Medial ankle ligament: Difference between revisions
No edit summary |
No edit summary |
||
| (14 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User: Nicolas D'Hondt | Nicolas D'Hondt]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
| Line 7: | Line 7: | ||
== Introduction == | == Introduction == | ||
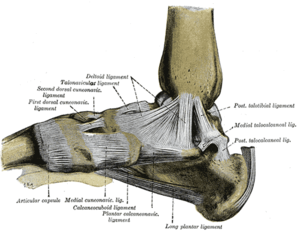
[[File: | [[File:Foot ligaments.png|alt=https://en.wikipedia.org/wiki/Deltoid_ligament#/media/File:Gray354.png|thumb|Medial Ankle Ligament]] | ||
The Deltoid ligament (or the medial ligament of [[Ankle Joint|talocrural joint]]) is a strong, flat and triangular band. It is made up of 4 ligaments that form the triangle, connecting the tibia to the [[navicular]], the [[calcaneus]], and the [[talus]]<ref name=":0">Manganaro D, Alsayouri K. [https://www.ncbi.nlm.nih.gov/books/NBK545158/ Anatomy, Bony Pelvis and Lower Limb, Ankle Joint.] 2020 Aug 16. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–. PMID: 31424742.</ref> .It is attached above to the apex and anterior and posterior borders of the medial malleolus. The plantar calcaneonavicular ligament can be considered as part of the medial ligament complex. | |||
The Deltoid ligament is composed of superficial and deep components. | The Deltoid ligament is composed of superficial and deep components. | ||
| Line 21: | Line 22: | ||
The anterior and posterior tibiotalar ligaments attach the tibia to the talus <ref name=":0" />. | The anterior and posterior tibiotalar ligaments attach the tibia to the talus <ref name=":0" />. | ||
{{#ev: youtube | r8zHxUZnvW0}} | {{#ev: youtube | r8zHxUZnvW0}} <ref>Medial Ligament Complex Of The Ankle Anatomy. Available from: http://www.youtube.com/watch?v=r8zHxUZnvW0</ref> | ||
<br> | <br> | ||
| Line 30: | Line 33: | ||
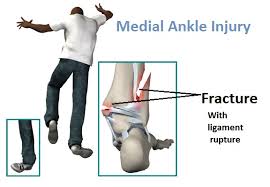
'''The deep deltoid''' originates on posterior border of anterior colliculus, intercollicular groove, & posterior colliculus. It is oriented transversely & inserts into the entire non articular surface of the medial talus. Deep deltoid extends the function of the medial malleolus, prevents lateral displacement and external rotation of the talus (this is mostly significant in plantar flexion, when deep deltoid tends to pull talus into internal rotation). [[File:Fracture with eversion injury.jpg|thumb]] | '''The deep deltoid''' originates on posterior border of anterior colliculus, intercollicular groove, & posterior colliculus. It is oriented transversely & inserts into the entire non articular surface of the medial talus. Deep deltoid extends the function of the medial malleolus, prevents lateral displacement and external rotation of the talus (this is mostly significant in plantar flexion, when deep deltoid tends to pull talus into internal rotation). [[File:Fracture with eversion injury.jpg|thumb]] | ||
Medial ankle stability is provided by the strong deltoid ligament, the anterior tibiofibular ligament and the bony mortise. Because of the bony articulation between the medial malleolus and the talus, medial [http://www.physio-pedia.com/Ankle_Sprain ankle sprains] are less common than [http://www.physio-pedia.com/Lateral_Ligament_Injury_of_the_Ankle lateral sprains]. In medial [http://www.physio-pedia.com/Ankle_Sprain ankle sprains], the mechanism of injury is excessive eversion and dorsiflexion. <ref>Wolfe MW | Medial ankle stability is provided by the strong deltoid ligament, the anterior tibiofibular ligament and the bony mortise. Because of the bony articulation between the medial malleolus and the talus, medial [http://www.physio-pedia.com/Ankle_Sprain ankle sprains] are less common than [http://www.physio-pedia.com/Lateral_Ligament_Injury_of_the_Ankle lateral sprains]. In medial [http://www.physio-pedia.com/Ankle_Sprain ankle sprains], the mechanism of injury is excessive eversion and dorsiflexion. <ref name=":1">Wolfe, MW & Uhl, Tim & Mattacola, Carl & McCluskey, LC. (2001). [https://www.researchgate.net/publication/299146294_Management_of_ankle_sprains_vol_63_pg_93_2001 Management of ankle sprains] (vol 63, pg 93, 2001). American family physician. 64. 386-386.</ref><ref name=":1" /> <br> | ||
Isolated deltoid ligament injuries are extremely rare and usually occur in combination with [http://www.physio-pedia.com/Ankle_%26_Foot_Fractures fractures] of the lateral malleolus. These are treated by | Isolated deltoid ligament injuries are extremely rare and usually occur in combination with [http://www.physio-pedia.com/Ankle_%26_Foot_Fractures fractures] of the lateral malleolus. These are treated by recognising the injury complex and stabilising the lateral side, being sure that the mortise is reduced. <ref>Brand RL, Collins MD. [https://pubmed.ncbi.nlm.nih.gov/7186838/ Operative management of ligamentous injuries to the ankle]. Clin Sports Med. 1982 Mar;1(1):117-30.</ref> | ||
{{#ev: youtube | R0WSeOUwX3s}} | {{#ev: youtube | R0WSeOUwX3s}}<ref>MRI Anatomy of Ankle Ligaments: Deltoid Ligament. Available from: http://www.youtube.com/watch?v=R0WSeOUwX3s </ref> | ||
== Physical Examination == | == Physical Examination == | ||
Eversion Test-<br> In neutral, it evaluates superficial deltoid ligament complex.<br> External rotation stress test evaluates syndesmotic ligaments and additionally - the deep deltoid ligament; | Eversion Test-<br> In neutral, it evaluates superficial deltoid ligament complex.<br> External rotation stress test evaluates syndesmotic ligaments and additionally - the deep deltoid ligament; | ||
The test is performed by everting and abducting the heel with one hand, while stabilizing the tibia (and fibula) with the other. Increased laxity or pain indicates a positive test <ref>de Vries JS, Kerkhoffs GM, Blankevoort L, van Dijk CN. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855027/ Clinical evaluation of a dynamic test for lateral ankle ligament laxity.] Knee Surg Sports Traumatol Arthrosc. 2010 May;18(5):628-33 | The test is performed by everting and abducting the heel with one hand, while stabilizing the tibia (and fibula) with the other. Increased laxity or pain indicates a positive test <ref>de Vries JS, Kerkhoffs GM, Blankevoort L, van Dijk CN. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855027/ Clinical evaluation of a dynamic test for lateral ankle ligament laxity.] Knee Surg Sports Traumatol Arthrosc. 2010 May;18(5):628-33. </ref>.<br><br> | ||
{{#ev: youtube | ou5KzSWaqE0}} | {{#ev: youtube | ou5KzSWaqE0}}<ref>Deltoid Ligament Stress Test Ankle | Clinical Physio Premium. Available from: http://www.youtube.com/watch?v=ou5KzSWaqE0</ref> | ||
== Radiographic Diagnosis of Injury == | == Radiographic Diagnosis of Injury == | ||
Deltoid is usually avulsed from tibial attachment, frequently with small flake of bone visible on x-rays; | Deltoid is usually avulsed from tibial attachment, frequently with small flake of bone visible on x-rays; | ||
* disruption of deltoid ligament can be diagnosed with relative confidence when medial clear space between talus & med malleolus is increased | |||
* lateral shift of talus, with increased medial joint space ( > 3 mm), but this may be apparent only on stress view or in post casting films, after swelling has subsided; | |||
* presence of medial tenderness & > 5 mm of visible space indicates substantial injury to the deltoid ligament;<br> | |||
== Treatment of Deltoid Tear == | == Treatment of Deltoid Tear == | ||
* such injuries should be treated as bimalleolar fractures w/ ORIF of lateral malleolus; | |||
* routine exploration of medial side of ankle is not necessary unless there is evidence that portion of deltoid lig has entered joint & is blocking reduction of talus. | |||
{{#ev: youtube | tYmrsM3f-b4}}<ref>case takeaway - maisonneuve ankle fracture and medial deltoid ligament injury - Lyndon Mason. Available from: http://www.youtube.com/watch?v=tYmrsM3f-b4 </ref> | |||
{{#ev: youtube | tYmrsM3f-b4}} | |||
<br> | <br> | ||
| Line 58: | Line 63: | ||
<br>To avoid [http://www.physio-pedia.com/Ankle_Sprain ankle sprains], or ankle instabilities there are rehab exercises which re enforce or retrain the medial ligaments of the [http://www.physio-pedia.com/Ankle_%26_Foot ankle]. These ligaments are important as they prevent excessive eversion of the [http://www.physio-pedia.com/Ankle_%26_Foot ankle] (eversion trauma). | <br>To avoid [http://www.physio-pedia.com/Ankle_Sprain ankle sprains], or ankle instabilities there are rehab exercises which re enforce or retrain the medial ligaments of the [http://www.physio-pedia.com/Ankle_%26_Foot ankle]. These ligaments are important as they prevent excessive eversion of the [http://www.physio-pedia.com/Ankle_%26_Foot ankle] (eversion trauma). | ||
First and second degree sprains are typically managed with conservative treatment. In the early stages, the conservative treatment consists of [http://www.physio-pedia.com/RICE RICE] (rest, ice, compress, elevate) and mobilization to prevent range of motion loss. When pain and inflammation are controlled, we can start with therapeutic exercises to increase the range of motion stability, strength proprioception and function. | First and second degree sprains are typically managed with conservative treatment. In the early stages, the conservative treatment consists of [http://www.physio-pedia.com/RICE RICE] (rest, ice, compress, elevate) and mobilization to prevent range of motion loss. When pain and inflammation are controlled, we can start with therapeutic exercises to increase the range of motion, stability, strength, proprioception and function. | ||
{{#ev: youtube |3TYj_ugUM7w}}<ref>Best Ankle Rehabilitation Exercises for Those Recovering From Ankle Injury. Available from: http://www.youtube.com/watch?v=3TYj_ugUM7w</ref> | |||
For third degree sprains, structural damage has most likely occurred, needing surgical interventions. After the surgery, the [http://www.physio-pedia.com/Ankle_%26_Foot ankle] is immobilized. In case there is pain or oedema after immobilization, the first treatment protocol is to attend to the pain and oedema. This will follow the same guidelines as for the first and second degree sprains conservative management as above. | |||
For | After two weeks or as and when the pain and swelling allows, strengthening exercises for the medial muscles and ligaments of the [http://www.physio-pedia.com/Ankle_%26_Foot ankle] can be started. The strengthening program can be started with low resistance exercises. For example, the patient sits on a chair or massage table with his/her leg extended (long sitting). The physiotherapist stabilizes the leg with one hand, just below the knee. With the other, the lateral side of the [http://www.physio-pedia.com/Ankle_%26_Foot ankle] is held. The physiotherapist moves the foot into inversion, and provides some manual resistance. The patient then has to perform eversion movement, against this resistance. The resistance is held for 3 to 5 seconds. The exercise is repeated for 10 to 12 times. <ref>Mattacola CG, Dwyer MK. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164373/. Rehabilitation of the Ankle After Acute Sprain or Chronic Instability]. ''J Athl Train''. 2002;37(4):413-429.</ref> | ||
<br>The above exercise can also be done without the resistance of a physiotherapist. The patient sits on a chair. An elastic tubing or resistance band is put around the foot, and the other foot is placed on the elastic tubing, while holding the elastic tubing in the contralateral hand. The same exercise movement is performed but using the band as the resistance. The patient pushes the foot outward, with the foot pad away from the mid-line of the body. | |||
< | {{#ev: youtube | VyeqglvCwdE}}<ref>Theraband Muscle Strengthening Inversion and Eversion. Available from: http://www.youtube.com/watch?v=VyeqglvCwdE</ref> | ||
{{#ev: youtube | | <br>Proprioceptive exercises can be included after 5 weeks. To make these exercises more difficult the therapist can vary the surfaces - on the floor/a balance board or any other an unstable ground.For example, the patient is made to sit on a chair, with their feet on a kinaesthetic ankle board (KAB). The patient is asked to keep their knees at a 90° angle, while maintaining contact with the top of the KAB with their respective extremities. Once in position, the patient rotates the board to the left side and then back to the right (=clockwise and counter clockwise), while maintain the side of the board in contact with the floor each time they moved the board to the left or right. This is done 25 repetitions x 3 sets. <ref>Mattacola CG, Lloyd JW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1319815/ Effects of a 6-week strength and proprioception training program on measures of dynamic balance: a single-case design]. ''J Athl Train''. 1997;32(2):127-135.</ref>. The progression of this exercise is single leg stance on the balance board and maintaining the stance, first with eyes open and thereafter closed, 30 second each manoeuvre. <ref>Söderman, Kerstin & Werner, S & Pietilä, T & Engström, B & Alfredson, Håkan. (2000). [https://pubmed.ncbi.nlm.nih.gov/11147154/ Balance board training: Prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study]. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 8. 356-63.</ref>. {{#ev: youtube | PB6469tDyLg}}<ref>Best Balance Board System for Ankle & Knee Rehab, Strength, Balance & Proprioception. Available from: http://www.youtube.com/watch?v=PB6469tDyLg</ref> | ||
Another way to increase the difficulty level is to attempt the exercises without visual input, by closing the eyes while performing the exercises. <br>An example for this is, the patient performs a single leg stance on a flat surface first with their eyes open and closed thereafter. The progression of this exercise can be performing the same maneuver but on a balance/wobble board with and with out visual input. Each exercise is performed 15 reps x 3 sets. Another progression using the wobble board can be standing with both feet on the board and perform circular movements as this will not only train eversion, but also inversion, dorsiflexion and plantar flexion. <br> | |||
The | The physiotherapist could also further increase the skill level of various above exercises by giving light perturbations while the subject balances on the balance board. | ||
{{#ev: youtube | aTNwQr2Pqcw}}<ref>Ankle Proprioception Exercise. Available from: http://www.youtube.com/watch?v=aTNwQr2Pqcw</ref> | |||
== Refrences == | == Refrences == | ||
| Line 84: | Line 89: | ||
[[Category:Anatomy]] | [[Category:Anatomy]] | ||
<references /> | <references /> | ||
[[Category:Ligaments]] | |||
[[Category:Ankle - Anatomy]] | |||
[[Category:Ankle - Ligaments]] | |||
Latest revision as of 19:41, 9 October 2020
Original Editor - Nicolas D'Hondt Top Contributors - Saumya Srivastava, Mariam Hashem, Nicolas D'Hondt, George Prudden, Venugopal Pawar and Priyanka Chugh
Introduction[edit | edit source]
The Deltoid ligament (or the medial ligament of talocrural joint) is a strong, flat and triangular band. It is made up of 4 ligaments that form the triangle, connecting the tibia to the navicular, the calcaneus, and the talus[1] .It is attached above to the apex and anterior and posterior borders of the medial malleolus. The plantar calcaneonavicular ligament can be considered as part of the medial ligament complex.
The Deltoid ligament is composed of superficial and deep components.
The superficial components:
- The tibiocalcaneal ligament descends almost vertically to the entire length of the sustentaculum tali to attach to the calcaneus inferiorly
- The tibionavicular ligament passes forwards to the navicular tuberosity (to attach to it anteriorly [1]) behind which they blend with the medial margin of the plantar calcaneonavicular ligament
- The posterior superficial tibiotalar ligament passes posterolaterally to the medial side of the talus and its medial tubercle
- The tibiospring ligament descends vertically and blends with the fibres of the spring ligament
The deep components:
- The anterior tibiotalar ligament (ATTL) passes from the tip of the medial malleolus to the non-articular part of the medial talar surface. It is crossed by the tendons of the tibialis posterior and flexor digitorum longus
- The posterior deep tibiotalar ligament (PDTL) from the medial malleolus to the talus and is covered by the superficial posterior tibiotalar and tibiocalcaneal ligaments
The anterior and posterior tibiotalar ligaments attach the tibia to the talus [1].
Clinically Relevant Anatomy[edit | edit source]
The deltoid ligament attaches the medial malleolus to multiple tarsal bones. Unlike the superficial layer of this ligament, the deep layer is intraarticular and is covered by synovium. Anatomically, in general, the superficial components arise from the anterior colliculus of the medial malleolus, and the deep components arise from the intercollicular groove (malleolar groove) and the posterior colliculus of the medial malleolus.
The superficial deltoid originates from the anterior & inferior aspects of medial malleolus fanning out & sending 3 bands to navicular and along plantar calcaneonavicular (spring) ligament, to sustenaculum tali of calcaneus and to medial tubercle. It is also partially covered by tendon sheaths & crural fascia. It primarily resists eversion of hindfoot; Tibionavicular portion suspends spring lig & prevents inward displacement of head of talus, while tibiocalcaneal portion prevents valgus displacement.
The deep deltoid originates on posterior border of anterior colliculus, intercollicular groove, & posterior colliculus. It is oriented transversely & inserts into the entire non articular surface of the medial talus. Deep deltoid extends the function of the medial malleolus, prevents lateral displacement and external rotation of the talus (this is mostly significant in plantar flexion, when deep deltoid tends to pull talus into internal rotation).
Medial ankle stability is provided by the strong deltoid ligament, the anterior tibiofibular ligament and the bony mortise. Because of the bony articulation between the medial malleolus and the talus, medial ankle sprains are less common than lateral sprains. In medial ankle sprains, the mechanism of injury is excessive eversion and dorsiflexion. [3][3]
Isolated deltoid ligament injuries are extremely rare and usually occur in combination with fractures of the lateral malleolus. These are treated by recognising the injury complex and stabilising the lateral side, being sure that the mortise is reduced. [4]
Physical Examination[edit | edit source]
Eversion Test-
In neutral, it evaluates superficial deltoid ligament complex.
External rotation stress test evaluates syndesmotic ligaments and additionally - the deep deltoid ligament;
The test is performed by everting and abducting the heel with one hand, while stabilizing the tibia (and fibula) with the other. Increased laxity or pain indicates a positive test [6].
Radiographic Diagnosis of Injury[edit | edit source]
Deltoid is usually avulsed from tibial attachment, frequently with small flake of bone visible on x-rays;
- disruption of deltoid ligament can be diagnosed with relative confidence when medial clear space between talus & med malleolus is increased
- lateral shift of talus, with increased medial joint space ( > 3 mm), but this may be apparent only on stress view or in post casting films, after swelling has subsided;
- presence of medial tenderness & > 5 mm of visible space indicates substantial injury to the deltoid ligament;
Treatment of Deltoid Tear[edit | edit source]
- such injuries should be treated as bimalleolar fractures w/ ORIF of lateral malleolus;
- routine exploration of medial side of ankle is not necessary unless there is evidence that portion of deltoid lig has entered joint & is blocking reduction of talus.
Physical Therapy Management[edit | edit source]
To avoid ankle sprains, or ankle instabilities there are rehab exercises which re enforce or retrain the medial ligaments of the ankle. These ligaments are important as they prevent excessive eversion of the ankle (eversion trauma).
First and second degree sprains are typically managed with conservative treatment. In the early stages, the conservative treatment consists of RICE (rest, ice, compress, elevate) and mobilization to prevent range of motion loss. When pain and inflammation are controlled, we can start with therapeutic exercises to increase the range of motion, stability, strength, proprioception and function.
For third degree sprains, structural damage has most likely occurred, needing surgical interventions. After the surgery, the ankle is immobilized. In case there is pain or oedema after immobilization, the first treatment protocol is to attend to the pain and oedema. This will follow the same guidelines as for the first and second degree sprains conservative management as above.
After two weeks or as and when the pain and swelling allows, strengthening exercises for the medial muscles and ligaments of the ankle can be started. The strengthening program can be started with low resistance exercises. For example, the patient sits on a chair or massage table with his/her leg extended (long sitting). The physiotherapist stabilizes the leg with one hand, just below the knee. With the other, the lateral side of the ankle is held. The physiotherapist moves the foot into inversion, and provides some manual resistance. The patient then has to perform eversion movement, against this resistance. The resistance is held for 3 to 5 seconds. The exercise is repeated for 10 to 12 times. [10]
The above exercise can also be done without the resistance of a physiotherapist. The patient sits on a chair. An elastic tubing or resistance band is put around the foot, and the other foot is placed on the elastic tubing, while holding the elastic tubing in the contralateral hand. The same exercise movement is performed but using the band as the resistance. The patient pushes the foot outward, with the foot pad away from the mid-line of the body.
[11]
Proprioceptive exercises can be included after 5 weeks. To make these exercises more difficult the therapist can vary the surfaces - on the floor/a balance board or any other an unstable ground.For example, the patient is made to sit on a chair, with their feet on a kinaesthetic ankle board (KAB). The patient is asked to keep their knees at a 90° angle, while maintaining contact with the top of the KAB with their respective extremities. Once in position, the patient rotates the board to the left side and then back to the right (=clockwise and counter clockwise), while maintain the side of the board in contact with the floor each time they moved the board to the left or right. This is done 25 repetitions x 3 sets. [12]. The progression of this exercise is single leg stance on the balance board and maintaining the stance, first with eyes open and thereafter closed, 30 second each manoeuvre. [13].
Another way to increase the difficulty level is to attempt the exercises without visual input, by closing the eyes while performing the exercises.
An example for this is, the patient performs a single leg stance on a flat surface first with their eyes open and closed thereafter. The progression of this exercise can be performing the same maneuver but on a balance/wobble board with and with out visual input. Each exercise is performed 15 reps x 3 sets. Another progression using the wobble board can be standing with both feet on the board and perform circular movements as this will not only train eversion, but also inversion, dorsiflexion and plantar flexion.
The physiotherapist could also further increase the skill level of various above exercises by giving light perturbations while the subject balances on the balance board.
Refrences[edit | edit source]
- ↑ 1.0 1.1 1.2 Manganaro D, Alsayouri K. Anatomy, Bony Pelvis and Lower Limb, Ankle Joint. 2020 Aug 16. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–. PMID: 31424742.
- ↑ Medial Ligament Complex Of The Ankle Anatomy. Available from: http://www.youtube.com/watch?v=r8zHxUZnvW0
- ↑ 3.0 3.1 Wolfe, MW & Uhl, Tim & Mattacola, Carl & McCluskey, LC. (2001). Management of ankle sprains (vol 63, pg 93, 2001). American family physician. 64. 386-386.
- ↑ Brand RL, Collins MD. Operative management of ligamentous injuries to the ankle. Clin Sports Med. 1982 Mar;1(1):117-30.
- ↑ MRI Anatomy of Ankle Ligaments: Deltoid Ligament. Available from: http://www.youtube.com/watch?v=R0WSeOUwX3s
- ↑ de Vries JS, Kerkhoffs GM, Blankevoort L, van Dijk CN. Clinical evaluation of a dynamic test for lateral ankle ligament laxity. Knee Surg Sports Traumatol Arthrosc. 2010 May;18(5):628-33.
- ↑ Deltoid Ligament Stress Test Ankle | Clinical Physio Premium. Available from: http://www.youtube.com/watch?v=ou5KzSWaqE0
- ↑ case takeaway - maisonneuve ankle fracture and medial deltoid ligament injury - Lyndon Mason. Available from: http://www.youtube.com/watch?v=tYmrsM3f-b4
- ↑ Best Ankle Rehabilitation Exercises for Those Recovering From Ankle Injury. Available from: http://www.youtube.com/watch?v=3TYj_ugUM7w
- ↑ Mattacola CG, Dwyer MK. Rehabilitation of the Ankle After Acute Sprain or Chronic Instability. J Athl Train. 2002;37(4):413-429.
- ↑ Theraband Muscle Strengthening Inversion and Eversion. Available from: http://www.youtube.com/watch?v=VyeqglvCwdE
- ↑ Mattacola CG, Lloyd JW. Effects of a 6-week strength and proprioception training program on measures of dynamic balance: a single-case design. J Athl Train. 1997;32(2):127-135.
- ↑ Söderman, Kerstin & Werner, S & Pietilä, T & Engström, B & Alfredson, Håkan. (2000). Balance board training: Prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 8. 356-63.
- ↑ Best Balance Board System for Ankle & Knee Rehab, Strength, Balance & Proprioception. Available from: http://www.youtube.com/watch?v=PB6469tDyLg
- ↑ Ankle Proprioception Exercise. Available from: http://www.youtube.com/watch?v=aTNwQr2Pqcw