Neck Pain: Clinical Practice Guidelines: Difference between revisions
(Formatting) |
Kim Jackson (talk | contribs) m (Text replacement - "</big>" to "") |
||
| (15 intermediate revisions by 2 users not shown) | |||
| Line 2: | Line 2: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''- [[User:Chad Adams|Chad Adams]], [[User:Jacob Melnick|Jacob Melnick]], & [[User:Tyler Shultz|Tyler Shultz]]<br> | '''Original Editors '''- [[User:Chad Adams|Chad Adams]], [[User:Jacob Melnick|Jacob Melnick]], & [[User:Tyler Shultz|Tyler Shultz]] as part of the[[Nottingham University Spinal Rehabilitation Project]]<br> | ||
'''Lead Editors''' {{Special:Contributors/{{FULLPAGENAME}}}}<br> | '''Lead Editors''' {{Special:Contributors/{{FULLPAGENAME}}}}<br> | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
[[File:Neck Pain Diagram.png|alt=|thumb| | [[File:Neck Pain Diagram.png|alt=|thumb|Pain in the neck.]] | ||
Neck Pain (NP) lacks a uniform operational definition. <ref>Moffett J., McLean S. [https://doi.org/10.1093/rheumatology/kei242 The role of physiotherapy in the management of non-specific back pain and neck pain]. Rheumatology. 2006 Apr 1;45(4):371-8.</ref> Nevertheless, the most commonly reported type is non-specific or [https://www.physio-pedia.com/Mechanical_Neck_Pain mechanical] NP | Neck Pain (NP) lacks a uniform operational definition. <ref>Moffett J., McLean S. [https://doi.org/10.1093/rheumatology/kei242 The role of physiotherapy in the management of non-specific back pain and neck pain]. Rheumatology. 2006 Apr 1;45(4):371-8.</ref> Nevertheless, the most commonly reported type is non-specific or [https://www.physio-pedia.com/Mechanical_Neck_Pain mechanical] NP characterised by symptoms of a non-specific nature or mechanical basis. <ref name=":1">Binder AI. [https://doi.org/10.1136/bmj.39127.608299.80 Cervical spondylosis and neck pain.] BMJ. 2007 Mar 8;334(7592):527-31.</ref> Common presentations of NP may include muscle pain, muscle spasm, headache, facet joint pain, nerve pain, referred pain and bone pain. <ref>Harvard Medical School The 7 Faces of Neck Pain. Havard Health Publishing. Available from:https://www.health.harvard.edu/pain/7-faces-of-neck-pain [accessed 4/3/2023]</ref> | ||
NP is becoming increasingly common throughout the world <ref name=":2">Hoy D., Protani M., De R., Buchbinder R. [https://pubmed.ncbi.nlm.nih.gov/21665126/ The epidemiology of neck pain]. Best Pract Res Clin Rheumatol. 2010 Dec;24(6):783-92.</ref> with around two thirds of people experiencing NP at one moment in their life. The prevalence of NP varies largely between studies; mean reported estimates are 7.6% for point prevalence and 48.5% for lifetime prevalence. <ref name=":1" /> Most studies indicate a higher incidence of NP among women, <ref name=":2" /> anxiety or [[depression]] sufferers <ref>Elbinoune I., Amine B., Shyen S., Gueddari S., Abouqal R., Hajjaj-Hassouni N. [https://www.ajol.info/index.php/pamj/article/view/143632 Chronic neck pain and anxiety-depression: prevalence and associated risk factors.] Pan African Medical Journal. 2016 Sep 9;24(1).</ref> and office workers with poor ergonomic positions. <ref>Hush J., Michaleff Z., Maher C., Refshauge K. [https://link.springer.com/article/10.1007/s00586-009-1011-z Individual, physical and psychological risk factors for neck pain in Australian office workers: a 1-year longitudinal study.] Eur Spine J. 2009 Oct;18(10):1532-40.</ref> | |||
== | === Anatomy === | ||
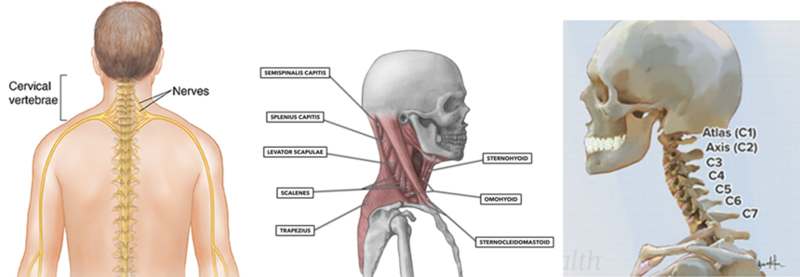
'''Bones and Joints'''- The neck consists of 7 bones C1-C7. The most common NP caused by problems to the bone is [[osteoarthritis]] with wear in cartilage between the joints causing the bones to rub together producing pain and stiffness. <ref>Abu-Naser S., Almurshidi S. A knowledge based system for neck pain diagnosis. 2016. Department of Information Technology. Available from: http://dstore.alazhar.edu.ps/xmlui/handle/123456789/384. [accessed 4/3/2023]</ref> These bones are linked together by facet joints which are small joints between vertebrae. | |||
= | |||
'''Bones and Joints'''- The neck consists of 7 bones C1-C7. The most common | |||
'''Muscles, Tendons and Ligaments'''- Large muscles of the neck such as the [[sternocleidomastoid]] and the [[trapezius]] enable gross motor movements in the neck. The most common pain produced by these structures is a neck strain which affects the cervical muscles and tendons or a sprain which affects the ligaments, both involving overstretching or tearing these structures. | '''Muscles, Tendons and Ligaments'''- Large muscles of the neck such as the [[sternocleidomastoid]] and the [[trapezius]] enable gross motor movements in the neck. The most common pain produced by these structures is a neck strain which affects the cervical muscles and tendons or a sprain which affects the ligaments, both involving overstretching or tearing these structures. | ||
'''Nerves'''- Cervical spine nerves provide functional control and sensation to different parts of the body based on the spinal level at which they sit. There are 8 cervical nerves: C1,C2 and C3 help control the head and neck, including movements forward, backward, and to the sides<ref name=":3">Magee DJ. Orthopedic physical assessment 5th ed. St. Louis, Mo, Saunders Elsevier. 2008.</ref> | '''Nerves'''- Cervical spine nerves provide functional control and sensation to different parts of the body based on the spinal level at which they sit. There are 8 cervical nerves: C1,C2 and C3 help control the head and neck, including movements forward, backward, and to the sides. <ref name=":3">Magee DJ. Orthopedic physical assessment 5th ed. St. Louis, Mo, Saunders Elsevier. 2008.</ref> C4 helps to control upward shoulder movement and helps to power the [[Diaphragmatic Breathing Exercises|diaphragm]], C5 helps to control the deltoids and the biceps. C6 helps to control the wrist extensors and provides some innervation to the biceps, <ref name=":4">Childress MA, Becker BA. [https://www.aafp.org/afp/2016/0501/p746.html?utm_cmpid=aafp&utm_div=pub&utm_mission=pe&utm_prod=afpj&hootPostID=897adeddb2b04f90e293a97eeadab602#afp20160501p746-c1 Nonoperative management of cervical radiculopathy]. American family physician. 2016 May 1;93(9):746-54.</ref> C7 helps control the triceps and wrist extensors, and finally C8 helps control movement of the hands, such as finger flexion. <ref name=":3" /><ref name=":4" /> Pain can be caused when a nerve branching away from the spinal cord is compressed or irritated and sensation such as tingling is often felt in the upper extremities aiding identification of the damaged nerve. | ||
[[File:Nerves, bones and muscles of the neck .png|thumb|Nerves, muscles and bones of the neck.|alt=|800x800px|center]] | [[File:Nerves, bones and muscles of the neck .png|thumb|Nerves, muscles and bones of the neck.|alt=|800x800px|center]] | ||
== | ===Causes=== | ||
The neck is responsible for supporting the weight for the head and is flexible to allow rotation, flexion, extension and lateral flexion to occur. The neck is also vulnerable to conditions that cause pain and restrict motion. There are a variety of | The neck is responsible for supporting the weight for the head and is flexible to allow rotation, flexion, extension and lateral flexion to occur. The neck is also vulnerable to conditions that cause pain and restrict motion. There are a variety of reasons that can contribute to NP, these may include: <ref>Cooper G. Types of Neck Pain. Spine-Health. Available from: https://www.spine-health.com/conditions/neck-pain/types-neck-pain [accessed 5/3/2023] | ||
</ref> | |||
* '''Muscle strains.''' The most common cause of NP. Neck strains are caused by overuse of the neck muscles such as too many hours sat hunched in a chair. | |||
*'''Weakness.''' Training the upper traps more than the lower and mid traps may lead to overstimulation of the upper traps resulting in NP. | |||
*'''Worn joints.''' As we age our joints in the neck become worn down. Osteoarthritis causes the cartilage between vertebrae to deteriorate. This can then cause osteophytes to form that can affect range of motion and cause pain. | |||
*'''Nerve compression.''' Herniated disks or osteophytes in the vertebrae of your neck can press on the nerves branching out from the intervertebral foramen. | |||
*'''Injuries.''' Motor collisions and sporting injuries can often result in whiplash injury, which occurs when the head is jerked backward and then forward, straining the soft tissues of the neck. | |||
*'''Diseases.''' Diseases, such as [[Rheumatoid Arthritis|rheumatoid arthritis]], [[meningitis]] or cancer, can cause NP. | |||
== Purpose == | |||
There are several guidelines on NP. The European have been systematically reviewed by Corp et al. <ref>Corp N., Mansell G., Stynes S., Wynne-Jones G., Morsø L., Hill J., van der Windt D. [https://pubmed.ncbi.nlm.nih.gov/33064878/ Evidence-based treatment recommendations for neck and low back pain across Europe: A systematic review of guidelines.] Eur J Pain 2021; 25;275-295.</ref> | |||
In this page, we report the American (APTA) guidance. In 2017, The Orthopaedic Section of the American Physical Therapy Association (APTA) revised the previous clinical practice guidelines of NP from 2008 and produced a new summary of recommendations from current peer-reviewed literature. <ref name=":5">Blanpied P., Gross A., Elliott J., Devaney L., Clewley D., Walton D., et al. [https://www.jospt.org/doi/10.2519/jospt.2017.0302 Neck pain: revision 2017: clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association.] JOSPT. 2017 Jul;47(7):A1-83.</ref> The purpose of the updated APTA clinical guidelines was to provide guidance and recommendations on the new evidence-based physical therapy practices around pathoanatomical features, examination, diagnosis/classification, intervention and treatment of musculoskeletal disorders related to NP. This guidance is described below. | |||
== | ==Classification== | ||
Clinicians should use limitation of motion in the cervical and upper thoracic regions, presence of cervical pain related [[headache]], history of trauma, and referred or radiating pain into an upper extremity as useful clinical findings for classifying a patient with | Clinicians should use limitation of motion in the cervical and upper thoracic regions, presence of cervical pain-related [[headache]], history of trauma, and referred or radiating pain into an upper extremity as useful clinical findings for classifying a patient with NP into the following categories: <ref name=":5" /> | ||
* Neck pain with mobility deficits | * Neck pain with mobility deficits | ||
| Line 65: | Line 44: | ||
* Neck pain with radiating pain | * Neck pain with radiating pain | ||
From examination, clinicians should categorise NP patients into one of the four previously mentioned groups in order to deliver the most appropriate treatment plan. To group patients, the clinician should carry out an appropriate subjective and objective examination (Grade of Recommendation: C). Below are the key findings to assess when placing patients into these categories. However, the classifications outlined are not exhaustive and therefore, designating patients requires individual clinical judgement based on the examination findings. | |||
=== Neck pain with mobility deficits: === | |||
=== | |||
* Central and/or unilateral neck pain | * Central and/or unilateral neck pain | ||
* Limitation in neck motion that consistently reproduces symptoms | * Limitation in neck motion that consistently reproduces symptoms | ||
* Associated (referred) [[shoulder]] girdle or upper extremity pain may be present | * Associated (referred) [[shoulder]] girdle or upper extremity pain may be present | ||
* Limited cervical ROM | * Limited cervical ROM | ||
* Neck pain reproduced at end ranges of active and passive motions | * Neck pain reproduced at end ranges of active and passive motions | ||
* Restricted cervical and thoracic segmental mobility | * Restricted cervical and thoracic segmental mobility | ||
* Intersegmental mobility testing reveals characteristic restriction | * Intersegmental mobility testing reveals characteristic restriction | ||
* Neck and referred pain reproduced with provocation of the involved cervical or upper thoracic segments or cervical musculature | * Neck and referred pain reproduced with provocation of the involved cervical or upper thoracic segments or cervical musculature | ||
* Deficits in cervicoscapulothoracic strength and motor control may be present in individuals with subacute or chronic neck pain | * Deficits in cervicoscapulothoracic strength and motor control may be present in individuals with subacute or chronic neck pain | ||
=== | ==='''Neck pain with movement coordination impairments (including Whiplash Associated Disorders):'''=== | ||
* Mechanism of onset linked to trauma or whiplash | * Mechanism of onset linked to trauma or whiplash | ||
* Associated (referred) shoulder girdle or upper extremity pain | * Associated (referred) shoulder girdle or upper extremity pain | ||
* Associated varied nonspecific [[Concussion|concussive]] signs and symptoms | * Associated varied nonspecific [[Assessment and Management of Concussion|concussive]] signs and symptoms | ||
* Dizziness/nausea | * Dizziness/nausea | ||
* Headache, concentration, or memory difficulties; confusion; hypersensitivity to mechanical, thermal, acoustic, odor, or light stimuli; heightened affective distress | * Headache, concentration, or memory difficulties; confusion; hypersensitivity to mechanical, thermal, acoustic, odor, or light stimuli; heightened affective distress | ||
| Line 154: | Line 70: | ||
* Point tenderness may include myofascial trigger points | * Point tenderness may include myofascial trigger points | ||
* Sensorimotor impairment may include altered muscle activation patterns, proprioceptive deficit, postural balance or control | * Sensorimotor impairment may include altered muscle activation patterns, proprioceptive deficit, postural balance or control | ||
* Neck and referred pain reproduced by provocation of the involved cervical segments | * Neck and referred pain reproduced by provocation of the involved cervical segments | ||
=== | ==='''Neck pain with headaches (cervicogenic headaches)'''=== | ||
* Non-continuous, unilateral neck pain and associated (referred) headache | * Non-continuous, unilateral neck pain and associated (referred) headache | ||
* Headache is precipitated or aggravated by neck movements or sustained positions/postures | * Headache is precipitated or aggravated by neck movements or sustained positions/postures | ||
| Line 165: | Line 81: | ||
* Strength, endurance, and coordination deficits of the neck muscle | * Strength, endurance, and coordination deficits of the neck muscle | ||
=== | ==='''Neck pain with radiating pain (radicular)'''=== | ||
* Neck pain with radiating (narrow band of lancinating) pain in the involved extremity | * Neck pain with radiating (narrow band of lancinating) pain in the involved extremity | ||
* Upper extremity dermatomal paresthesia or numbness, and myotomal muscle weakness | * Upper extremity dermatomal paresthesia or numbness, and myotomal muscle weakness | ||
| Line 171: | Line 87: | ||
* May have upper extremity sensory, strength, or reflex deficits associated with the involved nerve roots | * May have upper extremity sensory, strength, or reflex deficits associated with the involved nerve roots | ||
== | =='''Physical Impairment Measures'''== | ||
Physical examination should be undertaken to establish baselines and monitor changes over time (Grade of Recommendation: B). Physical assessments can also be useful in the ruling in/out of conditions/causes of NP. Algometric assessment of pressure pain threshold should be used for classifying pain. | |||
=== ''' | ===='''Neck Pain with Mobility Deficits'''==== | ||
* Physical Impairment Measures: Cervical active ROM, the cervical flexion-rotation test and thoracic segmental mobility tests. | |||
===='''Neck Pain with Movement Coordination Impairments'''==== | |||
* Physical Impairment Measures: Cranial cervical flexion test and neck flexor muscle endurance test. | |||
===='''Neck Pain with Headaches'''==== | |||
* Physical Impairment Measures: Cervical active ROM, the cervical flexion-rotation test and upper cervical segmental mobility testing. | |||
===='''Neck Pain with Radiating Pain'''==== | |||
* Assessment Criteria for [[Cervical Radiculopathy|cervical radiculopathy]] <ref>Rubinstein S., Pool J., van Tulder M., Riphagen I., de Vet HC. [https://pubmed.ncbi.nlm.nih.gov/17013656/ A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy.] Eur Spine J. 2007; 16(3): 307-19.</ref>: Sterling’s test; This test has a sensitivity of 50 and a specificity of 88; [[Upper Limb Tension Tests (ULTTs)|Upper limb tension test]]. This test has a sensitivity of 50 and specificity of 86; [[Distraction Test|Cranial distraction test.]] This test has a sensitivity of 48 and a specificity of 98. When all of these clinical features are present, the post-test probability of cervical radiculopathy is '''90%''' | |||
* Physical Impairment Measures: [[Neurodynamic Assessment|Neurodynamic testing]], [[Spurling's Test|Spurling’s test]], the [[Distraction Test|distraction test]] and Valsalva test. | |||
==Differential Diagnosis == | |||
If a patient’s impairments do not fall into the above classification system categories, or the interventions do not improve the clinical presentation, the clinician should consider serious pathological conditions or psychosocial factors as being possible explanations to the patient’s pain. | |||
=== '''Eliminating Red flags''' === | |||
Clinicians should ensure that they carry out a thorough subjective screening for patients who present with NP. Subjective assessments should be used to eliminate possible red flags or serious pathology such as: <ref>Ramanayake RP, Basnayake BM. [https://doi.org/10.4103/jfmpc.jfmpc_510_15 Evaluation of red flags minimizes missing serious diseases in primary care.] Journal of family medicine and primary care. 2018 Mar;7(2):315.</ref> | |||
*[[Fracture|Fractures]] | |||
* Instability of the vertebrae | |||
* Coronary Artery Dysfunction (CAD) | |||
*[[Myelopathy]] | |||
*[[Cancer Rehabilitation and the Importance of Balance Training|Cancer]] | |||
*[[Infection Prevention and Control|Infection]] | |||
* Visceral disorders | |||
* Clinicians should also consider eliminating the 5 D 3 N red flags to rule out potential myelopathy. | |||
* Dizziness | |||
* Diplopia (double vision) | |||
* Drop attacks | |||
*[[Dysphagia]] (swallowing difficulties) | |||
*[[Dysarthria]] (problems with speech) | |||
*[[Nystagmus]] (involuntary eye movements) | |||
* Nausea | |||
* Neurological symptoms | |||
==Other Examination Recommendations== | |||
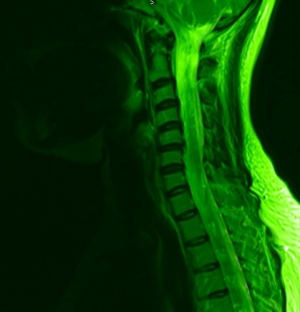
[[Image:Greenneck.jpg|thumb|right|Cervical Spine MRI.]] | |||
=== '''The use of Outcome Measures''' === | |||
Outcome tools can be used for evaluations, monitoring change over time, diagnosis and prognosis of NP. Validated self-report questionnaires should be used with patients (Grade of Recommendation: A). [[Neck Disability Index|The Neck Disability Index]] and the [[Patient Specific Functional Scale]] are two examples of these questionnaires. The main reason for this recommendation is that these tools establish a baseline status for pain, function, and disability that can be used later in intervention selection and goal tracking. | |||
Easily reproducible measures for activity and participation limitations related to NP should be used (Grade of Recommendation: F). This is to assess the change in function throughout the episode of care. An example of a tool to carry this out is the spinal function sort tool which like many other measures are more specific to [https://www.physio-pedia.com/Low_Back_Pain low back pain] and is part of the reasons for this recommendation being grade F. A study reports that the modified spinal function sort tool has good reliability and validity for assessing perceived self efficacy of work related tasks and the authors recommend this for patients with chronic musculoskeletal (MSK) disorders. <ref>Trippolini M., Janssen S., Hilfiker R., Oesch P. [https://link.springer.com/article/10.1007/s10926-017-9717-y Measurement properties of the modified spinal function sort (M-SFS): is it reliable and valid in workers with chronic musculoskeletal pain?]. Journal of Occupational Rehabilitation. 2018 Jun;28(2):322-31.</ref> | |||
=== '''The consideration of risk factors that can predispose a patient to chronic neck pain''' === | |||
On the first instance of treating a patient with acute NP, it may be useful to consider if the patient has any risk factors for developing chronic NP. (Grade of Recommendation: B) Early detection of risk factors can allow the clinician to implement strategies to decrease the likelihood of developing chronic pain. <ref>Kim R, Wiest C, Clark K, Cook C, Horn M. [https://doi.org/10.1016/j.msksp.2017.11.007 Identifying risk factors for first-episode neck pain: a systematic review]. Musculoskeletal Science and Practice. 2018 Feb 1;33:77-83.</ref> Possible risk factors are: | |||
* Female | |||
* History of NP | |||
* High job demands | |||
* Smoking | |||
* Low social/work support | |||
* History of [https://www.physio-pedia.com/Low_Back_Pain low back pain] | |||
* Older age | |||
* Depressed mood | |||
* High role conflict | |||
* Perceived muscular tension | |||
== Intervention & Treatment Recommendations == | |||
=== '''Neck Pain with Mobility Deficits'''=== | |||
==== '''Acute''' ==== | ==== '''Acute''' ==== | ||
Acute | Acute NP with mobility deficits can be managed in a variety of different ways. Recommended interventions include: thoracic manipulations, neck ROM exercises (such as movement through restricted range with increases in range to progress), scapulothoracic and UL and upper extremity strengthening, and cervical manipulation and/or mobilisation (such as AP glide of cervical spine). | ||
Practitioners should also aim to enhance | Practitioners should also aim to enhance programme adherence, which has been shown to improve with the inclusion of thoracic manipulation, neck ROM exercises and scapulothoracic and upper extremity strengthening. | ||
==== '''Subacute''' ==== | ==== '''Subacute''' ==== | ||
For subacute management of | For subacute management of NP with mobility deficits the following has been advised: neck and shoulder girdle endurance exercises (e.g. chin tuck endurance exercises. With gravity, against gravity, etc.), thoracic manipulation, and cervical manipulation and/or cervical mobilisation. | ||
==== '''Chronic''' ==== | ==== '''Chronic''' ==== | ||
Chronic | Chronic NP with mobility deficits benefit more from a multimodal management technique, to include: thoracic manipulation and cervical manipulation or mobilisation; mixed exercises for cervical/scapulothoracic regions: neuromuscular exercise (e.g. coordination, proprioception, and postural training), stretching, strengthening, endurance training, aerobic conditioning, and cognitive affective elements; or intermittent mechanical/manual traction. | ||
Dry needling can also be used as an intervention. It has been shown to be effective in short-term and long-term follow-ups when measuring its effect on: pain intensity, mechanical hyperalgesia, neck active range of motion, neck muscle strength, and perceived neck disability<ref>Cerezo-Téllez E, Torres-Lacomba M, Fuentes-Gallardo I, Perez-Muñoz M, Mayoral-del-Moral O, Lluch-Girbés E, Prieto-Valiente L, Falla D. [https://journals.lww.com/pain/Abstract/2016/09000/Effectiveness_of_dry_needling_for_chronic.7.aspx Effectiveness of dry needling for chronic nonspecific neck pain: a randomized, single-blinded, clinical trial]. Pain. 2016 Sep 1;157(9):1905-17.</ref> | Dry needling can also be used as an intervention. It has been shown to be effective in short-term and long-term follow-ups when measuring its effect on: pain intensity, mechanical hyperalgesia, neck active range of motion, neck muscle strength, and perceived neck disability. <ref>Cerezo-Téllez E., Torres-Lacomba M., Fuentes-Gallardo I., Perez-Muñoz M., Mayoral-del-Moral O., Lluch-Girbés E., Prieto-Valiente L., Falla D. [https://journals.lww.com/pain/Abstract/2016/09000/Effectiveness_of_dry_needling_for_chronic.7.aspx Effectiveness of dry needling for chronic nonspecific neck pain: a randomized, single-blinded, clinical trial]. Pain. 2016 Sep 1;157(9):1905-17.</ref> | ||
Low-effect laser therapy can provide relief from chronic | Low-effect laser therapy can provide relief from chronic NP for 2-6 months, with no serious side effects or complications being reported. <ref>Swedish Council on Health Technology Assessment. [https://www.sbu.se/en/publications/sbu-assesses/laser-treatment-of-neck-pain/ <nowiki>Laser Treatment of Neck Pain [Internet]</nowiki>]. Stockholm: Swedish Council on Health Technology Assessment (SBU); 2014 May 20. SBU Alert Report No. 2014-03. </ref> | ||
Furthermore, patient education should be provided in order to recommend an active lifestyle and address cognitive and affective factors – e.g. help to arrange a suitable weekly activity schedule. | Furthermore, patient education should be provided in order to recommend an active lifestyle and address cognitive and affective factors – e.g. help to arrange a suitable weekly activity schedule. | ||
| Line 194: | Line 171: | ||
Lastly, neck, shoulder girdle and trunk endurance exercises should be used – e.g. plank, side plank, shoulder shrugs, etc. | Lastly, neck, shoulder girdle and trunk endurance exercises should be used – e.g. plank, side plank, shoulder shrugs, etc. | ||
=== '''Neck Pain with Movement Coordination Impairments''' === | |||
=== ''' | |||
==== '''Acute''' ==== | ==== '''Acute''' ==== | ||
Acute management of | Acute management of NP with movement coordination impairments should be managed with a strong focus on education, to include: return to nonprovocative pre-accident activities as soon as they are able to; minimise use of cervical collar; encourage postural and mobility exercises to decrease pain and increase ROM; reassure the patient of average recovery times of up to 2-3 months. | ||
Furthermore, a multimodal approach is favoured, to include: manual mobilisation techniques alongside exercise (e.g. strengthening, endurance, flexibility, postural, coordination, aerobic, and functional exercises). | Furthermore, a multimodal approach is favoured, to include: manual mobilisation techniques alongside exercise (e.g. strengthening, endurance, flexibility, postural, coordination, aerobic, and functional exercises). | ||
If a patient is at low risk of progressing towards chronicity then the intervention applied should be focused around patient independence and involvement through education and a home exercise programme (HEP): a single session consisting of early advice, exercise instruction, and education; along with a comprehensive exercise program (to include strength and/or endurance with/without coordination exercises); and Transcutaneous electrical nerve stimulation (TENS) | If a patient is at low risk of progressing towards chronicity then the intervention applied should be focused around patient independence and involvement through education and a home exercise programme (HEP): a single session consisting of early advice, exercise instruction, and education; along with a comprehensive exercise program (to include strength and/or endurance with/without coordination exercises); and Transcutaneous electrical nerve stimulation (TENS). | ||
It has been found that an effective HEP has a strong correlation with reduced | It has been found that an effective HEP has a strong correlation with reduced NP, increased function, decreased disability and improved QoL. <ref>Zronek M., Sanker H., Newcomb J., Donaldson M. [https://doi.org/10.1179/2042618613Y.0000000047 The influence of home exercise programs for patients with non-specific or specific neck pain: a systematic review of the literature]. J Manual Manipulative Ther. 2016 Mar 14;24(2):62-73.</ref> Specifically, HEPs were more effective when they utilised self-mobilisation techniques, strengthening exercises, endurance exercises, and when the HEPs were designed to address a specific spinal level. | ||
The current research on TENS in relation to | The current research on TENS in relation to NP is fairly sparse. Although effects have been seen, they have been limited to short-term effects, that usually recur; and show no sign of responding to treatment in the long-term. It’s also been shown that TENS is more effective than placebo, and seems to have an effect in reducing the intensity of acute and chronic cervical pain. <ref>Paolucci T., Agostini F., Paoloni M., de Sire A., Verna S., Pesce M., Ribecco L., Mangone M., Bernetti A., Saggini R. [https://doi.org/10.3390/app11083423 Efficacy of TENS in Cervical Pain Syndromes: An Umbrella Review of Systematic Reviews]. Applied Sciences. 2021 Jan;11(8):3423.</ref><ref>Kroeling P., Gross A., Graham N., Burnie S., Szeto G., Goldsmith C., et al. [https://doi.org/10.1002/14651858.CD004251.pub5 Electrotherapy for neck pain.] Cochrane database of systematic reviews. 2013 Aug 26;(8): CD004251.</ref> | ||
Patients who are showing signs of progressing towards chronicity or delayed rehabilitation outcomes should be identified and monitored as early as possible, in order to provide them with a more intensive rehabilitation and an early pain education | Patients who are showing signs of progressing towards chronicity or delayed rehabilitation outcomes should be identified and monitored as early as possible, in order to provide them with a more intensive rehabilitation and an early pain education programme. | ||
==== '''Chronic''' ==== | ==== '''Chronic''' ==== | ||
Management of | Management of chronic NP with Movement Coordination Impairments follows a similar emphasis on education and advice, focusing on assurance, encouragement, prognosis, and pain management. | ||
Furthermore, mobilisation combined with an individualised, progressive submaximal exercise | Furthermore, mobilisation combined with an individualised, progressive submaximal exercise programme including cervicothoracic strengthening, endurance, flexibility, and coordination, using principles of cognitive behavioural therapy is advised. This can be used alongside TENS. | ||
=== ''' | === '''Neck Pain with Headaches'''=== | ||
==== '''Acute''' ==== | ==== '''Acute''' ==== | ||
For management of acute | For management of acute NP with headaches, an emphasis should be mainly placed on mobilisation. | ||
Active mobility exercises should be provided along with supervised instruction to be given by the practitioner. | Active mobility exercises should be provided along with supervised instruction to be given by the practitioner. | ||
| Line 225: | Line 200: | ||
Furthermore, C1-C2 self-sustained natural apophyseal glide (self-SNAG) exercises should also be provided to be completed independently. | Furthermore, C1-C2 self-sustained natural apophyseal glide (self-SNAG) exercises should also be provided to be completed independently. | ||
C1-C2 self-sustained natural apophyseal glide rotation exercises have shown improved results when combined with C1-C2 self-SNAG exercises, in comparison to C1-C2 self-SNAG exercises alone. This presented as a strong effect on pain intensity, physical function, CFRT and pain catastrophising. Furthermore, moderate improvements were seen in active | C1-C2 self-sustained natural apophyseal glide rotation exercises have shown improved results when combined with C1-C2 self-SNAG exercises, in comparison to C1-C2 self-SNAG exercises alone. This presented as a strong effect on pain intensity, physical function, CFRT and pain catastrophising. Furthermore, moderate improvements were seen in active cervical range of movement, kinesiophobia and fear-avoidance beliefs. <ref>Paquin J., Tousignant-Laflamme Y., Dumas J. [https://doi.org/10.1080/10669817.2020.1864960 Effects of SNAG mobilization combined with a self-SNAG home-exercise for the treatment of cervicogenic headache: a pilot study.] J Manual Manipulative Ther. 2021 Feb; 6:1-1.</ref> | ||
==== '''Subacute''' ==== | ==== '''Subacute''' ==== | ||
Subacute | Subacute NP with headaches should also be managed with an emphasis on mobilisation, both independent and passively employed by a practitioner. This is to include: | ||
* cervical manipulation and | * cervical manipulation and mobilisation. | ||
* C1–2 self-SNAG exercise and/or C1-2 SNAG rotation exercises | * C1–2 self-SNAG exercise and/or C1-2 SNAG rotation exercises | ||
==== '''Chronic''' ==== | ==== '''Chronic''' ==== | ||
Chronic | Chronic NP with headaches should be managed through an intervention of cervical or cervicothoracic manipulation or mobilisations. This can be paired with shoulder girdle and neck stretching, alongside strengthening and endurance exercises for the shoulder girdle and neck. | ||
=== '''Neck Pain with Radiating Pain''' === | |||
=== ''' | |||
==== '''Acute''' ==== | ==== '''Acute''' ==== | ||
Acute management of | Acute management of NP with radiating pain focuses on a few different modalities. One intervention available to practitioners is mobilising and stabilising exercises. Another intervention available to practitioners for acute management of NP with radiating pain, is laser intervention. Finally, practitioners may employ use of a cervical collar, but only in the short-term. | ||
Another intervention available to practitioners for acute management of | |||
Finally, practitioners may employ use of a cervical collar, but only in the short-term. | |||
==== '''Chronic''' ==== | ==== '''Chronic''' ==== | ||
Management of chronic | Management of chronic NP with radiating pain, completely differs from acute management. Mechanical intermittent cervical traction can be used as an intervention in chronic patients, in conjunction with stretching and strengthening exercises, and cervical and thoracic mobilisation and/or manipulation. | ||
Mechanical intermittent cervical traction can be used as an intervention in chronic patients, in conjunction with stretching and strengthening exercises, and cervical and thoracic mobilisation and/or manipulation. | |||
Traction should be used in conjunction with other interventions, because on its own it has found limited success. It has been shown that traction has no specific benefits as an intervention for chronic neck pain in adults when compared to standard physiotherapy interventions<ref>Borman P, Keskin D, Ekici B, Bodur H. [https://link.springer.com/article/10.1007%2Fs10067-008-0895-z The efficacy of intermittent cervical traction in patents with chronic neck pain]. Clinical | Traction should be used in conjunction with other interventions, because on its own it has found limited success. It has been shown that traction has no specific benefits as an intervention for chronic neck pain in adults when compared to standard physiotherapy interventions. <ref>Borman P., Keskin D., Ekici B., Bodur H. [https://link.springer.com/article/10.1007%2Fs10067-008-0895-z The efficacy of intermittent cervical traction in patents with chronic neck pain]. Clinical Rheumatology. 2008 Oct 1;27(10):1249-53.</ref> However, the research suggests exercise as a more relevant therapeutic management strategy. | ||
Alongside other interventions, education and counselling to encourage participation in exercises and occupational activities are recommended. | Alongside other interventions, education and counselling to encourage participation in exercises and occupational activities are recommended. | ||
== References == | == References == | ||
| Line 294: | Line 241: | ||
[[Category:Musculoskeletal/Orthopaedics]] | [[Category:Musculoskeletal/Orthopaedics]] | ||
[[Category:MCG Student Project]] | [[Category:MCG Student Project]] | ||
[[Category:Nottingham University Spinal Rehabilitation Project]] | |||
Latest revision as of 11:40, 26 April 2023
Original Editors - Chad Adams, Jacob Melnick, & Tyler Shultz as part of theNottingham University Spinal Rehabilitation Project
Lead Editors Tyler Shultz, Kim Jackson, Angeliki Chorti, Cindy John-Chu, Alexandra Malzer, Eric Robertson, Admin, Dorian Mars, Jacob Melnick, Evan Thomas, Zachary Cooper, Albert Alabaster, Scott Buxton, WikiSysop, Rachael Lowe, Nupur Smit Shah, Tony Lowe, Chad Adams, Simisola Ajeyalemi and Agoro Bukola Zainab
Introduction[edit | edit source]
Neck Pain (NP) lacks a uniform operational definition. [1] Nevertheless, the most commonly reported type is non-specific or mechanical NP characterised by symptoms of a non-specific nature or mechanical basis. [2] Common presentations of NP may include muscle pain, muscle spasm, headache, facet joint pain, nerve pain, referred pain and bone pain. [3]
NP is becoming increasingly common throughout the world [4] with around two thirds of people experiencing NP at one moment in their life. The prevalence of NP varies largely between studies; mean reported estimates are 7.6% for point prevalence and 48.5% for lifetime prevalence. [2] Most studies indicate a higher incidence of NP among women, [4] anxiety or depression sufferers [5] and office workers with poor ergonomic positions. [6]
Anatomy[edit | edit source]
Bones and Joints- The neck consists of 7 bones C1-C7. The most common NP caused by problems to the bone is osteoarthritis with wear in cartilage between the joints causing the bones to rub together producing pain and stiffness. [7] These bones are linked together by facet joints which are small joints between vertebrae.
Muscles, Tendons and Ligaments- Large muscles of the neck such as the sternocleidomastoid and the trapezius enable gross motor movements in the neck. The most common pain produced by these structures is a neck strain which affects the cervical muscles and tendons or a sprain which affects the ligaments, both involving overstretching or tearing these structures.
Nerves- Cervical spine nerves provide functional control and sensation to different parts of the body based on the spinal level at which they sit. There are 8 cervical nerves: C1,C2 and C3 help control the head and neck, including movements forward, backward, and to the sides. [8] C4 helps to control upward shoulder movement and helps to power the diaphragm, C5 helps to control the deltoids and the biceps. C6 helps to control the wrist extensors and provides some innervation to the biceps, [9] C7 helps control the triceps and wrist extensors, and finally C8 helps control movement of the hands, such as finger flexion. [8][9] Pain can be caused when a nerve branching away from the spinal cord is compressed or irritated and sensation such as tingling is often felt in the upper extremities aiding identification of the damaged nerve.
Causes[edit | edit source]
The neck is responsible for supporting the weight for the head and is flexible to allow rotation, flexion, extension and lateral flexion to occur. The neck is also vulnerable to conditions that cause pain and restrict motion. There are a variety of reasons that can contribute to NP, these may include: [10]
- Muscle strains. The most common cause of NP. Neck strains are caused by overuse of the neck muscles such as too many hours sat hunched in a chair.
- Weakness. Training the upper traps more than the lower and mid traps may lead to overstimulation of the upper traps resulting in NP.
- Worn joints. As we age our joints in the neck become worn down. Osteoarthritis causes the cartilage between vertebrae to deteriorate. This can then cause osteophytes to form that can affect range of motion and cause pain.
- Nerve compression. Herniated disks or osteophytes in the vertebrae of your neck can press on the nerves branching out from the intervertebral foramen.
- Injuries. Motor collisions and sporting injuries can often result in whiplash injury, which occurs when the head is jerked backward and then forward, straining the soft tissues of the neck.
- Diseases. Diseases, such as rheumatoid arthritis, meningitis or cancer, can cause NP.
Purpose[edit | edit source]
There are several guidelines on NP. The European have been systematically reviewed by Corp et al. [11]
In this page, we report the American (APTA) guidance. In 2017, The Orthopaedic Section of the American Physical Therapy Association (APTA) revised the previous clinical practice guidelines of NP from 2008 and produced a new summary of recommendations from current peer-reviewed literature. [12] The purpose of the updated APTA clinical guidelines was to provide guidance and recommendations on the new evidence-based physical therapy practices around pathoanatomical features, examination, diagnosis/classification, intervention and treatment of musculoskeletal disorders related to NP. This guidance is described below.
Classification[edit | edit source]
Clinicians should use limitation of motion in the cervical and upper thoracic regions, presence of cervical pain-related headache, history of trauma, and referred or radiating pain into an upper extremity as useful clinical findings for classifying a patient with NP into the following categories: [12]
- Neck pain with mobility deficits
- Neck pain with movement coordination impairments
- Neck pain with headaches
- Neck pain with radiating pain
From examination, clinicians should categorise NP patients into one of the four previously mentioned groups in order to deliver the most appropriate treatment plan. To group patients, the clinician should carry out an appropriate subjective and objective examination (Grade of Recommendation: C). Below are the key findings to assess when placing patients into these categories. However, the classifications outlined are not exhaustive and therefore, designating patients requires individual clinical judgement based on the examination findings.
Neck pain with mobility deficits:[edit | edit source]
- Central and/or unilateral neck pain
- Limitation in neck motion that consistently reproduces symptoms
- Associated (referred) shoulder girdle or upper extremity pain may be present
- Limited cervical ROM
- Neck pain reproduced at end ranges of active and passive motions
- Restricted cervical and thoracic segmental mobility
- Intersegmental mobility testing reveals characteristic restriction
- Neck and referred pain reproduced with provocation of the involved cervical or upper thoracic segments or cervical musculature
- Deficits in cervicoscapulothoracic strength and motor control may be present in individuals with subacute or chronic neck pain
Neck pain with movement coordination impairments (including Whiplash Associated Disorders):[edit | edit source]
- Mechanism of onset linked to trauma or whiplash
- Associated (referred) shoulder girdle or upper extremity pain
- Associated varied nonspecific concussive signs and symptoms
- Dizziness/nausea
- Headache, concentration, or memory difficulties; confusion; hypersensitivity to mechanical, thermal, acoustic, odor, or light stimuli; heightened affective distress
- Positive craniocervical flexion test
- Positive neck flexor muscle endurance test
- Positive pressure algometry
- Strength and endurance deficits of the neck muscles
- Neck pain with mid-range motion that worsens with end-range positions
- Point tenderness may include myofascial trigger points
- Sensorimotor impairment may include altered muscle activation patterns, proprioceptive deficit, postural balance or control
- Neck and referred pain reproduced by provocation of the involved cervical segments
Neck pain with headaches (cervicogenic headaches)[edit | edit source]
- Non-continuous, unilateral neck pain and associated (referred) headache
- Headache is precipitated or aggravated by neck movements or sustained positions/postures
- Positive cervical flexion rotation test
- Headache reproduced with provocation of the involved upper cervical segments
- Limited cervical ROM
- Restricted upper cervical segmental mobility
- Strength, endurance, and coordination deficits of the neck muscle
Neck pain with radiating pain (radicular)[edit | edit source]
- Neck pain with radiating (narrow band of lancinating) pain in the involved extremity
- Upper extremity dermatomal paresthesia or numbness, and myotomal muscle weakness
- Neck and neck-related radiating pain reproduced or relieved with radiculopathy testing: positive test cluster includes upper-limb nerve mobility, Spurling’s test, cervical distraction, cervical ROM
- May have upper extremity sensory, strength, or reflex deficits associated with the involved nerve roots
Physical Impairment Measures[edit | edit source]
Physical examination should be undertaken to establish baselines and monitor changes over time (Grade of Recommendation: B). Physical assessments can also be useful in the ruling in/out of conditions/causes of NP. Algometric assessment of pressure pain threshold should be used for classifying pain.
Neck Pain with Mobility Deficits[edit | edit source]
- Physical Impairment Measures: Cervical active ROM, the cervical flexion-rotation test and thoracic segmental mobility tests.
Neck Pain with Movement Coordination Impairments[edit | edit source]
- Physical Impairment Measures: Cranial cervical flexion test and neck flexor muscle endurance test.
Neck Pain with Headaches[edit | edit source]
- Physical Impairment Measures: Cervical active ROM, the cervical flexion-rotation test and upper cervical segmental mobility testing.
Neck Pain with Radiating Pain[edit | edit source]
- Assessment Criteria for cervical radiculopathy [13]: Sterling’s test; This test has a sensitivity of 50 and a specificity of 88; Upper limb tension test. This test has a sensitivity of 50 and specificity of 86; Cranial distraction test. This test has a sensitivity of 48 and a specificity of 98. When all of these clinical features are present, the post-test probability of cervical radiculopathy is 90%
- Physical Impairment Measures: Neurodynamic testing, Spurling’s test, the distraction test and Valsalva test.
Differential Diagnosis[edit | edit source]
If a patient’s impairments do not fall into the above classification system categories, or the interventions do not improve the clinical presentation, the clinician should consider serious pathological conditions or psychosocial factors as being possible explanations to the patient’s pain.
Eliminating Red flags[edit | edit source]
Clinicians should ensure that they carry out a thorough subjective screening for patients who present with NP. Subjective assessments should be used to eliminate possible red flags or serious pathology such as: [14]
- Fractures
- Instability of the vertebrae
- Coronary Artery Dysfunction (CAD)
- Myelopathy
- Cancer
- Infection
- Visceral disorders
- Clinicians should also consider eliminating the 5 D 3 N red flags to rule out potential myelopathy.
- Dizziness
- Diplopia (double vision)
- Drop attacks
- Dysphagia (swallowing difficulties)
- Dysarthria (problems with speech)
- Nystagmus (involuntary eye movements)
- Nausea
- Neurological symptoms
Other Examination Recommendations[edit | edit source]
The use of Outcome Measures[edit | edit source]
Outcome tools can be used for evaluations, monitoring change over time, diagnosis and prognosis of NP. Validated self-report questionnaires should be used with patients (Grade of Recommendation: A). The Neck Disability Index and the Patient Specific Functional Scale are two examples of these questionnaires. The main reason for this recommendation is that these tools establish a baseline status for pain, function, and disability that can be used later in intervention selection and goal tracking.
Easily reproducible measures for activity and participation limitations related to NP should be used (Grade of Recommendation: F). This is to assess the change in function throughout the episode of care. An example of a tool to carry this out is the spinal function sort tool which like many other measures are more specific to low back pain and is part of the reasons for this recommendation being grade F. A study reports that the modified spinal function sort tool has good reliability and validity for assessing perceived self efficacy of work related tasks and the authors recommend this for patients with chronic musculoskeletal (MSK) disorders. [15]
The consideration of risk factors that can predispose a patient to chronic neck pain[edit | edit source]
On the first instance of treating a patient with acute NP, it may be useful to consider if the patient has any risk factors for developing chronic NP. (Grade of Recommendation: B) Early detection of risk factors can allow the clinician to implement strategies to decrease the likelihood of developing chronic pain. [16] Possible risk factors are:
- Female
- History of NP
- High job demands
- Smoking
- Low social/work support
- History of low back pain
- Older age
- Depressed mood
- High role conflict
- Perceived muscular tension
Intervention & Treatment Recommendations[edit | edit source]
Neck Pain with Mobility Deficits[edit | edit source]
Acute[edit | edit source]
Acute NP with mobility deficits can be managed in a variety of different ways. Recommended interventions include: thoracic manipulations, neck ROM exercises (such as movement through restricted range with increases in range to progress), scapulothoracic and UL and upper extremity strengthening, and cervical manipulation and/or mobilisation (such as AP glide of cervical spine).
Practitioners should also aim to enhance programme adherence, which has been shown to improve with the inclusion of thoracic manipulation, neck ROM exercises and scapulothoracic and upper extremity strengthening.
Subacute[edit | edit source]
For subacute management of NP with mobility deficits the following has been advised: neck and shoulder girdle endurance exercises (e.g. chin tuck endurance exercises. With gravity, against gravity, etc.), thoracic manipulation, and cervical manipulation and/or cervical mobilisation.
Chronic[edit | edit source]
Chronic NP with mobility deficits benefit more from a multimodal management technique, to include: thoracic manipulation and cervical manipulation or mobilisation; mixed exercises for cervical/scapulothoracic regions: neuromuscular exercise (e.g. coordination, proprioception, and postural training), stretching, strengthening, endurance training, aerobic conditioning, and cognitive affective elements; or intermittent mechanical/manual traction.
Dry needling can also be used as an intervention. It has been shown to be effective in short-term and long-term follow-ups when measuring its effect on: pain intensity, mechanical hyperalgesia, neck active range of motion, neck muscle strength, and perceived neck disability. [17]
Low-effect laser therapy can provide relief from chronic NP for 2-6 months, with no serious side effects or complications being reported. [18]
Furthermore, patient education should be provided in order to recommend an active lifestyle and address cognitive and affective factors – e.g. help to arrange a suitable weekly activity schedule.
Lastly, neck, shoulder girdle and trunk endurance exercises should be used – e.g. plank, side plank, shoulder shrugs, etc.
Neck Pain with Movement Coordination Impairments[edit | edit source]
Acute[edit | edit source]
Acute management of NP with movement coordination impairments should be managed with a strong focus on education, to include: return to nonprovocative pre-accident activities as soon as they are able to; minimise use of cervical collar; encourage postural and mobility exercises to decrease pain and increase ROM; reassure the patient of average recovery times of up to 2-3 months.
Furthermore, a multimodal approach is favoured, to include: manual mobilisation techniques alongside exercise (e.g. strengthening, endurance, flexibility, postural, coordination, aerobic, and functional exercises).
If a patient is at low risk of progressing towards chronicity then the intervention applied should be focused around patient independence and involvement through education and a home exercise programme (HEP): a single session consisting of early advice, exercise instruction, and education; along with a comprehensive exercise program (to include strength and/or endurance with/without coordination exercises); and Transcutaneous electrical nerve stimulation (TENS).
It has been found that an effective HEP has a strong correlation with reduced NP, increased function, decreased disability and improved QoL. [19] Specifically, HEPs were more effective when they utilised self-mobilisation techniques, strengthening exercises, endurance exercises, and when the HEPs were designed to address a specific spinal level.
The current research on TENS in relation to NP is fairly sparse. Although effects have been seen, they have been limited to short-term effects, that usually recur; and show no sign of responding to treatment in the long-term. It’s also been shown that TENS is more effective than placebo, and seems to have an effect in reducing the intensity of acute and chronic cervical pain. [20][21]
Patients who are showing signs of progressing towards chronicity or delayed rehabilitation outcomes should be identified and monitored as early as possible, in order to provide them with a more intensive rehabilitation and an early pain education programme.
Chronic[edit | edit source]
Management of chronic NP with Movement Coordination Impairments follows a similar emphasis on education and advice, focusing on assurance, encouragement, prognosis, and pain management.
Furthermore, mobilisation combined with an individualised, progressive submaximal exercise programme including cervicothoracic strengthening, endurance, flexibility, and coordination, using principles of cognitive behavioural therapy is advised. This can be used alongside TENS.
Neck Pain with Headaches[edit | edit source]
Acute[edit | edit source]
For management of acute NP with headaches, an emphasis should be mainly placed on mobilisation.
Active mobility exercises should be provided along with supervised instruction to be given by the practitioner.
Furthermore, C1-C2 self-sustained natural apophyseal glide (self-SNAG) exercises should also be provided to be completed independently.
C1-C2 self-sustained natural apophyseal glide rotation exercises have shown improved results when combined with C1-C2 self-SNAG exercises, in comparison to C1-C2 self-SNAG exercises alone. This presented as a strong effect on pain intensity, physical function, CFRT and pain catastrophising. Furthermore, moderate improvements were seen in active cervical range of movement, kinesiophobia and fear-avoidance beliefs. [22]
Subacute[edit | edit source]
Subacute NP with headaches should also be managed with an emphasis on mobilisation, both independent and passively employed by a practitioner. This is to include:
- cervical manipulation and mobilisation.
- C1–2 self-SNAG exercise and/or C1-2 SNAG rotation exercises
Chronic[edit | edit source]
Chronic NP with headaches should be managed through an intervention of cervical or cervicothoracic manipulation or mobilisations. This can be paired with shoulder girdle and neck stretching, alongside strengthening and endurance exercises for the shoulder girdle and neck.
Neck Pain with Radiating Pain[edit | edit source]
Acute[edit | edit source]
Acute management of NP with radiating pain focuses on a few different modalities. One intervention available to practitioners is mobilising and stabilising exercises. Another intervention available to practitioners for acute management of NP with radiating pain, is laser intervention. Finally, practitioners may employ use of a cervical collar, but only in the short-term.
Chronic[edit | edit source]
Management of chronic NP with radiating pain, completely differs from acute management. Mechanical intermittent cervical traction can be used as an intervention in chronic patients, in conjunction with stretching and strengthening exercises, and cervical and thoracic mobilisation and/or manipulation.
Traction should be used in conjunction with other interventions, because on its own it has found limited success. It has been shown that traction has no specific benefits as an intervention for chronic neck pain in adults when compared to standard physiotherapy interventions. [23] However, the research suggests exercise as a more relevant therapeutic management strategy.
Alongside other interventions, education and counselling to encourage participation in exercises and occupational activities are recommended.
References[edit | edit source]
- ↑ Moffett J., McLean S. The role of physiotherapy in the management of non-specific back pain and neck pain. Rheumatology. 2006 Apr 1;45(4):371-8.
- ↑ 2.0 2.1 Binder AI. Cervical spondylosis and neck pain. BMJ. 2007 Mar 8;334(7592):527-31.
- ↑ Harvard Medical School The 7 Faces of Neck Pain. Havard Health Publishing. Available from:https://www.health.harvard.edu/pain/7-faces-of-neck-pain [accessed 4/3/2023]
- ↑ 4.0 4.1 Hoy D., Protani M., De R., Buchbinder R. The epidemiology of neck pain. Best Pract Res Clin Rheumatol. 2010 Dec;24(6):783-92.
- ↑ Elbinoune I., Amine B., Shyen S., Gueddari S., Abouqal R., Hajjaj-Hassouni N. Chronic neck pain and anxiety-depression: prevalence and associated risk factors. Pan African Medical Journal. 2016 Sep 9;24(1).
- ↑ Hush J., Michaleff Z., Maher C., Refshauge K. Individual, physical and psychological risk factors for neck pain in Australian office workers: a 1-year longitudinal study. Eur Spine J. 2009 Oct;18(10):1532-40.
- ↑ Abu-Naser S., Almurshidi S. A knowledge based system for neck pain diagnosis. 2016. Department of Information Technology. Available from: http://dstore.alazhar.edu.ps/xmlui/handle/123456789/384. [accessed 4/3/2023]
- ↑ 8.0 8.1 Magee DJ. Orthopedic physical assessment 5th ed. St. Louis, Mo, Saunders Elsevier. 2008.
- ↑ 9.0 9.1 Childress MA, Becker BA. Nonoperative management of cervical radiculopathy. American family physician. 2016 May 1;93(9):746-54.
- ↑ Cooper G. Types of Neck Pain. Spine-Health. Available from: https://www.spine-health.com/conditions/neck-pain/types-neck-pain [accessed 5/3/2023]
- ↑ Corp N., Mansell G., Stynes S., Wynne-Jones G., Morsø L., Hill J., van der Windt D. Evidence-based treatment recommendations for neck and low back pain across Europe: A systematic review of guidelines. Eur J Pain 2021; 25;275-295.
- ↑ 12.0 12.1 Blanpied P., Gross A., Elliott J., Devaney L., Clewley D., Walton D., et al. Neck pain: revision 2017: clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association. JOSPT. 2017 Jul;47(7):A1-83.
- ↑ Rubinstein S., Pool J., van Tulder M., Riphagen I., de Vet HC. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J. 2007; 16(3): 307-19.
- ↑ Ramanayake RP, Basnayake BM. Evaluation of red flags minimizes missing serious diseases in primary care. Journal of family medicine and primary care. 2018 Mar;7(2):315.
- ↑ Trippolini M., Janssen S., Hilfiker R., Oesch P. Measurement properties of the modified spinal function sort (M-SFS): is it reliable and valid in workers with chronic musculoskeletal pain?. Journal of Occupational Rehabilitation. 2018 Jun;28(2):322-31.
- ↑ Kim R, Wiest C, Clark K, Cook C, Horn M. Identifying risk factors for first-episode neck pain: a systematic review. Musculoskeletal Science and Practice. 2018 Feb 1;33:77-83.
- ↑ Cerezo-Téllez E., Torres-Lacomba M., Fuentes-Gallardo I., Perez-Muñoz M., Mayoral-del-Moral O., Lluch-Girbés E., Prieto-Valiente L., Falla D. Effectiveness of dry needling for chronic nonspecific neck pain: a randomized, single-blinded, clinical trial. Pain. 2016 Sep 1;157(9):1905-17.
- ↑ Swedish Council on Health Technology Assessment. Laser Treatment of Neck Pain [Internet]. Stockholm: Swedish Council on Health Technology Assessment (SBU); 2014 May 20. SBU Alert Report No. 2014-03.
- ↑ Zronek M., Sanker H., Newcomb J., Donaldson M. The influence of home exercise programs for patients with non-specific or specific neck pain: a systematic review of the literature. J Manual Manipulative Ther. 2016 Mar 14;24(2):62-73.
- ↑ Paolucci T., Agostini F., Paoloni M., de Sire A., Verna S., Pesce M., Ribecco L., Mangone M., Bernetti A., Saggini R. Efficacy of TENS in Cervical Pain Syndromes: An Umbrella Review of Systematic Reviews. Applied Sciences. 2021 Jan;11(8):3423.
- ↑ Kroeling P., Gross A., Graham N., Burnie S., Szeto G., Goldsmith C., et al. Electrotherapy for neck pain. Cochrane database of systematic reviews. 2013 Aug 26;(8): CD004251.
- ↑ Paquin J., Tousignant-Laflamme Y., Dumas J. Effects of SNAG mobilization combined with a self-SNAG home-exercise for the treatment of cervicogenic headache: a pilot study. J Manual Manipulative Ther. 2021 Feb; 6:1-1.
- ↑ Borman P., Keskin D., Ekici B., Bodur H. The efficacy of intermittent cervical traction in patents with chronic neck pain. Clinical Rheumatology. 2008 Oct 1;27(10):1249-53.
- Interventions
- Cervical Spine - Interventions
- Clinical Guidelines
- Cervical Spine - Guidelines
- Thoracic Spine - Guidelines
- Cervical Spine
- Cervical Spine - Assessment and Examination
- Thoracic Spine
- Thoracic Spine - Interventions
- EBP
- Musculoskeletal/Orthopaedics
- MCG Student Project
- Nottingham University Spinal Rehabilitation Project