Muscle Injuries: Difference between revisions
No edit summary |
Rachael Lowe (talk | contribs) mNo edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''- [[User:Els Van Haver|Els Van Haver]] <br> | '''Original Editors '''- [[User:Els Van Haver|Els Van Haver]] <br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> <div align="justify"> | |||
== Introduction == | == Introduction == | ||
Skeletal [[muscle]] injuries represent great part of all traumas in sports medicine, with an incidence from 10% to 55% of all sustained injuries. They should be treated with necessary precaution since a failed treatment can postpone an athlete’s return to the field with weeks or even months and cause recidivism. | Skeletal [[muscle]] injuries represent great part of all traumas in sports medicine, with an incidence from 10% to 55% of all sustained injuries. They should be treated with necessary precaution since a failed treatment can postpone an athlete’s return to the field with weeks or even months and cause recidivism. | ||
</div> | </div> | ||
== Types of Skeletal Muscle Injuries == | == Types of Skeletal Muscle Injuries == | ||
<div align="justify"> | <div align="justify"> | ||
Literature study does not reveal great consensus when it comes to classifying muscle injuries, despite their clinical importance. However, the most differentiating factor is the trauma mechanism. Muscle injuries can therefore be broadly classified as either traumatic (acute) or overuse (chronic) injuries. | Literature study does not reveal great consensus when it comes to classifying muscle injuries, despite their clinical importance. However, the most differentiating factor is the trauma mechanism. Muscle injuries can therefore be broadly classified as either traumatic (acute) or overuse (chronic) injuries. | ||
''' | '''Acute''' injuries are usually the result of a single traumatic event and cause a macro-trauma to the muscle. There is an obvious link between the cause and noticeable symptoms. They mostly occur in contact sports such as rugby, soccer and basketball because of their dynamic and high collision nature<ref name="Eight" /><ref name="Twelve">Beiner J, Jokl P. Muscle Contusion Injuries: Current Treatment Options. J Am Acad Orthop Surg July 2001; 9:227-237</ref>. | ||
'''Overuse''', chronic or exercise-induced injuries are subtler and usually occur over a longer period of time. They result from repetitive micro-trauma to the muscle. Diagnosing is more challenging since there is a less obvious link between the cause of the injury and the symptoms<ref name="Eight">Best TM. Soft-tissue injuries and muscle tears. Clin Sports Med. Jul 1997; 16(3):419-34</ref>. The below video gives a brief talk on these chronic injuries. | |||
{{#ev:youtube|https://www.youtube.com/watch?v=EkdllXH5AME|width}}<ref>Universal Hospitals Common muscle and sports injuries Available from: https://www.youtube.com/watch?v=EkdllXH5AME (last accessed 7.6.2019)</ref> | |||
== Muscle Strains == | == Muscle Strains == | ||
[[File:Muscle-strain-grades.png|thumb]] | |||
A [[Muscle Strain|strain to the muscle]] or muscle [[Tendon Pathophysiology|tendon]] is the equivalent of a sprain to ligaments. It is a contraction-induced injury in which muscle fibres tear due to extensive mechanical stress. This mostly occurs as result of a powerful eccentric contraction or over-stretching of the muscle. Therefore, it is typical for non contact sports with dynamic character such as sprinting, jumping <ref name="Three">Garrett WE. Muscle strain injuries. Am J Sports Med. 1996; 24:S2-88</ref>. | |||
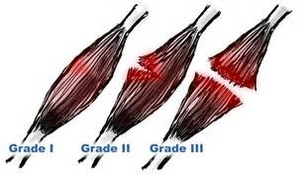
Strains are | Strains are categorised into 3 grades of severity<ref name="One">Tero AH Järvinen, Teppo LN Järvinen, Minna Kääriäinen, Hannu Kalimo, Markku Järvinen. Basic Science Update: Muscle Treatment. Am J Sports;May;33:745-&shy;‐764</ref><ref name="Six">Järvinen M, Tero AH. Muscle strain injuries. Rheumatology. 2010(2); 12: 155-161</ref><ref name="Nine">Kneeland JP. MR imaging of muscle and tendon injury. Eur J Radiol. Nov 1997; 25(3):198-208</ref>: | ||
'''Grade I '''(Mild) | '''Grade I '''(Mild) | ||
*Strains affect only a limited number of | *Strains affect only a limited number of fibres in the muscle. There is no decrease in strength and there is full active and passive range of motion. Pain and tenderness are often delayed to the next day. | ||
'''Grade II''' (Moderate) | '''Grade II''' (Moderate) | ||
*Strains have nearly half of muscle | *Strains have nearly half of muscle fibres torn. Acute and significant pain is accompanied by swelling and a minor decrease in muscle strength. Pain is reproduced on muscle contraction. | ||
'''Grade III''' (Severe) | '''Grade III''' (Severe) | ||
| Line 57: | Line 54: | ||
*[[Rotator Cuff Tears|Rotator Cuff Tears]] | *[[Rotator Cuff Tears|Rotator Cuff Tears]] | ||
*[[Rupture Long Head Biceps|Rupture Long Head Biceps]] | *[[Rupture Long Head Biceps|Rupture Long Head Biceps]] | ||
*[[Achilles Rupture|Achilles Rupture]] | *[[Achilles Rupture|Achilles Rupture]] | ||
== Muscle Contusion == | == Muscle Contusion == | ||
A bruise, or contusion, is a type of | A bruise, or [[Quadriceps Muscle Contusion|contusion]], is a type of haematoma of tissue in which capillaries and sometimes venules are damaged by trauma, allowing blood to seep, haemorrhage, or extravasate into the surrounding interstitial tissues. Bruises, which do not blanch under pressure, can involve capillaries at the level of skin, subcutaneous tissue, muscle, or bone. As a type of haematoma, a bruise is caused by internal bleeding into the interstitial tissues which does not break through the skin, usually initiated by blunt trauma, which causes damage through physical compression and deceleration forces. Trauma sufficient to cause bruising can occur across a wide range of sports. Bruises often induce pain, but small bruises are not normally dangerous alone. Sometimes bruises can be serious, leading to other more life-threatening forms of haematoma, such as when associated with serious injuries, including fractures and more severe internal bleeding. The likelihood and severity of bruising depends on many factors, including type and healthiness of affected tissues. | ||
== Muscle Cramp == | == Muscle Cramp == | ||
| Line 73: | Line 66: | ||
Muscle cramps during exercise are very common, even in elite athletes. Muscles that cramp the most often are the calves, thighs, and arches of the foot. Such cramping is associated with strenuous physical activity and can be intensely painful; however, they can even occur while inactive/relaxed. Around 40% of people who experience skeletal cramps are likely to endure extreme muscle pain, and may be unable to use the entire limb that contains the "locked-up" muscle group. It may take up to seven days for the muscle to return to a pain-free state. | Muscle cramps during exercise are very common, even in elite athletes. Muscles that cramp the most often are the calves, thighs, and arches of the foot. Such cramping is associated with strenuous physical activity and can be intensely painful; however, they can even occur while inactive/relaxed. Around 40% of people who experience skeletal cramps are likely to endure extreme muscle pain, and may be unable to use the entire limb that contains the "locked-up" muscle group. It may take up to seven days for the muscle to return to a pain-free state. | ||
According to Brukner & Kahn <ref name="CSM">Brukner P. Brukner & Khan's Clinical Sports Medicine. McGraw-Hill Education; 2017. </ref> disturbances at various levels of the central and peripheral nervous system and skeletal muscle are involved in the mechanism of cramp and may explain the diverse range of conditions in which cramp occurs. Other popular theories as to the cause of cramps include dehydration, low potassium or low sodium levels, inadequate carbohydrate intake or excessively tight muscles but these hypotheses appear to be falling out of | According to Brukner & Kahn<ref name="CSM">Brukner P. Brukner & Khan's Clinical Sports Medicine. McGraw-Hill Education; 2017. </ref> disturbances at various levels of the central and peripheral nervous system and skeletal muscle are involved in the mechanism of cramp and may explain the diverse range of conditions in which cramp occurs. Other popular theories as to the cause of cramps include dehydration, low potassium or low sodium levels, inadequate carbohydrate intake or excessively tight muscles but these hypotheses appear to be falling out of favour as the weight of evidence supports the ‘neural excitability’ hypothesis. | ||
== Muscle Soreness == | == Muscle Soreness == | ||
</div> | </div> | ||
==== '''Repair Process''' ==== | ==== '''Repair Process''' ==== | ||
<div align="justify" | <div align="justify"> | ||
Regardless the underlying cause, the processes occurring in injured muscles tend to follow the same pattern. Functional recovery however varies from one type of injury to another. Two phases can be distinguished in the repair process | Regardless the underlying cause, the processes occurring in injured muscles tend to follow the same pattern. Functional recovery however varies from one type of injury to another. Two phases can be distinguished in the repair process<ref name="One" /><ref name="Two">Kalimo H, Rantanen J, Järvinen M. Muscle injuries in sports. Baillieres Clin Orthop. 1997;2: 1-24</ref><ref name="Seven">Huard J, Li Y, Fu FH. Muscle injuries and repair: Current trends in research. J Bone Joint Surg AM. 2002; 84:822-832</ref>. | ||
'''Destruction Phase''' | '''Destruction Phase''' | ||
Starts with the actual trauma that causes muscle | Starts with the actual trauma that causes muscle fibres to tear. Immediate necrosis of myofibres takes place due to deterioration of the sarcoplasm, a process that is halted within hours after the trauma by lysosomal vesicles forming a temporary membrane<ref name="Nine" />. An inflammatory process takes place as a reaction on the torn blood vessels. Specialised cells start removing necrotised parts of the fibres<ref name="Ten">Kasemkijwattana C, Menetrey J, Somogyl G, et al. Development of approaches to improve the healing following muscle contusion. Cell Transplant. Nov-Dec 1998; 7(6):585-98</ref>. | ||
'''Repair and | '''Repair and Remodelling Phase''' | ||
The actual repair of the injured muscle takes place. | The actual repair of the injured muscle takes place. Myofibres start regenerating out of satellite cells (= undifferentiated reserve cells) and a connective tissue scar is being formed in the gap between the torn muscle fibres. In the first 10 days after the trauma, this scar tissue is the weakest point of the affected muscle. After 10 days however, eventual re-rupture will rather affect adjacent muscle tissue than the scar tissue itself, although full recovery (up to the point of pre-injury strength) can take a relatively long time. Vascularisation of the injured area is a prerequisite for recovering from a muscle injury. New capillaries originate from the remaining injured blood vessels and find their way to the centre of the injured area. Early mobilisation plays a very important role since it stimulates the vascularisation process. Similar wise, intramuscular nerves will regenerate to re-establish the nerve-muscle contact<ref name="Five">Järvinen M, Sorvari T. A histochemical study of the effect of mobilization and immobilization on the metabolism of healing muscle injury. In: Landry F, ed. Sports Medicine. Miami, Fla: Symposia Specialists, Orban WAR; 1978:177-181</ref><ref name="Eleven">Nozaki M, Li Y, Zhu J, et al. Improved muscle healing after contusion injury by the inhibitory effect of suramin on myostatin, a negative regulator of muscle growth. Am J Sports Med Dec 2008; 36(12): 2354-62</ref>. | ||
</div> | </div> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 98: | Line 91: | ||
==== Acute Skeletal Muscle Injuries ==== | ==== Acute Skeletal Muscle Injuries ==== | ||
<div align="justify"> | <div align="justify">The [[POLICE Principle|POLICE]] '''principle (an updated version of [[RICE]]'''-principle) is generally considered as being the best method to minimise swelling and relief pain within the first 24 to 48 hours. Although the different components of the RICE-principle have each shown their effectiveness in experimental studies, the use of the all-round concept is yet to be proved in randomised clinical trials<ref name="One" />. | ||
After first aid, therapy must be tailor made according to the severity and extent of the injury. A short period of '''immobilisation''' after the trauma prevents excessive formation of scar tissue (which will have a deleterious effect on mobility and strength of the healed muscle) and prevents re-rupture by allowing the scar tissue to gain sufficient strength to bear contraction forces. Immobilisation should not be continued after the acute phase (first few days) to avoid the negative effects such as muscle atrophy, retarded strength recovery and excessive formation of connective tissue within the muscle<ref name="Five" />. | |||
Early '''mobilisation''' already starts after a few days, if the acute phase has passed without further complications and recovery seems to be progressing. In comparison to immobilisation, mobilisation induces significant histological changes such as increased vascularisation of the injured area, better regeneration of muscle fibres and more parallel orientation. It has the additional advantage that the muscle will sooner gain its original strength<ref name="One" /><ref name="Four">Järvinen M, Lehto MUK. The effect of early mobilization and immobilization on the healing process following muscle injuries. Sports Med. 1993; 15:78-89</ref><ref name="Six" />. | |||
Early ''' | |||
The active treatment needs to be built up gradually from isometric exercises to isotonic exercises. Only if those exercises can be performed without pain, isokinetic training should be started. | The active treatment needs to be built up gradually from isometric exercises to isotonic exercises. Only if those exercises can be performed without pain, isokinetic training should be started. | ||
As muscle injuries generally recover well with conservative treating, '''surgical intervention''' is only to be considered in cases with very specific indications | As muscle injuries generally recover well with conservative treating, '''surgical intervention''' is only to be considered in cases with very specific indications<ref name="One" />: | ||
* Large intramuscular haematoma | |||
*Large intramuscular | * Complete muscle tear (strain of third degree) | ||
* Partial strain (2<sup>nd</sup> degree) if more than half of the muscle belly is affected | |||
*Complete muscle tear (strain of third degree) | * Scar adhesions that cause persistent pain and limited extension (>4-6 months) | ||
</div> | |||
*Partial strain (2<sup>nd</sup> degree) if more than half of the muscle belly is affected | |||
*Scar adhesions that cause persistent pain and limited extension (>4-6 months)</div> | |||
==== '''Chronic Skeletal Muscle Injuries''' ==== | ==== '''Chronic Skeletal Muscle Injuries''' ==== | ||
<div align="justify"> | <div align="justify"> | ||
Overuse sports injuries outnumber acute, instantaneous injuries in almost every athletic activity. Because they don't not instantly, disabling the person, they attract less medical attention than acute injuries. Their frequency of occurrence is almost always underestimated in surveys of athletic injuries. The treatment of overuse sports injuries is made difficult by various factors eg an insidious onset. When athletes actually present for treatment, the injuries are well established and more difficult to manage successfully. | Overuse sports injuries outnumber acute, instantaneous injuries in almost every athletic activity. Because they don't not instantly, disabling the person, they attract less medical attention than acute injuries. Their frequency of occurrence is almost always underestimated in surveys of athletic injuries. The treatment of overuse sports injuries is made difficult by various factors eg an insidious onset. When athletes actually present for treatment, the injuries are well established and more difficult to manage successfully. | ||
Injury occurs when cumulative forces exceed the tissue’s ability to withstand such forces— either due to isolated macrotraumatic events or repetitive | Injury occurs when cumulative forces exceed the tissue’s ability to withstand such forces— either due to isolated macrotraumatic events or repetitive micro-traumatic events. Often, specific biomechanical or physiological factors predispose an athlete to injury. A physiotherapist should properly identify and assist the athlete in correcting these conditions to treat, prevent, and possibly reverse the detrimental effects. As always, prevention is always the best treatment but, failing that, the next best thing is proper and successful rehabilitation.<ref>Elmer G. Pinzon, MD, MPH, DABIPP and Mick Larrabee, PT, MS, SCS, EMT, CSCS [https://www.practicalpainmanagement.com/pain/acute/sports-overuse/chronic-overuse-sports-injuries Chronic Overuse Sports Injuries] Available from: https://www.practicalpainmanagement.com/pain/acute/sports-overuse/chronic-overuse-sports-injuries (last accessed 7.6.2019)</ref> | ||
</div> | </div> | ||
==== '''Clinical Bottom Line''' ==== | ==== '''Clinical Bottom Line''' ==== | ||
<div align="justify"> | <div align="justify"> | ||
Treatment of muscle injuries usually have good outcomes. Physiotherapists must ensure the muscle is rehabilitated in all functional aspects before resuming usual activities or high demand sporting activities. | Treatment of muscle injuries usually have good outcomes. Physiotherapists must ensure the muscle is rehabilitated in all functional aspects before resuming usual activities or high demand sporting activities. | ||
</div> | </div> | ||
Revision as of 10:32, 10 June 2019
Original Editors - Els Van Haver
Top Contributors - Els Van Haver, Naomi O'Reilly, Wanda van Niekerk, Kim Jackson, Lucinda hampton, Vidya Acharya, Nina Lefeber, Evan Thomas, Admin, Uchechukwu Chukwuemeka, Mande Jooste, Jess Bell, Maxime Tuerlinckx, Claire Knott, 127.0.0.1 and Rachael Lowe
Introduction[edit | edit source]
Skeletal muscle injuries represent great part of all traumas in sports medicine, with an incidence from 10% to 55% of all sustained injuries. They should be treated with necessary precaution since a failed treatment can postpone an athlete’s return to the field with weeks or even months and cause recidivism.
Types of Skeletal Muscle Injuries[edit | edit source]
Literature study does not reveal great consensus when it comes to classifying muscle injuries, despite their clinical importance. However, the most differentiating factor is the trauma mechanism. Muscle injuries can therefore be broadly classified as either traumatic (acute) or overuse (chronic) injuries.
Acute injuries are usually the result of a single traumatic event and cause a macro-trauma to the muscle. There is an obvious link between the cause and noticeable symptoms. They mostly occur in contact sports such as rugby, soccer and basketball because of their dynamic and high collision nature[1][2].
Overuse, chronic or exercise-induced injuries are subtler and usually occur over a longer period of time. They result from repetitive micro-trauma to the muscle. Diagnosing is more challenging since there is a less obvious link between the cause of the injury and the symptoms[1]. The below video gives a brief talk on these chronic injuries.
[3]Muscle Strains[edit | edit source]
A strain to the muscle or muscle tendon is the equivalent of a sprain to ligaments. It is a contraction-induced injury in which muscle fibres tear due to extensive mechanical stress. This mostly occurs as result of a powerful eccentric contraction or over-stretching of the muscle. Therefore, it is typical for non contact sports with dynamic character such as sprinting, jumping [4].
Strains are categorised into 3 grades of severity[5][6][7]:
Grade I (Mild)
- Strains affect only a limited number of fibres in the muscle. There is no decrease in strength and there is full active and passive range of motion. Pain and tenderness are often delayed to the next day.
Grade II (Moderate)
- Strains have nearly half of muscle fibres torn. Acute and significant pain is accompanied by swelling and a minor decrease in muscle strength. Pain is reproduced on muscle contraction.
Grade III (Severe)
- Strains represent complete rupture of the muscle. This means either the tendon is separated from the muscle belly or the muscle belly is actually torn in 2 parts. Severe swelling and pain and a complete loss of function are characteristic for this type of strain. Th is is seen most frequently at the musculotendinous junction.
A number of factors predispose an athlete to muscle strains:
- Inadequate Warm-up
- Insufficient Joint Range of Motion
- Excessive Muscle Tightness
- Fatigue / Overuse / Inadequate Recovery
- Muscle Imbalance
- Previous Injury
- Faulty Technique / Biomechanics
- Spinal Dysfunction
Common Strain Injuries:
- Hamstring Strain
- Quadriceps Muscle Contusion
- Calf Strain
- Groin strain
- Rotator Cuff Tears
- Rupture Long Head Biceps
- Achilles Rupture
Muscle Contusion[edit | edit source]
A bruise, or contusion, is a type of haematoma of tissue in which capillaries and sometimes venules are damaged by trauma, allowing blood to seep, haemorrhage, or extravasate into the surrounding interstitial tissues. Bruises, which do not blanch under pressure, can involve capillaries at the level of skin, subcutaneous tissue, muscle, or bone. As a type of haematoma, a bruise is caused by internal bleeding into the interstitial tissues which does not break through the skin, usually initiated by blunt trauma, which causes damage through physical compression and deceleration forces. Trauma sufficient to cause bruising can occur across a wide range of sports. Bruises often induce pain, but small bruises are not normally dangerous alone. Sometimes bruises can be serious, leading to other more life-threatening forms of haematoma, such as when associated with serious injuries, including fractures and more severe internal bleeding. The likelihood and severity of bruising depends on many factors, including type and healthiness of affected tissues.
Muscle Cramp[edit | edit source]
Sudden, involuntary muscle contraction or over-shortening; while generally temporary and non-damaging, they can cause mild-to-excruciating pain, and a paralysis-like immobility of the affected muscle(s). Onset is usually sudden, and it resolves on its own over a period of several seconds, minutes, or hours. Cramps may occur in a skeletal muscle or smooth muscle. Skeletal muscle cramps may be caused by muscle fatigue or a lack of electrolytes (e.g., low sodium, low potassium, or low magnesium).
Muscle cramps during exercise are very common, even in elite athletes. Muscles that cramp the most often are the calves, thighs, and arches of the foot. Such cramping is associated with strenuous physical activity and can be intensely painful; however, they can even occur while inactive/relaxed. Around 40% of people who experience skeletal cramps are likely to endure extreme muscle pain, and may be unable to use the entire limb that contains the "locked-up" muscle group. It may take up to seven days for the muscle to return to a pain-free state.
According to Brukner & Kahn[8] disturbances at various levels of the central and peripheral nervous system and skeletal muscle are involved in the mechanism of cramp and may explain the diverse range of conditions in which cramp occurs. Other popular theories as to the cause of cramps include dehydration, low potassium or low sodium levels, inadequate carbohydrate intake or excessively tight muscles but these hypotheses appear to be falling out of favour as the weight of evidence supports the ‘neural excitability’ hypothesis.
Muscle Soreness[edit | edit source]
Repair Process[edit | edit source]
Regardless the underlying cause, the processes occurring in injured muscles tend to follow the same pattern. Functional recovery however varies from one type of injury to another. Two phases can be distinguished in the repair process[5][9][10].
Destruction Phase
Starts with the actual trauma that causes muscle fibres to tear. Immediate necrosis of myofibres takes place due to deterioration of the sarcoplasm, a process that is halted within hours after the trauma by lysosomal vesicles forming a temporary membrane[7]. An inflammatory process takes place as a reaction on the torn blood vessels. Specialised cells start removing necrotised parts of the fibres[11].
Repair and Remodelling Phase
The actual repair of the injured muscle takes place. Myofibres start regenerating out of satellite cells (= undifferentiated reserve cells) and a connective tissue scar is being formed in the gap between the torn muscle fibres. In the first 10 days after the trauma, this scar tissue is the weakest point of the affected muscle. After 10 days however, eventual re-rupture will rather affect adjacent muscle tissue than the scar tissue itself, although full recovery (up to the point of pre-injury strength) can take a relatively long time. Vascularisation of the injured area is a prerequisite for recovering from a muscle injury. New capillaries originate from the remaining injured blood vessels and find their way to the centre of the injured area. Early mobilisation plays a very important role since it stimulates the vascularisation process. Similar wise, intramuscular nerves will regenerate to re-establish the nerve-muscle contact[12][13].
Diagnostic Procedures[edit | edit source]
Both for acute and chronic injuries, thorough anamnesis is primary in identifying muscle injuries. Particular attention for the history of occurrence of the trauma is needed. A clinical examination and testing of the muscle function together with the anamnesis are mostly sufficient for making the right diagnosis. In some cases, additional tests (MRI, X-ray, Ultrasound, CT Scan) may be required to determine the extent of the injury or to identify possible additional injuries.
The video below gives a good insight into diagnostic procedures for muscle injuries[14]Physiotherapy Treatment[edit | edit source]
Acute Skeletal Muscle Injuries[edit | edit source]
After first aid, therapy must be tailor made according to the severity and extent of the injury. A short period of immobilisation after the trauma prevents excessive formation of scar tissue (which will have a deleterious effect on mobility and strength of the healed muscle) and prevents re-rupture by allowing the scar tissue to gain sufficient strength to bear contraction forces. Immobilisation should not be continued after the acute phase (first few days) to avoid the negative effects such as muscle atrophy, retarded strength recovery and excessive formation of connective tissue within the muscle[12].
Early mobilisation already starts after a few days, if the acute phase has passed without further complications and recovery seems to be progressing. In comparison to immobilisation, mobilisation induces significant histological changes such as increased vascularisation of the injured area, better regeneration of muscle fibres and more parallel orientation. It has the additional advantage that the muscle will sooner gain its original strength[5][15][6].
The active treatment needs to be built up gradually from isometric exercises to isotonic exercises. Only if those exercises can be performed without pain, isokinetic training should be started.
As muscle injuries generally recover well with conservative treating, surgical intervention is only to be considered in cases with very specific indications[5]:
- Large intramuscular haematoma
- Complete muscle tear (strain of third degree)
- Partial strain (2nd degree) if more than half of the muscle belly is affected
- Scar adhesions that cause persistent pain and limited extension (>4-6 months)
Chronic Skeletal Muscle Injuries[edit | edit source]
Overuse sports injuries outnumber acute, instantaneous injuries in almost every athletic activity. Because they don't not instantly, disabling the person, they attract less medical attention than acute injuries. Their frequency of occurrence is almost always underestimated in surveys of athletic injuries. The treatment of overuse sports injuries is made difficult by various factors eg an insidious onset. When athletes actually present for treatment, the injuries are well established and more difficult to manage successfully.
Injury occurs when cumulative forces exceed the tissue’s ability to withstand such forces— either due to isolated macrotraumatic events or repetitive micro-traumatic events. Often, specific biomechanical or physiological factors predispose an athlete to injury. A physiotherapist should properly identify and assist the athlete in correcting these conditions to treat, prevent, and possibly reverse the detrimental effects. As always, prevention is always the best treatment but, failing that, the next best thing is proper and successful rehabilitation.[16]
Clinical Bottom Line[edit | edit source]
Treatment of muscle injuries usually have good outcomes. Physiotherapists must ensure the muscle is rehabilitated in all functional aspects before resuming usual activities or high demand sporting activities.
References[edit | edit source]
- ↑ 1.0 1.1 Best TM. Soft-tissue injuries and muscle tears. Clin Sports Med. Jul 1997; 16(3):419-34
- ↑ Beiner J, Jokl P. Muscle Contusion Injuries: Current Treatment Options. J Am Acad Orthop Surg July 2001; 9:227-237
- ↑ Universal Hospitals Common muscle and sports injuries Available from: https://www.youtube.com/watch?v=EkdllXH5AME (last accessed 7.6.2019)
- ↑ Garrett WE. Muscle strain injuries. Am J Sports Med. 1996; 24:S2-88
- ↑ 5.0 5.1 5.2 5.3 5.4 Tero AH Järvinen, Teppo LN Järvinen, Minna Kääriäinen, Hannu Kalimo, Markku Järvinen. Basic Science Update: Muscle Treatment. Am J Sports;May;33:745-­‐764
- ↑ 6.0 6.1 Järvinen M, Tero AH. Muscle strain injuries. Rheumatology. 2010(2); 12: 155-161
- ↑ 7.0 7.1 Kneeland JP. MR imaging of muscle and tendon injury. Eur J Radiol. Nov 1997; 25(3):198-208
- ↑ Brukner P. Brukner & Khan's Clinical Sports Medicine. McGraw-Hill Education; 2017.
- ↑ Kalimo H, Rantanen J, Järvinen M. Muscle injuries in sports. Baillieres Clin Orthop. 1997;2: 1-24
- ↑ Huard J, Li Y, Fu FH. Muscle injuries and repair: Current trends in research. J Bone Joint Surg AM. 2002; 84:822-832
- ↑ Kasemkijwattana C, Menetrey J, Somogyl G, et al. Development of approaches to improve the healing following muscle contusion. Cell Transplant. Nov-Dec 1998; 7(6):585-98
- ↑ 12.0 12.1 Järvinen M, Sorvari T. A histochemical study of the effect of mobilization and immobilization on the metabolism of healing muscle injury. In: Landry F, ed. Sports Medicine. Miami, Fla: Symposia Specialists, Orban WAR; 1978:177-181
- ↑ Nozaki M, Li Y, Zhu J, et al. Improved muscle healing after contusion injury by the inhibitory effect of suramin on myostatin, a negative regulator of muscle growth. Am J Sports Med Dec 2008; 36(12): 2354-62
- ↑ Chris Beaulieu Muscle injuries and interventions. Available from: https://www.youtube.com/watch?v=MPqjFEhEBB4&app=desktop (last accessed 7.6.2019)
- ↑ Järvinen M, Lehto MUK. The effect of early mobilization and immobilization on the healing process following muscle injuries. Sports Med. 1993; 15:78-89
- ↑ Elmer G. Pinzon, MD, MPH, DABIPP and Mick Larrabee, PT, MS, SCS, EMT, CSCS Chronic Overuse Sports Injuries Available from: https://www.practicalpainmanagement.com/pain/acute/sports-overuse/chronic-overuse-sports-injuries (last accessed 7.6.2019)