for children whose walking and standing potential has been established.
In case of failure of precedent procedures, a bony procedure may be considered. There are good results for children of 4 years and older with these procedures. Every surgery is usually followed by a plaster cast for two to three months. The recovery after surgery takes about 6 months to 1 year to heal completely and to recover completely on a functional level.[4][14][15]
Physical Therapy Management[edit | edit source]
The aim of physical therapy is to minimize pain, increase foot flexibility, strengthen weak muscles, train proprioception, and patient education and reassurance. As part of the assessment process, the physiotherapist can assist in evaluating the gait, gross motor skills and the impact the foot deformity has on functional activities. Assess endurance, speed, fatigability, pain and ability to walk on different terrains, with a focus on assessing function, not just structural abnormalities.
Pain management includes rest, activity modification, cryotherapy, massage, and nonsteroidal anti-inflammatory medication. Ultrasound and pulsed electrical stimulation can also be used for pain relief. Electric stimulation will aid blood circulation, promoting healing processes and diminishing discomfort and oedema.
- Encouraging walking bear foot
- Flexibility exercises are passive ROM exercises of the ankle and all foot joints; Stretching of gastrocnemius soleus complex and peroneus brevis muscles to facilitate varus and foot adduction; Heel-cord stretch for the Achilles tendon and calf muscles to relief tight heel cord.[33]
- Strengthening Exercises:
- Strengthening exercises are given to anterior and posterior tibialis muscles and the flexor hallucis longus, Intrinsic, interosseus plantaris muscles, and the abductor hallucis to prevent valgus and flattening of the anterior arch.[16] Arch muscle strengthening exercise with theraband.
- Global activation of the muscles known to support the medial longitudinal arch and the varus with and without resistance.
- Single leg weight bearing
- Toe walking
- For Proprioception, Toe and heel walking, Single leg weight bearing, and Descending an inclined surface are exercises that could be prescribed. Also, Toe clawing of towel and pebbles, forefoot standing on a stair, toe extension and toe fanning/spreading, and heel walking are all good exercises to maintain viable foot arches.
- Counselling on proper footwear, recommendation on motion control shoes, orthotics and braces are also needed. Foot orthotics such as shoe inserts are used to support the arch for foot pain secondary to pes planus alone or combination with leg, knee, and back pain.
- Obese and overweight individuals should be counseled on weight loss through exercise and dieting; Possibly refer to a dietician for appropriate insight.
- Other co-morbidities amenable to physiotherapy can also be treated following a proper examination and treatment plan[11].[32]
- For children with pes planus treatment includes: [26][15]
- Advice on appropriate footwear. [4][27]
- Advice on appropriate insoles to improve foot position and referral to an podiatrist and an orthotist: in-shoe wedging, foot splints, night stretch splints and cast orthoses. The primary action splint therapy is aimed at stabilising the rear foot and midfoot but not blocking the forefoot. Age-expected foot position, stance and gait are dynamic considerations and need to be well understood. [27]
- Reducing pain and risk of secondary joint problems. [4][26][5].
- Providing an exercise program to increase strength in the muscles that stabilise the arches. Examples being: walking up on tip-toes; walking on the heels; activities to improve the dynamic arch such as walking barefoot on soft sand, flexing the toes (eg picking up a tissue with the toes), rolling a ball under the arch of the foot when seared; encouraging climbing and other gross motor activities. Try to engage the family in the exercise therapy eg incorporating games and activities that can be part of child’s day[30]
References[edit | edit source]
- ↑ Troiano G, Nante N, Citarelli GL. Pes planus and pes cavus in Southern. Annali dell'Istituto superiore di sanita. 2017 Jun 7;53(2):142-5.
- ↑ Squibb M, Sheerin K, Francis P. Measurement of the Developing Foot in Shod and Barefoot Paediatric Populations: A Narrative Review. Children. 2022 May 19;9(5):750.
- ↑ 3.0 3.1 Evans AM, Karimi L. The relationship between paediatric foot posture and body mass index: do heavier children really have flatter feet?. Journal of foot and ankle research. 2015 Dec;8(1):1-7.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Chen KC, Yeh CJ, Tung LC, Yang JF, Yang SF, Wang CH. Relevant factors influencing flatfoot in preschool-aged children. European journal of pediatrics. 2011 Jul;170(7):931-6.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Cass AD, Camasta CA. A review of tarsal coalition and pes planovalgus: clinical examination, diagnostic imaging, and surgical planning. The Journal of foot and ankle surgery. 2010 May 1;49(3):274-93.
- ↑ 6.0 6.1 Kothari A, Bhuva S, Stebbins J, Zavatsky AB, Theologis T. An investigation into the aetiology of flexible flat feet: the role of subtalar joint morphology.A The Bone & Joint Journal. 2016 Apr;98(4):564-8.
- ↑ 7.0 7.1 Wilson DJ. Flexible vs Rigid Flat Foot, 2019. Available from: https://www.news-medical.net/health/Flexible-vs-Rigid-Flat-Foot.aspx (Accessed 29 June 2020)
- ↑ 8.0 8.1 Halabchi F, Mazaheri R, Mirshahi M, Abbasian L. Pediatric flexible flatfoot; clinical aspects and algorithmic approach. Iranian journal of pediatrics. 2013 Jun;23(3):247.
- ↑ Suciati T, Adnindya MR, Septadina IS, Pratiwi PP. Correlation between flat feet and body mass index in primary school students. InJournal of Physics: Conference Series 2019 Jul 1 (Vol. 1246, No. 1, p. 012063). IOP Publishing.
- ↑ 10.0 10.1 10.2 10.3 Raj MA, Tafti D, Kiel J Pes Planus Available: https://www.ncbi.nlm.nih.gov/books/NBK430802/ (accessed 2.7.2022)
- ↑ 11.0 11.1 11.2 11.3 Raj MA, Tafti D, Kiel J. Pes Planus (Flat Feet). StatPearl-NCBI Bookshelf, 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430802/ (Accessed 29 June 2020)
- ↑ Banwell HA, Paris ME, Mackintosh S, Williams CM. Paediatric flexible flat foot: how are we measuring it and are we getting it right? A systematic review. Journal of foot and ankle research. 2018 Dec;11(1):1-3.
- ↑ 13.0 13.1 Atik A, Ozyurek S. Flexible flatfoot. Northern clinics of Istanbul. 2014;1(1):57.
- ↑ 14.0 14.1 14.2 14.3 Turriago CA, Arbeláez MF, Becerra LC. Talonavicular joint arthrodesis for the treatment of pes planus valgus in older children and adolescents with cerebral palsy. Journal of children's orthopaedics. 2009 Jun;3(3):179-83.
- ↑ 15.0 15.1 15.2 Evans AM. The paediatric flat foot and general anthropometry in 140 Australian school children aged 7-10 years. Journal of foot and ankle research. 2011 Dec;4(1):1-8.
- ↑ 16.00 16.01 16.02 16.03 16.04 16.05 16.06 16.07 16.08 16.09 16.10 16.11 16.12 16.13 16.14 16.15 16.16 SM Javad M, Ramin E, Taghi B. Flatfoot in children: how to approach? Iran Journal of Paediatrics.2007. 17(No.2): 163-170.
- ↑ Cheong IY, Kang HJ, Ko H, Sung J, Song YM, Hwang JH. Genetic influence on accessory navicular bone in the foot: a Korean twin and family study. Twin Research and Human Genetics. 2017 Jun;20(3):236-41.
- ↑ Mosca VS. Flexible flatfoot in children and adolescents. J Child Orthop. 2010;4(2):107–121
- ↑ Cleveland Clinic. 2019. Available from:https://my.clevelandclinic.org/health/diseases/15961-adult-acquired-flatfoot#:~:text=In%20people%20with%20diabetes%2C%20a,notice%20as%20their%20foot%20collapses. (Accessed 29 June 2020)
- ↑ 20.0 20.1 20.2 Berlet GC. Pes Planus (Flatfoot). Medscape, 2019. Available from: https://emedicine.medscape.com/article/1236652-overview#a8 (accessed 29 June 2020)
- ↑ Indy Podiatry. Common foot and ankle problems during pregnancy, 2019. Available from: https://indypodiatry.com/your-feet-during-pregnancy/#:~:text=Over%2Dpronation%2C%20or%20flat%20feet,feet)%20leading%20to%20significant%20pain. (accessed 29 June 2020)
- ↑ Conder R, Zamani R, Akrami M. The biomechanics of pregnancy: A systematic review. Journal of Functional Morphology and Kinesiology. 2019 Dec 2;4(4):72.
- ↑ Pecheva M, Devany A, Nourallah B, Cutts S, Pasapula C. Long-term follow-up of patients undergoing tibialis posterior transfer: is acquired pes planus a complication?. The Foot. 2018 Mar 1;34:83-9.
- ↑ Mount Sinai Health Systems. What causes flat foot? Available from: http://www.youtube.com/watch?v=GPS10HfgYDY [last accessed 29/6/2020]
- ↑ East Coast Podiatry. Flat Feet (Pes Planus) - Georgina Tay, Singapore Podiatrist . Available from: http://www.youtube.com/watch?v=9tlzxA8o0w0 [last accessed 29/6/2020]
- ↑ 26.0 26.1 26.2 Oeffinger DJ, Pectol Jr RW, Tylkowski CM. Foot pressure and radiographic outcome measures of lateral column lengthening for pes planovalgus deformity. Gait & posture. 2000 Dec 1;12(3):189-95.
- ↑ 27.0 27.1 27.2 27.3 27.4 27.5 27.6 27.7 27.8 Evans AM. Pocket Podiatry: Paediatrics E-Book. Elsevier Health Sciences; 2010 Jan 26.
- ↑ Lowth M. Pes Planus (Flat feet). Patient, 2016. Available from: https://patient.info/doctor/pes-planus-flat-feet (Accessed 30 June 2020)
- ↑ Yadav S, Rawal G. Shprintzen-Goldberg syndrome: A rare disorder. Pan African Medical Journal. 2016; 23:227 doi:10.11604/pamj.2016.23.227.7482
- ↑ 30.0 30.1 Turner C, Gardiner MD, Midgley A, Stefanis A. A guide to the management of paediatric pes planus. Australian journal of general practice. 2020 May;49(5):245-9.
- ↑ Henry JK, Shakked R, Ellis SJ. Adult-acquired flatfoot deformity. Foot & ankle orthopaedics. 2019 Jan 14;4(1):2473011418820847.
- ↑ 32.0 32.1 Carr JB, Yang S, Lather LA. Pediatric pes planus: a state-of-the-art review. Pediatrics. 2016 Mar 1;137(3).
- ↑ Blitz NM, Stabile RJ, Giorgini RJ, DiDomenico LA. Flexible pediatric and adolescent pes planovalgus: conservative and surgical treatment options. Clinics in podiatric medicine and surgery. 2010 Jan 1;27(1):59-77.
- ↑ AskDoctorJo. 7 Best Flat Feet Treatments - Ask Doctor Jo. Available from: http://www.youtube.com/watch?v=y6b4GeYY9sg [last accessed 30/6/2020]