Metatarsalgia: Difference between revisions
No edit summary |
No edit summary |
||
| (31 intermediate revisions by 7 users not shown) | |||
| Line 3: | Line 3: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition == | == Definition == | ||
[[File:Metatarsalgia.jpg|435x435px|<ref>https://greenbayacupuncture.co/2017/05/17/metatarsalgia-forefoot-pain/</ref>|right|frameless]] | |||
[[File:Metatarsal bone animation01.gif|right|frameless]] | |||
Metatarsalgia is a general term for [[Pain Behaviours|pain]] in the area of the metatarsophalangeal joints. This is often seen in clinical practice, the deformity and pain can deteriorate gait function and decrease quality of life<ref name=":5">Park CH, Chang MC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6784640/ Forefoot disorders and conservative treatment.] Yeungnam University Journal of Medicine. 2019 May;36(2):92.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6784640/ (last accessed 25.6.2020)</ref>. | |||
Most common causes include: | |||
* Interdigital nerve pain ([[Morton's Neuroma|Morton]] neuroma) | |||
* Metatarsophalangeal joint pain | |||
* [[Sesamoiditis]] | |||
* Submetatarsal head fat pad atrophy typically associated with [[Older People - An Introduction|aging]]<ref name=":4">Mercks manual. [https://www.merckmanuals.com/professional/musculoskeletal-and-connective-tissue-disorders/foot-and-ankle-disorders/metatarsophalangeal-joint-pain MTP joint pain] Available from:https://www.merckmanuals.com/professional/musculoskeletal-and-connective-tissue-disorders/foot-and-ankle-disorders/metatarsophalangeal-joint-pain (last accessed 25.6.2020)</ref> | |||
Metatarsalgies are often accompanied by excessive callus formation over a bony protrusion, with severe pain and pressure sensitivity around the callus.<ref>Doty, Jesse F., and Michael J. Coughlin. "Metatarsophalangeal joint instability of the lesser toes." The Journal of Foot and Ankle Surgery 53.4 (2014): 440-445. | |||
</ref><ref name=":1">Espinosa, Norman, Ernesto Maceira, and Mark S. Myerson. "Current concept review: | |||
metatarsalgia." Foot & ankle international 29.8 (2008) </ref> | |||
[[File:Metatarsals .jpg|324x324px|Metatarsals of the Right foot|right|frameless]] | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
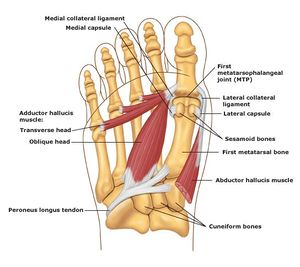
The most important and relevant anatomy is the | The most important and relevant anatomy is the forefoot and the metatarsal. The metatarsus of the [[Foot Anatomy|foot]] consists of five long [[Bone|bones]], which are called the metatarsals. | ||
Metatarsals: | |||
* Comprised of: proximal base; shaft; distal head. | |||
* Proximally connected to the tarsal bones and distally to the phalanges. | |||
* Named I to V medially to laterally, from the dorsal surface of the foot. | |||
* Convex on their dorsal surfaces but concave on their plantar surfaces | |||
* Along with the tarsals, help form the [[Arches of the Foot|arches of the foot]], which are essential in both weight-bearing and walking.<ref name=":3">https://www.kenhub.com/en/library/anatomy/metatarsal-bones</ref> | |||
The joints between the head of the metatarsals and the respective proximal phalanx are called the metatarsophalangeal joint (MTP). | |||
* These joints form the ball of the foot, and the ability to move in these joints is very important for normal walking. | |||
* In addition, the bases of the metatarsals articulate with each other to form intermetatarsal joints.<ref name=":3" /> | |||
== Etiology == | |||
Common causes include: | |||
* Overtraining | |||
* Interdigital ([[Morton's Neuroma|Morton]]) neuroma | |||
* Freiberg infraction | |||
*[[File:Foot 1.jpg|right|frameless]]Stress fractures involving the foot | |||
* Intermetatarsal bursitis | |||
* Adventitial bursitis | |||
* Inflammatory and degenerative arthritis | |||
* Metatarsophalangeal joint synovitis/capsulitis | |||
* Tendinosis/tenosynovitis | |||
* Plantar plate disruption / plantar plate tears | |||
* Schwannoma<ref>Radiopedia [https://radiopaedia.org/articles/metatarsalgia Metatarsalgia] Available from:https://radiopaedia.org/articles/metatarsalgia (last accessed 25.6.2020)</ref> | |||
* [[Pes cavus]] or high arched foot | |||
* Excessive pronation of the foot | |||
* Clawing or hammer toes | |||
* Tight extensor tendons of the toes | |||
* Prominent metatarsal heads | |||
* Morton’s foot—there is a shortened first metatarsal, which results in an abnormal subtalar joint, and increased weight going through the second metatarsophalangeal joint.<ref name=":0">Brukner P. Brukner & Khan's clinical sports medicine. North Ryde: McGraw-Hill; 2012.</ref> | |||
== | == Causes == | ||
[[File:Hallux valgus anatomy.jpg|right|frameless]]There can be multiple causative factors. Often localized to the first metatarsal head.Next most frequent site of metatarsal head pain is under the second metatarsal.<ref name=":1" /><ref name=":2">G. McPoil Thomas and Schuit Dale. “Management of metatarsalgia secondary to | |||
biomechanical disorders”. Physical Therapy 66(6): 970-2; July 1986 </ref><ref>Sobel Ellen, D.P.M., Ph. D., C.PED. and Levitz Steven, D.P.M.; “Metatarsalgia : Diagnosis | |||
and Manangement, Etiologies and Differential diagnoses”. Podiatry Management </ref> | |||
Factors that can cause excessive pressure are: | |||
*Participating in high impact activities without proper footwear and/or [[Introduction to Orthotics|orthotics]] | |||
*[[Older People - An Introduction|Older age]] as the pad in the foot tends to thin out making it much more susceptible pressue and pain | |||
*Participating in high impact activities without proper footwear and/or orthotics | |||
*Older age as the pad in the foot tends to thin out making it much more susceptible pressue and pain | |||
*An imbalance in the length of the metatarsals | *An imbalance in the length of the metatarsals | ||
*Disturbances in gait | *Majority seem to be related to foot and [[Ankle & Foot|ankle]] deformity | ||
*Disturbances in [[gait]] | |||
*Morphology of the foot (e.g. increased bone length that protrudes into the bottom of the foot) | *Morphology of the foot (e.g. increased bone length that protrudes into the bottom of the foot) | ||
*A shortened [http://www.physio-pedia.com/index.php5?title=Achilles_tendon_repair Achilles tendon] | *A shortened [http://www.physio-pedia.com/index.php5?title=Achilles_tendon_repair Achilles tendon] | ||
=== Subtypes === | |||
*'''Primary metatarsalgia''' refers to symptoms arising from innate abnormalities in the patient’s anatomy leading to overload of the affected metatarsal. <ref name="p2">Espinosa, Norman, Ernesto Maceira, and Mark S. Myerson. "Current concept review: metatarsalgia." Foot & ankle international 29.8 (2008)</ref> | |||
*'''Secondairy metatarsalgia''' can be caused by systemic conditions such as [[arthritis]] of the MTP joint. | |||
*'''Iatrogenic metatarsalgia''' can occur after (failed) reconstructive surgery. | |||
*'''Primary metatarsalgia''' refers to symptoms arising from innate abnormalities in the patient’s anatomy leading to overload of the affected metatarsal | |||
*'''Secondairy metatarsalgia''' can be caused by systemic conditions such as arthritis of the MTP joint. | |||
*'''Iatrogenic metatarsalgia''' can occur after (failed) reconstructive surgery. | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
# Metatarsalgia most commonly results from misalignment of the joint surfaces with altered foot biomechanics, may cause | |||
Metatarsalgia | #* Joint subluxations, | ||
#* Flexor plate tears (a fibrocartilaginous structure that lies directly plantar to the lesser metatarsal heads and acts as a sesamoid-like mechanism for each lesser joint (MPJ) of the foot<ref>Podiatry today [https://www.podiatrytoday.com/understanding-biomechanics-plantar-plate-injuries Understanding PP injuries] Available from:https://www.podiatrytoday.com/understanding-biomechanics-plantar-plate-injuries (last accessed 25.6.2020)</ref>) | |||
#* Increased pain during the mid-stance and propulsion phases of walking as body weight is shifted forward onto the forefoot.<ref>G. McPoil Thomas and Schuit Dale. “Management of metatarsalgia secondary to biomechanical disorders”. Physical Therapy 66(6): 970-2; July 1986</ref> | |||
#* Capsular impingement | |||
#* Joint [[cartilage]] destruction (osteoarthrosis). | |||
#* Misaligned joints synovial impingement, with minimal if any heat and swelling (osteoarthritic synovitis). | |||
*Increased pain during the mid-stance and propulsion phases of walking as body weight is shifted forward onto the forefoot.<ref>G. McPoil Thomas and Schuit Dale. “Management of metatarsalgia secondary to biomechanical disorders”. Physical Therapy 66(6): 970-2; July 1986</ref> | #* Metatarsophalangeal joint subluxation - May occur as a result of chronic inflammatory arthropathy, particularly [[Rheumatoid Arthritis|rheumatoid arthritis]] (RA) | ||
#* Metatarsophalangeal joint pain - weight bearing and a sense of stiffness in the morning. | |||
#* Loss of metatarsal fat pad (usually cushions the stress between the metatarsals and interdigital nerves during walking) tends to move distally under the toes, causing interdigital neuralgia/Morton neuroma. | |||
#* To compensate for the loss of cushioning, adventitial calluses and bursae may develop. | |||
#* Coexisting rheumatoid nodules beneath or near the plantarflexed metatarsal heads may increase pain.<br>The 2nd metatarsophalangeal joint is most commonly affected. | |||
#* Usually, inadequate 1st ray (1st cuneiform and 1st metatarsal) function results from excessive pronation (the foot rolling inward and the hindfoot turning outward or everted), often leading to capsulitis and hammer toe deformities. | |||
#* Overactivity of the anterior shin muscles in patients with [[pes cavus]] (high arch) and ankle equinus (shortened Achilles tendon that restricts ankle dorsiflexion) deformities tends to cause dorsal joint subluxations with retracted (clawed) digits and retrograde, increased submetatarsal head pressure and pain<ref name=":4" />.[[File:Hallux rigidus XR.jpg|right|frameless]] | |||
#Metatarsophalangeal joint pain may also result from functional [[Hallux Rigidus|hallux limitus]] (see xray R) | |||
#* Limits passive and active joint motion at the 1st metatarsophalangeal joint. | |||
#* Patients usually have foot pronation disorders that result in elevation of the 1st ray with lowering of the medial longitudinal arch during weight bearing. | |||
#* As a result of the 1st ray elevation, the proximal phalanx of the great toe cannot freely extend on the 1st metatarsal head; the result is jamming at the dorsal joint leading to osteoarthritic changes and loss of joint motion (with time, pain may develop). | |||
#Another cause of 1st metatarsophalangeal joint pain due to limited motion is direct trauma with stenosis of the flexor hallucis brevis, usually occurring within the tarsal tunnel. If pain is chronic, the joint may become less mobile with an arthrosis (hallux rigidus), which can be debilitating. | |||
#Acute arthritis can occur secondary to systemic arthritides such as [[gout]], RA, and [[Spondyloarthropathy--AS|spondyloarthropathy]].<ref name=":4" /> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
#[http://www.physio-pedia.com/Plantarfasciitis Plantar fasciitis] | #[http://www.physio-pedia.com/Plantarfasciitis Plantar fasciitis] | ||
#[http://www.physio-pedia.com/Morton's_Toe Morton's toe] | #[http://www.physio-pedia.com/Morton's_Toe Morton's toe] | ||
#[http://www.physio-pedia.com/RA_(Rheumatoid_Arthritis) Systemic Arthtritis] | #[http://www.physio-pedia.com/RA_(Rheumatoid_Arthritis) Systemic Arthtritis] | ||
= | === Diagnostic Procedures === | ||
* Mainly clinical evaluation | |||
* Exclusion of infection or arthropathy if signs of inflammation | |||
== Diagnostic Procedures == | * To differentiate one diagnosis from another, the use of the patient’s history, physical exam, roentgenograms, cholesterol-crystal force-plate analysis, intra-articular/digital injections, and additional laboratory studies (electromyography, arteriograms, venograms,..) can be used.<ref>J Bone Joint Surg Am. 1980 Jul;62(5):723-32. Scranton PE Jr; Metatarsalgia: diagnosis and treatment</ref> | ||
* Investigations - [[X-Rays|X-rays]] can be performed to assess the degree of degeneration of the joint. | |||
To differentiate one diagnosis from another, the use of the patient’s history, physical exam, roentgenograms, cholesterol-crystal force-plate analysis, intra-articular/digital injections and additional laboratory studies (electromyography, arteriograms, venograms,..) can be used.<ref>J Bone Joint Surg Am. 1980 Jul;62(5):723-32. Scranton PE Jr; Metatarsalgia: diagnosis and treatment</ref> | |||
== Outcome Measures == | == Outcome Measures == | ||
*[http://www.physio-pedia.com/Foot_Function_Index_(FFI) Foot Function Index (FFI)] - The Brazilian-Portuguese version of the FFI questionnaire was found to be a valid and reliable instrument for foot function evaluation, and can be used both in scientific settings and in clinical practice. | *[http://www.physio-pedia.com/Foot_Function_Index_(FFI) Foot Function Index (FFI)] - The Brazilian-Portuguese version of the FFI questionnaire was found to be a valid and reliable instrument for foot function evaluation, and can be used both in scientific settings and in clinical practice.<ref name="Martinez 2016">Martinez, Bruna Reclusa, et al. Validity and reliability of the Foot Function Index (FFI) questionnaire Brazilian-Portuguese version. 2016.</ref> | ||
*[[Foot Posture Index (FP1-6)|Foot Posture Index]] (FP1-6) - No scientific evidence found correlated to metarsalgia<ref name="Haque 2015">Haque, Syed, et al. Outcome of Minimally Invasive Distal Metatarsal Metaphyseal Osteotomy (DMMO) for Lesser Toe Metatarsalgia. Foot & Ankle International. 2015.</ref> | |||
* | |||
== Medical Management == | == Medical Management == | ||
Orthotics : | |||
*[[File:Pointed toe box.jpg|right|frameless|182x182px]]Foot orthoses with metatarsal pads may help redistribute and relieve pressure from the noninflamed joints. | |||
* With excess subtalar eversion or when the feet are highly arched, an orthotic that corrects these abnormal alignments should be prescribed. | |||
* Shoes with rocker sole modifications may also help. | |||
* For functional hallux limitus, orthosis modifications may further help to plantarflex the 1st ray to improve metatarsophalangeal joint motion and reduce pain. | |||
* If the 1st ray elevation cannot be reduced by these means, an extended 1st ray elevation pad may be helpful. | |||
* For more severe limitation of 1st metatarsophalangeal motion or pain, the use of rigid orthoses, carbon fiber plates, or external shoe bars or rocker soles may be necessary to reduce motion at the joint.<ref name=":4" /> | |||
Surgery may be needed if conservative therapies are ineffective. If inflammation (synovitis) is present, injection of a local corticosteroid/anesthetic mixture may be useful. | |||
[[NSAIDs in the Management of Rheumatoid Arthritis|NSAIDS]] are most commonly used for the relief of mild to moderate pain. But you have to use the right shoes.<ref name=":2" />, | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
For the management of these disorders, physiotherapy treatment is usually attempted prior to surgical intervention. | |||
Physiotherapy Treatments include - education, orthoses & corrective shoes, stretching of specific lower limb muscles, small foot strengthening exercises, | |||
# Education | |||
#* Initially reducing or stopping exercise, substitute a non WB exercise eg pool running, cycling. | |||
#* Suspend training until the pain begins to subside | |||
#* Once client ready to exercise/walk again avoid future injury by educating re appropriate footwear | |||
#* Pain relief and apply ice packs to the affected area (pain-killers that contain anti-inflammatories to help reduce any swelling). Swelling can also be reduced by elevating feet. | |||
#[[Foot Orthoses|Orthoses]] | |||
#* For symptomatic relief, an MT pad made of rubber, polyurethane, or silicone can be applied. | |||
#* The pad reduces pressure under painful MT heads by spreading it to a larger area, improving functional ability. | |||
#* The optimal method is to apply an MT pad just proximal to the MT head. It also elevates the horizontal arch of the forefoot, which can widen the space between MT heads, reducing interdigital nerve compression and irritation<ref name=":5" />. | |||
#* Use of an MT bar or forefoot cushion is also effective for controlling metatarsalgia | |||
#* In a double-blind study, tear-drop shaped, polyurethane metatarsal pads were applied by experienced physiatrists to a total of 18 feet. As a result, there were significantly decreased maximal peak pressures and pressure time intervals during exercise that correlated with better pain and function outcomes. <ref name=":1" />, | |||
#* Accommodative insoles may redistribute pressure under the foot while functional orthoses are intended to control abnormal intersegmental motion.<ref>Espinosa, Norman, Ernesto Maceira, and Mark S. Myerson. "Current concept review: metatarsalgia." Foot & ankle international 29.8</ref>[[File:Calf Stretch Composite.jpg|right|frameless|500x500px]] | |||
#[[Stretching|Stretches]] | |||
#* A stretching regime is a fundamental element in recovery (helps to alleviate pain) | |||
#* Gajdosic et al demonstrated that a 6-week stretching program increased the maximal ankle dorsiflexion angle and length extensibility and enhanced the dynamic passive length and passive resistive properties. <ref>Gajdosik, RL, et al., A stretching program increases the dynamic passive length and passive resistive properties of the calf muscle-tendon unit of unconditioned younger women. Eur J Appl Physiol.</ref>.The most important areas to focus on are the calf muscles, [[Achilles Tendon|achilles tendon]]<nowiki/>s, ankles, and toes. Below are five recommended stretches. | |||
#* Calf-stretch Stand at an arm’s length away from a wall, placing your hands on it. Step forward with one foot, keeping the back heel on the floor with your knee straight. Hold the stretch for 30-60 seconds before switching legs Achilles tendon - Stretch Stand on a step, with your heels hanging off the edge. Slowly lower your heels until you feel the stretch, and hold for a few seconds. Lift your heels back up so that they’re level with the step. Repeat. | |||
#* Ankle Extension Sit in a chair, and cross the injured foot over your knee. Hold the ankle with your hand on the same side, and your toes in the opposite hand. Pull your toes towards you until it’s uncomfortable (but not painful). Hold for 5-10 seconds. Ankle Flex Again, sit in a chair with the injured foot over your knee. This time, hold your ankle with the hand of the opposite side, and your toes with the hand of the same side. Pull your toes towards you until it’s uncomfortable. Hold for 5-10 seconds.[[File:Towel crunch.PNG|right|frameless]] | |||
# Strengthening - Strengthening key muscles which can help in preventing metatarsalgia. Yoo et all found - After small foot exercising for 2 weeks, the pressure pain threshold increased from 1 to 1.5 kg, while the peak contact pressure decreased from 0.63 to 0.50 kg/cm2, and the navicular drop improved from 5 to 8 mm<ref>Yoo WG. Effect of the Intrinsic Foot Muscle Exercise Combined with Interphalangeal Flexion Exercise on Metatarsalgia with Morton’s Toe. Journal of physical therapy science. 2014;26(12):1997-8. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4273076/ (last accessed 25.6.2020)</ref>. | |||
#* Toe towel-scrunches: Stand barefooted, with one foot in front standing on a towel. Maintain a slight bend in the leg that is touching the towel. Use your toes to scrunch up the towel, making sure that the rest of the foot does not leave the ground. Perform 3 sets of 15 scrunches per foot. | |||
#Electrotherapeutic modalities such as [[Cryotherapy|icing]], ultrasound or interferential therapy may be of assistance to reduce pain and inflammation in the beginning stages of treatment as well<ref>enertor [https://enertor.com/blogs/injury-prevention-and-advice/metatarsalgia-exercises metatarsalgia exercises] Available from:https://enertor.com/blogs/injury-prevention-and-advice/metatarsalgia-exercises (last accessed 25.6.2020)</ref>. | |||
#Sometimes, in very specific cases, an infiltration, followed by taping a few weeks, brings some comfort.<ref name=":1" /> | |||
* | |||
* | |||
* | == Final Comments == | ||
* Metatarsalgia is a condition in which the ball the foot becomes painful and inflamed. | |||
[[File:Heel-foot-feature-1021x517.jpg|right|frameless]] | |||
* Causes include - activities that involve running and jumping, foot deformities and shoes that are too tight or too loose. | |||
* Generally not serious | |||
* Conservative measures such as ice and rest, often relieve symptoms. Wearing proper footwear with shock-absorbing insoles or orthoses may prevent or minimize future problems with metatarsalgia. | |||
== References == | == References == | ||
[[Category:Foot]] | |||
[[Category:Foot - Conditions]] | |||
[[Category:Conditions]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
<references /> | |||
[[Category:Foot]] [[Category: | |||
Latest revision as of 23:33, 13 August 2023
Original Editors - David De Meyer
Top Contributors - Diego Zaragoza, Lucinda hampton, Maxim de Clippele, David De Meyer, Evan Thomas, Kim Jackson, Admin, Rachael Lowe, Adam Vallely Farrell, Chrysolite Jyothi Kommu, Jess Bell, 127.0.0.1, Simisola Ajeyalemi, Khloud Shreif and WikiSysop
Definition[edit | edit source]
Metatarsalgia is a general term for pain in the area of the metatarsophalangeal joints. This is often seen in clinical practice, the deformity and pain can deteriorate gait function and decrease quality of life[2].
Most common causes include:
- Interdigital nerve pain (Morton neuroma)
- Metatarsophalangeal joint pain
- Sesamoiditis
- Submetatarsal head fat pad atrophy typically associated with aging[3]
Metatarsalgies are often accompanied by excessive callus formation over a bony protrusion, with severe pain and pressure sensitivity around the callus.[4][5]
Clinically Relevant Anatomy[edit | edit source]
The most important and relevant anatomy is the forefoot and the metatarsal. The metatarsus of the foot consists of five long bones, which are called the metatarsals.
Metatarsals:
- Comprised of: proximal base; shaft; distal head.
- Proximally connected to the tarsal bones and distally to the phalanges.
- Named I to V medially to laterally, from the dorsal surface of the foot.
- Convex on their dorsal surfaces but concave on their plantar surfaces
- Along with the tarsals, help form the arches of the foot, which are essential in both weight-bearing and walking.[6]
The joints between the head of the metatarsals and the respective proximal phalanx are called the metatarsophalangeal joint (MTP).
- These joints form the ball of the foot, and the ability to move in these joints is very important for normal walking.
- In addition, the bases of the metatarsals articulate with each other to form intermetatarsal joints.[6]
Etiology[edit | edit source]
Common causes include:
- Overtraining
- Interdigital (Morton) neuroma
- Freiberg infraction
- Stress fractures involving the foot
- Intermetatarsal bursitis
- Adventitial bursitis
- Inflammatory and degenerative arthritis
- Metatarsophalangeal joint synovitis/capsulitis
- Tendinosis/tenosynovitis
- Plantar plate disruption / plantar plate tears
- Schwannoma[7]
- Pes cavus or high arched foot
- Excessive pronation of the foot
- Clawing or hammer toes
- Tight extensor tendons of the toes
- Prominent metatarsal heads
- Morton’s foot—there is a shortened first metatarsal, which results in an abnormal subtalar joint, and increased weight going through the second metatarsophalangeal joint.[8]
Causes[edit | edit source]
There can be multiple causative factors. Often localized to the first metatarsal head.Next most frequent site of metatarsal head pain is under the second metatarsal.[5][9][10]
Factors that can cause excessive pressure are:
- Participating in high impact activities without proper footwear and/or orthotics
- Older age as the pad in the foot tends to thin out making it much more susceptible pressue and pain
- An imbalance in the length of the metatarsals
- Majority seem to be related to foot and ankle deformity
- Disturbances in gait
- Morphology of the foot (e.g. increased bone length that protrudes into the bottom of the foot)
- A shortened Achilles tendon
Subtypes[edit | edit source]
- Primary metatarsalgia refers to symptoms arising from innate abnormalities in the patient’s anatomy leading to overload of the affected metatarsal. [11]
- Secondairy metatarsalgia can be caused by systemic conditions such as arthritis of the MTP joint.
- Iatrogenic metatarsalgia can occur after (failed) reconstructive surgery.
Characteristics/Clinical Presentation[edit | edit source]
- Metatarsalgia most commonly results from misalignment of the joint surfaces with altered foot biomechanics, may cause
- Joint subluxations,
- Flexor plate tears (a fibrocartilaginous structure that lies directly plantar to the lesser metatarsal heads and acts as a sesamoid-like mechanism for each lesser joint (MPJ) of the foot[12])
- Increased pain during the mid-stance and propulsion phases of walking as body weight is shifted forward onto the forefoot.[13]
- Capsular impingement
- Joint cartilage destruction (osteoarthrosis).
- Misaligned joints synovial impingement, with minimal if any heat and swelling (osteoarthritic synovitis).
- Metatarsophalangeal joint subluxation - May occur as a result of chronic inflammatory arthropathy, particularly rheumatoid arthritis (RA)
- Metatarsophalangeal joint pain - weight bearing and a sense of stiffness in the morning.
- Loss of metatarsal fat pad (usually cushions the stress between the metatarsals and interdigital nerves during walking) tends to move distally under the toes, causing interdigital neuralgia/Morton neuroma.
- To compensate for the loss of cushioning, adventitial calluses and bursae may develop.
- Coexisting rheumatoid nodules beneath or near the plantarflexed metatarsal heads may increase pain.
The 2nd metatarsophalangeal joint is most commonly affected. - Usually, inadequate 1st ray (1st cuneiform and 1st metatarsal) function results from excessive pronation (the foot rolling inward and the hindfoot turning outward or everted), often leading to capsulitis and hammer toe deformities.
- Overactivity of the anterior shin muscles in patients with pes cavus (high arch) and ankle equinus (shortened Achilles tendon that restricts ankle dorsiflexion) deformities tends to cause dorsal joint subluxations with retracted (clawed) digits and retrograde, increased submetatarsal head pressure and pain[3].
- Metatarsophalangeal joint pain may also result from functional hallux limitus (see xray R)
- Limits passive and active joint motion at the 1st metatarsophalangeal joint.
- Patients usually have foot pronation disorders that result in elevation of the 1st ray with lowering of the medial longitudinal arch during weight bearing.
- As a result of the 1st ray elevation, the proximal phalanx of the great toe cannot freely extend on the 1st metatarsal head; the result is jamming at the dorsal joint leading to osteoarthritic changes and loss of joint motion (with time, pain may develop).
- Another cause of 1st metatarsophalangeal joint pain due to limited motion is direct trauma with stenosis of the flexor hallucis brevis, usually occurring within the tarsal tunnel. If pain is chronic, the joint may become less mobile with an arthrosis (hallux rigidus), which can be debilitating.
- Acute arthritis can occur secondary to systemic arthritides such as gout, RA, and spondyloarthropathy.[3]
Differential Diagnosis[edit | edit source]
Diagnostic Procedures[edit | edit source]
- Mainly clinical evaluation
- Exclusion of infection or arthropathy if signs of inflammation
- To differentiate one diagnosis from another, the use of the patient’s history, physical exam, roentgenograms, cholesterol-crystal force-plate analysis, intra-articular/digital injections, and additional laboratory studies (electromyography, arteriograms, venograms,..) can be used.[14]
- Investigations - X-rays can be performed to assess the degree of degeneration of the joint.
Outcome Measures[edit | edit source]
- Foot Function Index (FFI) - The Brazilian-Portuguese version of the FFI questionnaire was found to be a valid and reliable instrument for foot function evaluation, and can be used both in scientific settings and in clinical practice.[15]
- Foot Posture Index (FP1-6) - No scientific evidence found correlated to metarsalgia[16]
Medical Management[edit | edit source]
Orthotics :
- Foot orthoses with metatarsal pads may help redistribute and relieve pressure from the noninflamed joints.
- With excess subtalar eversion or when the feet are highly arched, an orthotic that corrects these abnormal alignments should be prescribed.
- Shoes with rocker sole modifications may also help.
- For functional hallux limitus, orthosis modifications may further help to plantarflex the 1st ray to improve metatarsophalangeal joint motion and reduce pain.
- If the 1st ray elevation cannot be reduced by these means, an extended 1st ray elevation pad may be helpful.
- For more severe limitation of 1st metatarsophalangeal motion or pain, the use of rigid orthoses, carbon fiber plates, or external shoe bars or rocker soles may be necessary to reduce motion at the joint.[3]
Surgery may be needed if conservative therapies are ineffective. If inflammation (synovitis) is present, injection of a local corticosteroid/anesthetic mixture may be useful.
NSAIDS are most commonly used for the relief of mild to moderate pain. But you have to use the right shoes.[9],
Physical Therapy Management[edit | edit source]
For the management of these disorders, physiotherapy treatment is usually attempted prior to surgical intervention.
Physiotherapy Treatments include - education, orthoses & corrective shoes, stretching of specific lower limb muscles, small foot strengthening exercises,
- Education
- Initially reducing or stopping exercise, substitute a non WB exercise eg pool running, cycling.
- Suspend training until the pain begins to subside
- Once client ready to exercise/walk again avoid future injury by educating re appropriate footwear
- Pain relief and apply ice packs to the affected area (pain-killers that contain anti-inflammatories to help reduce any swelling). Swelling can also be reduced by elevating feet.
- Orthoses
- For symptomatic relief, an MT pad made of rubber, polyurethane, or silicone can be applied.
- The pad reduces pressure under painful MT heads by spreading it to a larger area, improving functional ability.
- The optimal method is to apply an MT pad just proximal to the MT head. It also elevates the horizontal arch of the forefoot, which can widen the space between MT heads, reducing interdigital nerve compression and irritation[2].
- Use of an MT bar or forefoot cushion is also effective for controlling metatarsalgia
- In a double-blind study, tear-drop shaped, polyurethane metatarsal pads were applied by experienced physiatrists to a total of 18 feet. As a result, there were significantly decreased maximal peak pressures and pressure time intervals during exercise that correlated with better pain and function outcomes. [5],
- Accommodative insoles may redistribute pressure under the foot while functional orthoses are intended to control abnormal intersegmental motion.[17]
- Stretches
- A stretching regime is a fundamental element in recovery (helps to alleviate pain)
- Gajdosic et al demonstrated that a 6-week stretching program increased the maximal ankle dorsiflexion angle and length extensibility and enhanced the dynamic passive length and passive resistive properties. [18].The most important areas to focus on are the calf muscles, achilles tendons, ankles, and toes. Below are five recommended stretches.
- Calf-stretch Stand at an arm’s length away from a wall, placing your hands on it. Step forward with one foot, keeping the back heel on the floor with your knee straight. Hold the stretch for 30-60 seconds before switching legs Achilles tendon - Stretch Stand on a step, with your heels hanging off the edge. Slowly lower your heels until you feel the stretch, and hold for a few seconds. Lift your heels back up so that they’re level with the step. Repeat.
- Ankle Extension Sit in a chair, and cross the injured foot over your knee. Hold the ankle with your hand on the same side, and your toes in the opposite hand. Pull your toes towards you until it’s uncomfortable (but not painful). Hold for 5-10 seconds. Ankle Flex Again, sit in a chair with the injured foot over your knee. This time, hold your ankle with the hand of the opposite side, and your toes with the hand of the same side. Pull your toes towards you until it’s uncomfortable. Hold for 5-10 seconds.
- Strengthening - Strengthening key muscles which can help in preventing metatarsalgia. Yoo et all found - After small foot exercising for 2 weeks, the pressure pain threshold increased from 1 to 1.5 kg, while the peak contact pressure decreased from 0.63 to 0.50 kg/cm2, and the navicular drop improved from 5 to 8 mm[19].
- Toe towel-scrunches: Stand barefooted, with one foot in front standing on a towel. Maintain a slight bend in the leg that is touching the towel. Use your toes to scrunch up the towel, making sure that the rest of the foot does not leave the ground. Perform 3 sets of 15 scrunches per foot.
- Electrotherapeutic modalities such as icing, ultrasound or interferential therapy may be of assistance to reduce pain and inflammation in the beginning stages of treatment as well[20].
- Sometimes, in very specific cases, an infiltration, followed by taping a few weeks, brings some comfort.[5]
Final Comments[edit | edit source]
- Metatarsalgia is a condition in which the ball the foot becomes painful and inflamed.
- Causes include - activities that involve running and jumping, foot deformities and shoes that are too tight or too loose.
- Generally not serious
- Conservative measures such as ice and rest, often relieve symptoms. Wearing proper footwear with shock-absorbing insoles or orthoses may prevent or minimize future problems with metatarsalgia.
References[edit | edit source]
- ↑ https://greenbayacupuncture.co/2017/05/17/metatarsalgia-forefoot-pain/
- ↑ 2.0 2.1 Park CH, Chang MC. Forefoot disorders and conservative treatment. Yeungnam University Journal of Medicine. 2019 May;36(2):92.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6784640/ (last accessed 25.6.2020)
- ↑ 3.0 3.1 3.2 3.3 Mercks manual. MTP joint pain Available from:https://www.merckmanuals.com/professional/musculoskeletal-and-connective-tissue-disorders/foot-and-ankle-disorders/metatarsophalangeal-joint-pain (last accessed 25.6.2020)
- ↑ Doty, Jesse F., and Michael J. Coughlin. "Metatarsophalangeal joint instability of the lesser toes." The Journal of Foot and Ankle Surgery 53.4 (2014): 440-445.
- ↑ 5.0 5.1 5.2 5.3 Espinosa, Norman, Ernesto Maceira, and Mark S. Myerson. "Current concept review: metatarsalgia." Foot & ankle international 29.8 (2008)
- ↑ 6.0 6.1 https://www.kenhub.com/en/library/anatomy/metatarsal-bones
- ↑ Radiopedia Metatarsalgia Available from:https://radiopaedia.org/articles/metatarsalgia (last accessed 25.6.2020)
- ↑ Brukner P. Brukner & Khan's clinical sports medicine. North Ryde: McGraw-Hill; 2012.
- ↑ 9.0 9.1 G. McPoil Thomas and Schuit Dale. “Management of metatarsalgia secondary to biomechanical disorders”. Physical Therapy 66(6): 970-2; July 1986
- ↑ Sobel Ellen, D.P.M., Ph. D., C.PED. and Levitz Steven, D.P.M.; “Metatarsalgia : Diagnosis and Manangement, Etiologies and Differential diagnoses”. Podiatry Management
- ↑ Espinosa, Norman, Ernesto Maceira, and Mark S. Myerson. "Current concept review: metatarsalgia." Foot & ankle international 29.8 (2008)
- ↑ Podiatry today Understanding PP injuries Available from:https://www.podiatrytoday.com/understanding-biomechanics-plantar-plate-injuries (last accessed 25.6.2020)
- ↑ G. McPoil Thomas and Schuit Dale. “Management of metatarsalgia secondary to biomechanical disorders”. Physical Therapy 66(6): 970-2; July 1986
- ↑ J Bone Joint Surg Am. 1980 Jul;62(5):723-32. Scranton PE Jr; Metatarsalgia: diagnosis and treatment
- ↑ Martinez, Bruna Reclusa, et al. Validity and reliability of the Foot Function Index (FFI) questionnaire Brazilian-Portuguese version. 2016.
- ↑ Haque, Syed, et al. Outcome of Minimally Invasive Distal Metatarsal Metaphyseal Osteotomy (DMMO) for Lesser Toe Metatarsalgia. Foot & Ankle International. 2015.
- ↑ Espinosa, Norman, Ernesto Maceira, and Mark S. Myerson. "Current concept review: metatarsalgia." Foot & ankle international 29.8
- ↑ Gajdosik, RL, et al., A stretching program increases the dynamic passive length and passive resistive properties of the calf muscle-tendon unit of unconditioned younger women. Eur J Appl Physiol.
- ↑ Yoo WG. Effect of the Intrinsic Foot Muscle Exercise Combined with Interphalangeal Flexion Exercise on Metatarsalgia with Morton’s Toe. Journal of physical therapy science. 2014;26(12):1997-8. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4273076/ (last accessed 25.6.2020)
- ↑ enertor metatarsalgia exercises Available from:https://enertor.com/blogs/injury-prevention-and-advice/metatarsalgia-exercises (last accessed 25.6.2020)
![[1]](/images/thumb/5/5f/Metatarsalgia.jpg/435px-Metatarsalgia.jpg)