Patellar Tendinopathy
Original Editors - Dorien De Ganck
Top Contributors - George Prudden, Admin, Mathieu Henrotte, Dorien De Ganck, Kim Jackson, Derycker Andries, Chelsy De Bruyn, Vanessa Rhule, Rachael Lowe, Wendy Walker, Evan Thomas, Jess Bell, Yarne Leuckx, Alexandre Effinger, Wanda van Niekerk, Tarina van der Stockt, WikiSysop, Simisola Ajeyalemi, Joris De Pot, Fee Waveryns, Claire Knott, Scott Buxton, Oyemi Sillo, Wendy Snyders, Naomi O'Reilly, Robin Tacchetti, Wajeeha Hassan, Mariam Hashem and 127.0.0.1
Topic Expert - Claire Robertson
Description[edit | edit source]
Patellar tendinopathy is a source of anterior knee pain, characterised by pain localised to the inferior pole of the patella. Pain is aggravated by loading and increased with the demand on the knee extensor musculature, notably in activities that store and release energy in the patellar tendon[1].
Patellar tendinopathy is primarily a condition of relatively young (15-30 years old) athletes, especially men, who participate in sports such as basketball, volleyball, athletic jump events, tennis, and football, which require repetitive loading of the patellar tendon[2].
Clinically Relevant Anatomy[edit | edit source]
|
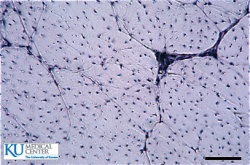
Cross section of a tendon. Collagen fibers |
The quadriceps muscles are connected to the inferior pole of the patella by the common quadriceps tendon through a sesmoid bone, the patella. The patellar ligament then connects the bottom of the patella to the tibial tuberosity. The force generated from the quadriceps muscles acts through the patellar as a pulley, causing the knee to extend[4]
A healthy tendon is composed mostly of parallel collagen fibers closely packed together (86%)[5]. Collagen is predominantly type I. Other components of the tendon matrix are elastin (2%), proteoglycans (1–5%), and inorganic components (0.2%). The collagen in tendons are held together with proteoglycan components Decorin and Aggrecan, which bind to the collagen fibrils at specific locations[6]
Tenocytes are a tendon specific fibroblast type cells that produce the collagen molecules, which cluster together to fom collagen fibrils. Fibril bundles are organized to form fibres with the elongated tenocytes closely packed between them. The cells communicate with each other through gap junctions, and this signalling gives them the ability to detect and respond to mechanical load[7].
Blood vessels run parallel to collagen fibres within the tendon with some branching transverse anastomoses. There is thought to be no nerve supply to the internal tendon but adjacent to the tendon are nerve endings and Golgi tendon organs are present at the junction between tendon and muscle.
Pathological Process
[edit | edit source]
Cook & Purdam decribed a continuum model of tendon pathology with three disinct stages[8]:
- Reactive tendinopathy
- Tendon disrepair
- Degenerative tendinopathy
Load is considered to be the primary stimulus which drives tendon health forward and back along the continuum.
Reactive tendinopathy
[edit | edit source]
A non-inflammatory proliferative response in the cell and matrix, occurs with acute tensile or compressive overload.This causes a short-term adaptation to the tendon in that it thickens which has the net results of reducing stress by increasing cross-sectional area or allow adaptation to compression. This is different from the normal tendon response to load, which generally occurs through tendon stiffening. Clinically, reactive tendinopathies occur with unaccustomed physical activity. Less commonly after a direct blow such as falling directly onto the patellar tendon.
Tendon disrepair
[edit | edit source]
The continued attempt of tendon healing following the reactive stage but with greater matrix breakdown. There is an increase in number of cells present in the matrix, which results in an increase in protein production (proteoglycan and collagen). The increase in proteoglycans results in separation and disorganisation of collagen. There may be an increase in vascularity and neuronal growth. Clinically, this stage of the pathology is seen in chronically overloaded tendons and appears across a spectrum of ages and loading environments.
Degenerative tendinopathy
[edit | edit source]
There are areas of cell death due to apoptosis, trauma or tenocyte exhaustion. There are large areas of the matrix that are disordered and filled with vessels, matrix breakdown products and little collagen. There is little capacity for reversibility of pathological changes at this stage.This stage is primarily seen in the older person.
Clinical Presentation[edit | edit source]
Patellar tendinopathy, is one of many potential diagnoses for a patient presenting with anterior knee pain. There is considered to be two defining clinical features[1]:
- Pain localized to the inferior pole of the patella
- Load-related pain that increases with the demand on the knee extensors, notably in activities that store and release energy in the patellar tendon.
The patient may complain of pain with prolonged sitting, squatting, and stairs, but these complaints are features of other pathologies such as patellofemoral pain. Pain is rarely experienced in a resting state. Pain occurs instantly with loading and usually ceases almost immediately when the load is removed. The pain may improve with repeated loading. An important feature of tendinopathies is that they are dose-dependent, pain increases as the magnitude or rate of application of the load on the tendon increases[9].The practical application of this is in an examination pain should increase when progressing from a shallow to a deeper squat, or from a smaller to a greater hop height.
Aggravating activities are predominantly loading activities, such as walking down stairs or when performing a decline squat.
Diagnostic Procedures
[edit | edit source]
Dose-dependent pain, see previous section. Deficits in energy-storage activities can be assessed clinically by observing jumping and hopping. Stiff-knee vertical jump-landing strategy may be used by individuals with a past history of patellar tendinopathy[10].
Examination of the complete lower extremity is necessary to identify relevant deficits at the hip, knee, and ankle/foot regions. Atrophy, reduced strength, malaligned foot posture, quadriceps and hamstring inflexibility, reduced ankle dorsiflexion have been associated with patellar tendinopathy and should also be assessed[1].
Patellar tendon imaging does not confirm patellar tendon pain, as pathology observed via ultrasound imaging may be present in asymptomatic individuals[11].
Outcome Measures[edit | edit source]
- Pain provocation (Visual Analogue Scale or Victorian Institute of Sport Assessment-patella[12])
- Tendon swelling
- Return to activity
Medical Management
[edit | edit source]
Non-steroidal anti-inflammatory drugs
[edit | edit source]
The use of non-steroidal anti-inflammatory drugs (NSAID’s) in the treatment of tendinopathy remains controversial both in the acute stage and in the chronic stage. NSAIDs have been reported to impede soft tissue healing. Although pain may be reduced, they have a negative effect on tendon repair[13]. In reactive tendinopathy, this may be a preferred effect, as this may inhibit proteins responsible for tendon swelling[14].
Corticosteroid injections
[edit | edit source]
Corticosteroids are used to decrease pain but also decrease cell proliferation and protein production and therefore could be used in the reactive tendinopathies. Repeated peritendinous corticosteroid has been shown to reduce tendon diameter at 7 and 21 days after injection in tendons[15].
Surgical treatment
[edit | edit source]
Surgery for chronic painful tendons has produced varied outcomes, with 50–80% of athletes able to return to sport at their previous level[16]. Surgery in nonathletic people produced poorer results than in active people[17]. Surgery is considered a reasonable option in those who have failed all conservative interventions.
Physiotherapy Management
[edit | edit source]
| Leg extension is a useful exercise as it can be progressed by quantifiable increments. |
Advice regarding selective rest should be provided to allow appropriate tendon healing following a period of acute overloading or unaccustomed exercise [18] . There should be a focus on an early return to activities.
Pain relief[edit | edit source]
Isometrics have been suggested as a possible analgesic exercise where isotonic exercises are not possible due to fatigue and high SIN. In a systematic review by Naugle et al.[19] isometric exercise has been found to be superior to aerobic and resistance exercises at reducing pain.
Rehabilitation[edit | edit source]
A variety of loading programs have been suggested for the treatment of patella tendinopathy with the main types being[20]:
- Eccentric loading
- Eccentric-concentric loading
| Program |
Exercise type |
Sets & reps |
Frequency |
Progression |
Pain |
|---|---|---|---|---|---|
| Alfredson |
Eccentric |
3x15 |
Twice daily |
Load |
Enough load to achieve up to moderate pain |
| Stanish and Curwin/Silbernagel |
Eccentric-concentric |
3x10-20 |
Daily |
Speed then load, type of exercise |
Enough load to be painful in third set |
| Heavy slow resistance training |
Eccentric-concentric |
4x6-15 |
3x/week |
6-15RM |
Acceptable if was not worse after |
Eccentric loading has been the most dominant approach for rehabilitation. Evidence suggests that all loading programs are beneficial in reducing pain and returning function however the eccentric-concentric type has greater patient subjective satisfaction[20]. This is perhaps due to time commitment and pain required from eccentric programs. Eccentric-concentric exercises can begin with body weight squats but a significant load is important. Gym machines such as leg press or knee extension provides control to the amount of loading. If suitable for the patient a barbell squat or lunge can be an excellent progression.
Protocol[edit | edit source]
| Protocol as suggested by Malliaris et al. (2015)[1] | ||
| Stage |
Indication to initiate |
Dosage |
| 1. Isometric loading |
More than minimal pain during isometric exercise |
5 repetitions of 45 seconds, 2 to 3 times per day; progress to 70% maximal voluntary contraction as pain allows |
| 2. Isotonic loading |
Minimal pain during isotonic exercise |
3 to 4 sets at a load of 15RM, progressing to a load of 6RM, every second day; fatiguing load |
| 3. Energy-storing loading |
(A) Adequate strength and consistent with other side (B) Load tolerance with initial-level energy storage exercise (ie, minimal pain during exercise and pain on load tests returning to baseline within 24 h) |
Progressively develop volume and then intensity of relevant energy-storage exercise to replicate demands of sport |
| 4. Return to sport |
Load tolerance to energy-storage exercise progression that replicates demands of training |
Progressively add training drills, then competition, when tolerant to full training |
Malliaris and colleagues report common management pitfalls, which are worth considering when planning treatment:
- Unrealistic rehabilitation time frames
- Inaccurate beliefs and expectations about pain
- Failure to identify central sensitization
- Over-reliance on passive treatments
- Not addressing isolated muscle deficits
- Failure to address kinetic-chain deficits
- Not adequately addressing biomechanics
Differential Diagnosis[edit | edit source]
- Infrapatellar bursitis
- Fat pad impingement
- Patellofemoral pain
- Plica injuries
- Osgood-Schlatter syndrome
- Sinding-Larsen-Johansson syndrome
Key Evidence[edit | edit source]
- Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. (Rio 2015)
- Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. (Malliaris 2015)
- Physiotherapy management of patellar tendinopathy (jumper's knee). (Rudavsky 2014)
- Achilles and patellar tendinopathy loading programmes. (Malliaris 2013)
Resources[edit | edit source]
Case Studies[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=10AkQ1Iw49RKj2Dls_4vN-p0FB75-E6HcklAbWTJWvSBefDQfb|charset=UTF-8|short|max=10: Error parsing XML for RSS
References
[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Malliaras P, Cook J, Purdam C, Rio E. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. The Journal of orthopaedic and sports physical therapy. 2015 Sep:1-33.
- ↑ Lian ØB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports a cross-sectional study. The American journal of sports medicine. 2005 Apr 1;33(4):561-7.
- ↑ http://www.kumc.edu/instruction/medicine/anatomy/histoweb/
- ↑ Palastanga N, Field D, Soames R. Anatomy and human movement: structure and function. Elsevier Health Sciences; 2012.
- ↑ Lin TW, Cardenas L, Soslowsky LJ. Biomechanics of tendon injury and repair. Journal of biomechanics. 2004 Jun 30;37(6):865-77.
- ↑ Zhang G, Ezura Y, Chervoneva I, Robinson PS, Beason DP, Carine ET, Soslowsky LJ, Iozzo RV, Birk DE. Decorin regulates assembly of collagen fibrils and acquisition of biomechanical properties during tendon development. Journal of cellular biochemistry. 2006 Aug 15;98(6):1436-49.
- ↑ McNeilly CM, Banes AJ, Benjamin M, Ralphs JR. Tendon cells in vivo form a three dimensional network of cell processes linked by gap junctions. Journal of anatomy. 1996 Dec;189(Pt 3):593
- ↑ Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. British journal of sports medicine. 2009 Jun 1;43(6):409-16.
- ↑ Kountouris A, Cook J. Rehabilitation of Achilles and patellar tendinopathies. Best practice & research clinical rheumatology. 2007 Apr 30;21(2):295-316.
- ↑ Bisseling RW, Hof AL, Bredeweg SW, Zwerver J, Mulder T. Relationship between landing strategy and patellar tendinopathy in volleyball. British journal of sports medicine. 2007 Jul 1;41(7):e8-.
- ↑ Malliaras P, Cook J, Ptasznik R, Thomas S. Prospective study of change in patellar tendon abnormality on imaging and pain over a volleyball season. British journal of sports medicine. 2006 Mar 1;40(3):272-4.
- ↑ Visentini PJ, Khan KM, Cook JL, Kiss ZS, Harcourt PR, Wark JD, Victorian Institute of Sport Tendon Study Group. The VISA score: an index of severity of symptoms in patients with jumper's knee (patellar tendinosis). Journal of Science and Medicine in Sport. 1998 Jan 31;1(1):22-8.
- ↑ Ferry ST, Dahners LE, Afshari HM, Weinhold PS. The effects of common anti-inflammatory drugs on the healing rat patellar tendon. The American journal of sports medicine. 2007 Aug 1;35(8):1326-33.
- ↑ Riley GP, Cox M, Harrall RL, Clements S, Hazleman BL. Inhibition of tendon cell proliferation and matrix glycosaminoglycan synthesis by non-steroidal anti-inflammatory drugs in vitro. Journal of Hand Surgery (British and European Volume). 2001 Jun 1;26(3):224-8.
- ↑ Fredberg U, Bolvig L, Pfeiffer‐Jensen M, Clemmensen D, Jakobsen BW, Stengaard‐Pedersen K. Ultrasonography as a tool for diagnosis, guidance of local steroid injection and, together with pressure algometry, monitoring of the treatment of athletes with chronic jumper's knee and Achilles tendinitis: a randomized, double‐blind, placebo‐controlled study. Scandinavian journal of rheumatology. 2004 Mar 1;33(2):94-101.
- ↑ Tallon C, Coleman BD, Khan KM, Maffulli N. Outcome of surgery for chronic Achilles tendinopathy a critical review. The American Journal of Sports Medicine. 2001 May 1;29(3):315-20.
- ↑ Maffulli N, Testa V, Capasso G, Oliva F, Sullo A, Benazzo F, Regine R, King JB. Surgery for chronic Achilles tendinopathy yields worse results in nonathletic patients. Clinical Journal of Sport Medicine. 2006 Mar 1;16(2):123-8.
- ↑ Simpson M, Smith T. Quadriceps tendinopathy-a forgotten pathology for physiotherapists? A systematic review of the current evidence-base. Phys Ther Rev. 2011;16(6):455-61.
- ↑ Naugle KM, Fillingim RB, Riley JL. A meta-analytic review of the hypoalgesic effects of exercise. The Journal of pain. 2012;13(12):1139-50.
- ↑ 20.0 20.1 Malliaras P, Barton CJ, Reeves ND, Langberg H. Achilles and patellar tendinopathy loading programmes. Sports Med. 2013;43(4):267-86.